Analysis of Cause-of-Death Mortality in Children and Young Adults with Diabetes: A Nationwide 10-Year Follow-Up Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Database and Type of Study
2.2. Diabetes Mellitus (DM) Group
2.3. Control (Non-DM) Group
2.4. Check Points
2.5. Statistical Analysis
2.6. Ethics Approval and Consent to Participate
3. Results
3.1. Comparison of Baseline Clinical Characteristics
3.2. Mortality and HR for Death with Diabetes
3.3. The Number of Patients and Deaths According to the Follow-Up Date
3.4. Hazard Ratios for Death during the 12 yr Study Period
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, D.C.; Gallagher, M.P.; Gopalan, A.; Osorio, M.; Vinson, A.J.; Wall, S.P.; Ravenell, J.E.; Sevick, M.A.; Elbel, B. Identifying geographic disparities in diabetes prevalence among adults and children using emergency claims Data. J. Endocr. Soc. 2018, 2, 460–470. [Google Scholar] [CrossRef] [PubMed]
- Saydah, S.; Imperatore, G.; Cheng, Y.; Geiss, L.S.; Albright, A. Disparities in diabetes deaths among children and adolescents—United States. 2000–2014. MMWR. Morb. Mortal. Wkly. Rep. 2017, 66, 502–505. [Google Scholar] [CrossRef] [PubMed]
- Ogunwole, S.M.; Sherita, H. Social Ddeterminants of health and structural inequities—Root causes of diabetes disparities Golden. Diabetes Care 2021, 44, 11–13. [Google Scholar] [CrossRef]
- Shin, H.; Kim, J.; Lee, S.; Park, M.S.; Park, S.; Huh, S. Cause-of-death statistics in 2018 in the Republic of Korea. J. Korean Med Assoc. 2020, 63, 286–297. [Google Scholar] [CrossRef]
- Han, E.; Song, S.O.; Kim, H.S.; Son, K.J.; Ha Jee, S.; Cha, B.-S.; Lee, B.-W.; Cha, B.; Lee, B. Improvement in age at mortality and changes in causes of death in the population with diabetes: An analysis of data from the Korean national health insurance and statistical information service, 2006 to 2018. Endocrinol. Metab. 2022, 37, 466–474. [Google Scholar] [CrossRef]
- Gregg, E.W.; Li, Y.; Wang, J.; Burrows, N.R.; Ali, M.K.; Rolka, D.; Williams, D.E.; Geiss, L. Changes in diabetes-related complications in the United States, 1990–2010. N. Engl. J. Med. 2014, 370, 1514–1523. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.H. Diabetes mellitus, still major threat to mortality from various causes. Diabetes Metab. J. 2019, 43, 273–275. [Google Scholar] [CrossRef] [PubMed]
- Rosengren, A.; Dikaiou, P. Cardiovascular outcomes in type 1 and type 2 diabetes. Diabetologia 2023, 66, 425–437. [Google Scholar] [CrossRef]
- You, Y.S.; Kim, J.S.; Jeong, J.S.; Yeom, S.W.; Kim, D.H.; Kwon, S.H.; Lee, Y.C. Septal deviation could be associated with the development of bronchial asthma: A nationwide cohort study. J. Allergy Clin. Immunol. Pract. 2022, 10, 1099–1101.e1. [Google Scholar] [CrossRef] [PubMed]
- Jeong, J.S.; Choi, J.Y.; Kim, J.S.; Park, S.O.; Kim, W.; Yoon, Y.G.; Park, H.J.; Park, K.H.; Kim, D.H.; Kim, J.M.; et al. SARS-CoV-2 infection in severe asthma is associated with worsening of COVID-19 through respiratory NLRP3 inflammasome activation. Allergy 2023, 78, 287–290. [Google Scholar] [CrossRef]
- Kim, J.S.; Lee, I.J.; Lee, M.G.; Yeom, S.W.; Nam, K.H.; Yun, S.K.; Park, J. Periodontitis and risk of alopecia areata: A nationwide population-based cohort study in Korea. J. Eur. Acad. Dermatol. Venereol 2022. online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.G.; Kang, M.G.; Lee, M.G.; Yang, S.J.; Yeom, S.W.; Lee, J.H.; Choi, S.M.; Yoon, J.H.; Lee, E.J.; Noh, S.J.; et al. Periodontitis is associated with the development of fungal sinusitis: A nationwide 12-year follow-up study. J. Clin. Periodontol. 2022. online ahead of print. [Google Scholar] [CrossRef]
- Hwang, J.H.; You, Y.S.; Yeom, S.W.; Lee, M.G.; Lee, J.H.; Kim, M.G.; Kim, J.S. Influenza viral infection is a risk factor for severe illness in COVID-19 patients: A nationwide population-based cohort study. Emerg. Microbes Infect. 2022, 29, 1–32. [Google Scholar] [CrossRef]
- Youth Population and Composition Ratio. Available online: http://www.index.go.kr/potal/main/EachDtlPageDetail.do?idx_cd=1597 (accessed on 1 August 2022).
