The Role of Mannose-Binding Lectin and Inflammatory Markers in Establishing the Course and Prognosis of Community-Acquired Pneumonia in Children
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Blood Sampling
2.3. Biomarker Analysis
2.4. Biomarker Reference
- <2 ng/mL: Systemic infection is possible, but unlikely;
- 2–10 ng/mL: Systemic infection is likely;
- ≥10 ng/mL: High likelihood of severe bacterial sepsis or septic shock.
2.5. Classification
2.6. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Cohort Analysis Based on CRP Levels
3.3. Cohort Analysis Based on PCT Levels
3.4. Cohort Analysis Based on MBL Levels
4. Discussion
5. Limitations of This Study
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wilmott, R.; Bush, A.; Deterding, R.; Ratjen, F.; Sly, P.; Zar, H.; Li, A.P. Disorders of the Respiratory Tract in Children, 9th ed.; Elsevier: Amsterdam, The Netherlands, 2019; pp. 1596–1644. [Google Scholar]
- Ionescu, M.D.; Popescu, N.A.; Stănescu, D.; Enculescu, A.; Bălgrădean, M.; Căpitănescu, G.M.; Bumbăcea, D. The Challenging Diagnosis of Interstitial Lung Disease in Children—One Case Report and Literature Review. J. Clin. Med. 2022, 11, 6736. [Google Scholar] [CrossRef] [PubMed]
- Tuomanen, E.; Kaplan, S.; Olarte, L.C. Pneumococcal Pneumonia in Children; UpToDate: Waltham, MA, USA, 2017. [Google Scholar]
- Ionescu, M.D.; Balgradean, M.; Cirstoveanu, C.G.; Balgradean, I.; Popa, L.I.; Pavelescu, C.; Capitanescu, A.; Berghea, E.C.; Filip, C. Myopericarditis Associated with COVID-19 in a Pediatric Patient with Kidney Failure Receiving Hemodialysis. Pathogens 2021, 10, 486. [Google Scholar] [CrossRef] [PubMed]
- Pomerantz, W.J.; Weiss, S.L. Systemic Inflammatory Response Syndrome (SIRS) and Sepsis in Children: Definitions, Epidemiology, Clinical Manifestations, and Diagnosis—UpToDate. 2022. Available online: https://www.uptodate.com/contents/systemic-inflammatory-response-syndrome-sirs-and-sepsis-in-children-definitions-epidemiology-clinical-manifestations-and-diagnosis (accessed on 26 June 2023).
- Uwaezuoke, S.N.; Ayuk, A.C. Prognostic scores and biomarkers for pediatric community-acquired pneumonia: How far have we come? Pediatr. Health Med. Ther. 2017, 8, 9–18. [Google Scholar] [CrossRef]
- Atkinson, A.J., Jr.; Colburn, W.A.; DeGruttola, V.G.; DeMets, D.L.; Downing, G.J.; Hoth, D.F.; Oates, J.A.; Peck, C.C.; Schooley, R.T.; Spilker, B.A.; et al. Biomarkers and surrogate endpoints: Preferred definitions and conceptual framework. Clin. Pharmacol. Ther. 2001, 69, 89–95. [Google Scholar]
- Dalton, W.S.; Friend, S.H. Cancer Biomarkers—An Invitation to the Table. Science 2006, 312, 1165–1168. [Google Scholar] [CrossRef]
- Bucher, H.C.; Guyatt, G.H.; Cook, D.J.; Holbrook, A.; McAlister, F.A.; Evidence-Based Medicine Working Group. Users’ Guides to the Medical Literature: XIX. Applying Clinical Trial Results A. How to Use an Article Measuring the Effect of an Intervention on Surrogate End Points. JAMA 1999, 282, 771–778. [Google Scholar] [CrossRef] [PubMed]
