Abstract
Background: Spinal deformities in children can be caused by various etiologies, such as congenital, syndromic, neuromuscular, or idiopathic. Early-onset scoliosis (EOS) is diagnosed before the age of ten years, and when the curvature continues to progress and exceeds a Cobb angle of 60–65 degrees, surgical treatment should be considered. Initial minimally invasive surgery and the implantation of magnetically controlled growing rods (MCGRs) allows for the noninvasive distraction of the spine, growing, and avoids multiple operations associated with the classic distractions of standard growing rods. Case presentation: A 2-year-old girl was admitted to our clinic with rapidly progressive thoracic scoliosis. The major curve of the thoracic spine Cobb angle was 122° at 30 months. No congenital deformities were detected. The surgical technique was the less-invasive percutaneous and subfascial implantation of MCGRs, without long incisions on the back and the non-invasive ambulatory lengthening of her spine over the next 4 years. Conclusions: MCGR is a safe procedure for EOS patients. It is extremely effective at correcting spinal deformity; controlling the growth and curvature of the spine as the child develops during growth; reducing the number of hospitalizations and anesthesia; and minimizing the physical and mental burden of young patients, parents, and their families.
1. Introduction
Spinal deformities in children and adolescents can be caused by various etiologies, such as congenital, syndromic, neuromuscular, or idiopathic [1]. According to the age of diagnosis, we can distinguish early-onset scoliosis (EOS), which is diagnosed before the age of ten years, and late-onset scoliosis, which is diagnosed under the age of ten years [2,3]. At the time of diagnosis, conservative treatment, rehabilitation, and a brace are recommended. In the absence of satisfactory results, when the curvature continues to progress and exceeds a Cobb angle of more than 60 degrees, surgical treatment should be considered [1]. The earlier surgery is started, the more complications we can expect during the entire course of treatment.
The most common procedure for EOS management is the surgical correction of the deformity with growing rods. The most significant disadvantage of this technique is the repetition of successive operations as the child grows, on average every 6 months under general anesthesia, which results in high rates of complications related to the procedure (up to 58%) [4]. MCGRs were designed in 2009 for the surgical treatment of spinal deformity in patients who are less than 10 years of age and have a thoracic spine height of less than 22 cm [5,6,7,8,9]. After the initial surgery and implantation of MCGRs, they allow noninvasive distractions, can reduce complications, and avoid multiple operations associated with the classic distractions of standard growing rods [6,10,11].
Since there are few descriptions and reports in the literature describing the point-by-point implantation techniques of MCGRs, we would like to share our many years of experience in using MCGRs. The aim of our work is to present the less-invasive surgical technique of the implantation of MCGRs and experiences of this procedure gained during the treatment of children with EOS less than 10 years of age, based on a case report of a young child in Europe with severe early-onset idiopathic scoliosis treated surgically with the use of MCGRs, followed by a 6-year observation period.
2. Case Presentation
A 2-year-old girl was admitted to our clinic with rapidly progressive thoracic scoliosis. Previously, the patient had undergone conservative treatment with a brace and physical therapy. The patient had no other disorders. The major curve of the thoracic spine Cobb angle was 70° at 16 months of age, 100° at 22 months, and 122° at 30 months (Figure 1).

Figure 1.
Showed standing: (from left to right) AP X-rays at 16 months old (70 degrees), 22 months old (100 degrees), and 30 months old (122 degrees).
Computed tomography and magnetic resonance imaging were performed. The spinal cord was intact. No other congenital deformities were detected. The patient was born through natural childbirth without any comorbidities (Figure 2).
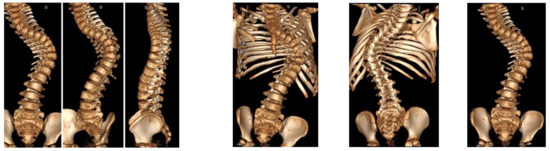
Figure 2.
CT-3D preoperative images.