- Tohi, M.; Bay, J.L.; Tu’akoi, S.; Vickers, M.H. The Developmental Origins of Health and Disease: Adolescence as a Critical Lifecourse Period to Break the Transgenerational Cycle of NCDs—A Narrative Review. Int. J. Environ. Res. Public Health 2022, 19, 6024. [Google Scholar] [CrossRef] [PubMed]
- Muggeo, M.; Verlato, G.; Bonora, E.; Bressan, F.; Girotto, S.; Corbellini, M.; Gemma, M.L.; Moghetti, P.; Zenere, M.; Cacciatori, V.; et al. The Verona diabetes study: A population-based survey on known diabetes mellitus prevalence and 5-year all-cause mortality. Diabetologia 1995, 38, 318–325. [Google Scholar] [CrossRef] [PubMed]
- Reunanen, A. Mortality in type 2 diabetes. Ann. Clin. Res. 1983, 15, 26–28. [Google Scholar] [PubMed]
- Roper, N.A.; Bilous, R.W.; Kelly, W.F.; Unwin, N.C.; Connolly, V.M. Excess mortality in a population with diabetes compared to local and national controls, and the impact of material deprivation: Longitudinal population based study. BMJ 2001, 322, 1389–1393. [Google Scholar] [CrossRef]
- Vilbergsson, S.; Sigurdsson, G.; Sigvaldason, H.; Sigfusson, N. Coronary heart disease mortality amongst non-insulin-dependent diabetic subjects in Iceland: The independent effect of diabetes: The Reykjavik Study 17-year follow up. J. Intern. Med. 1998, 244, 309–316. [Google Scholar] [CrossRef] [PubMed]
- de Marco, R.; Locatelli, F.; Zoppini, G.; Verlato, G.; Bonora, E.; Muggeo, M. Cause-specific mortality in type 2 diabetes: The Verona Diabetes Study. Diabetes Care 1999, 22, 756–761. [Google Scholar] [CrossRef]
- Raymond, N.T.; Langley, J.D.; Goyder, E.; Botha, J.L.; Burden, A.C.; Hearnshaw, J.R. Insulin treated diabetes mellitus: Causes of death determined from record linkage of population based registers in Leicestershire, UK. J. Epidemiol. Community Health 1995, 49, 570–574. [Google Scholar] [CrossRef] [PubMed]
- Moss, S.E.; Klein, R.; Klein, B.E. Cause-specific mortality in a population-based study of diabetes. Am. J. Public Health 1991, 81, 1158–1162. [Google Scholar] [CrossRef]
- Gu, K.; Cowie, C.C.; Harris, M.I. Mortality in adults with and without diabetes in a national cohort of the U.S. Population 1971–1993. Diabetes Care 1998, 21, 1138–1145. [Google Scholar] [CrossRef] [PubMed]
- Gu, K.; Cowie, C.C.; Harris, M.I. Diabetes and decline in heart disease mortality in US adults. JAMA 1999, 281, 1291–1297. [Google Scholar] [CrossRef]
- Roper, N.A.; Bilous, R.W.; Kelly, W.F.; Unwin, N.C.; Connolly, V.M.; South Tees Diabetes Mortality Study. Cause-specific mortality in a population with diabetes: South Tees Diabetes Mortality Study. Diabetes Care 2002, 25, 43–48. [Google Scholar] [CrossRef]
- Svane, J.; Lynge, T.H.; Pedersen-Bjergaard, U.; Jespersen, T.; Gislason, G.H.; Risgaard, B.; Winkel, B.G.; Tfelt-Hansen, J. Cause-specific mortality in children and young adults with diabetes mellitus: A Danish nationwide cohort study. Eur. J. Prev. Cardiol. 2021, 28, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Rawshani, A.; Sattar, N.; Franze´n, S.; Rawshani, A.; Hattersley, A.T.; Svensson, A.; Eliasson, B.; Gudbjörnsdottir, S. Excess mortality and cardiovascular disease. in young adults with type 1 diabetes in relation to age at onset: A nationwide, register-based cohort study. Lancet 2018, 392, 477–486. [Google Scholar] [CrossRef]
- Diabetes in Children. Available online: https://www.healthychildren.org/English/health-issues/conditions/chronic/Pages/Diabetes.aspx (accessed on 1 February 2022).
