Analysis of Clinical Symptoms and Biochemical Parameters in Odontogenic Cellulitis of the Head and Neck Region in Children
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nair, P.N. Pathogenesis of apical periodontitis and the causes of endodontic failures. Crit. Rev. Oral Biol. Med. 2004, 15, 348–381. [Google Scholar] [CrossRef]
- Bali, R.K.; Sharma, P.; Gaba, S.; Kaur, A.; Ghanghas, P. A review of complications of odontogenic infections. Natl. J. Maxillofac. Surg. 2015, 6, 136–143. [Google Scholar] [CrossRef]
- Han, X.; An, J.; Zhang, Y.; Gong, X.; He, Y. Risk Factors for Life-Threatening Complications of Maxillofacial Space Infection. J. Craniofac. Surg. 2016, 27, 385–390. [Google Scholar] [CrossRef]
- Giunta Crescente, C.; Soto de Facchin, M.; Acevedo Rodríguez, A.M. Medical-dental considerations in the care of children with facial cellulitis of odontogenic origin. A disease of interest for pediatricians and pediatric dentists. Arch. Argent Pediatr. 2018, 116, 548–553. [Google Scholar] [CrossRef]
- Biasotto, M.; Pellis, T.; Cadenaro, M.; Bevilacqua, L.; Berlot, G.; Di Lenarda, R. Odontogenic infections and descending necrotising mediastinitis: Case report and review of the literature. Int. Dent. J. 2004, 54, 97–102. [Google Scholar] [CrossRef]
- Gonzalez, L.P.; Pignaton, W.; Kusano, P.S.; Módolo, N.S.; Braz, J.R.; Braz, L.G. Anesthesia-related mortality in pediatric patients: A systematic review. Clinics 2012, 67, 381–387. [Google Scholar] [CrossRef]
- da Fonseca, M.A.; Nelson, T. The use of general anesthesia in behavior management. In Behavior Management in Dentistry for Children, 2nd ed.; Wright, G.Z., Kupietzky, A., Eds.; John Wiley & Sons: Chichester, UK, 2014; pp. 185–195. [Google Scholar]
- Perina, V.; Szaraz, D.; Harazim, H.; Urik, M.; Klabusayova, E. Paediatric Deep Neck Infection-The Risk of Needing Intensive Care. Children 2022, 9, 979. [Google Scholar] [CrossRef]
- Orzechowska-Wylęgała, B.; Wylęgała, A.; Buliński, M.; Niedzielska, I.; Madej, A. Pharmacoeconomic analysis of antibiotic therapy in maxillofacial surgery. BDJ Open. 2017, 3, 17002. [Google Scholar] [CrossRef]
- Wylęgała, A.; Paluch, M.; Orzechowska-Wylęgała, B.; Galicka-Brzezina, A.; Chyrek, K.; Madej, A. Pharmacoeconomic analysis of antibiotic therapy in surgical site infections. Int. J. Clin. Pharmacol. Ther. 2019, 57, 429–436. [Google Scholar] [CrossRef]