- Marshall, J.C.; Reinhart, K. Biomarkers of sepsis. Crit. Care Med. 2009, 37, 2290–2298. [Google Scholar] [CrossRef]
- O’Brien, K.L.; Wolfson, L.J.; Watt, J.P.; Henkle, E.; Deloria-Knoll, M.; McCall, N.; Lee, E.; Mulholland, K.; Levine, O.S.; Cherian, T.; et al. Burden of disease caused by Streptococcus pneumoniae in children younger than 5 years: Global estimates. Lancet 2009, 374, 893–902. [Google Scholar] [CrossRef]
- Hoffmann, J.A.; Kafatos, F.C.; Janeway, C.A.; Ezekowitz, R.A.B. Phylogenetic Perspectives in Innate Immunity. Science 1999, 284, 1313–1318. [Google Scholar] [CrossRef]
- Turner, M.W. Mannose-binding lectin: The pluripotent molecule of the innate immune system. Immunol. Today 1996, 17, 532–540. [Google Scholar] [CrossRef]
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13, S31. [Google Scholar] [CrossRef] [PubMed]
- Langley, J.M.; Bradley, J.S. Defining pneumonia in critically ill infants and children. Pediatr. Crit. Care Med. 2005, 6, S9–S13. [Google Scholar] [CrossRef] [PubMed]
- Laborator Synevo. Referintele Specifice Tehnologiei de Lucru Utilizate; Laborator Synevo: Bucharest, Romania, 2010. [Google Scholar]
- Beberashvili, I.; Omar, M.A.; Nizri, E.; Stav, K.; Efrati, S. Combined use of CRP with neutrophil-to-lymphocyte ratio in differentiating between infectious and noninfectious inammation in hemodialysis patients. Sci. Rep. 2023. epub ahead pof print. [Google Scholar] [CrossRef]
- Koozi, H.; Lengquist, M.; Frigyesi, A. C-reactive protein as a prognostic factor in intensive care admissions for sepsis: A Swedish multicenter study. J. Crit. Care 2020, 56, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Devran, Ö.; Karakurt, Z.; Adıgüzel, N.; Güngör, G.; Moçin, Ö.Y.; Balcı, M.K.; Çelik, E.; Saltürk, C.; Takır, H.B.; Kargın, F.; et al. C-reactive protein as a predictor of mortality in patients affected with severe sepsis in intensive care unit. Multidiscip. Respir. Med. 2012, 7, 47. [Google Scholar] [CrossRef]
- Chalmers, J.D.; Singanayagam, A.; Hill, A.T. C-Reactive Protein Is an Independent Predictor of Severity in Community-acquired Pneumonia. Am. J. Med. 2008, 121, 219–225. [Google Scholar] [CrossRef]
- Jensch, A.; Mahla, E.; Toller, W.; Herrmann, M.; Mangge, H. Procalcitonin measurement by DiazymeTM immunturbidimetric and Elecsys BRAHMSTM PCT assay on a Roche COBAS modular analyzer. Clin. Chem. Lab. Med. 2021, 59, E362–E366. [Google Scholar] [CrossRef]
- Rogić, D.; Juroš, G.F.; Petrik, J.; Vrančić, A.L. Advances and Pitfalls in Using Laboratory Biomarkers for the Diagnosis and Management of Sepsis. EJIFCC 2017, 28, 114–121. [Google Scholar]
- Pneumonia|CDC. Available online: https://www.cdc.gov/pneumonia/index.html (accessed on 26 June 2023).
