Oral Health Status of Ngäbe-Buglé Children in Panama: A Cross Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
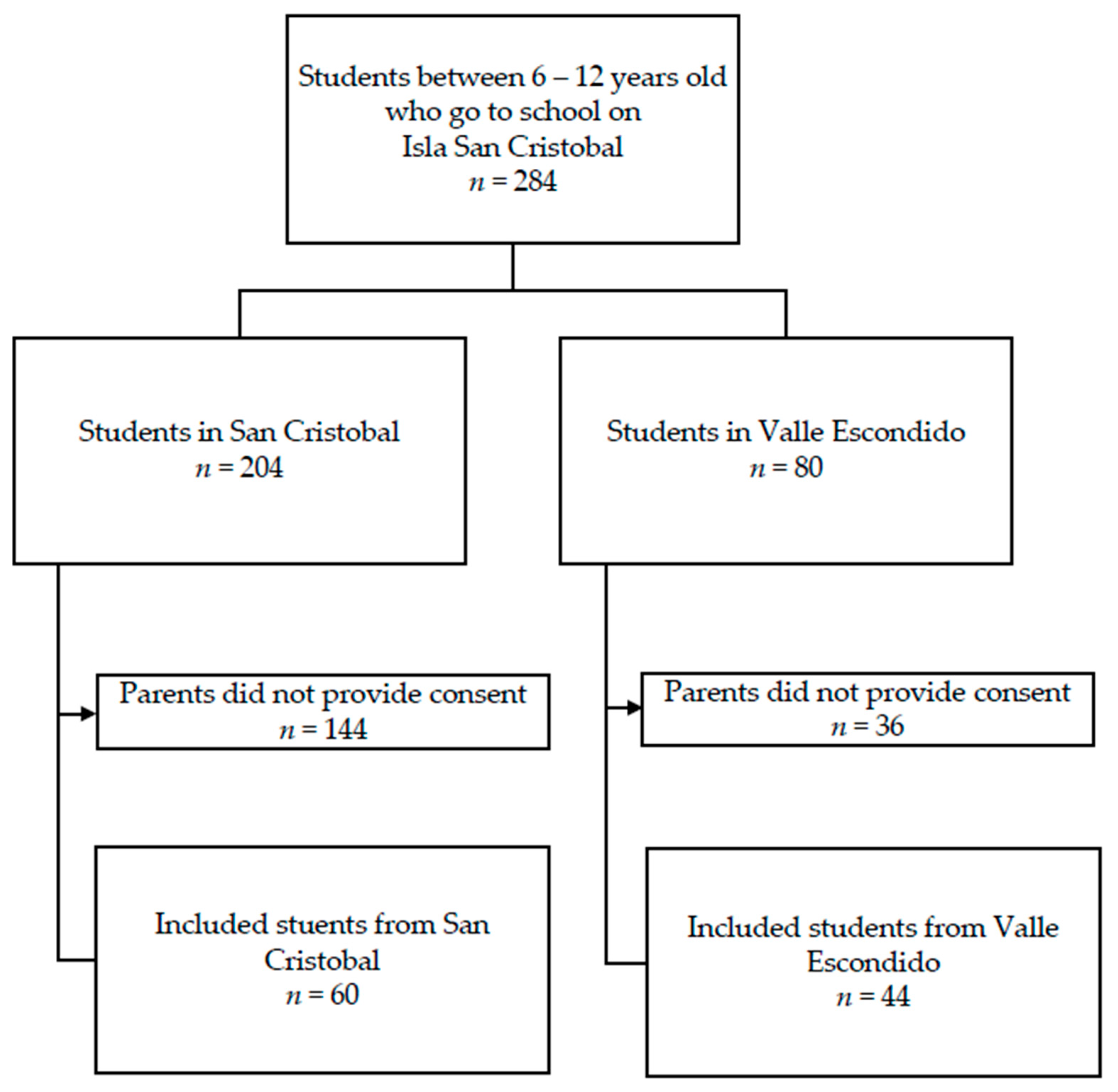
2.1. Study Population
2.2. Study Procedures
2.3. Assessment of Oral Health
2.4. Assessment of Orthodontic Characteristics
2.5. Statistical Analysis
3. Results
3.1. Oral Health Outcomes
3.2. Orthodontic Characteristics
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AOB | Anterior open-bite |
| BASCD | British Association of the Study Community Dentistry |
| DDE | Dental defects of the enamel |
| DMFT | Decayed, missing due to caries, and filled teeth (permanent teeth) |
| dmft | Decayed, missing due to caries, and filled teeth (primary teeth) |
| FDI | Federation Dental International |
| MINSA | Ministry of Health in Panama |
| NGO | Non-governmental organization |
| SD | Standard deviation |
| WHO | World Health Organization |
Appendix A
| 1 |
Cuál es tu nombre y apellido?/ Cual es tu nombre completo? • What is your name and last name?/What is your full name? |
| 2 | Cuál es tu fecha de nacimiento?/ Cuando es tu cumpleaños?/ Cuando naciste? • What is your date of birth?/When is your birthday?/When were you born? |
| 3 | Te cepillas los dientes por lo menos una vez al día?/ Tu cepillas los dientes todos los días? • Do you brush your teeth at least once a day?/Do you brush your teeth every day? |
| 4 | Comes dulces o tomas bebidas con azúcar durante el día? Por ejemplo: confites, galletas, chocolates, caramelos, duros, soda, refresco, pinolio, café con azúcar, chocolito. • Do you eat candy or drink water during the day? For example: candy, cookies, chocolates, caramel, soda, refresco, soda, pinolio, coffee with sugar, chocolito |
| 5 | Tomas soda cada dia?/diario?/todos los dias? • Do you drink soda each day?/daily?/everyday? |
| 6 | Tomas chocolito cada dia?/ diario?/ todos los dias? • Do you drink Chocolito each day?/daily?/everyday? |
| 7 | Tomas confites cada dia?/ diario?/ todos los dias? • Do you eat candy each day?/daily?/everyday? |