- Unkel, J.H.; McKibben, D.H.; Fenton, S.J.; Nazif, M.M.; Moursi, A.; Schuit, K. Comparison of odontogenic and nonodontogenic facial cellulitis in a pediatric hospital population. Pediatr. Dent. 1997, 19, 476–479. [Google Scholar]
- Biederman, G.R.; Dodson, T.B. Epidemiologic review of facial infections in hospitalized pediatric patients. J. Oral Maxillofac. Surg. 1994, 52, 1042–1045. [Google Scholar] [CrossRef]
- Lin, Y.T.; Lu, P.W. Retrospective study of pediatric facial cellulitis of odontogenic origin. Pediatr. Infect. Dis. J. 2006, 25, 339–342. [Google Scholar] [CrossRef]
- Doll, C.; Carl, F.; Neumann, K.; Voss, J.O.; Hartwig, S.; Waluga, R.; Heiland, M.; Raguse, J.D. Odontogenic Abscess-Related Emergency Hospital Admissions: A Retrospective Data Analysis of 120 Children and Young People Requiring Surgical Drainage. Biomed. Res. Int. 2018, 2018, 3504727. [Google Scholar] [CrossRef]
- Pepys, M.B.; Booth, S.E.; Tennent, G.A.; Butler, P.J.; Williams, D.G. Binding of pentraxins to different nuclear structures: C-reactive protein binds to small nuclear ribonucleoprotein particles, serum amyloid P component binds to chromatin and nucleoli. Clin. Exp. Immunol. 1994, 97, 152–157. [Google Scholar] [CrossRef]
- Ylijoki, S.; Suuronen, R.; Jousimies-Somer, H.; Meurman, J.H.; Lindqvist, C. Differences between patients with or without the need for intensive care due to severe odontogenic infections. J. Oral Maxillofac. Surg. 2001, 59, 867–873. [Google Scholar] [CrossRef]
- Stathopoulos, P.; Igoumenakis, D.; Shuttleworth, J.; Smith, W.; Ameerally, P. Predictive factors of hospital stay in patients with odontogenic maxillofacial infections: The role of C-reactive protein. Br. J. Oral Maxillofac. Surg. 2017, 55, 367–370. [Google Scholar] [CrossRef]
- Sharma, A.; Giraddi, G.; Krishnan, G.; Shahi, A.K. Efficacy of Serum Prealbumin and CRP Levels as Monitoring Tools for Patients with Fascial Space Infections of Odontogenic Origin: A Clinicobiochemical Study. J. Maxillofac. Oral Surg. 2014, 13, 1–9. [Google Scholar] [CrossRef]
- Pinilla, J.C.; Hayes, P.; Laverty, W.; Arnold, C.; Laxdal, V. The C-reactive protein to prealbumin ratio correlates with the severity of multiple organ dysfunction. Surgery 1998, 124, 799–806. [Google Scholar] [CrossRef]
- Bègue, L.; Schlund, M.; Raoul, G.; Ferri, J.; Lauwers, L.; Nicot, R. Biological factors predicting the length of hospital stay in odontogenic cellulitis. J. Stomatol. Oral Maxillofac. Surg. 2022, 123, 303–308. [Google Scholar] [CrossRef]
