Modeling the Risk Factors of Undernutrition among Children below Five Years of Age in Uganda Using Generalized Structural Equation Models
Abstract
1. Introduction
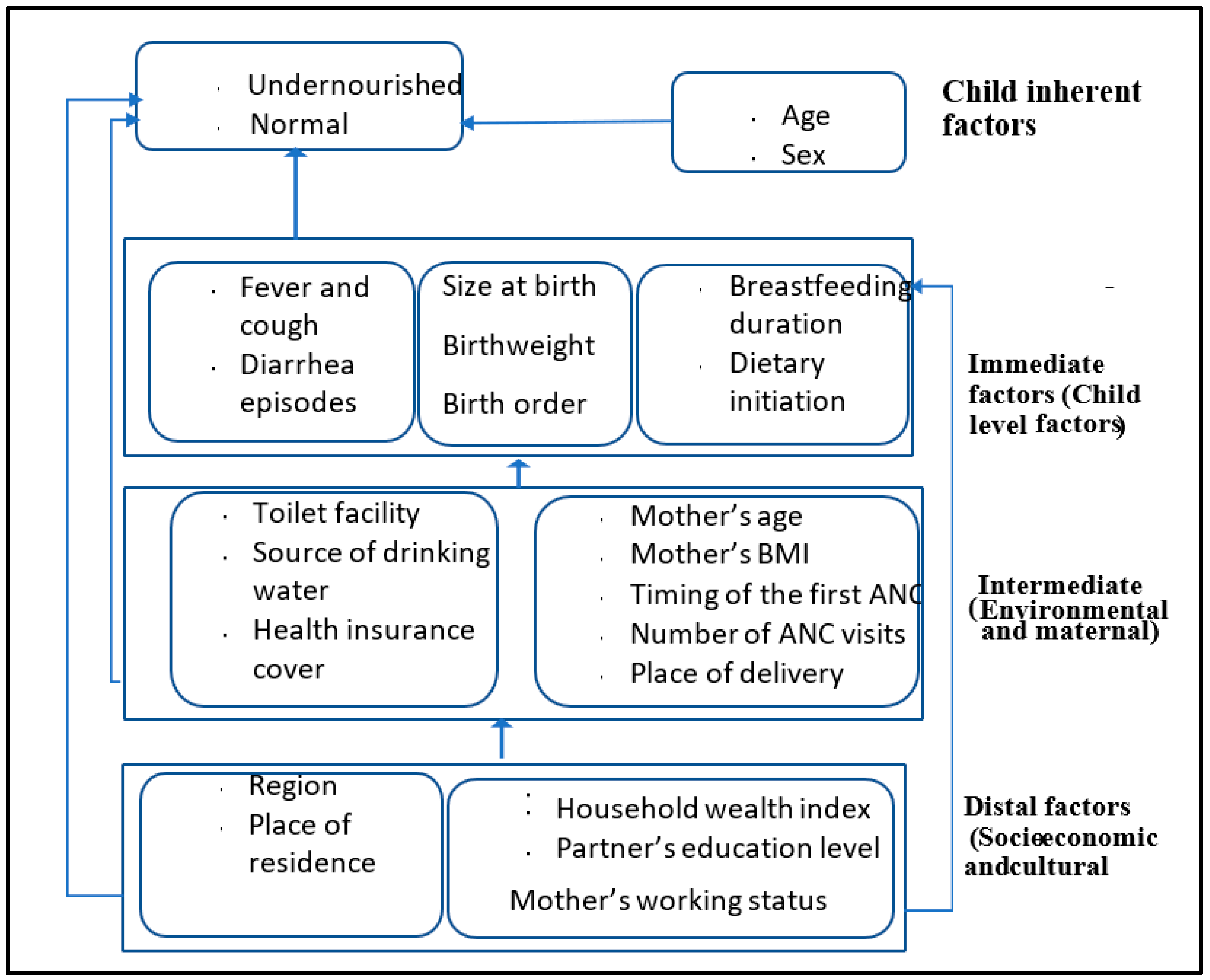