All examinations, specialist consultations, and clinical statuses showed other causes of spinal deformity. We diagnosed early-onset idiopathic scoliosis with fast progression, which qualified for surgical treatment with growing rods (Figure 3). The flexibility was approximately 30%, so we performed anterior release and spine correction with intraoperative halo traction (Figure 4).

Figure 3.
X-rays and clinical preoperative images.
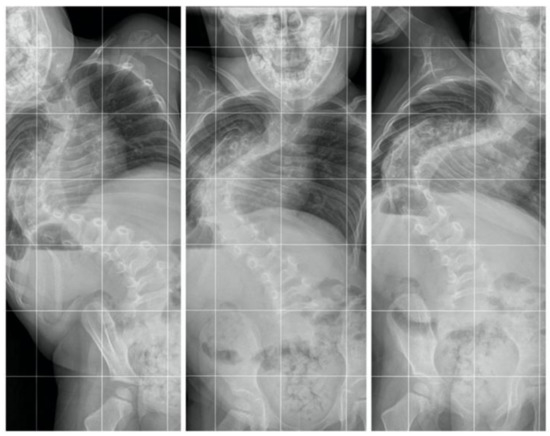
Figure 4.
AP standing bending films.
We placed the patient in a prone position on a Jackson table according to the standard procedure. Each procedure is carried out under the control of the neuromonitoring of the spinal cord. We selected the levels of stabilization of the upper and lower screws before the procedure, and after the analysis of the examined patient, we took X-ray images in the standing position and after assessing spine flexibility on the bending films. Then, after positioning the patient under the control of the C-arm, we marked the screw location levels on the skin, usually T2–T4 and L1–L3. Then, we made a skin incision, usually about 4–5 cm long (depending on the child’s height), to gain access to the levels of screw implantation only (Figure 5).
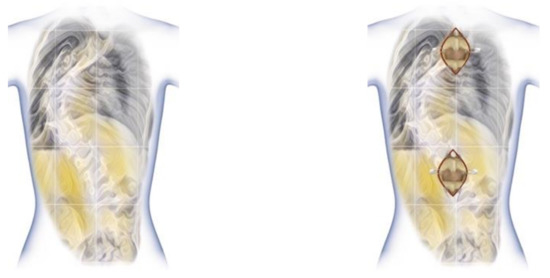
Figure 5.
Less-invasive approach for upper and lower spine.
It is very important to prepare fixation points using two small separate incisions, and the rest of the spine should be left untouched. Next, we undertook the less-invasive implantation of screws, usually using a free-hand technique, but other techniques can also be used, such as navigation or robotic. After checking the adequate position of the screws with the C-arm and neuromonitoring, we made two subfascial tunnels on the left and right sides of the spine to insert the magnetic rods. Using a paean of the right size, we created rod tunnels immediately under the fascia not reaching the spine. To make it easier to guide the rods without damaging the muscles and to avoid perforation to the pleura, we inserted No. 16 drains into the created tunnels. First, we used a temporary rod to identify what the length of the final rod should be, as well as to assess the best method of obtaining the best rod bend (Figure 6a–c).
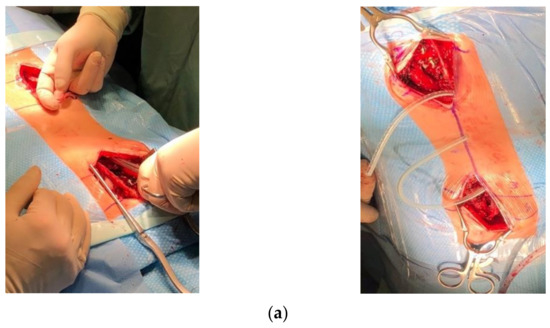
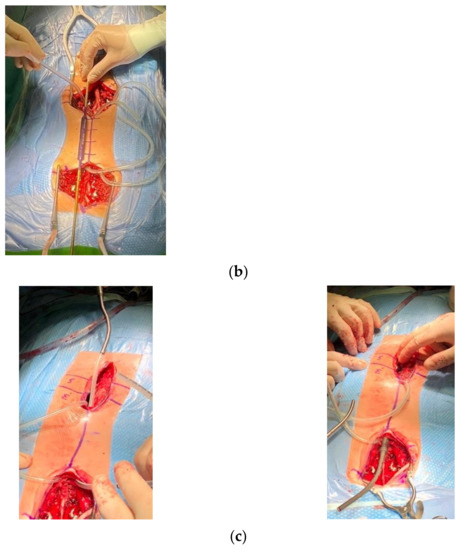
Figure 6.
