The Variable Influence of Orthotic Management on Hip and Pelvic Rotation in Children with Unilateral Neurogenic Equinus Deformity
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measurements
2.3. Data Analysis
2.4. Statistical Analysis
2.5. Sample Size
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aiona, M.D.; Sussman, M.D. Treatment of spastic diplegia in patients with cerebral palsy: Part II. J. Pediatr. Orthop. B 2004, 13, S13–S38. [Google Scholar]
- Wren, T.A.; Rethlefsen, S.; Kay, R.M. Prevalence of specific gait abnormalities in children with cerebral palsy: Influence of cerebral palsy subtype, age, and previous surgery. J. Pediatr. Orthop. 2005, 25, 79–83. [Google Scholar]
- Gage, J. The Treatment of Gait Problems in Cerebral Palsy. Section 3: Gait Pathology in Cerebral Palsy; Mac Keith: London, UK, 2004; ISBN 1898683379. [Google Scholar]
- Carty, C.P.; Walsh, H.P.; Gillett, J.G.; Phillips, T.; Edwards, J.M.; Delacy, M.; Boyd, R.N. The effect of femoral derotation osteotomy on transverse plane hip and pelvic kinematics in children with cerebral palsy: A systematic review and meta-analysis. Gait Posture 2014, 40, 333–340. [Google Scholar] [CrossRef]
- Brunner, R.; Baumann, J.U. Long-term effects of intertrochanteric varus-derotation osteotomy on femur and acetabulum in spastic cerebral palsy: An 11- to 18-year follow-up study. J. Pediatr. Orthop. 1997, 17, 585–591. [Google Scholar] [CrossRef]
- Kim, H.; Aiona, M.; Sussman, M. Recurrence After Femoral Derotational Osteotomy in Cerebral Palsy. J. Pediatr. Orthop. 2005, 25, 739–743. [Google Scholar] [CrossRef]
- Arnold, A.S.; Delp, S.L. Rotational moment arms of the medial hamstrings and adductors vary with femoral geometry and limb position: Implications for the treatment of internally rotated gait. J. Biomech. 2001, 34, 437–447. [Google Scholar] [CrossRef]
- Arnold, A.S.; Komallu, A.V.; Delp, S.L. Internal rotation gait: A compensatory mechanism to restore abduction capacity decreased by bone deformity? Dev. Med. Child Neurol. 1997, 39, 40–44. [Google Scholar] [CrossRef]
- Delp, S.L.; Hess, W.E.; Hungerford, D.S.; Jones, L.C. Variation of rotation moment arms with hip flexion. J. Biomech. 1999, 32, 493–501. [Google Scholar] [CrossRef] [PubMed]