- Libman, I.; Haynes, A.; Lyons, S.; Pradeep, P.; Rwagasor, E.; Tung, J.Y.; Jefferies, C.A.; Oram, R.A.; Dabelea, D.; Craig, M.E. ISPAD Clinical Practice Consensus Guidelines 2022: Definition, epidemiology, and classification of diabetes in children and adolescents. Pediatr Diabetes 2022, 23, 1160–1174. [Google Scholar] [CrossRef]
- Patterson, C.C.; Dahlquist, G.; Harjutsalo, V.; Joner, G.; Feltbower, R.G.; Svensson, J.; Schober, E.; Gyürüs, E.; Castell, C.; Urbonaité, B.; et al. Early mortality in EURODIAB population-based cohorts of type 1 diabetes diagnosed in childhood since 1989. Diabetologia 2007, 50, 2439–2442. [Google Scholar] [CrossRef] [PubMed]
- Statistics About Diabetes. Available online: https://diabetes.org/about-us/statistics/about-diabetes (accessed on 14 November 2022).
- Saydah, S.; Lochner, K. Socioeconomic status and risk of diabetes-related mortality in the U.S. Public Health Rep. 2010, 125, 377–388. [Google Scholar] [CrossRef]
- Scott, A.; Chambers, D.; Goyder, E.; O’Cathain, A. Socioeconomic inequalities in mortality, morbidity and diabetes management for adults with type 1 diabetes: A systematic review. PLoS ONE 2017, 12, e0177210. [Google Scholar] [CrossRef] [PubMed]
- Chuang, W.C.; Chu, C.H.; Hsu, Y.H.; Yao, C. Effect of socioeconomic status on survival in patients on the Diabetes Shared Care Program: Finding from a Taiwan nationwide cohort. J. Chin. Med Assoc. 2022, 85, 311–316. [Google Scholar] [CrossRef] [PubMed]
- Zara, S.; Kruse, J.; Leveling, A.M.; Schmitz, J.; Hempler, I.; Kampling, H. Capturing Diabetes-Related Distress and Burden From the Perspective of Patients With Type 1 or Type 2 Diabetes: Protocol for an Explorative Mixed Methods Study. JMIR Res. Protoc. 2022, 11, e38477. [Google Scholar] [CrossRef] [PubMed]
- Wenter, A.; Schickl, M.; Sevecke, K.; Juen, B.; Exenberger, S. Children’s mental health during the first two years of the COVID-19 pandemic: Burden, Risk Factors and Posttraumatic Growth–A Mixed-Methods Parents’ Perspective. Front. Psychol. 2022, 13, 901205. [Google Scholar] [CrossRef]
