Early-Term Neonates Demonstrate a Higher Likelihood of Requiring Phototherapy Compared to Those Born Full-Term
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Subjects
2.2. The Timing for Determining Whether to Administer Phototherapy
2.3. Types of Neonatal Feeding
2.4. Statistical Analysis
3. Results
3.1. Differences between Neonates with a Gestational Age of ≤38 and 6/7 Weeks and Those ≥39 and 0/7 Weeks
3.2. Comparison between Groups Who Have Previously Received Phototherapy and Those Who Have Not
3.3. Multivariable Logistic Regression Analysis for Determining Factors Associated with the Administration of Phototherapy
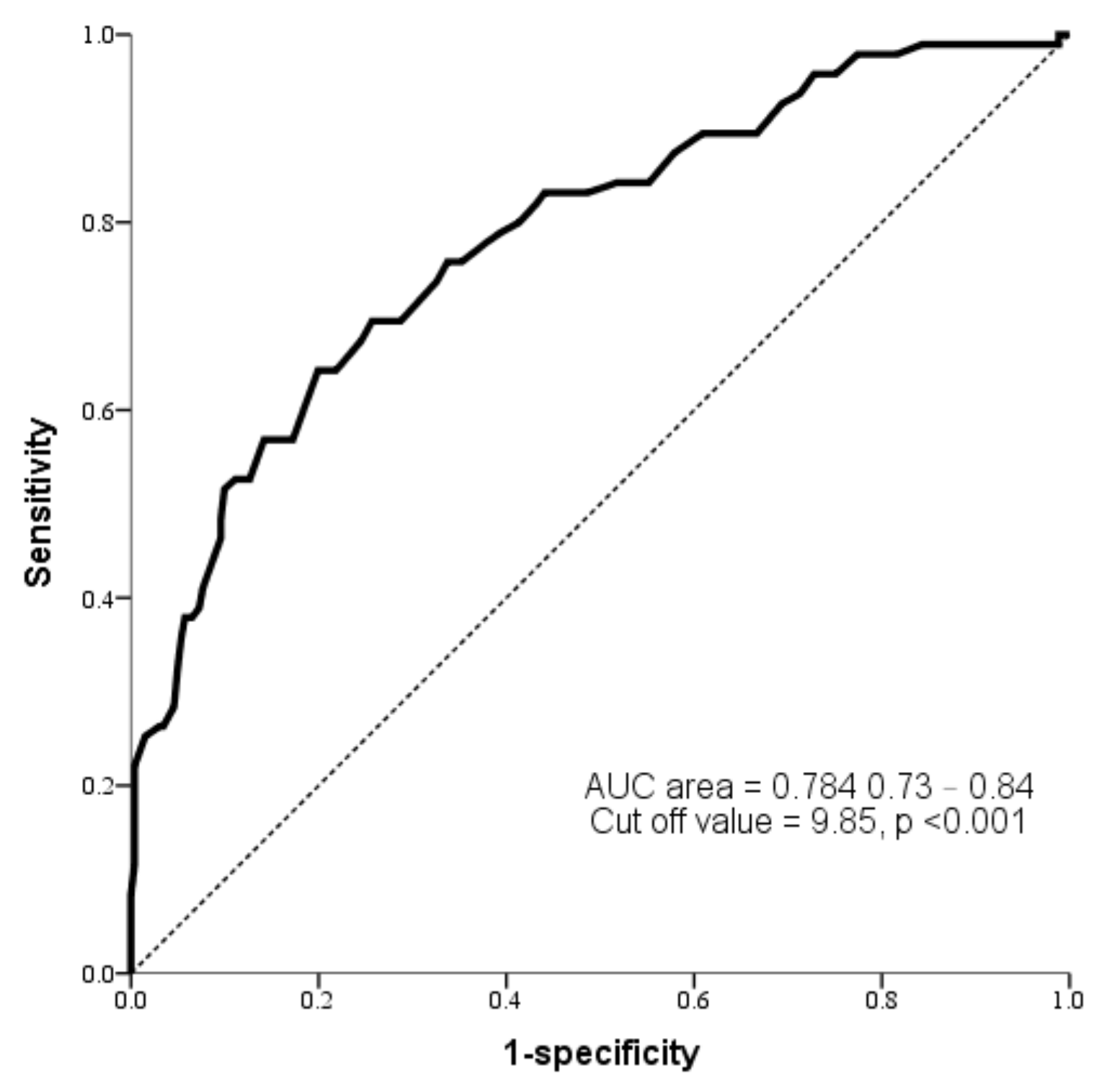
3.4. Evaluating the Diagnostic Value of TcB Levels between 24 and 48 h Postpartum in Predicting the Necessity of Phototherapy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Parikh, L.I.; Reddy, U.M.; Männistö, T.; Mendola, P.; Sjaarda, L.; Hinkle, S.; Chen, Z.; Lu, Z.; Laughon, S.K. Neonatal outcomes in early term birth. Am. J. Obstet. Gynecol. 2014, 211, 265.e1–265.e11. [Google Scholar] [CrossRef] [PubMed]
- Mally, P.V.; Agathis, N.T.; Bailey, S.M. Early term infants are at increased risk of requiring neonatal intensive care. World J. Pediatr. 2016, 12, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Sengupta, S.; Carrion, V.; Shelton, J.; Wynn, R.J.; Ryan, R.M.; Singhal, K.; Lakshminrusimha, S. Adverse neonatal outcomes associated with early-term birth. JAMA Pediatr. 2013, 167, 1053–1059. [Google Scholar] [CrossRef] [PubMed]
- Espel, E.V.; Glynn, L.M.; Sandman, C.A.; Davis, E.P. Longer gestation among children born full term influences cognitive and motor development. PLoS ONE 2014, 9, e113758. [Google Scholar] [CrossRef] [PubMed]
- Maisels, M.J.; Bhutani, V.K.; Bogen, D.; Newman, T.B.; Stark, A.R.; Watchko, J.F. Hyperbilirubinemia in the newborn infant ≥35 weeks’ gestation: An update with clarifications. Pediatrics 2009, 124, 1193–1198. [Google Scholar] [CrossRef] [PubMed]
- Bhutani, V.K.; Johnson, L.; Sivieri, E.M. Predictive ability of a predischarge hour-specific serum bilirubin for subsequent significant hyperbilirubinemia in healthy term and near-term newborns. Pediatrics 1999, 103, 6–14. [Google Scholar] [CrossRef]
- Sarici, S.U.; Ozcan, M.; Akpinar, M.; Altun, D.; Yasartekin, Y.; Koklu, E.; Serdar, M.A.; Sarici, D. Transcutaneous Bilirubin Levels and Risk of Significant Hyperbilirubinemia in Early-Term and Term Newborns. J. Obstet. Gynecol. Neonatal. Nurs. 2021, 50, 307–315. [Google Scholar] [CrossRef] [PubMed]