- Brunner, R.; Dreher, T.; Romkes, J.; Frigo, C. Effects of plantarflexion on pelvis and lower limb kinematics. Gait Posture 2008, 28, 150–156. [Google Scholar] [CrossRef]
- Pasin Neto, H.; Grecco, L.A.C.; Ferreira, L.A.B.; Duarte, N.A.C.; Galli, M.; Oliveira, C.S. Postural insoles on gait in children with cerebral palsy: Randomized controlled double-blind clinical trial. J. Bodyw. Mov. Ther. 2017, 21, 890–895. [Google Scholar] [CrossRef]
- Romkes, J.; Brunner, R. Comparison of a dynamic and a hinged ankle–foot orthosis by gait analysis in patients with hemiplegic cerebral palsy. Gait Posture 2002, 15, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Altschuck, N.; Bauer, C.; Nehring, I.; Böhm, H.; Jakobeit, M.; Schröder, A.S.; Mall, V.; Jung, N.H. Efficacy of prefabricated carbon-composite ankle foot orthoses for children with unilateral spastic cerebral palsy exhibiting a drop foot pattern. J. Pediatr. Rehabil. Med. 2019, 12, 171–180. [Google Scholar] [CrossRef] [PubMed]
- Boudarham, J.; Pradon, D.; Roche, N.; Bensmail, D.; Zory, R. Effects of a dynamic-ankle-foot orthosis (Liberté®) on kinematics and electromyographic activity during gait in hemiplegic patients with spastic foot equinus. Neurorehabilitation 2014, 35, 369–379. [Google Scholar] [CrossRef] [PubMed]
- Desloovere, K.; Molenaers, G.; Van Gestel, L.; Huenaerts, C.; Van Campenhout, A.; Callewaert, B.; Van de Walle, P.; Seyler, J. How can push-off be preserved during use of an ankle foot orthosis in children with hemiplegia? A prospective controlled study. Gait Posture 2006, 24, 142–151. [Google Scholar] [CrossRef]
- Balaban, B.; Yasar, E.; Dal, U.; Yazicioglu, K.; Mohur, H.; Kalyon, T.A. The effect of hinged ankle-foot orthosis on gait and energy expenditure in spastic hemiplegic cerebral palsy. Disabil. Rehabil. 2007, 29, 139–144. [Google Scholar] [CrossRef]
- Lintanf, M.; Bourseul, J.-S.; Houx, L.; Lempereur, M.; Brochard, S.; Pons, C. Effect of ankle-foot orthoses on gait, balance and gross motor function in children with cerebral palsy: A systematic review and meta-analysis. Clin. Rehabil. 2018, 32, 1175–1188. [Google Scholar] [CrossRef]