- Bruel, A.V.D.; Thompson, M.J.; Haj-Hassan, T.; Stevens, R.; Moll, H.; Lakhanpaul, M.; Mant, D. Diagnostic value of laboratory tests in identifying serious infections in febrile children: Systematic review. BMJ 2011, 342, d3082. [Google Scholar] [CrossRef]
- Kaya, Z.; Küçükcongar, A.; Vurallı, D.; Emeksiz, H.C.; Gürsel, T. Leukocyte Populations and C-Reactive Protein as Predictors of Bacterial Infections in Febrile Outpatient Children. [Polikliniğe Başvuran Ateşli Çocuklarda Bakteriyel Enfeksiyonu Belirlemek için CRP Düzeyi ve Lökosit Popülasyonu]. Turk. J.Haematol. Off. J. Turk. Soc. Haematol. 2014, 31, 49–55. [Google Scholar] [CrossRef]
- Sarsu, S.B.; Sarac, F. Diagnostic Value of White Blood Cell and C-Reactive Protein in Pediatric Appendicitis. BioMed Res. Int. 2016, 2016, 6508619. [Google Scholar] [CrossRef][Green Version]
- Pääkkönen, M.; Kallio, M.J.T.; Kallio, P.E.; Peltola, H. Sensitivity of erythrocyte sedimentation rate and C-reactive protein in childhood bone and joint infections. Clin. Orthop. Relat. Res. 2010, 468, 861–866. [Google Scholar] [CrossRef] [PubMed]
- Francesco, D.; Erwin, M. Proteins: Laboratory Testing and Clinical Use; DiaSys Diagnostic Systems GmbH: Holzheim, Germany, 2005; p. 564. [Google Scholar]
- Brunkhorst, F.M.; Wegscheider, K.; Forycki, Z.F.; Brunkhorst, R. Procalcitonin for early diagnosis and differentiation of SIRS, sepsis, severe sepsis, and septic shock. Intensive Care Med. 2000, 26, S148–S152. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.-P.; Xu, X.-J.; Liao, C.; Zhao, N.; Chen, Y.-Y.; Song, H.; Xu, W.-Q.; Liang, J.; Shen, D.-Y.; Zhang, J.-Y.; et al. The predictive utility of cytokines, procalcitonin and C-reactive protein among febrile pediatric hematology and oncology patients with severe sepsis or septic shock. Pediatr. Hematol. Oncol. 2023; epub ahead of print. [Google Scholar] [CrossRef]
- Florin, T.A.; Ambroggio, L.; Brokamp, C.; Zhang, Y.; Rattan, M.; Crotty, E.; Belsky, M.A.; Krueger, S.; Epperson, T.N.; Kachelmeyer, A.; et al. Biomarkers and Disease Severity in Children with Community-Acquired Pneumonia. Pediatrics 2020, 145, e20193728. [Google Scholar] [CrossRef]
- Nargis, W.; Ibrahim, M.; Ahamed, B. Procalcitonin versus C-reactive protein: Usefulness as biomarker of sepsis in ICU patient. Int. J. Crit. Illn. Inj. Sci. 2014, 4, 195. [Google Scholar] [CrossRef]
- Luzzani, A.; Polati, E.; Dorizzi, R.; Rungatscher, A.; Pavan, R.; Merlini, A. Comparison of procalcitonin and C-reactive protein as markers of sepsis. Crit. Care Med. 2003, 31, 1737–1741. [Google Scholar] [CrossRef]
- Samsudin, I.; Vasikaran, S.D. Clinical Utility and Measurement of Procalcitonin. Clin. Biochem. Rev. 2017, 38, 59. [Google Scholar]
- Gentilotti, E.; De Nardo, P.; Cremonini, E.; Górska, A.; Mazzaferri, F.; Canziani, L.M.; Hellou, M.M.; Olchowski, Y.; Poran, I.; Leeflang, M.; et al. Diagnostic accuracy of point-of-care tests in acute community-acquired lower respiratory tract infections. A systematic review and meta-analysis. Clin. Microbiol. Infect. 2022, 28, 13–22. [Google Scholar] [CrossRef]