2. Methods and Materials
2.1. The Study Area and Data
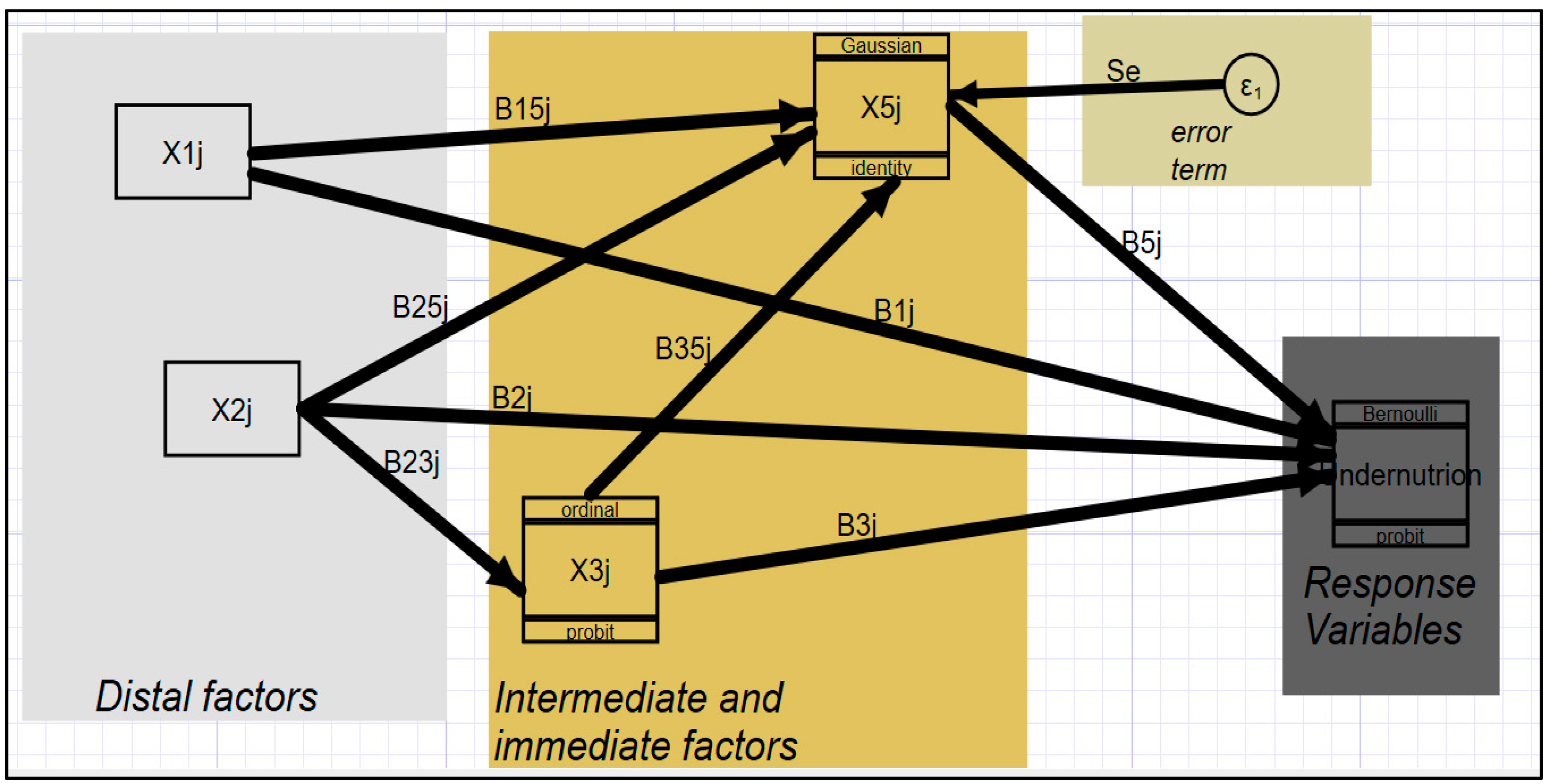
2.2. Model Building and Estimation Methods
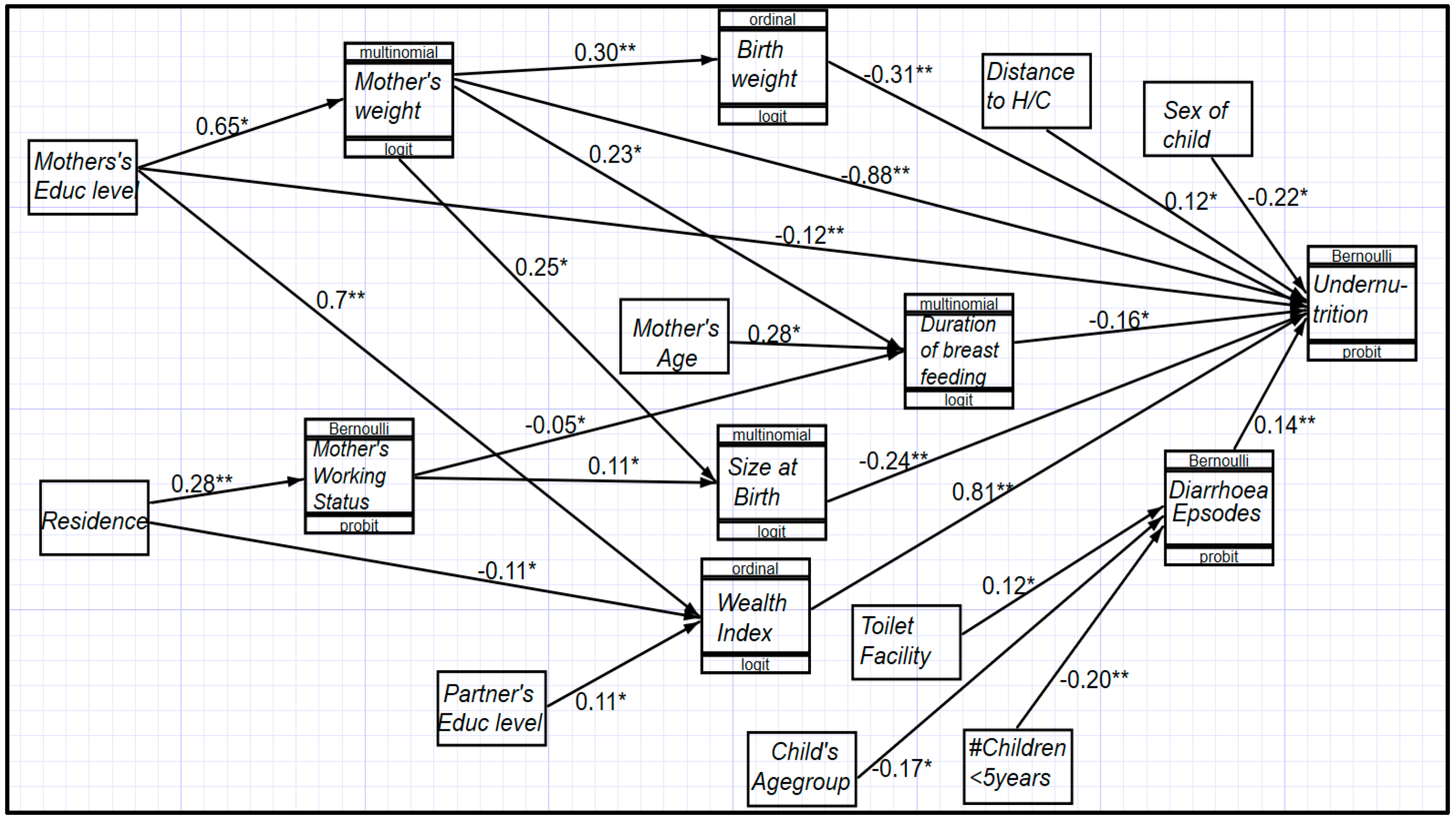
3. Results
- (i)
- Having no education was associated with limited working opportunities to generate some income, which increased the likelihood of a low household wealth status and, hence, increased the chances of undernutrition.