- Butler, P.B.; Farmer, S.E.; Stewart, C.; Jones, P.W.; Forward, M. The effect of fixed ankle foot orthoses in children with cerebral palsy. Disabil. Rehabil. Assist. Technol. 2007, 2, 51–58. [Google Scholar] [CrossRef]
- Aboutorabi, A.; Arazpour, M.; Bani, M.A.; Saeedi, H.; Head, J.S. Efficacy of ankle foot orthoses types on walking in children with cerebral palsy: A systematic review. Ann. Phys. Rehabil. Med. 2017, 60, 393–402. [Google Scholar] [CrossRef]
- Novacheck, T.F.; Gage, J.R. Orthopedic management of spasticity in cerebral palsy. Child’s Nerv. Syst. 2007, 23, 1015–1031. [Google Scholar] [CrossRef]
- Sapienza, M.; Kapoor, R.; Alberghina, F.; Maheshwari, R.; McCracken, K.L.; Canavese, F.; Johari, A.N. Adverse Effects Following Botulinum Toxin A Injections in Children with Cerebral Palsy. Journal of Pediatric Orthopaedics B. 2023. Available online: https://journals.lww.com/jpo-b/Abstract/9900/Adverse_effects_following_botulinum_toxin_A.85.aspx (accessed on 1 February 2023).
- Hong, Z.; Sui, M.; Zhuang, Z.; Liu, H.; Zheng, X.; Cai, C.; Jin, D. Effectiveness of Neuromuscular Electrical Stimulation on Lower Limbs of Patients with Hemiplegia After Chronic Stroke: A Systematic Review. Arch. Phys. Med. Rehabil. 2018, 99, 1011–1022.e1. [Google Scholar] [CrossRef]
- Wong, P.; Fransch, S.; Gallagher, C.; Francis, K.L.; Khot, A.; Rutz, E.; Graham, H.K. Split anterior tibialis tendon transfer to peroneus brevis for spastic equinovarus in children with hemiplegia. J. Child. Orthop. 2021, 15, 279–290. [Google Scholar] [CrossRef] [PubMed]
- Rodda, J.; Graham, H.K. Classification of gait patterns in spastic hemiplegia and spastic diplegia: A basis for a management algorithm. Eur. J. Neurol. 2001, 8 (Suppl. S5), 98–108. [Google Scholar] [CrossRef] [PubMed]
- Kadaba, M.P.; Ramakrishnan, H.K.; Wootten, M.E. Measurement of lower extremity kinematics during level walking. J. Orthop. Res. 1990, 8, 383–392. [Google Scholar] [CrossRef] [PubMed]
- Martins, E.; Cordovil, R.; Oliveira, R.; Pinho, J.; Diniz, A.; Vaz, J.R. The Immediate Effects of a Dynamic Orthosis on Gait Patterns in Children with Unilateral Spastic Cerebral Palsy: A Kinematic Analysis. Front. Pediatr. 2019, 7, 42. [Google Scholar] [CrossRef]