- Selberg, O.; Hecker, H.; Martin, M.; Klos, A.; Bautsch, W.; Köhl, J. Discrimination of sepsis and systemic inflammatory response syndrome by determination of circulating plasma concentrations of procalcitonin, protein complement 3a, and interleukin-6. Crit. Care Med. 2000, 28, 2793–2798. [Google Scholar] [CrossRef]
- Suprin, E.; Camus, C.; Gacouin, A.; Le Tulzo, Y.; Lavoue, S.; Feuillu, A.; Thomas, R. Procalcitonin: A valuable indicator of infection in a medical ICU? Intensive Care Med. 2000, 26, 1232–1238. [Google Scholar] [CrossRef] [PubMed]
- Müller, B.; Becker, K.L.; Schächinger, H.; Rickenbacher, P.R.; Huber, P.R.; Zimmerli, W.; Ritz, R. Calcitonin precursors are reliable markers of sepsis in a medical intensive care unit. Crit. Care Med. 2000, 28, 977–983. [Google Scholar] [CrossRef] [PubMed]
- Guven, H.; Altintop, L.; Baydin, A.; Esen, S.; Aygun, D.; Hokelek, M.; Doganay, Z.; Bek, Y. Diagnostic value of procalcitonin levels as an early indicator of sepsis. Am. J. Emerg. Med. 2002, 20, 202–206. [Google Scholar] [CrossRef]
- BalcI, C.; Sungurtekin, H.; Gürses, E.; Sungurtekin, U.; Kaptanoglu, B. Usefulness of procalcitonin for diagnosis of sepsis in the intensive care unit. Crit. Care 2003, 7, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Vallès, X.; Roca, A.; Lozano, F.; Morais, L.; Suárez, B.; Casals, F.; Mandomando, I.; Sigaúque, B.; Nhalungo, D.; Esquinas, C.; et al. Serotype-specific pneumococcal disease may be influenced by mannose-binding lectin deficiency. Eur. Respir. J. 2010, 36, 856–863. [Google Scholar] [CrossRef]
- Vuononvirta, J.; Toivonen, L.; Gröndahl-Yli-Hannuksela, K.; Barkoff, A.-M.; Lindholm, L.; Mertsola, J.; Peltola, V.; He, Q. Nasopharyngeal Bacterial Colonization and Gene Polymorphisms of Mannose-Binding Lectin and Toll-Like Receptors 2 and 4 in Infants. PLoS ONE 2011, 6, e26198. [Google Scholar] [CrossRef] [PubMed]
- Koch, A.; Melbye, M.; Sørensen, P.; Homøe, P.; Madsen, H.O.; Mølbak, K.; Hansen, C.H.; Andersen, L.H.; Hahn, G.W.; Garred, P. Acute respiratory tract infections and mannose-binding lectin insufficiency during early childhood. JAMA 2001, 285, 1316–1321. [Google Scholar] [CrossRef]
- van Kessel, D.A.; Hoffman, T.W.; van Velzen-Blad, H.; Zanen, P.; Rijkers, G.T.; Grutters, J.C. Response to pneumococcal vaccination in mannose-binding lectin-deficient adults with recurrent respiratory tract infections. Clin. Exp. Immunol. 2014, 177, 272–279. [Google Scholar] [CrossRef]
- García-Laorden, M.I.; de Castro, F.R.; Solé-Violán, J.; Payeras, A.; Briones, M.L.; Borderías, L.; Aspa, J.; Blanquer, J.; Rajas, O.; Marcos-Ramos, J.A.; et al. The role of mannose-binding lectin in pneumococcal infection. Eur. Respir. J. 2013, 41, 131–139. [Google Scholar] [CrossRef]