- Heim, N.; Wiedemeyer, V.; Reich, R.H.; Martini, M. The role of C-reactive protein and white blood cell count in the prediction of length of stay in hospital and severity of odontogenic abscess. J. Craniomaxillofac. Surg. 2018, 46, 2220–2226. [Google Scholar] [CrossRef]
- Ren, Y.F.; Malmstrom, H.S. Rapid quantitative determination of C-reactive protein at chair side in dental emergency patients. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 104, 49–55. [Google Scholar] [CrossRef]
- Aminzadeh, Z.; Parsa, E. Relationship between Age and Peripheral White Blood Cell Count in Patients with Sepsis. Int. J. Prev. Med. 2011, 2, 238–242. [Google Scholar]
- Boucher, N.E., Jr.; Hanrahan, J.J.; Kihara, F.Y. Occurrence of C-reactive protein in oral disease. J. Dent. Res. 1967, 46, 624. [Google Scholar] [CrossRef]
- Kaur, A.; Sandhu, A.; Kaur, T.; Bhullar, R.S.; Dhawan, A.; Kaur, J. Correlation Between Clinical Course and Biochemical Analysis in Odontogenic Space Infections. J. Maxillofac. Oral Surg. 2019, 18, 203–209. [Google Scholar] [CrossRef]
- Bagul, R.; Chandan, S.; Sane, V.D.; Patil, S.; Yadav, D. Comparative Evaluation of C-Reactive Protein and WBC Count in Fascial Space Infections of Odontogenic Origin. J. Maxillofac. Oral Surg. 2017, 16, 238–242. [Google Scholar] [CrossRef]
- Peters, E.S.; Fong, B.; Wormuth, D.W.; Sonis, S.T. Risk factors affecting hospital length of stay in patients with odontogenic maxillofacial infections. J. Oral Maxillofac. Surg. 1996, 54, 1386–1392. [Google Scholar] [CrossRef]
- Wang, J.; Ahani, A.; Pogrel, M.A. A five-year retrospective study of odontogenic maxillofacial infections in a large urban public hospital. Int. J. Oral Maxillofac. Surg. 2005, 34, 646–649. [Google Scholar] [CrossRef]
- Huang, Z.; Fu, Z.; Huang, W.; Huang, K. Prognostic value of neutrophil-to-lymphocyte ratio in sepsis: A meta-analysis. Am. J. Emerg. Med. 2020, 38, 641–647. [Google Scholar] [CrossRef]
- Dogruel, F.; Gonen, Z.B.; Gunay-Canpolat, D.; Zararsiz, G.; Alkan, A. The Neutrophil-to-Lymphocyte ratio as a marker of recovery status in patients with severe dental infection. Med. Oral Patol. Oral Cir. Bucal. 2017, 22, 440–445. [Google Scholar] [CrossRef]
- Gallagher, N.; Collyer, J.; Bowe, C.M. Neutrophil to lymphocyte ratio as a prognostic marker of deep neck space infections secondary to odontogenic infection. Br. J. Oral Maxillofac. Surg. 2021, 59, 228–232. [Google Scholar] [CrossRef]