- Park, K.-B.; Park, H.; Park, B.K.; Abdel-Baki, S.W.; Kim, H.W. Clinical and Gait Parameters Related to Pelvic Retraction in Patients with Spastic Hemiplegia. J. Clin. Med. 2019, 8, 679. [Google Scholar] [CrossRef]
- Aminian, A.; Vankoski, S.J.; Dias, L.; Novak, R.A. Spastic Hemiplegic Cerebral Palsy and the Femoral Derotation Osteotomy: Effect at the Pelvis and Hip in the Transverse Plane During Gait. J. Pediatr. Orthop. 2003, 23, 314–320. [Google Scholar] [CrossRef]
- Arnold, A.S.; Asakawa, D.J.; Delp, S.L. Do the hamstrings and adductors contribute to excessive internal rotation of the hip in persons with cerebral palsy? Gait Posture 2000, 11, 181–190. [Google Scholar] [CrossRef]
- Rutz, E.; Passmore, E.; Baker, R.; Graham, K.H. Multilevel Surgery Improves Gait in Spastic Hemiplegia but Does Not Resolve Hip Dysplasia. Clin. Orthop. Relat. Res. 2012, 470, 1294–1302. [Google Scholar] [CrossRef]
- Ito, I.; Miura, K.; Kimura, Y.; Sasaki, E.; Tsuda, E.; Ishibashi, Y. Retraction: Differences between the Craig’s test and computed tomography in measuring femoral anteversion in patients with anterior cruciate ligament injuries. J. Phys. Ther. Sci. 2020, 32, 365–369. [Google Scholar] [CrossRef]
- Uota, S.; Morikita, I.; Shimokochi, Y. Validity and clinical significance of a clinical method to measure femoral anteversion. J. Sports Med. Phys. Fit. 2019, 59, 1908–1914. [Google Scholar] [CrossRef]


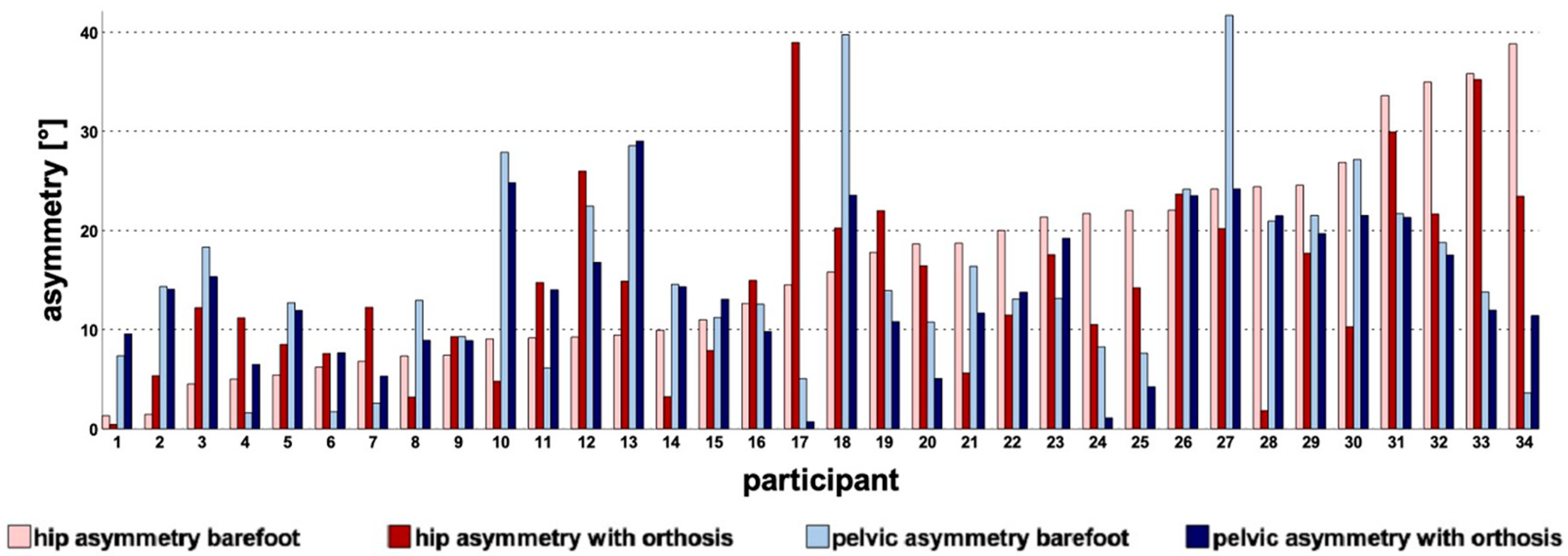
| Variable | Calculation |
|---|---|
| Pelvic asymmetry barefoot [°] | |mean pelvic rotation GC affected/unaffected side| |
| Pelvic asymmetry with orthosis [°] | |mean pelvic rotation GC affected/unaffected side| |
| Δ pelvic asymmetry [°] | barefoot affected side/orthotic affected side |
| Hip asymmetry barefoot [°] | |mean hip rotation ST affected/unaffected side| |
| Hip asymmetry with orthosis [°] | |mean hip rotation ST affected/unaffected side| |
| Δ hip asymmetry [°] | barefoot affected side/orthotic affected side |
| Δ mean hip rotation ST [°] | orthotic affected side/barefoot affected side |
| Δ hip rotation IC [°] | orthotic affected side/barefoot affected side |
| Δ hip rotational moments ST [°] | orthotic affected side/barefoot affected side |