- Beltrame, M.H.; Boldt, A.B.; Catarino, S.J.; Mendes, H.C.; Boschmann, S.E.; Goeldner, I.; Messias-Reason, I. MBL-associated serine proteases (MASPs) and infectious diseases. Mol. Immunol. 2015, 67, 85–100. [Google Scholar] [CrossRef]
- Charchaflieh, J.; Wei, J.; Labaze, G.; Hou, Y.J.; Babarsh, B.; Stutz, H.; Lee, H.; Worah, S.; Zhang, M. The role of complement system in septic shock. Clin. Dev. Immunol. 2012, 2012, 407324. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.-H.; Li, Q.; Zhang, P.; Su, Y.; Zhang, X.-R.; Sun, Q.; Ulehlova, J.; Slavik, L.; Kucerova, J.; Krcova, V.; et al. Serum Mannose-Binding Lectin and C-Reactive Protein Are Potential Biomarkers for Patients with Community-Acquired Pneumonia. Genet. Test. Mol. Biomark. 2014, 18, 630–635. [Google Scholar] [CrossRef] [PubMed]
- Dima, M.; Iacob, D.; Duta, C.; Pantea, S.; Marginean, O.; Bernad, E.; Craina, M.; Boglut, A.; Petre, I. Association Between Mannose-binding Lectin and Serum Parameters of Neonatal Sepsis. Rev. Chim. 2016, 67, 557. [Google Scholar]
- Berghea, E.C.; Balgradean, M.; Pavelescu, C.; Cirstoveanu, C.G.; Toma, C.L.; Ionescu, M.D.; Bumbacea, R.S. Clinical Experience with Anti-IgE Monoclonal Antibody (Omalizumab) in Pediatric Severe Allergic Asthma—A Romanian Perspective. Children 2021, 8, 1141. [Google Scholar] [CrossRef] [PubMed]
- Leyenaar, J.K.M.; Lagu, T.; Shieh, M.-S.; Pekow, P.S.; Lindenauer, P.K.M. Management and Outcomes of Pneumonia Among Children with Complex Chronic Conditions. Pediatr. Infect. Dis. J. 2014, 33, 907–911. [Google Scholar] [CrossRef]
- Filip, C.; Cirstoveanu, C.; Bizubac, M.; Berghea, E.C.; Căpitănescu, A.; Bălgrădean, M.; Pavelescu, C.; Nicolescu, A.; Ionescu, M.D. Pulse Wave Velocity as a Marker of Vascular Dysfunction and Its Correlation with Cardiac Disease in Children with End-Stage Renal Disease (ESRD). Diagnostics 2021, 12, 71. [Google Scholar] [CrossRef] [PubMed]






| CAP Is an Acute, Symptomatic Infection of the Pulmonary Parenchyma in a Child Who Has Not Been Hospitalized in a Healthcare Facility for ≤14 Days before the Onset of Symptoms. The Diagnosis Requires Two Clinical Findings Plus Fever and Tachypnoea, with Laboratory and Radiographic Confirmation. |
|---|
| Clinical findings (≥two of the following) |
| -Cough |
| -New onset of lower respiratory tract secretions, change in character of secretions, or increase in the quantity or suctioning requirements |
| -Auscultatory findings of consolidation (rales, bronchial breath sounds, egophony, decreased breath sounds) |
| -Dyspnoea |
| Vital signs (mandatory) |
| -Fever defined by age group |
| -Tachypnoea defined by age group |
| Laboratory findings |
| -White blood cell count (WBC) ≥15,000 or ≤4000 per cubic millimeter |
| Radiographic findings |
| -Chest X-ray revealing the presence of new infiltrate(s) consistent with infection (interstitial, bronchial, alveolar), consolidation, cavitation, abscess, or pneumatoceles |