- Bulut, O.; Buyukkayhan, D. Early term delivery is associated with increased neonatal respiratory morbidity. Pediatr. Int. 2021, 63, 60–64. [Google Scholar] [CrossRef]
- Taylor, J.A.; Burgos, A.E.; Flaherman, V.; Chung, E.K.; Simpson, E.A.; Goyal, N.K.; Von Kohorn, I.; Dhepyasuwan, N. BORN Investigators. Utility of Decision Rules for Transcutaneous Bilirubin Measurements. Pediatrics 2016, 137, e20153032. [Google Scholar] [CrossRef]
- Tomashek, K.M.; Shapiro-Mendoza, C.K.; Davidoff, M.J.; Petrini, J.R. Differences in mortality between late-preterm and term singleton infants in the United States, 1995–2002. J Pediatr. 2007, 151, 450–456.e1. [Google Scholar] [CrossRef] [PubMed]
- Bastek, J.A.; Sammel, M.D.; Paré, E.; Srinivas, S.K.; Posencheg, M.A.; Elovitz, M.A. Adverse neonatal outcomes: Examining the risks between preterm, late preterm, and term infants. Am. J. Obstet. Gynecol. 2008, 199, 367.e1–367.e8. [Google Scholar] [CrossRef]
- Ko, H.S.; Jang, Y.R.; Yun, H.; Wie, J.; Choi, S.K.; Park, I.Y.; Shin, J.C. Late-preterm infants, early-term infants, and timing of elective deliveries; current status in a Korean medical center. J. Matern. Fetal Neonatal Med. 2019, 32, 1267–1274. [Google Scholar] [CrossRef]
- Brown, H.K.; Speechley, K.N.; Macnab, J.; Natale, R.; Campbell, M.K. Neonatal morbidity associated with late preterm and early term birth: The roles of gestational age and biological determinants of preterm birth. Int. J. Epidemiol. 2014, 43, 802–814. [Google Scholar] [CrossRef] [PubMed]
- Quigley, M.A.; Poulsen, G.; Boyle, E.; Wolke, D.; Field, D.; Alfirevic, Z.; Kurinczuk, J.J. Early term and late preterm birth are associated with poorer school performance at age 5 years: A cohort study. Arch. Dis. Child. Fetal Neonatal. Ed. 2012, 97, F167–F173. [Google Scholar] [CrossRef] [PubMed]
- Machado, L.C., Jr.; Passini, R., Jr.; Rosa, I.R.; Carvalho, H.B. Neonatal outcomes of late preterm and early term birth. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014, 179, 204–208. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Platt, R.W.; Kramer, M.S. Variation in child cognitive ability by week of gestation among healthy term births. Am. J. Epidemiol. 2010, 171, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Tsao, P.C.; Yeh, H.L.; Chang, Y.C.; Chiang, P.H.; Shiau, Y.S.; Chiang, S.H.; Soong, W.J.; Jeng, M.J.; Hsiao, K.J. Outcomes of neonatal jaundice in Taiwan. Arch. Dis. Child. 2018, 103, 927–929. [Google Scholar] [CrossRef] [PubMed]