- Laing, S.P.; Jones, M.E.; Swerdlow, A.J.; Burden, A.C.; Gatling, W. Psychosocial and Socioeconomic Risk Factors for Premature Death in Young People With Type 1 Diabetes. Diabetes Care 2005, 28, 1618–1623. [Google Scholar] [CrossRef] [PubMed]
- Grey, M.; Boland, E.; Yu, C.; Sullivan-Bolyai, S.; Tamborlane, W.V. Personal and family factors associated with quality of life in adolescents with diabetes. Diabetes Care 1998, 21, 909–913. [Google Scholar] [CrossRef] [PubMed]


| Variables | Before Matched | After Matched | ||||
|---|---|---|---|---|---|---|
| Non-DM Group (n = 374,601) | DM Group (n = 10,006) | SMD | Non-DM Group (n = 10,006) | DM Group (n = 10,006) | SMD | |
| Sex | 0.039 | 0.003 | ||||
| Male | 194,754 | 5007 | 4992 | 5007 | ||
| Female | 179,847 | 4999 | 5014 | 4999 | ||
| Age | 0.447 | 0.006 | ||||
| <25 | 296,655 | 5909 | 5877 | 5909 | ||
| ≥25 | 77,946 | 4097 | 4129 | 4097 | ||
| Residential area | 0.088 | 0.003 | ||||
| Rural | 199,135 | 5077 | 5075 | 5077 | ||
| Metro | 100,060 | 2552 | 2541 | 2552 | ||
| Urban | 75,406 | 2377 | 2390 | 2377 | ||
| Economic status | 0.077 | 0.004 | ||||
| ≧50 (high) | 184,614 | 4545 | 4567 | 4545 | ||
| <50 (low) | 189,987 | 5461 | 5439 | 5461 | ||
| Allergic rhinnitis | 0.009 | 0.001 | ||||
| No | 287,502 | 7716 | 7719 | 7716 | ||
| Yes | 87,099 | 2290 | 2287 | 2290 | ||
| Asthma | 0.152 | 0.021 | ||||
| No | 325,550 | 9166 | 9223 | 9166 | ||
| Yes | 49,051 | 840 | 783 | 840 | ||
| Atopy | 0.135 | 0.013 | ||||
| No | 336,683 | 9365 | 9397 | 9365 | ||
| Yes | 37,918 | 641 | 609 | 641 | ||
| Cardiac illness | 0.345 | 0.007 | ||||
| No | 361,965 | 8746 | 8770 | 8746 | ||
| Yes | 12,636 | 1260 | 1236 | 1260 | ||
| Mental illness | 0.302 | 0.003 | ||||
| No | 354,919 | 8597 | 8607 | 8597 | ||
| Yes | 19,682 | 1409 | 1399 | 1409 | ||
| Death | 0.116 | 0.101 | ||||
| No | 374,133 | 9907 | 9985 | 9907 | ||
| Yes | 468 | 99 | 21 | 99 | ||
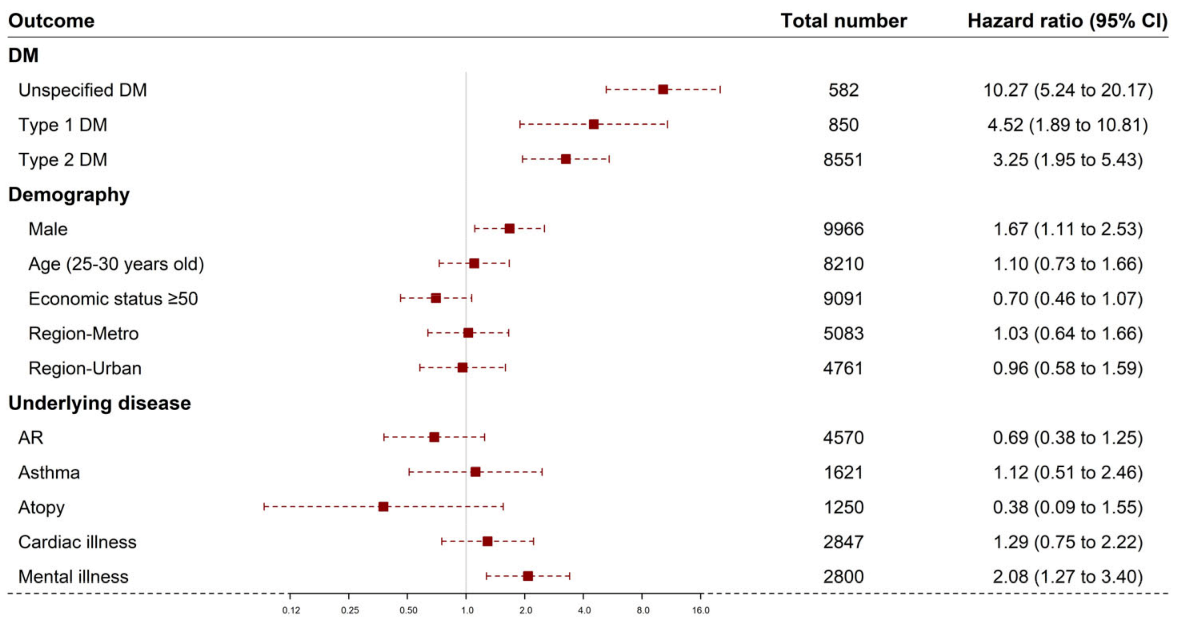
| Group | Total | Number of Mortality Cases (%) | Hazard Ratio (95% Confidence Interval, Lower–Upper) |
|---|---|---|---|
| Control | 9983 | 20 (0.2) | 1 |
| Type 1 DM | 850 | 7 (0.82) | 4.52 (1.89–10.82) |
| Type 2 DM | 8551 | 55 (0.64) | 3.25 (1.95–5.43) |