(a) Intraoperative pictures: using a paean, we created rod tunnels immediately under the fascia not reaching the spine. (b) Using drains as a guide for the insertion of temporary MCGRs. (c) Inserting MCGRs followed by drains.
The next step is to properly cut and bend the magnetic rods. We always use one standard rod and one offset rod. After measuring and cutting the MCGRs, we need to test the efficiency of the rod distraction actuator. The testing of the actuator should be performed before bending the rods and after their proper modeling and contouring to exclude possible damage to the mechanism during the bending of the rod. A very important element of bending the rods is modeling the rods 1 cm above and below the ends of the actuator. This is to prevent mechanical damage to the actuator. However, this method is not perfect, and due to the inability to bend the actuator in any way, we must contend with a completely straight part of the rod with a length of 90 mm or 110 mm, depending on the type of rod used. Another important element is to plan the implantation of magnetic rods in such a way that the actuators of the rods are preferably at the same height. After the rods are properly prepared, we are able to proceed with their insertion. Our technique involves placing the first rod on the left side for right-sided curves and vice versa for left-sided ones. For this patient, we led the rod through the previously prepared tunnel, placing the end of the drain on the end of the rod (Figure 6a–c). We led the rod in the cephalad direction. After affixing the rod to the heads of the screws, we derotated it to an adequate sagittal position and temporarily blocked it. Subsequently, we repeated the process on the opposite side with the second rod. After rod insertion, we performed a gentle distraction distally across the base after the proximal set screws and finished final tightening. We do not routinely use a proximal cross-connector between the rods. For patients with poor bone quality, we use transverse process hooks at the top for the prevention of upper implant pull out. We then completed the final irrigation, the decortication of the bone at the screws, the covering of the bone grafts with vancomycin powder, and a standard closure. During surgery, we used safety distraction for the neuromonitoring of the spinal cord. There were no changes in the SSEP and MEP. No postoperative complications occurred. The patient was discharged on the sixth day after surgery with a brace (for three months). We started distraction after three months. We distracted the MCGRs with the external remote control (ERC) by 1.5–2.5 mm every 8–10 weeks. The radiographic parameters are listed in Table 1. Between 2017 and 2022, 28 distractions were performed (48 mm total).

Table 1.
Radiological parameters before and after surgical treatment.
No deep infections were observed during follow-up. At follow-up after 4.5 years, we observed a loss of distraction without other known radiological signs mentioned in the literature (Figure 7).
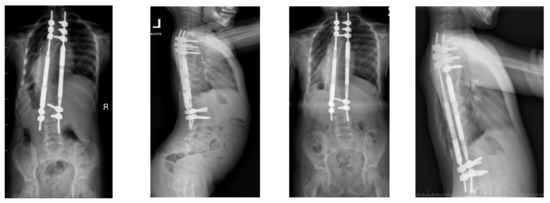
Figure 7.
X-rays at follow-up after 1 year (left AP and LAT) and at follow-up after 4.5 years (right AP and LAT) before revision surgery for MCGR replacement.
We decided to replace the 4.5 MCGR with a 5.5 MCGR. We performed revision surgery to replace the screws and MCGRs in January 2022 (Figure 8).
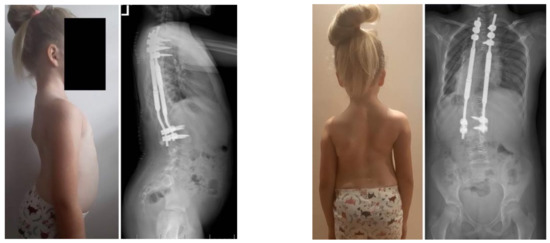
Figure 8.