| 8 | Tienes una problema de salud?/Tienes problemas médicos?/ Has visitado al médico regularmente? • Do you have health problems?/Do you have medical problems?/Have you visited the doctor regularly? |
| 9 | Sabes que enfermedad tienes?/ Sabes el nombre de la enfermedad? • Do you know what disease you have?/Do you know the name of the disease? |
| 10 | Tomas pastillas diarias?/ Tomas algunas medicamentos regularmente? • Do you take pills daily?/Do you take medication regularly? |
| 11 | Sabes el nombre del medicamento?/ Como se llama los pastillas? • Do you know the name of the medication?/What is the name of the pills? |
| 12 | Has visitado una dentista antes?/ Es tu primera vez al dentista?/ Has ido al dentista antes? • Have you visited a dentist before?/Is this your first time at a dentist?/ Have you gone to a dentist before? |
| 13 | Tu primera visita con la dentista era con los doctores flotantes?/ Fuiste al dentista con doctores flotantes antes? • What your first dental visit with Floating Doctors?/Did you go to a Floating Doctor’s dentist before? |
References
- Fiorillo, L. Oral Health: The First Step to Well-Being. Medicina 2019, 55, 676. [Google Scholar] [CrossRef] [PubMed]
- Institute for Health Metrics and Evaluation (IHME). Global Burden of Disease Study 2019 (GBD 2019); University of Washington: Seattle, DC, USA, 2020; Available online: http://ghdx.healthdata.org/gbd-results-tool (accessed on 1 October 2020).
- World Health Organization. Available online: https://www.who.int/news-room/fact-sheets/detail/oral-health (accessed on 14 December 2021).
- Thomson, S.; Cylus, J.E.T. Can People Afford to Pay for Heatlh Care? New Evidence on Financial Protection in Europe; WHO Regional Office for Europe: Copenhagen, Denmark, 2019. [Google Scholar]
- Bernabé, E.; Masood, M.; Vujicic, M. The impact of out-of-pocket payments for dental care on household finances in low and middle income countries. BMC Public Health 2017, 17, 109. [Google Scholar] [CrossRef] [PubMed]
- MINSA. Programa de Salud Bucal. Available online: https://www.minsa.gob.pa/programa/programa-de-salud-bucal (accessed on 1 September 2022).