- Leone, A.; Ersfeld, P.; Adams, M.; Schiffer, P.M.; Bucher, H.U.; Arlettaz, R. Neonatal morbidity in singleton late preterm infants compared with full-term infants. Acta Paediatr. 2012, 101, e6–e10. [Google Scholar] [CrossRef]
- Sarici, S.U.; Serdar, M.A.; Korkmaz, A.; Erdem, G.; Oran, O.; Tekinalp, G.; Yurdakök, M.; Yigit, S. Incidence, course, and prediction of hyperbilirubinemia in near-term and term newborns. Pediatrics 2004, 113, 775–780. [Google Scholar] [CrossRef] [PubMed]
- Leal, M.D.C.; Esteves-Pereira, A.P.; Nakamura-Pereira, M.; Domingues, R.M.S.M.; Dias, M.A.B.; Moreira, M.E.; Theme-Filha, M.; da Gama, S.G.N. Burden of early-term birth on adverse infant outcomes: A population-based cohort study in Brazil. BMJ Open 2017, 7, e017789. [Google Scholar] [CrossRef] [PubMed]
- Tioseco, J.A.; Aly, H.; Milner, J.; Patel, K.; El-Mohandes, A.A. Does gender affect neonatal hyperbilirubinemia in low-birth-weight infants? Pediatr. Crit. Care Med. 2005, 6, 171–174. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.Y.; Ithnin, A.; Azma, R.Z.; Othman, A.; Salvador, A.; Cheah, F.C. Glucose-6-Phosphate Dehydrogenase Deficiency and Neonatal Hyperbilirubinemia: Insights on Pathophysiology, Diagnosis, and Gene Variants in Disease Heterogeneity. Front. Pediatr. 2022, 10, 875877. [Google Scholar] [CrossRef]
- Sukla, K.K.; Tiwari, P.K.; Kumar, A.; Raman, R. Low birthweight (LBW) and neonatal hyperbilirubinemia (NNH) in an Indian cohort: Association of homocysteine, its metabolic pathway genes and micronutrients as risk factors. PLoS ONE 2013, 8, e71587. [Google Scholar] [CrossRef]
- Muchowski, K.E. Evaluation and treatment of neonatal hyperbilirubinemia. Am. Fam. Physician 2014, 89, 873–878. [Google Scholar] [PubMed]
- Bertini, G.; Dani, C.; Tronchin, M.; Rubaltelli, F.F. Is breastfeeding really favoring early neonatal jaundice? Pediatrics 2001, 107, E41. [Google Scholar] [CrossRef]
- Chang, P.F.; Lin, Y.C.; Liu, K.; Yeh, S.J.; Ni, Y.H. Identifying term breast-fed infants at risk of significant hyperbilirubinemia. Pediatr. Res. 2013, 74, 408–412. [Google Scholar] [CrossRef][Green Version]
- Daunhawer, I.; Kasser, S.; Koch, G.; Sieber, L.; Cakal, H.; Tütsch, J.; Pfister, M.; Wellmann, S.; Vogt, J.E. Enhanced early prediction of clinically relevant neonatal hyperbilirubinemia with machine learning. Pediatr. Res. 2019, 86, 122–127. [Google Scholar] [CrossRef]