X-rays at 5-year follow-up, after revision surgery for MCGR replacement.
Intraoperatively, metallosis was observed around the screw–rod junction. After revision surgery, the patient was discharged on the fifth day after surgery without a brace. There was no external rod fracture, but there were many wear marks at the junction between the extended portion of the rod and actuator (Figure 9).

Figure 9.
MCGRs and metallosis during revision surgery.
The removed rods did not function when checked with the ERC. After revision surgery, the child was examined and her new MCGRs were distracted and confirmed via X-ray.
3. Discussion
Initially, EOS can be treated conservatively with rehabilitation and a series of castings, corsets, or braces [1,2,12,13,14]. In the event of failure of this treatment and the further progression of the spinal curvature exceeding a Cobb angle of 60–65 degrees, surgical treatment should be considered [3,5,6,7,12,13,15,16,17,18].
After implantation, the MCGRs correct the curvature by initial spinal distraction; then, they maintain the resulting deformity correction by controlling both spinal curvature and spinal growth and promoting growth with further non-invasive instrumentation distractions. The non-invasive possibility of lengthening MCGRs reduces the risk of complications and significantly reduces the number of hospital stays, the amount of subsequent anesthesia (up to invasive spinal distraction), as well as the related mental and social feelings of children and parents [19,20,21].
The MCGR system might seem ideal, but it cannot be used for every patient with EOS, and the treatment with this system is limited. Not every patient can be implanted with this type of rod, due to their size and the limited possibilities of intraoperative bending. More precisely, they do not fit all curvatures and patients. There are also some risks of complications. Several studies have reported certain drawbacks and complications in the treatment course, such as deep wound infection, proximal junctional kyphosis (PJK), rod fracture, the failure of the rods to distract, and the auto-fusion of the spine before the end of treatment [20,22,23]. According to the data available in the literature, implant failure is most often associated with magnetic rod fracture or the loss of ability to continue distraction. In patients treated with the MCGR system in the medium and long-term observation period, the overall number of complications was found to be about 73%, but this is also related to the results of the treatment of congenital, neuromuscular, or syndromic scoliosis using this system. Furthermore, as we know, scoliosis with an etiology other than idiopathic has an increased risk of complications overall [9,11,22,23,24,25]. Other studies have also reported several unique complications, including rod slippage, mismatches between the target and achieved distraction length, metallosis, and actuator pin fracture. In comparison to other surgical techniques for EOS treatment, MCGRs can be inserted as a less-invasive surgical technique with a mini-open approach [26,27,28]. In order to limit the high risk of spontaneous spinal fusion in a growing spine [29,30,31] during surgery procedures with a wide approach to the spine, MCGRs should be placed subfascially. Metallosis resulting from the use of MCGRs appears to be of significant clinical importance (Figure 9). Although there are no studies confirming the toxic effects of this metallosis on soft tissues and the body, MCGR instruments should be removed at the end of the growth-promoting procedure, and final spine instrumentation should be made [27,29]. The use of MCGRs is still a safe and effective surgical technique in patients undergoing primary EOS surgery [5,6,7,10,17,18,22,23,32,33,34,35,36].
4. Conclusions
MCGR is a safe surgical technique in patients undergoing primary EOS surgery and is currently widely used. The MCGR system can be used as a less-invasive procedure that allows for the avoidance of many periodic invasive procedures for children, reducing the number of elective hospitalizations and anesthesia to a minimum and lessening the physical and mental burden of young patients, parents, and their families. Moreover, lengthening on an outpatient basis represents an advancement in the treatment of EOS.
Author Contributions
Conceptualization, P.G. and I.J.H.; methodology, I.J.H. and P.G.; software, M.G.; validation, K.C. and I.J.H.; formal analysis, P.G. and M.G.; investigation, P.G.; resources, P.G.; data curation, P.G. and I.J.H.; writing—original draft preparation, P.G. and K.C.; writing—review and editing, I.J.H. and M.G.; visualization, P.G. and K.C.; supervision, I.J.H.; project administration, P.G.; funding acquisition, P.G. All authors have read and agreed to the published version of the manuscript.