- World Data Atlas. Ngabe-Bugle—Total—Life Expectancy at Birth (Years). 2011. Available online: https://knoema.com/atlas/Panama/Ngabe-Bugle/Life-Expectancy-at-birth (accessed on 1 September 2022).
- Matsuo, M.-C.; Gottlieb, J.; Goodrich, L.; Ewald, I.; Velasco, A.; Steller, J. Trends in Prenatal Care Among the Ngöbe Population of Panama [34M]. Obstet. Gynecol. [Internet] 2017, 129, S141. Available online: https://journals.lww.com/greenjournal/Fulltext/2017/05001/Trends_in_Prenatal_Care_Among_the_Ng_be_Population.505.aspx (accessed on 1 September 2022). [CrossRef]
- González-Fernández, D.; Koski, K.G.; Sinisterra, O.T.; Del Carmen Pons, E.; Murillo, E.; Scott, M.E. Interactions among urogenital, intestinal, skin, and oral infections in pregnant and lactating Panamanian Ngäbe women: A neglected public health challenge. Am. J. Trop. Med. Hyg. 2015, 92, 1100–1110. [Google Scholar] [CrossRef] [PubMed]
- Naimi-Akbar, A.; Nordström, M. Oral Health Country/Area Profile Project (CAPP); Oral Health Country/Area Profile Project. Malmö University: Malmö, Sweden. Available online: https://capp.mau.se/country-areas/panama/ (accessed on 1 September 2022).
- Floating Doctors. Available online: https://floatingdoctors.com/ (accessed on 1 September 2022).
- Pitts, N.B.; Evans, D.J.; Pine, C.M. British Association for the Study of Community Dentistry (BASCD) diagnostic criteria for caries prevalence surveys-1996/97. Community Dent. Health 1997, 14, 6–9. Available online: http://europepmc.org/abstract/MED/9114553 (accessed on 1 September 2022). [PubMed]
- WHO. Oral Health Surveys, Basic Methods, 5th ed; WHO: Geneva, Switzerland, 2013; Available online: https://capp.mau.se/media/1016/who-oral-health-surveys-basic-methods-5th-ed.pdf (accessed on 1 September 2022).
- Bazmi, B.A.; Mandal, S.; Ghosh, C.; Sarkar, S.; Pal, J.; Kar, S. Assessment of oral health status of Santal (Tribal) children of West Bengal. J. Indian Soc. Pedod. Prev. Dent. 2015, 33, 44–47. [Google Scholar] [CrossRef] [PubMed]
- Clarkson, J. Review of Terminology, Classifications, and Indices of Developmental Defects of Enamel. Adv. Dent. Res. 1989, 3, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Horowitz, H.S. Indexes for Measuring Dental Fluorosis. J. Public Health Dent. 1986, 46, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Proffit, W.; Fields, H.; Larson, B.; Sarver, D. Contemporary Orthodontics, 6th ed; Elsevier: Amsterdam, The Netherlands, 2018. [Google Scholar]
- Astroth, J.; Berg, R.; Berkey, D.; McDowell, J.; Hamman, R.; Mann, J. Dental caries prevalence and treatment need in Chiriqui Province, Panama. Int. Dent. J. 1998, 48, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Pawlaczyk-Kamieńska, T.; Torlińska-Walkowiak, N.; Borysewicz-Lewicka, M. The relationship between oral hygiene level and gingivitis in children. Adv. Clin. Exp. Med. 2018, 27, 1397–1401. [Google Scholar] [CrossRef]