- (ii)
- Rurality was also associated with an increased likelihood of undernutrition through association with poor and/or low employment opportunities within rural areas.
- (iii)
- A shorter duration of breastfeeding was a common phenomenon in urban areas and was associated with an increased likelihood of undernutrition in such areas.
- (iv)
- The rest of the factors, sex of the child and distance to a health center, are purely exogenous in this model.
- (v)
- Children who were aged 6–47 months had an increased likelihood of undernutrition, especially those who were in unhealthy environments, such as poor households or environments with no toilet facilities, since these environments were associated with an increased likelihood of diarrhea episodes. The age category from 48 to 59 months turned out to be a statistically insignificant factor in influencing undernutrition among children below 5 years of age in Uganda.
4. Discussion of the Results
5. Conclusions
6. Strength of This Study
7. Limitations of This Study
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Levels and Trends in Child Malnutrition; World Health Organization: Geneva, Switzerland, 2021.
- Boah, M.; Azupogo, F.; Amporfro, D.A.; Abada, L.A. The epidemiology of undernutrition and its determinants in children under five years in Ghana. PLoS ONE 2019, 14, e0219665. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Raine, A. Nutritional status and social behavior in preschool children: The mediating effects of neurocognitive functioning. Matern. Child Nutr. 2017, 13, e12321. [Google Scholar] [CrossRef] [PubMed]
- Ghattas, H.; Acharya, Y.; Jamaluddine, Z.; Assi, M.; El Asmar, K.; Jones, A.D. Child-level double burden of malnutrition in the MENA and LAC regions: Prevalence and social determinants. Matern. Child Nutr. 2020, 16, e12923. [Google Scholar] [CrossRef] [PubMed]
- Madrigano, J. 基因的改变 NIH Public Access. Occup. Environ. Med. 2008, 23, 1–7. [Google Scholar]
- Fisher Walker, C.L.; Lamberti, L.; Adair, L.; Guerrant, R.L.; Lescano, A.G.; Martorell, R.; Pinkerton, R.C.; Black, R.E. Does childhood diarrhea influence cognition beyond the diarrhea-stunting pathway? PLoS ONE 2012, 7, e47908. [Google Scholar] [CrossRef]
- Lorntz, B.; Soares, A.M.; Moore, S.R.; Pinkerton, R.; Gansneder, B.; Bovbjerg, V.E.; Guyatt, H.; Lima, A.M.; Guerrant, R.L. Early childhood diarrhea predicts impaired school performance. Pediatr. Infect. Dis. J. 2006, 25, 513–520. [Google Scholar] [CrossRef]
- Thompson, D.S.; Younger-Coleman, N.; Lyew-Ayee, P.; Greene, L.-G.; Boyne, M.S.; Forrester, T.E. Socioeconomic factors associated with severe acute malnutrition in Jamaica. PLoS ONE 2017, 12, e0173101. [Google Scholar] [CrossRef]
- Zerga, A.A.; Tadesse, S.E.; Ayele, F.Y.; Ayele, S.Z. Impact of malnutrition on the academic performance of school children in Ethiopia: A systematic review and meta-analysis. SAGE Open Med. 2022, 10. [Google Scholar] [CrossRef]
- Wali, N.; Agho, K.E.; Renzaho, A.M.N. Wasting and associated factors among children under 5 years in five south asian countries (2014–2018): Analysis of demographic health surveys. Int. J. Environ. Res. Public Health 2021, 18, 4578. [Google Scholar] [CrossRef]
- United Nations Children’s Fund (UNICEF). Southeast Asia Regional Report on Maternal Nutrition and Complementary Feeding; United Nations Children’s Fund (UNICEF): New York, NY, USA, 2021; p. 83. [Google Scholar]
- World Bank Group. Health at a Glance: Latin America and the Caribbean 2020; Organisation for Economic Co-Operation and Development (OECD): Paris, France, 2020. [Google Scholar] [CrossRef]
- UNICEF. Progress on Children’s Well-Being: Centring Child Rights in the 2030 Agenda; United Nations Children’s Fund (UNICEF): New York, NY, USA, 2023. [Google Scholar]
- UBOS. Uganda Demographic and Health Survey 2016: Key Indicators Report; UBOS: Kampala, Uganda, 2018.