Funding
The APC was funded by P.G.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Patient consent for publication was waived due to us not reporting details that might identify our patient.
Data Availability Statement
Not applicable.
Acknowledgments
We are immensely grateful to our patient and her parents for their consent to publish this case study and their cooperation in the diagnostic and treatment processes.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Helenius, I.J. Standard and magnetically controlled growing rods for the treatment of early onset scoliosis. Ann. Transl. Med. 2020, 8, 26. [Google Scholar] [CrossRef] [PubMed]
- Helenius, I.J. Treatment strategies for early-onset scoliosis. EFORT Open Rev. 2018, 3, 287–293. [Google Scholar] [CrossRef] [PubMed]
- Tsirikos, A.I.; Roberts, S.B. Magnetic controlled growth rods in the treatment of scoliosis: Safety, efficacy and patient selection. Med. Devices 2020, 13, 75–85. [Google Scholar] [CrossRef] [PubMed]
- Bess, S.; Akbarnia, B.A.; Thompson, G.H.; Sponseller, P.D.; Shah, S.A.; El Sebaie, H.; Boachie-Adjei, O.; Karlin, L.I.; Canale, S.; Poe-Kochert, C.; et al. Complications of growing-rod treatment for early-onset scoliosis: Analysis of one hundred and forty patients. J. Bone Jt. Surg. Am. 2010, 92, 2533–2543. [Google Scholar] [CrossRef] [PubMed]
- Cheung, J.P.Y.; Yiu, K.; Kwan, K.; Cheung, K.M.C. Mean 6-year follow-up of magnetically controlled growing rod patients with early onset scoliosis: A glimpse of what happens to graduates. Neurosurgery 2019, 84, 1112–1123. [Google Scholar] [CrossRef]
- Flynn, J.M.; Tomlinson, L.A.; Pawelek, J.; Thompson, G.H.; McCarthy, R.; Akbarnia, B.A.; Growing Spine Study Group. Growing-rod graduates: Lessons learned from ninety-nine patients who completed lengthening. J. Bone Jt. Surg. Am. 2013, 95, 1745–1750. [Google Scholar] [CrossRef]
- Figueiredo, N.; Kananeh, S.F.; Siqueira, H.H.; Figueiredo, R.C.; Al Sebai, M.W. The use of magnetically controlled growing rod device for pediatric scoliosis. Neurosciences 2016, 21, 17–25. [Google Scholar] [CrossRef]
- Meyer, C.S.; Rickers, K.; Eiskjær, S.P. Magnetically controlled growing rods in early-onset scoliosis. Dan. Med. J. 2021, 69, A08210627. [Google Scholar]
- Cheung, J.P.Y.; Sze, K.Y.; Cheung, K.M.C.; Zhang, T. The first magnetically controlled growing rod (MCGR) in the world—Lessons learned and how the identified complications helped to develop the implant in the past decade: Case report. BMC Musculoskelet. Disord. 2021, 22, 319. [Google Scholar] [CrossRef]
- Dahl, B.; Dragsted, C.; Ohrt-Nissen, S.; Andersen, T.; Gehrchen, M. Use of a distraction-to-stall lengthening procedure in magnetically controlled growing rods: A single-center cohort study. J. Orthop. Surg. 2018, 26, 2309499018779833. [Google Scholar] [CrossRef]
- Cheung, J.P.Y.; Cheung, K.M. Current status of the magnetically controlled growing rod in treatment of early-onset scoliosis: What we know after a decade of experience. J. Orthop. Surg. 2019, 27, 2309499019886945. [Google Scholar] [CrossRef]
- Fletcher, N.D.; McClung, A.; Rathjen, K.E.; Denning, J.R.; Browne, R.; Johnston, C.E., 3rd. Serial casting as a delay tactic in the treatment of moderate-to-severe early-onset scoliosis. J. Pediatr. Orthop. 2012, 32, 664–671. [Google Scholar] [CrossRef]