| Unspecified DM | 582 | 15 (2.58) | 10.20 (5.24–20.18) |
| Sex | |||
| Female | 10,000 | 37 (0.37) | 1 |
| Male | 9966 | 60 (0.6) | 1.67 (1.11–2.53) |
| Age | |||
| < 25 | 11,756 | 52 (0.44) | 1 |
| ≧ 25 | 8210 | 45 (0.55) | 1.10 (0.73–1.67) |
| Residential Area | |||
| Rural | 10,122 | 49 (0.48) | 1 |
| Urban | 4761 | 22 (0.46) | 0.96 (0.58–1.59) |
| Metropolitan | 5083 | 26 (0.51) | 1.02 (0.64–1.66) |
| Economic Status | |||
| <50 (low) | 10,875 | 61 (0.56) | 1 |
| ≧50 (high) | 9091 | 36 (0.4) | 0.70 (0.46–1.07) |
| Underlying disease | |||
| Allergic rhinnitis | |||
| No | 15,396 | 84 (0.55) | 1 |
| Yes | 4570 | 13 (0.28) | 0.68 (0.38–1.25) |
| Asthma | |||
| No | 18,345 | 90 (0.49) | 1 |
| Yes | 1621 | 7 (0.43) | 1.11(0.51–2.45) |
| Atopy | |||
| No | 18,716 | 95 (0.51) | 1 |
| Yes | 1250 | 2 (0.16) | 0.37(0.09–1.55) |
| Cardiac diseases | |||
| No | 17,479 | 81 (0.46) | 1 |
| Yes | 2487 | 16 (0.64) | 1.29(0.75–2.22) |
| Mental Disorder | |||
| No | 17,166 | 76 (0.44) | 1 |
| Yes | 2800 | 21 (0.75) | 2.08 (1.27–3.40) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, I.-H.; Yeom, S.-W.; Kim, S.-Y.; You, J.; Kim, J.-S.; Kim, M. Analysis of Cause-of-Death Mortality in Children and Young Adults with Diabetes: A Nationwide 10-Year Follow-Up Cohort Study. Children 2023, 10, 358. https://doi.org/10.3390/children10020358
Choi I-H, Yeom S-W, Kim S-Y, You J, Kim J-S, Kim M. Analysis of Cause-of-Death Mortality in Children and Young Adults with Diabetes: A Nationwide 10-Year Follow-Up Cohort Study. Children. 2023; 10(2):358. https://doi.org/10.3390/children10020358
Chicago/Turabian StyleChoi, Iee-Ho, Sang-Woo Yeom, Sun-Young Kim, Jihye You, Jong-Seung Kim, and Minsun Kim. 2023. "Analysis of Cause-of-Death Mortality in Children and Young Adults with Diabetes: A Nationwide 10-Year Follow-Up Cohort Study" Children 10, no. 2: 358. https://doi.org/10.3390/children10020358
APA StyleChoi, I.-H., Yeom, S.-W., Kim, S.-Y., You, J., Kim, J.-S., & Kim, M. (2023). Analysis of Cause-of-Death Mortality in Children and Young Adults with Diabetes: A Nationwide 10-Year Follow-Up Cohort Study. Children, 10(2), 358. https://doi.org/10.3390/children10020358