| Barefoot Δ hip rotation [°] | hip rotation midstance/hip rotation initial contact |
| Orthotic Δ hip rotation [°] | hip rotation midstance/hip rotation initial contact |
| Δ ankle dorsi/plantar flexion IC [°] | orthotic affected side/barefoot affected side |
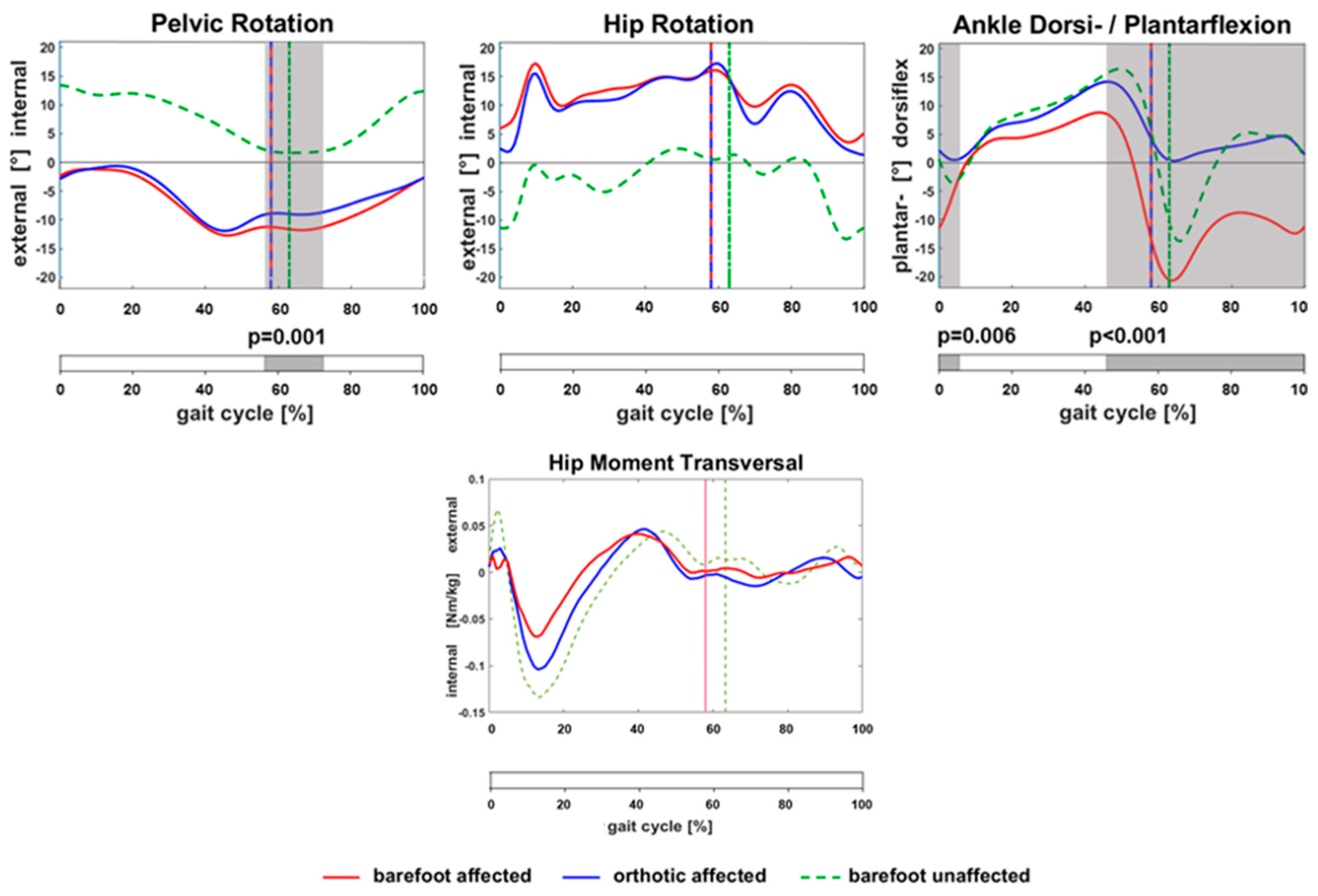
| Parameter | Barefoot (Mean ± SD) [°] | Orthoses (Mean ± SD) [°] | p-Value |
|---|---|---|---|
| Pelvic rotation GC (mean) | −7.4 ± 5.5 | −6.1 ± 4.7 | 0.018 |
| Pelvic rotation GC (ROM) | 16.6 ± 4.3 | 16.3 ± 4.9 | 0.657 |
| Pelvic asymmetry | 15.5 ± 9.8 | 13.9 ± 7.2 | 0.106 |
| Hip rotation ST (mean) | 12.9 ± 6.3 | 11.6 ± 8.4 | 0.398 |
| Hip rotation ST (ROM) | 21.1 ± 8.2 | 25.1 ± 9.4 | <0.001 |
| Hip asymmetry | 16.2 ± 10.2 | 14.6 ± 9.3 | 0.326 |
| Ankle dorsi/plantar flexion IC | −11.5 ± 6.0 | 2.2 ± 4.1 | <0.001 |
| Ankle dorsi/plantar flexion ST (mean) | 3.2 ± 8.8 | 8.0 ± 4.6 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grisch, D.; Stäuble, M.; Baumgartner, S.; van Hedel, H.J.A.; Meyer-Heim, A.; Dreher, T.; Krautwurst, B. The Variable Influence of Orthotic Management on Hip and Pelvic Rotation in Children with Unilateral Neurogenic Equinus Deformity. Children 2023, 10, 307. https://doi.org/10.3390/children10020307
Grisch D, Stäuble M, Baumgartner S, van Hedel HJA, Meyer-Heim A, Dreher T, Krautwurst B. The Variable Influence of Orthotic Management on Hip and Pelvic Rotation in Children with Unilateral Neurogenic Equinus Deformity. Children. 2023; 10(2):307. https://doi.org/10.3390/children10020307
Chicago/Turabian StyleGrisch, Domenic, Manuela Stäuble, Sandra Baumgartner, Hubertus J. A. van Hedel, Andreas Meyer-Heim, Thomas Dreher, and Britta Krautwurst. 2023. "The Variable Influence of Orthotic Management on Hip and Pelvic Rotation in Children with Unilateral Neurogenic Equinus Deformity" Children 10, no. 2: 307. https://doi.org/10.3390/children10020307
APA StyleGrisch, D., Stäuble, M., Baumgartner, S., van Hedel, H. J. A., Meyer-Heim, A., Dreher, T., & Krautwurst, B. (2023). The Variable Influence of Orthotic Management on Hip and Pelvic Rotation in Children with Unilateral Neurogenic Equinus Deformity. Children, 10(2), 307. https://doi.org/10.3390/children10020307