| Parameters | Distribution |
|---|---|
| Male (%) | 101 (49.5%) |
| Age (months)—median [min, max] | 42 [4, 212] |
| Onset of fever (days)—median [min, max] | 3 [1, 14] |
| Onset of cough (days)—median [min, max] | 5 [1, 21] |
| Vaccination status—n (%) | 188 (92.15%) |
| Fever (degrees Celsius)—median [min, max] | 39 [37, 41] |
| Altered mental status—n (%) | 5 (2.45%) |
| SpO2%—median [min, max] | 96% [60%, 99%] |
| Respiratory rate (breaths per minute)—median [min, max] | 30 [20, 75] |
| Apnea—n (%) | 3 (1.47%) |
| Grunting—n (%) | 23 (11.27%) |
| Thoracic pain—n (%) | 17 (8.33%) |
| Cyanosis—n (%) | 8 (3.92%) |
| Tachycardia—(%) | 77 (37.74%) |
| Capillary refill ≥ 3 s—n (%) | 3 (1.47%) |
| Respiratory failure—n (%) | 42 (20.58%) |
| Local complications—n (%) | 57 (27.94%) |
| 49 (24.01%) |
| 7 (3.43%) |
| 1 (0.49%) |
| Systemic complications—n (%) | 96 (47.05%) |
| 35 (17.15%) |
| 49 (24.01%) |
| 12 (5.88%) |
| Antibiotic treatment (days)—median [min, max] | 7 [3, 35] |
| Oxygen therapy—n (%) | 41 (20.09%) |
| Oxygen therapy (days required)—median [min, max] | 2 [1, 7] |
| Surgical intervention (%) | 16 (7.84%) |
| 7 (3.43%) |
| 4 (1.96%) |
| 5 (2.45%) |
| Admission to the ICU—n (%) | 12 (5.88%) |
| Duration of ICU stay (days)—median [min, max] | 1 [1, 14] |
| Death—n (%) | 3 (1.47%) |
| Duration of hospitalization (days)—median [min, max] | 7 [3, 35] |
| Paraclinical Parameters | Distribution |
|---|---|
| MBL (ng/mL)—median [min, max] | 1580 [50, 4150] |
| 37 (18, 13%) |
| 167 (81, 86%) |
| White blood cells (cells/µL)—median [min, max] | 17,615 [1300, 57,980] |
| 77% [15, 92] |
| 14% [2, 55] |
| Platelets (cells/µL)—median [min, max] | 334,000 [10,000, 1, 100,000] |
| CRP (mg/L)—median [min, max] | 100.5 [1.5, 481] |
| 95 (46.56%) |
| 109 (53.41%) |
| PCT (ng/mL)—median [min, msax] | 0.485 [0.01, 40] |
| 141 (69.11%) |
| 29 (14.21%) |
| 34 (16.6%) |
| Creatinine (mg/dl)—median [min, max] | 0.3 [0.1, 5.2] |
| Urea (mmol/L)—median [min, max] | 2.34 [0.83, 9.96] |
| Elevated liver enzymes (%) n (%) | 9 (4.41%) |
| APTT (seconds)—median [min, max] | 24 [12, 64] |
| Imaging findings (X-ray/Thoracic ultrasound/CT)—n (%) | |
| 146 (71.56%) |
| 18 (8.82%) |
| 7 (3.43%) |
| 49 (24.01%) |
| Clinical Feature | Group A CRP < 100 mg/L; N = 95 | Group B CRP ≥ 100 mg/L; N = 109 | p Value * |
|---|---|---|---|
| Peripheral oxygen saturation %—median [min, max] | 97% [65%, 99%] | 95% [60%, 99%] | 0.00128 |
| Acute respiratory failure—n (%) | 7 (7.36%) | 35 (32.11%) | 0.00076 |
| Incidence of local complications—n (%) | 17 (17.9%) | 40 (36.7%) | 0.002832 |
| Pleurisy—n (%) | 16 (16.84%) | 33 (30.27%) | 0.025072 |
| Lung abscess—n (%) | 1 (1.05%) | 6 (5.5%) | 0.081431 |
| Necrotizing pneumonia—n (%) | 0 (0%) | 1 (0.9%) | 1 |
| Incidence of systemic complications—n (%) | 10 (10.5%) | 86 (78.9%) | 0.00001 |
| SIRS—n (%) | 6 (6.31%) | 29 (26.6%) | 0.000126 |