- Ashaba, S.; Rukundo, G.Z.; Beinempaka, F.; Ntaro, M.; LeBlanc, J.C. Maternal depression and malnutrition in children in southwest Uganda: A case control study. BMC Public Health 2015, 15, 1303. [Google Scholar] [CrossRef]
- Maniragaba, V.N.; Atuhaire, L.K.; Rutayisire, P.C. Undernutrition among the children below five years of age in Uganda: A spatial analysis approach. BMC Public Health 2023, 23, 390. [Google Scholar] [CrossRef] [PubMed]
- Amegbor, P.M.; Zhang, Z.; Dalgaard, R.; Sabel, C.E. Multilevel and spatial analyses of childhood malnutrition in Uganda: Examining individual and contextual factors. Sci. Rep. 2020, 10, 20019. [Google Scholar] [CrossRef] [PubMed]
- Amusa, L.B.; Yahya, W.B.; Bengesai, A.V. Spatial variations and determinants of malnutrition among under-five children in Nigeria: A population-based cross-sectional study. PLoS ONE 2023, 18, e0284270. [Google Scholar] [CrossRef] [PubMed]
- Seboka, B.T.; Hailegebreal, S.; Mamo, T.T.; Yehualashet, D.E.; Gilano, G.; Kabthymer, R.H.; Ewune, H.A.; Kassa, R.; Debisa, M.A.; Yawo, M.N.; et al. Spatial trends and projections of chronic malnutrition among children under 5 years of age in Ethiopia from 2011 to 2019: A geographically weighted regression analysis. J. Health Popul. Nutr. 2022, 41, 28. [Google Scholar] [CrossRef]
- (UBOS) Uganda Bureau of Statistics. National Population and Housing Census 2014—Main Report; Uganda Bureau of Statistics (UBOS): Kampala, Uganda, 2016.
- Habaasa, G. An investigation on factors associated with malnutrition among underfive children in Nakaseke and Nakasongola districts, Uganda. BMC Pediatr. 2015, 15, 134. [Google Scholar] [CrossRef]
- Permatasari, T.A.E.; Chadirin, Y. Assessment of undernutrition using the composite index of anthropometric failure (CIAF) and its determinants: A cross-sectional study in the rural area of the Bogor District in Indonesia. BMC Nutr. 2022, 8, 133. [Google Scholar] [CrossRef]
- Dipierri, J.E.; Román, E.M.; Abdo, G. Composite index of anthropometric failure and geographic altitude in children from Jujuy (1 to 5 years old). Arch. Argent Pediatr. 2014, 112, 526–531. [Google Scholar]
- Nandy, S.; Svedberg, P. The Composite Index of Anthropometric Failure (CIAF): An alternative indicator for malnutrition in young children. In Handbook of Anthropometry; Springer: Berlin/Heidelberg, Germany, 2012; pp. 127–137. [Google Scholar]
- UNICEF. UNICEF Nutrition Strategy 2020–2030; UNICEF: New York, NY, USA, 2021; No. 65; p. 202020. [Google Scholar]
- Lombardi, S.; Santini, G.; Marchetti, G.M.; Focardi, S. Generalized structural equations improve sexual-selection analyses. PLoS ONE 2017, 12, e0181305. [Google Scholar] [CrossRef]
- Richter, L.M.; Daelmans, B.; Lombardi, J.; Heymann, J.; Boo, F.L.; Behrman, J.R.; Lu, C.; Lucas, J.E.; Perez-Escamilla, R.; Dua, T.; et al. Investing in the foundation of sustainable development: Pathways to scale up for early childhood development. Lancet 2017, 389, 103–118. [Google Scholar] [CrossRef]
- Olwedo, M.A.; Mworozi, E.; Bachou, H.; Orach, C.G. Factors associated with malnutrition among children in internally displaced person’s camps, northern Uganda. Afr. Health Sci. 2008, 8, 244–252. [Google Scholar]