- Subedi, K.; Shrestha, A.; Bhagat, T.; Baral, D. Effectiveness of oral health education intervention among 12–15-year-old school children in Dharan, Nepal: A randomized controlled trial. BMC Oral Health 2021, 21, 525. [Google Scholar] [CrossRef] [PubMed]
- Uauy, R.; Monteiro, C.A. The challenge of improving food and nutrition in Latin America. Food Nutr. Bull. 2004, 25, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Levin, A.; Sokal-Gutierrez, K.; Hargrave, A.; Funsch, E.; Hoeft, K.S. Maintaining Traditions: A Qualitative Study of Early Childhood Caries Risk and Protective Factors in an Indigenous Community. Int. J. Environ. Res. Public Health 2017, 14, 907. [Google Scholar] [CrossRef] [PubMed]
- Association Between the Severity of Malocclusion, Assessed by Occlusal Indices, and Oral Health Related Quality of Life: A Systematic Review and Meta-Analysis. Oral Health Prev. Dent. 2018, 16, 211–223. [CrossRef]
- Alhammadi, M.S.; Halboub, E.; Fayed, M.S.; Labib, A.; El-Saaidi, C. Global distribution of malocclusion traits: A systematic review. Dent. Press J. Orthod. 2018, 23, 40.e1–40.e10. [Google Scholar] [CrossRef] [PubMed]
- Barros, S.E.; Chiqueto, K.; Janson, G.; Ferreira, E. Factors influencing molar relationship behavior in the mixed dentition. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 782–792. [Google Scholar] [CrossRef] [PubMed]
- Aamodt, K.; Reyna-Blanco, O.; Sosa, R.; Hsieh, R.; De la Garza Ramos, M.; Garcia Martinez, M.; Orellana, M.F. Prevalence of caries and mal-occlusion in an indigenous population in Chiapas, Mexico. Int. Dent. J. 2015, 65, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Ling, H.T.B.; Sum, F.H.K.M.H.; Zhang, L.; Yeung, C.P.W.; Li, K.Y.; Wong, H.M.; Yang, Y. The association between nutritive, non-nutritive sucking habits and primary dental occlusion. BMC Oral. Health 2018, 18, 145. [Google Scholar] [CrossRef] [PubMed]

| San Cristobal | Valle Escondido | Total | p Value | |
|---|---|---|---|---|
| n = 60 | n = 46 | n = 106 | ||
| mean (SD) | mean (SD) | mean (SD) | ||
| Age | 8.7 (1.7) | 8.6 (1.8) | 8.7 (1.7) | 0.600 |
| BMI | 17.8 (2.1) | 19 (3.2) | 18.3 (2.7) | 0.018 |
| n (%) | n (%) | n (%) | ||
| Systemic diseases ^ | 2 (3.3) | 2 (4.2) | 4 (3.8) | 0.787 |
| Regular medication use * | 0 | 3 (6.5) | 3 (2.8) | 0.079 |
| Type of dentition | 0.156 | |||
| Primary dentition | 0 | 2 (4.3) | 2 (1.9) | |
| Mixed dentition | 44 (73.3) | 30 (65.2) | 74 (69.8) | |
| Permanent dentition | 16 (26.7) | 14 (30.4) | 30 (28.3) | |
| First dental examination | 40 (66.7) | 41 (89.1) | 81 (76.4) | 0.007 |
| Daily toothbrushing | 43 (71.7) | 26 (56.5) | 69 (65.1) | 0.105 |
| Sugar intake outside of main meals | 59 (98.3) | 46 (100) | 105 (99.1) | 0.284 |
| Daily intake of soda drinks | 17 (28.3) | 9 (19.6) | 26 (24.5) | 0.298 |
| Daily intake of hot chocolate | 31 (51.7) | 10 (21.7) | 41 (38.7) | 0.002 |
| Daily intake of candies | 19 (31.7) | 9 (19.6) | 28 (26.4) | 0.161 |
| San Cristobal | Valle Escondido | Total | |
|---|---|---|---|
| n = 60 | n = 46 | n = 106 | |
| PI, mean (SD) | 2.8 (0.8) | 2.9 (0.7) | 2.8 (0.8) |