- Evans, D.C.; Corkins, M.R.; Malone, A.; Miller, S.; Mogensen, K.M.; Guenter, P.; Jensen, G.L.; the ASPEN Malnutrition Committee. The Use of Visceral Proteins as Nutrition Markers: An ASPEN Position Paper. Nutr. Clin. Pract. 2021, 36, 22–28. [Google Scholar] [CrossRef]
- Cunningham, L.L., Jr.; Madsen, M.J.; Van Sickels, J.E. Using prealbumin as an inflammatory marker for patients with deep space infections of odontogenic origin. J. Oral Maxillofac. Surg. 2006, 64, 375–378. [Google Scholar] [CrossRef]
- Adeosun, P.O.; Fatusi, O.A.; Adedeji, T.A. Assessment of Severity of Illness and Monitoring Response to Treatment of Odontogenic Space Infection Using Serum Prealbumin. J. Maxillofac. Oral Surg. 2019, 18, 106–111. [Google Scholar] [CrossRef]
- Johnson, E.D.; Schell, J.C.; Rodgers, G.M. The D-dimer assay. Am. J. Hematol. 2019, 94, 833–839. [Google Scholar] [CrossRef]
- Sánchez-Siles, M.; Rosa-Salazar, V.; Salazar-Sánchez, N.; Camacho-Alonso, F. Periodontal disease as a risk factor of recurrence of venous thromboembolic disease: A prospective study. Acta Odontol. Scand. 2015, 73, 8–13. [Google Scholar] [CrossRef]
- Ramseier, C.A.; Kinney, J.S.; Herr, A.; Braun, T.; Sugai, J.V.; Shelburne, C.A.; Rayburn, L.A.; Tran, H.M.; Singh, A.K.; Giannobile, W.V. Identification of pathogen and host-response markers correlated with periodontal disease. J. Periodontol. 2009, 80, 436–446. [Google Scholar] [CrossRef]
- Levi, M.; van der Poll, T.; Büller, H.R. Bidirectional relation between inflammation and coagulation. Circulation 2004, 109, 2698–2704. [Google Scholar] [CrossRef]


| Number | CRP | WBC Count | D-Dimer | Prealbumin | NLR Ratio |
|---|---|---|---|---|---|
| 1 | 32.2 | 5.39 | 618 | 0.14 | 2.5 |
| 2 | 166.60 | 11.5 | 1051 | 0.13 | 7.5 |
| 3 | 112 | 12.5 | 1167 | 0.15 | 6.2 |
| 4 | 129.6 | 13.66 | 1138 | 0.09 | 9.8 |
| 5 | 26.7 | 14.3 | 1038 | 0.08 | 3.4 |
| 6 | 102.2 | 14.2 | 1207 | 0.09 | 8.25 |
| 7 | 3 | 6.4 | 417 | 0.16 | 1.1 |
| 8 | 12.9 | 12 | 540 | 0.13 | 8.1 |
| 9 | 13.3 | 6.4 | 1599 | 0.11 | 7.1 |
| 10 | 44.7 | 10.24 | 2180 | 0.12 | 6.6 |
| 11 | 40 | 10.22 | 246 | 0.14 | 3.8 |
| 12 | 33.8 | 15.3 | 390 | 0.13 | 4.2 |
| 13 | 45.1 | 8.5 | 511 | 0.15 | 2.5 |
| 14 | 11 | 6.37 | 179 | 0.15 | 2.7 |
| 15 | 34.1 | 16.1 | 795 | 0.1 | 3.5 |
| 16 | 40 | 13.4 | 466 | 0.1 | 3.4 |
| 17 | 147.9 | 22.6 | 2797 | 0.13 | 23.7 |
| 18 | 121.6 | 14.2 | 12,958 | 0.13 | 41.1 |
| 19 | 98 | 11.3 | 453 | 0.15 | 5.2 |
| 20 | 70 | 12.5 | 671 | 0.14 | 2.15 |
| Number | CRP | WBC Count | D-Dimer | Prealbumin | NRL Ratio |
|---|---|---|---|---|---|