- De, P.; Chattopadhyay, N. Effects of malnutrition on child development: Evidence from a backward district of India. Clin. Epidemiol. Glob. Health 2019, 7, 439–445. [Google Scholar] [CrossRef]
- De Onis, M.; Branca, F. Childhood stunting: A global perspective. Matern. Child Nutr. 2016, 12, 12–26. [Google Scholar] [CrossRef] [PubMed]
- Van de Poel, E.; Hosseinpoor, A.R.; Jehu-Appiah, C.; Vega, J.; Speybroeck, N. Malnutrition and the disproportional burden on the poor: The case of Ghana. Int. J. Equity Health 2007, 6, 21. [Google Scholar] [CrossRef]
- Maleta, K.; Virtanen, S.M.; Espo, M.; Kulmala, T.; Ashorn, P. Childhood malnutrition and its predictors in rural Malawi. Paediatr. Perinat. Epidemiol. 2003, 17, 384–390. [Google Scholar] [CrossRef] [PubMed]
- Rayhan, M.I.; Khan, M.S.H. Factors causing malnutrition among under five children in Bangladesh. Pak. J. Nutr. 2006, 5, 558–562. [Google Scholar]
- Jehn, M.; Brewis, A. Paradoxical malnutrition in mother–child pairs: Untangling the phenomenon of over-and under-nutrition in underdeveloped economies. Econ. Hum. Biol. 2009, 7, 28–35. [Google Scholar] [CrossRef]
- Siddiqi, M.N.A.; Haque, M.N.; Goni, M.A. Malnutrition of under-five children: Evidence from Bangladesh. Asian J. Med. Sci. 2011, 2, 113–119. [Google Scholar] [CrossRef]
- Kimani-Murage, E.W.; Muthuri, S.K.; Oti, S.O.; Mutua, M.K.; van de Vijver, S.; Kyobutungi, C. Evidence of a double burden of malnutrition in urban poor settings in Nairobi, Kenya. PLoS ONE 2015, 10, e0129943. [Google Scholar] [CrossRef]
- Bouzitou, G.D.N.; Fayomi, B.; Delisle, H. Child malnutrition and maternal overweight in same households in poor urban areas of Benin. Cah. D’études Rech. Francoph. Santé 2005, 15, 263–270. [Google Scholar]
- Mahmudiono, T.; Nindya, T.S.; Andrias, D.R.; Megatsari, H.; Rosenkranz, R.R. The effectiveness of nutrition education for overweight/obese mothers with stunted children (NEO-MOM) in reducing the double burden of malnutrition in Indonesia: Study protocol for a randomized controlled trial. BMC Public Health 2016, 16, 486. [Google Scholar] [CrossRef]
- Khan, N.; Rahman, M.; Shariff, A.A.; Rahman, M.; Rahman, S.; Rahman, A. Maternal undernutrition and excessive body weight and risk of birth and health outcomes. Arch. Public Health 2017, 75, 12. [Google Scholar] [CrossRef] [PubMed]
- Wamani, H.; Tylleskär, T.; Åstrøm, A.N.; Tumwine, J.K.; Peterson, S. Mothers’ education but not fathers’ education, household assets or land ownership is the best predictor of child health inequalities in rural Uganda. Int. J. Equity Health 2004, 3, 9. [Google Scholar] [CrossRef] [PubMed]
- Yu, T.; Chen, C.; Jin, Z.; Yang, Y.; Jiang, Y.; Hong, L.; Yu, X.; Mei, H.; Jiang, F.; Huang, H.; et al. Association of number of siblings, birth order, and thinness in 3- To 12-year-old children: A population-based cross-sectional study in Shanghai, China. BMC Pediatr. 2020, 20, 367. [Google Scholar] [CrossRef]