| Excellent hygiene (PI = 0), n (%) | 6 (10.0) | 2 (4.3) | 8 (7.5) |
| Good hygiene (PI = 0.1–0.9), n (%) | 9 (15.0) | 8 (17.4) | 17 (16.0) |
| Fair hygiene (PI = 1.0–1.9), n (%) | 35 (58.3) | 30 (65.2) | 65 (61.3) |
| Poor hygiene (PI = 2.0–3.0), n (%) | 10 (16.7) | 6 (13.00) | 16 (15.1) |
| San Cristobal | Valle Escondido | Total | p Values | |
|---|---|---|---|---|
| n = 60 | n = 46 | n = 106 | ||
| mean (SD) | mean (SD) | mean (SD) | ||
| Prevalence of children with caries, n (%) | 48 (80.0) | 36 (78.3) | 84 (79.2) | 0.827 |
| DMFT/dmft in children with caries | 3.7 (2.5) | 4.6 (2.9) | 4.05 (2.7) | 0.184 |
| DMFT/dmft in the entire sample | 3.1 (2.6) | 3.6 (3.2) | 3.3 (2.9) | 0.520 |
| D/d | 2.9 (2.6) | 3.3 (2.1) | 3.1 (2.8) | 0.497 |
| M/m | 0.1 (0.1 | 0.2 (0.7) | 0.1 (0.5) | 0.189 |
| F/f | 0.2 (0.7) | 0.2 (1.0) | 0.2 (0.8) | 0.765 |
| * DMFT in the entire sample | 0.5 (0.8) | 0.8 (1.4) | 0.6 (1.1) | 0.945 |
| DT | 0.5 (0.8) | 0.6 (1.2) | 0.6 (1.0) | 0.672 |
| MT | 0.0 (0.1) | 0.0 (0.1) | 0.0 (0.1) | 0.850 |
| FT | 0 | 0.1 (0.4) | 0.0 (0.3) | 0.105 |
| * dmft in the entire sample | 3.5 (2.7) | 4.2 (3.2) | 3.8 (2.9) | 0.378 |
| dt | 2.4 (2.7) | 2.7 (3.2) | 2.51 (2.9) | 0.887 |
| mt | 0 | 0.1 (0.7) | 0.1 (0.4) | 0.105 |
| ft | 0.2 (0.7) | 0.1 (0.7) | 0.2 (0.7) | 0.437 |
| San Cristobal | Valle Escondido | Total | p Value | |
|---|---|---|---|---|
| n = 60 n (%) | n = 44 n (%) | n = 104 n (%) | ||
| Sagittal Molar Class | 0.122 | |||
| Class I | 47 (78.3) | 36 (81.8) | 83 (78.3) | |
| Class II | 4 (6.7) | 6 (13.0) | 10 (9.4) | |
| Class III | 9 (15.0) | 2 (4.3) | 11 (10.4) | |
| Anterior open bite | 5 (8.3) | 6 (13.0) | 11 (10.4) | 0.521 |
| Lateral crossbite in habitual occlusion | 0.230 | |||
| Absent | 56 (93.3%) | 44 (97.8) | 99 (93.4) | |
| Unilateral | 4 (6.7) | 1 (2.2) | 5 (4.7) | |
| Bilateral | 0 | 0 | 0 | |
| Anterior crossbite | 1 (1.7) | 2 (4.3) | 2 (1.9) | 0.578 |
| Scissor bite | 0 | 0 | 0 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hagens, E.R.C.; Preatoni, S.M.; Bazzini, E.M.; Akam, D.; McKalip, K.S.; LaBrot, B.; Cagetti, M.G. Oral Health Status of Ngäbe-Buglé Children in Panama: A Cross Sectional Study. Children 2023, 10, 294. https://doi.org/10.3390/children10020294
Hagens ERC, Preatoni SM, Bazzini EM, Akam D, McKalip KS, LaBrot B, Cagetti MG. Oral Health Status of Ngäbe-Buglé Children in Panama: A Cross Sectional Study. Children. 2023; 10(2):294. https://doi.org/10.3390/children10020294
Chicago/Turabian StyleHagens, Eliza R. C., Sofia Maddalena Preatoni, Elena M. Bazzini, Daniel Akam, Konrad S. McKalip, Ben LaBrot, and Maria Grazia Cagetti. 2023. "Oral Health Status of Ngäbe-Buglé Children in Panama: A Cross Sectional Study" Children 10, no. 2: 294. https://doi.org/10.3390/children10020294
APA StyleHagens, E. R. C., Preatoni, S. M., Bazzini, E. M., Akam, D., McKalip, K. S., LaBrot, B., & Cagetti, M. G. (2023). Oral Health Status of Ngäbe-Buglé Children in Panama: A Cross Sectional Study. Children, 10(2), 294. https://doi.org/10.3390/children10020294