- Anne, R.P.; Rahiman, E.A.; Dudeja, S.; Kumar, A. Diagnostic Accuracy of Cord Bilirubin to Predict the Need for Phototherapy in Healthy Neonates >35-Week Gestational Age: A Systematic Review and Meta-Analysis. J. Clin. Exp. Hepatol. 2023, 13, 666–681. [Google Scholar] [CrossRef]
- Bhutani, V.K.; Stark, A.R.; Lazzeroni, L.C.; Poland, R.; Gourley, G.R.; Kazmierczak, S.; Meloy, L.; Burgos, A.E.; Hall, J.Y.; Stevenson, D.K. Initial Clinical Testing Evaluation and Risk Assessment for Universal Screening for Hyperbilirubinemia Study Group. Predischarge screening for severe neonatal hyperbilirubinemia identifies infants who need phototherapy. J. Pediatr. 2013, 162, 477–482.e1. [Google Scholar] [CrossRef]
- Jain, M.; Bang, A.; Tiwari, A.; Jain, S. Prediction of significant hyperbilirubinemia in term neonates by early non-invasive bilirubin measurement. World J. Pediatr. 2017, 13, 222–227. [Google Scholar] [CrossRef]
- Kemper, A.R.; Newman, T.B.; Slaughter, J.L.; Maisels, M.J.; Watchko, J.F.; Downs, S.M.; Grout, R.W.; Bundy, D.G.; Stark, A.R.; Bogen, D.L.; et al. Clinical Practice Guideline Revision: Management of Hyperbilirubinemia in the Newborn Infant 35 or More Weeks of Gestation. Pediatrics 2022, 150, e2022058859. [Google Scholar] [CrossRef]
- Casnocha Lucanova, L.; Zibolenova, J.; Matasova, K.; Docekalova, L.; Zibolen, M. Accuracy of enhanced transcutaneous bilirubinometry according to various measurement sites. Turk. Arch. Pediatr. 2021, 56, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Khoshnoud Shariati, M.; Taslimi Taleghani, N.; Izadi, N.; Miri, A.; Taheri Tafti, R.; Abdollah Gorji, F. Which Is More Accurate: Transcutaneous Bilirubin Measurement on the Forehead or Sternum? Arch. Iran. Med. 2022, 25, 552–556. [Google Scholar] [CrossRef] [PubMed]
- Kawamoto, K.; Kukhareva, P.; Shakib, J.H.; Kramer, H.; Rodriguez, S.; Warner, P.B.; Shields, D.; Weir, C.; Del Fiol, G.; Taft, T.; et al. Association of an electronic health record add-on App for neonatal bilirubin management with physician efficiency and care quality. JAMA Netw. Open 2019, 2, e1915343. [Google Scholar] [CrossRef] [PubMed]

| Early Term (n = 187) | Full-Term (n = 169) | p * | |
|---|---|---|---|
| GA a (weeks) | 38.13 ± 0.53 | 39.59 ± 0.42 | <0.05 |
| Sex | 0.83 | ||
| Boy | 93 (49.7%) | 82 (48.5%) | |