- Dharmaraj, A.; Ghimire, A.; Chinnaiyan, S.; Tiwari, A.K.; Barik, R.K. Comparison of Growth in Children of 6 to 59 Months of Age According to Birth Order: Insights from the National Family Health Survey-4. J. Clin. Diagn. Res. 2021, 15, 25–32. [Google Scholar] [CrossRef]
- Abor, P.A.; Abekah-Nkrumah, G.; Sakyi, K.; Adjasi, C.K.; Abor, J. The socio-economic determinants of maternal health care utilization in Ghana. Int. J. Soc. Econ. 2011, 38, 628–648. [Google Scholar] [CrossRef]
- Nankinga, O.; Kwagala, B.; Walakira, E.J. Maternal employment and child nutritional status in Uganda. PLoS ONE 2019, 14, e0226720. [Google Scholar] [CrossRef]
- Shahraki, M.; Agheli, L.; Arani, A.A.; Sadeqi, H.; Ghaderi, S. The relationship between mother’s socioeconomic status and child health. J. Res. Health 2018, 8, 143–151. [Google Scholar] [CrossRef][Green Version]
- Saibul, N.; Shariff, Z.M.; Lin, K.G.; Kandiah, M.; Nawalyah, A.G.; Hejar, A.R. Food Variety Score Is Associated with Dual Burden of Malnutrition in ‘Orang Asli’ (Malaysian Indigenous Peoples) Households: Implications for Health Promotion. Asia Pac. J. Clin. Nutr. 2009, 18, 412–422. [Google Scholar]
- Jain, A.; Agnihotri, S.B. Assessing inequalities and regional disparities in child nutrition outcomes in India using MANUSH–a more sensitive yardstick. Int. J. Equity Health 2020, 19, 138. [Google Scholar] [CrossRef]
- Sharaf, M.F.; Rashad, A.S. Regional inequalities in child malnutrition in Egypt, Jordan, and Yemen: A Blinder-Oaxaca decomposition analysis. Health Econ. Rev. 2016, 6, 23. [Google Scholar] [CrossRef]
- Wu, Y.; Qi, D. Urban-rural and provincial disparities in child malnutrition in China. Soc. Work Public Health 2016, 31, 574–588. [Google Scholar] [CrossRef] [PubMed]
- Larrea, C.; Kawachi, I. Does economic inequality affect child malnutrition? The case of Ecuador. Soc. Sci. Med. 2005, 60, 165–178. [Google Scholar] [CrossRef] [PubMed]
- Latunji, O.O.; Akinyemi, O.O. Factors influencing health-seeking behaviour among civil servants in Ibadan, Nigeria. Ann. Ibadan Postgrad. Med. 2018, 16, 52–60. [Google Scholar]
- Acharya, D.; Singh, J.K.; Kadel, R.; Yoo, S.-J.; Park, J.-H.; Lee, K. Maternal factors and utilization of the antenatal care services during pregnancy associated with low birth weight in rural Nepal: Analyses of the antenatal care and birth weight records of the MATRI-SUMAN trial. Int. J. Environ. Res. Public Health 2018, 15, 2450. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.S.; Howlader, T.; Masud, M.S.; Rahman, M.L. Association of low-birth weight with malnutrition in children under five years in Bangladesh: Do mother’s education, socio-economic status, and birth interval matter? PLoS ONE 2016, 11, e0157814. [Google Scholar] [CrossRef]
- Larson, L.M.; Martorell, R.; Bauer, P.J. A Path Analysis of Nutrition, Stimulation, and Child Development Among Young Children in Bihar, India. Child Dev. 2018, 89, 1871–1886. [Google Scholar] [CrossRef]
- Shifti, D.M.; Chojenta, C.; Holliday, E.G.; Loxton, D. Maternal anemia and baby birth size mediate the association between short birth interval and under-five undernutrition in Ethiopia: A generalized structural equation modeling approach. BMC Pediatr. 2022, 22, 108. [Google Scholar] [CrossRef]