| Sepsis—n (%) | 3 (3.15%) | 46 (42.2%) | 0.00001 |
| Septic shock—n (%) | 1 (1.05%) | 11 (10.09%) | 0.0062 |
| Duration of antibiotic therapy (days)—median [min, max] | 7 [3, 25] | 10 [4, 35] | 0.00001 |
| Combination of antibiotics—median [min, max] | 1 [1, 3] | 2 [1, 4] | 0.00001 |
| Oxygen therapy—n (%) | 6 (6.31%) | 35 (32.11%) | 0.00001 |
| Duration of oxygen therapy (days)—median [min, max] | 0 [0, 3] | 0 [0, 7] | 0.00128 |
| Surgical intervention—n (%) | 2 (2.1%) | 14 (12.84%) | 0.00443 |
| Admission to the ICU—n (%) | 2 (2.1%) | 10 (9.17%) | 0.032317 |
| Duration of ICU stay (days)—median [min, max] | 0 [0, 10] | 0 [0, 14] | 0.00001 |
| Death—n (%) | 0 (0%) | 3 (2.75%) | 0.2499 |
| Duration of hospitalization (days)—median [min, max] | 7 [3, 25] | 10 [4, 35] | 0.00001 |
| Parameter | Group X PCT < 2 ng/mL N = 141 | Group Y 2 ng/mL < PCT< 10 ng/mL N = 29 | Group Z PCT ≥ 10 ng/mL N = 34 | p Value * |
|---|---|---|---|---|
| Peripheral oxygen saturation %—median [min, max] | 97 [60, 99] | 95 [77, 99] | 91 [65, 98] | 0.00001 |
| Acute respiratory failure—n (%) | 15 (10.63%) | 6 (20.69%) | 21 (61.76%) | 0.00001 |
| Incidence of local complications—n (%) | 28 (19.58%) | 12 (41.37%) | 17 (50%) | 0.000455 |
| Pleurisy—n (%) | 26 (18.43%) | 11 (37.93%) | 12 (35.29%) | 0.026516 |
| Abscess—n (%) | 1 (0.7%) | 1 (3.44%) | 5 (14.7%) | 0.00095 |
| Necrotizing pneumonia—n (%) | 1 (0.7%) | 0 (0%) | 0 (0%) | 1 |
| Incidence of systemic complications—n (%) | 34 (24.11%) | 28 (96.55%) | 34 (100%) | 0.00001 |
| SIRS—n (%) | 21 (14.89%) | 12 (41.37%) | 2 (5.88%) | 0.000426 |
| Sepsis—n (%) | 13 (9.21%) | 16 (55.17%) | 20 (58.82%) | 0.00001 |
| Septic shock—n (%) | 0% (0%) | 0% (0%) | 12 (35.29%) | 0.00001 |
| Duration of antibiotic treatment (days)—median [min, max] | 7 [3, 30] | 10 [5, 26] | 14 [7, 35] | 0.00001 |
| Combination of antibiotics | 1 [1, 4] | 2 [1, 4] | 2 [2, 4] | 0.00001 |
| Oxygen therapy—n (%) | 14 (9.92%) | 6 (20.69%) | 21 (61.76%) | 0.00001 |
| Duration of oxygen therapy (days)—median [min, max] | 0 [0, 7] | 0 [0, 4] | 1 [0, 5] | 0.00001 |
| Surgical intervention—n (%) | 3 (2.12%) | 3 (10.34%) | 10 (29.41%) | 0.00001 |
| Admission to the ICU—n (%) | 1 (0.7%) | 1 (3.44%) | 10 (29.41%) | 0.00001 |
| Duration of ICU stay (days)—median [min, max] | 0 [0, 1] | 0 [0, 2] | 0 [0, 14] | 0.07056 |
| Death—n (%) | 1 (0.7%) | 0 (0%) | 2 (5.88%) | 0.13 |
| Duration of hospitalization (days)—median [min, max] | 7 [3, 30] | 10 [0, 26] | 14 [7, 35] | 0.00001 |
| Parameter | Group α MBL < 450 ng/mL; N = 37 | Group β MBL ≥ 450 ng/mL; N = 167 | p Value * |
|---|---|---|---|
| Peripheral oxygen saturation %—median [min, max] | 92 [60, 98] | 97 [72, 99] | 0.00008 |
| Acute respiratory failure—n (%) | 21 (56.75%) | 20 (11.97%) | 0.00001 |
| Incidence of local complications—n (%) | 18 (48.64%) | 39 (23.35%) | 0.02 |
| Pleurisy—n (%) | 13 (35.13%) | 36 (21.55%) | 0.080246 |