| Girl | 94 (50.3%) | 87 (51.5%) | |
| Birth weight | 3043.72 ± 327.78 | 3143.99 ± 305.71 | <0.05 |
| Mode of delivery | <0.05 | ||
| Vaginal delivery | 111 (59.4%) | 154 (91.1%) | |
| Cesarean section | 76 (40.6%) | 15 (8.9%) | |
| Feeding | 0.52 | ||
| Exclusive breastfeeding | 68 (36.4%) | 67 (39.6%) | |
| Non-exclusivebreastfeeding | 119 (63.6%) | 102 (60.4%) | |
| Mothers requested | 90 (48.1%) | 85 (50.3%) | |
| Crystalluria | 11 (5.9%) | 9 (5.3%) | |
| Weight loss exceeding 10% of the initial birth weight | 13 (6.9%) | 6 (3.6%) | |
| Currently taking medications not recommended for breastfeeding | 5 (2.7%) | 2 (1.2%) | |
| G6PD b deficiency | <0.05 | ||
| Yes | 4 (2.1%) | 12 (7.1%) | |
| No | 183 (97.9%) | 157 (92.9%) | |
| TcB c level (<24 h) | 5.04 ± 1.89 | 4.90 ± 1.92 | 0.49 |
| TcB c level (24–48 h) | 8.80 ± 2.04 | 8.89 ± 2.06 | 0.70 |
| Small for gestational age | 0.13 | ||
| Yes | 29 (15.5%) | 17 (10.1%) | |
| No | 158 (84.5%) | 152 (89.9%) | |
| Received phototherapy | <0.05 | ||
| Yes | 59 (31.6%) | 36 (21.3%) | |
| No | 128 (68.4%) | 133 (78.7%) | |
| Maternal diabetes | 0.09 | ||
| Yes | 19 (10.2%) | 9 (5.3%) | |
| No | 168 (89.8) | 160 (94.7) | |
| Caput succedaneum or cephalohematoma | 0.34 | ||
| Yes | 7 (3.7%) | 10 (5.9%) | |
| No | 180 (96.3%) | 159 (94.1%) |
| Non-Phototherapy (n = 261) | Phototherapy (n = 95) | p * | |
|---|---|---|---|
| GA a (weeks) | 38.88 ± 0.87 | 38.68 ± 0.87 | 0.06 |
| GA a | <0.05 | ||
| ≤38 and 6/7 weeks (early term) | 128 (49.0%) | 59 (62.1%) | |
| ≥39 and 0/7 weeks (full term) | 133 (51.0%) | 36 (37.9%) | |
| Sex | 0.40 | ||
| Boy | 132 (50.6%) | 43 (45.3%) | |
| Girl | 129 (49.4%) | 52 (54.7%) | |
| Birth weight | 3096.53 ± 325.54 | 3077.00 ± 309.35 | 0.60 |
| Mode of delivery | 0.84 | ||
| Vaginal delivery | 195 (74.7%) | 70 (73.7%) | |
| Cesarean section | 66 (25.3%) | 25 (26.3%) | |
| Feeding type | 0.14 | ||
| Exclusive breastfeeding | 105 (40.2%) | 30 (31.6%) | |
| Non-exclusive breastfeeding | 156 (59.8%) | 65 (68.4%) | |
| Mothers requested | 123 (47.1%) | 52 (54.7%) | |
| Crystalluria | 16 (6.1%) | 4 (4.2%) | |
| Weight loss exceeding 10% of the initial birth weight | 13 (5.1%) | 6 (6.3%) | |
| Currently taking medications not recommended for breastfeeding | 4 (1.5%) | 3 (3.2%) | |
| G6PD b deficiency | <0.05 | ||
| Yes | 8 (3.1%) | 8 (8.4%) | |
| No | 253 (96.9%) | 87 (91.6%) | |
| Small for gestational age | 0.42 | ||