- Yang, S.; Andras, L.M.; Redding, G.J.; Skaggs, D.L. Early-onset scoliosis: A review of history, current treatment, and future directions. Pediatrics 2016, 137, e20150709. [Google Scholar] [CrossRef]
- Thorsness, R.J.; Faust, J.R.; Behrend, C.J.; Sanders, J.O. Nonsurgical management of early-onset scoliosis. J. Am. Acad. Orthop. Surg. 2015, 23, 519–528. [Google Scholar] [CrossRef]
- Karol, L.A. The natural history of early-onset scoliosis. J. Pediatr. Orthop. 2019, 39 (Suppl. S1), S38–S43. [Google Scholar] [CrossRef]
- Hardesty, C.K.; Huang, R.P.; El-Hawary, R.; Samdani, A.; Hermida, P.B.; Bas, T.; Balioğlu, M.B.; Gurd, D.; Pawelek, J.; McCarthy, R.; et al. Early-onset scoliosis: Updated treatment techniques and results. Spine Deform. 2018, 6, 467–472. [Google Scholar] [CrossRef] [PubMed]
- Abdelaal, A.; Munigangaiah, S.; Trivedi, J.; Davidson, N. Magnetically controlled growing rods in the treatment of early onset scoliosis: A single centre experience of 44 patients with mean follow-up of 4.1 years. Bone Jt. Open. 2020, 1, 405–414. [Google Scholar] [CrossRef]
- Welborn, M.C.; Bouton, D. Outcomes of MCGR at >3 year average follow-up in severe scoliosis: Who undergoes elective revision vs. UPROR? Spine Deform. 2022, 10, 457–463. [Google Scholar] [CrossRef]
- Cheung, P.W.H.; Wong, C.K.H.; Sadiang-Abay, J.T.; Lau, S.T.; Cheung, J.P.Y. Longitudinal comparison of direct medical cost, radiological and health-related quality of life treatment outcomes between traditional growing rods and magnetically controlled growing rods from preoperative to maturity. BMC Musculoskelet. Disord. 2022, 23, 791. [Google Scholar] [CrossRef]
- Doany, M.E.; Olgun, Z.D.; Kinikli, G.I.; Bekmez, S.; Kocyigit, A.; Demirkiran, G.; Karaagaoglu, A.E.; Yazici, M. Health-related quality of life in early-onset scoliosis patients treated surgically: EOSQ scores in traditional growing rod versus magnetically controlled growing rods. Spine 2018, 43, 148–153. [Google Scholar] [CrossRef]
- Tahir, M.; Mehta, D.; Sandhu, C.; Jones, M.; Gardner, A.; Mehta, J.S. A comparison of the post-fusion outcome of patients with early-onset scoliosis treated with traditional and magnetically controlled growing rods. Bone Jt. J. 2022, 104, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Sun, M.M.; Buckler, N.J.; Al Nouri, M.; Howard, J.J.; Vaughan, M.; St Hilaire, T.; Sponseller, P.D.; Smith, J.T.; Thompson, G.H.; El-Hawary, R.; et al. No difference in the rates of unplanned return to the operating room between magnetically controlled growing rods and traditional growth friendly surgery for children with cerebral palsy. J. Pediatr. Orthop. 2022, 42, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.; Yaszay, B.; Mundis, G.; Hosseini, P.; Pawelek, J.; Alanay, A.; Berk, H.; Cheung, K.; Demirkiran, G.; Ferguson, J.; et al. Implant complications after magnetically controlled growing rods for early onset scoliosis: A multicenter retrospective review. J. Pediatr. Orthop. 2017, 37, e588–e592. [Google Scholar] [CrossRef] [PubMed]
- Bekmez, S.; Afandiyev, A.; Dede, O.; Karaismailoğlu, E.; Demirkiran, H.G.; Yazici, M. Is magnetically controlled growing rod the game changer in early-onset scoliosis? A preliminary report. J. Pediatr. Orthop. 2019, 39, e195–e200. [Google Scholar] [CrossRef] [PubMed]