| Abscess—n (%) | 5 (13.51%) | 2 (1.19%) | 0.000196 |
| Necrotizing pneumonia—n (%) | 0 (0%) | 1 (0.59%) | 1 |
| Incidence of systemic complications—n (%) | 31 (83.78%) | 65 (38.92%) | 0.00001 |
| SIRS—n (%) | 5 (13.51%) | 30 (17.96%) | 0.515888 |
| Sepsis—n (%) | 23 (62.16%) | 34 (20.35%) | 0.00001 |
| Septic shock—n (%) | 3 (8.1%) | 1 (0.59%) | 0.002875 |
| Duration of antibiotic therapy (days)—median [min, max] | 14 [7, 35] | 7 [3, 10] | 0.00001 |
| Combination of antibiotics—median [min, max] | 2 [1, 4] | 1 [1, 4] | 0.00001 |
| Oxygen therapy—n (%) | 19 (51.35%) | 22 (13.17%) | 0.00001 |
| Duration of oxygen therapy (days)—median [min, max] | 3 [1, 7] | 2 [1, 5] | 0.00001 |
| Surgical intervention—n (%) | 9 (24.32%) | 7 (4.19%) | 0.000038 |
| Admission to the ICU—n (%) | 8 (21.62%) | 4 (2.39%) | 0.00001 |
| Duration of ICU stay (days)—median [min, max] | 14 [7, 35] | 0 [0, 5] | 0.00001 |
| Death—n (%) | 2 (5.4%) | 1 (0.59%) | 0.028 |
| Duration of hospitalization (days)—median [min, max] | 14 [7, 35] | 7 [3, 30] | 0.00001 |
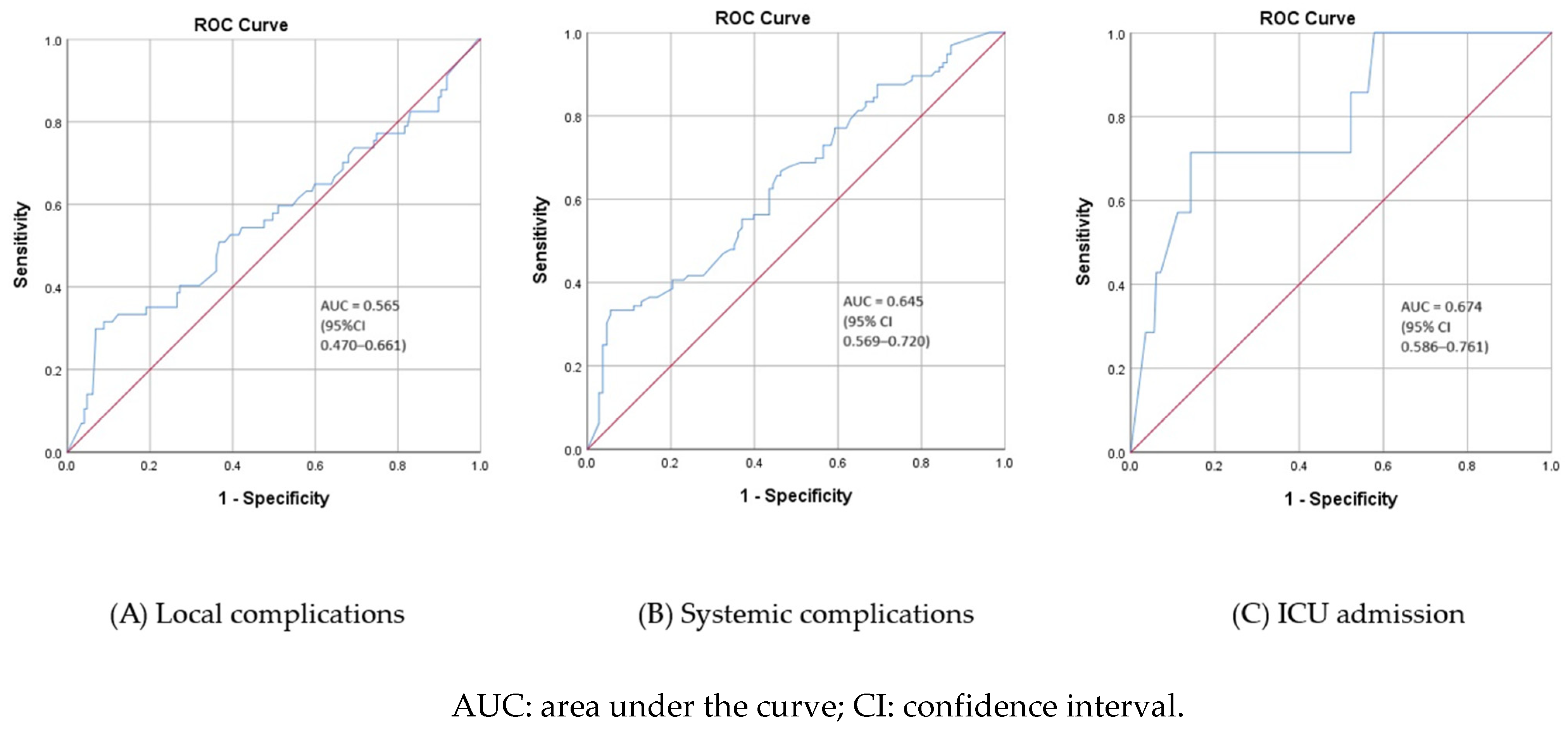
| Local Complications | Systemic Complications | ICU Admission | |||||||
|---|---|---|---|---|---|---|---|---|---|
| CRP (mg/L) | PCT (ng/mL) | MBL (ng/mL) | CRP (mg/L) | PCT (ng/mL) | MBL (ng/mL) | CRP (mg/L) | PCT (ng/mL) | MBL (ng/mL) | |
| Cutoff value | 139 | 2.7 | 272 | 116 | 0.5 | 479 | 154 | 7.7 | 388 |
| Sensitivity (%) | 61% | 51% | 30% | 83% | 90% | 33% | 75% | 75% | 71% |
| Specificity (%) | 74% | 78% | 32% | 90% | 87% | 95% | 73% | 83% | 86% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taraș, R.; Mahler, B.; Bălgrădean, M.; Derewicz, D.; Lazăr, M.I.; Vidlescu, R.; Berghea, F. The Role of Mannose-Binding Lectin and Inflammatory Markers in Establishing the Course and Prognosis of Community-Acquired Pneumonia in Children. Children 2023, 10, 1744. https://doi.org/10.3390/children10111744
Taraș R, Mahler B, Bălgrădean M, Derewicz D, Lazăr MI, Vidlescu R, Berghea F. The Role of Mannose-Binding Lectin and Inflammatory Markers in Establishing the Course and Prognosis of Community-Acquired Pneumonia in Children. Children. 2023; 10(11):1744. https://doi.org/10.3390/children10111744
Chicago/Turabian StyleTaraș, Roxana, Beatrice Mahler, Mihaela Bălgrădean, Diana Derewicz, Miruna Ioana Lazăr, Ruxandra Vidlescu, and Florian Berghea. 2023. "The Role of Mannose-Binding Lectin and Inflammatory Markers in Establishing the Course and Prognosis of Community-Acquired Pneumonia in Children" Children 10, no. 11: 1744. https://doi.org/10.3390/children10111744
APA StyleTaraș, R., Mahler, B., Bălgrădean, M., Derewicz, D., Lazăr, M. I., Vidlescu, R., & Berghea, F. (2023). The Role of Mannose-Binding Lectin and Inflammatory Markers in Establishing the Course and Prognosis of Community-Acquired Pneumonia in Children. Children, 10(11), 1744. https://doi.org/10.3390/children10111744