| Yes | 36 (13.8%) | 10 (10.5%) | |
| No | 225 (86.2%) | 85 (89.5%) | |
| TcB c level (<24 h) | 4.67 ± 1.79 | 5.79 ± 1.98 | <0.05 |
| TcB c level (24–48 h) | 8.30 ± 1.83 | 10.33 ± 1.87 | <0.05 |
| Maternal diabetes | 0.83 | ||
| Yes | 21 (8.0%) | 7 (7.4%) | |
| No | 240 (92%) | 88 (92.6%) | |
| Caput succedaneum or cephalohematoma | 0.80 | ||
| Yes | 12 (4.6%) | 5 (5.3%) | |
| No | 249 (95.4%) | 90 (94.7%) |
| Crude | Adjusted e | |||
|---|---|---|---|---|
| Variables | B (95% CI) | p * | B (95% CI) | p * |
| GA a (≤38 and 6/7 weeks vs. ≥39 and 0/7 weeks) | 1.70 (1.05–2.75) | <0.05 | 2.15 (1.21–3.80) | <0.05 |
| Birth weight | 1.00 (0.99–1.00) | 0.61 | 1.00 (0.99–1.00) | 0.27 |
| Gender | 0.81 (0.50–1.30) | 0.38 | 0.81 (0.46–1.43) | 0.46 |
| Feeding type c | 0.69 (0.42–1.13) | 0.14 | 0.66 (0.37–1.18) | 0.15 |
| G6PD b deficiency | 0.34 (0.13–0.94) | <0.05 | 0.56 (0.17–1.80) | 0.33 |
| TcB d level (<24 h) | 1.37 (1.20–1.57) | <0.05 | 0.92 (0.77–1.10) | 0.37 |
| TcB d level (24–48 h) | 1.89 (1.60–2.23) | <0.05 | 2.04 (1.65–2.52) | <0.05 |
| Maternal diabetes | 0.91 (0.37–2.21) | 0.83 | 1.06 (0.29–3.93) | 0.93 |
| Caput succedaneum or cephalohematoma | 1.15 (0.40–3.36) | 0.80 | 0.86 (0.32–2.33) | 0.77 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tan, T.-J.; Chen, W.-J.; Lin, W.-C.; Yang, M.-C.; Tsai, C.-C.; Yang, Y.-N.; Yang, S.-N.; Liu, H.-K. Early-Term Neonates Demonstrate a Higher Likelihood of Requiring Phototherapy Compared to Those Born Full-Term. Children 2023, 10, 1819. https://doi.org/10.3390/children10111819
Tan T-J, Chen W-J, Lin W-C, Yang M-C, Tsai C-C, Yang Y-N, Yang S-N, Liu H-K. Early-Term Neonates Demonstrate a Higher Likelihood of Requiring Phototherapy Compared to Those Born Full-Term. Children. 2023; 10(11):1819. https://doi.org/10.3390/children10111819
Chicago/Turabian StyleTan, Teck-Jin, Wan-Ju Chen, Wan-Chun Lin, Ming-Chun Yang, Ching-Chung Tsai, Yung-Ning Yang, San-Nan Yang, and Hsien-Kuan Liu. 2023. "Early-Term Neonates Demonstrate a Higher Likelihood of Requiring Phototherapy Compared to Those Born Full-Term" Children 10, no. 11: 1819. https://doi.org/10.3390/children10111819
APA StyleTan, T.-J., Chen, W.-J., Lin, W.-C., Yang, M.-C., Tsai, C.-C., Yang, Y.-N., Yang, S.-N., & Liu, H.-K. (2023). Early-Term Neonates Demonstrate a Higher Likelihood of Requiring Phototherapy Compared to Those Born Full-Term. Children, 10(11), 1819. https://doi.org/10.3390/children10111819