- Ilharreborde, B.; Ponchelet, L.; Sales de Gauzy, J.; Choufani, E.; Baudoux, M.; Pesenti, S.; Simon, A.L. How does magnetically controlled growing rods insertion affect sagittal alignment in ambulatory early onset scoliosis patients? Eur. Spine J. 2022, 31, 1036–1044. [Google Scholar] [CrossRef]
- Kılıçaslan, Ö.F.; Tokgöz, M.A.; Bütün, Ş.; Nabi, V.; Akalın, S. Management and results of early-onset scoliosis with dual magnetically controlled growing rods: Additional preliminary results of spinal fusion surgery. Jt. Dis. Relat. Surg. 2021, 32, 478–488. [Google Scholar] [CrossRef]
- Zhang, T.; Sze, K.Y.; Peng, Z.W.; Cheung, K.M.C.; Lui, Y.F.; Wong, Y.W.; Kwan, K.Y.H.; Cheung, J.P.Y. Systematic investigation of metallosis associated with magnetically controlled growing rod implantation for early-onset scoliosis. Bone Jt. J. 2020, 102, 1375–1383. [Google Scholar] [CrossRef]
- Borde, M.D.; Sapare, S.; Schutgens, E.; Ali, C.; Noordeen, H. Analysis of serum levels of titanium and aluminium ions in patients with early onset scoliosis operated upon using the magnetic growing rod-a single centre study of 14 patients. Spine Deform. 2021, 9, 1473–1478. [Google Scholar] [CrossRef]
- Green, A.H.; Brzezinski, A.; Ishmael, T.; Adolfsen, S.; Bowe, J.A. Premature spinal fusion after insertion of magnetically controlled growing rods for treatment of early-onset scoliosis: Illustrative case. J. Neurosurg. Case Lessons 2021, 2, CASE21446. [Google Scholar] [CrossRef]
- Akbarnia, B.A.; Emans, J.B. Complications of growth-sparing surgery in early onset scoliosis. Spine 2010, 35, 2193–2204. [Google Scholar] [CrossRef]
- Mundis, G.M.; Kabirian, N.; Akbarnia, B.A. Dual growing rods for the treatment of early-onset scoliosis. JBJS Essent. Surg. Tech. 2013, 3, e6. [Google Scholar] [CrossRef]
- Matsumoto, H.; Sinha, R.; Roye, B.D.; Ball, J.R.; Skaggs, K.F.; Brooks, J.T.; Welborn, M.C.; Emans, J.B.; Anari, J.B.; Johnston, C.E.; et al. Contraindications to magnetically controlled growing rods: Consensus among experts in treating early onset scoliosis. Spine Deform. 2022, 10, 1289–1297. [Google Scholar] [CrossRef]
- Calderaro, C.; Labianca, L.; Dolan, L.A.; Yamashita, K.; Weinstein, S.L. Early-onset scoliosis treated with magnetically controlled growing rods. Orthopedics 2020, 43, e601–e608. [Google Scholar] [CrossRef]
- Li, X.; Li, Z.; Lin, Y.; Tan, H.; Chen, C.; Shen, J. Growing-rod implantation improves nutrition status of early-onset scoliosis patients: A case series study of minimum 3-year follow-up. BMC Surg. 2021, 21, 106. [Google Scholar] [CrossRef]
- Welborn, M.C.; Krajbich, J.I.; D’Amato, C. Use of magnetic spinal growth rods (mcgr) with and without preoperative halo-gravity traction (HGT) for the treatment of severe early-onset scoliosis (EOS). J. Pediatr. Orthop. 2019, 39, e293–e297. [Google Scholar] [CrossRef]
- Heyer, J.H.; Anari, J.B.; Baldwin, K.D.; Mitchell, S.L.; Luhmann, S.J.; Sturm, P.F.; Flynn, J.M.; Cahill, P.J.; Pediatric Spine Study Group. Lengthening behavior of magnetically controlled growing rods in early-onset scoliosis: A multicenter study. J. Bone Jt. Surg. Am. 2022. ahead of print. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).