- Chirande, L.; Charwe, D.; Mbwana, H.; Victor, R.; Kimboka, S.; Issaka, A.I.; Baines, S.K.; Dibley, M.J.; Agho, K.E. Determinants of stunting and severe stunting among under-fives in Tanzania: Evidence from the 2010 cross-sectional household survey. BMC Pediatr. 2015, 15, 165. [Google Scholar] [CrossRef]
| Variable and Category Level | Coefficient | P >|z| | [95%Conf. Interval] |
|---|---|---|---|
| Child inherent level | |||
| Sex | −0.333 | 0.000 | −0.494 −0.171 |
| Immediate or child level factors | |||
| Birth weight | −0.296 | 0.003 | −0.489 −0.103 |
| Birth size | −0.308 | 0.004 | −0.516 −0.100 |
| Breast feeding duration | 0.183 | 0.001 | 0.078 0.287 |
| Intermediate (environmental and maternal) level factors | |||
| Mother’s BMI | −0.020 | 0.000 | −0.067 −0.772 |
| Distal factors | |||
| Wealth index | −0.126 | 0.001 | −0.198 −0.054 |
| Mother’s educ | −0.125 | 0.076 | −0.263 0.013 |
| Distance to HC | 0.196 | 0.021 | 0.029 0.362 |
| Risk Factors of Undernutrition | Coefficient | z | P > |z| |
|---|---|---|---|
| Age group | |||
| 0–5 * | |||
| 6–11 | 0.365 | 2.13 | 0.033 |
| 12–23 | 1.000 | 4.22 | 0.000 |
| 24–35 | 0.729 | 2.66 | 0.008 |
| 36–47 | 0.741 | 2.62 | 0.009 |
| Birth weight category | |||
| small * | |||
| normal | −0.344 | −2.72 | 0.007 |
| big | 0.556 | 2.88 | 0.004 |
| Wealth index | |||
| first * | |||
| middle | −0.249 | −1.71 | 0.088 |
| fourth | −0.466 | −2.93 | 0.003 |
| highest | −0.900 | 4.43 | 0.000 |
| Duration of breast feeding | |||
| 0–11 * | |||
| >24 months | 0.940 | 2.80 | 0.005 |
| Perceived size at birth | |||
| small * | |||
| large | −0.342 | −3.08 | 0.002 |
| Mother’s education level | |||
| no education * | |||
| primary | −0.372 | −2.44 | 0.015 |
| higher | −0.495 | −1.68 | 0.093 |
| Distance to a health center | |||
| not a big problem * | |||
| big problem | 0.204 | 2.25 | 0.025 |
| Sex of the child | |||
| male * | |||
| female | −0.325 | −3.76 | 0.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maniragaba, V.N.; Atuhaire, L.K.; Rutayisire, P.C. Modeling the Risk Factors of Undernutrition among Children below Five Years of Age in Uganda Using Generalized Structural Equation Models. Children 2023, 10, 1926. https://doi.org/10.3390/children10121926
Maniragaba VN, Atuhaire LK, Rutayisire PC. Modeling the Risk Factors of Undernutrition among Children below Five Years of Age in Uganda Using Generalized Structural Equation Models. Children. 2023; 10(12):1926. https://doi.org/10.3390/children10121926
Chicago/Turabian StyleManiragaba, Vallence Ngabo, Leonard K. Atuhaire, and Pierre Claver Rutayisire. 2023. "Modeling the Risk Factors of Undernutrition among Children below Five Years of Age in Uganda Using Generalized Structural Equation Models" Children 10, no. 12: 1926. https://doi.org/10.3390/children10121926
APA StyleManiragaba, V. N., Atuhaire, L. K., & Rutayisire, P. C. (2023). Modeling the Risk Factors of Undernutrition among Children below Five Years of Age in Uganda Using Generalized Structural Equation Models. Children, 10(12), 1926. https://doi.org/10.3390/children10121926