| 1 | 2.2 | 8.52 | 544 | 0.26 | 1.7 |
| 2 | 2.4 | 9.3 | 560 | 0.25 | 2.1 |
| 3 | 3.1 | 9.69 | 98 | 0.24 | 2.5 |
| 4 | 1.9 | 9.32 | 64 | 0.18 | 0.6 |
| 5 | 0.4 | 4.2 | 14 | 0.2 | 1.5 |
| 6 | 4.7 | 6.58 | 35 | 0.2 | 1 |
| 7 | 0 | 5.9 | 47 | 0.26 | 1.3 |
| 8 | 3.4 | 6.46 | 466 | 0.21 | 0.8 |
| 9 | 0.7 | 8.56 | 21 | 0.16 | 3.5 |
| 10 | 0.3 | 4.83 | 167 | 0.26 | 1.5 |
| 11 | 0.3 | 5.99 | 199 | 0.23 | 1 |
| 12 | 1.6 | 6 | 680 | 0.26 | 1.9 |
| 13 | 2.5 | 4.2 | 182 | 0.18 | 1.2 |
| 14 | 0 | 5.9 | 359 | 0.21 | 1.7 |
| 15 | 0.6 | 4.23 | 319 | 0.28 | 1.3 |
| 16 | 0.9 | 5.8 | 189 | 0.19 | 2.6 |
| 17 | 0.7 | 5.5 | 158 | 0.24 | 2.6 |
| 18 | 1.1 | 6.1 | 236 | 0.19 | 2.9 |
| 19 | 0.3 | 4.7 | 141 | 0.18 | 1.8 |
| 20 | 3.4 | 6.7 | 278 | 0.2 | 2.0 |
| Parameter | SS + CS | SS | CS | p Value |
|---|---|---|---|---|
| CRP | 32.9 ± 46.7 | 64.2 ± 49.0 | 1.5 ± 1.3 | <0.001 |
| WBC Count | 9.1 ±4.1 | 11.9 ± 4.0 | 6.4 ± 1.7 | <0.001 |
| NLR | 4.7 ± 7.0 | 7.6 ± 9.0 | 1.8 ± 0.7 | 0.007 |
| D-dimer | 879.4 ± 2019.3 | 1521.0 ± 2701.1 | 237.8 ± 189.8 | 0.046 |
| Prealbumin | 0.2 ± 0.1 | 0.1 ± 0.0 | 0.2 ± 0.0 | <0.001 |
| Hospitalization | 2.1 ± 2.1 | 4.0 ± 2.6 | 1.0 ± 0.0 | <0.001 |
| Parameter | CRP | WBC | NLR | D-dimer | Prealbumin |
|---|---|---|---|---|---|
| CRP | 1.00 | ||||
| WBC Count | 0.43 | 1.00 | |||
| NLR | 0.57 * | 0.45 | 1.00 | ||
| D-dimer | 0.55 * | 0.39 | 0.67 * | 1.00 | |
| Prealbumin | −0.14 | −0.58 * | −0.45 * | −0.49 * | 1.00 |
| Number | Trismus [mm] | Extraoral Swelling [mm] | Intraoral Swelling | Length of Hospitalization | Number of Anatomic Spaces Involved |
|---|---|---|---|---|---|
| 1 | 25 | 12 | + | 4 | 2 |
| 2 | 19 | 24 | + | 3 | 2 |
| 3 | − | 12 | + | 6 | 2 |
| 4 | 22 | 22 | + | 5 | 1 |
| 5 | − | 10 | + | 2 | 2 |
| 6 | 27 | 19 | + | 3 | 3 |
| 7 | 29 | 14 | + | 1 | 1 |
| 8 | 20 | 17 | + | 4 | 2 |
| 9 | − | 16 | + | 2 | 1 |
| 10 | 24 | 20 | + | 1 | 3 |
| 11 | − | 0 | − | 4 | 0 |
| 12 | − | 0 | − | 3 | 0 |
| 13 | − | 0 | + | 3 | 2 |
| 14 | − | 0 | + | 1 | 2 |
| 15 | 28 | 18 | + | 5 | 1 |
| 16 | − | 0 | + | 1 | 1 |
| 17 | 22 | 26 | + | 10 | 3 |
| 18 | 23 | 23 | + | 7 | 3 |
| 19 | 25 | 20 | + | 1 | 1 |
| 20 | − | 0 | + | 1 | 2 |
| Parameter | Trismus | Extraoral Swelling | Length of Hospitalization | Number of Anatomic Spaces Involved |
|---|---|---|---|---|
| CRP | −0.43 | 0.56 * | 0.44 (p = 0.054) | 0.36 |
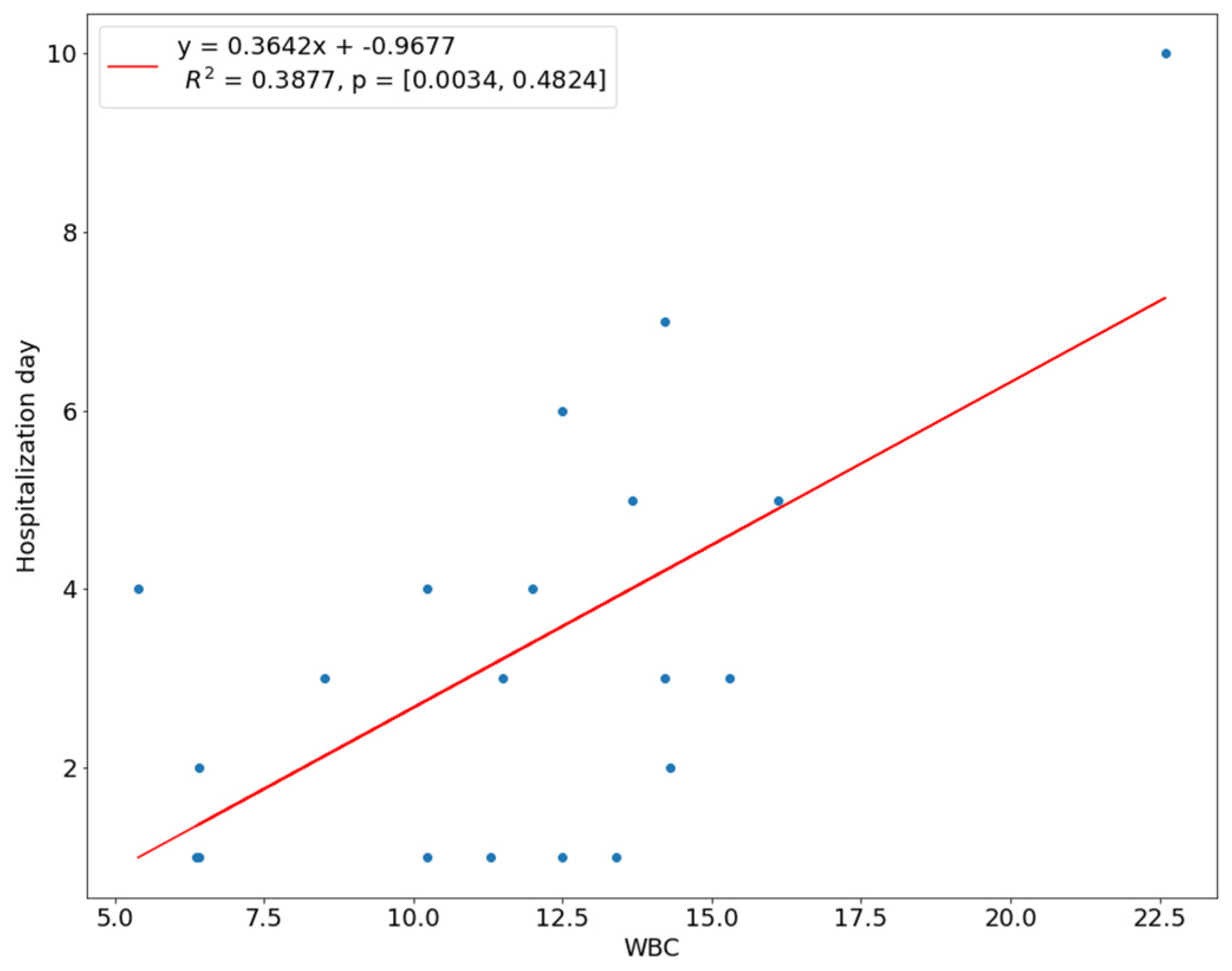
| WBC Count | −0.16 | 0.29 | 0.44 (p = 0.05) | 0.12 |
| NLR | −0.63 * | 0.76 * | 0.56 * | 0.34 |
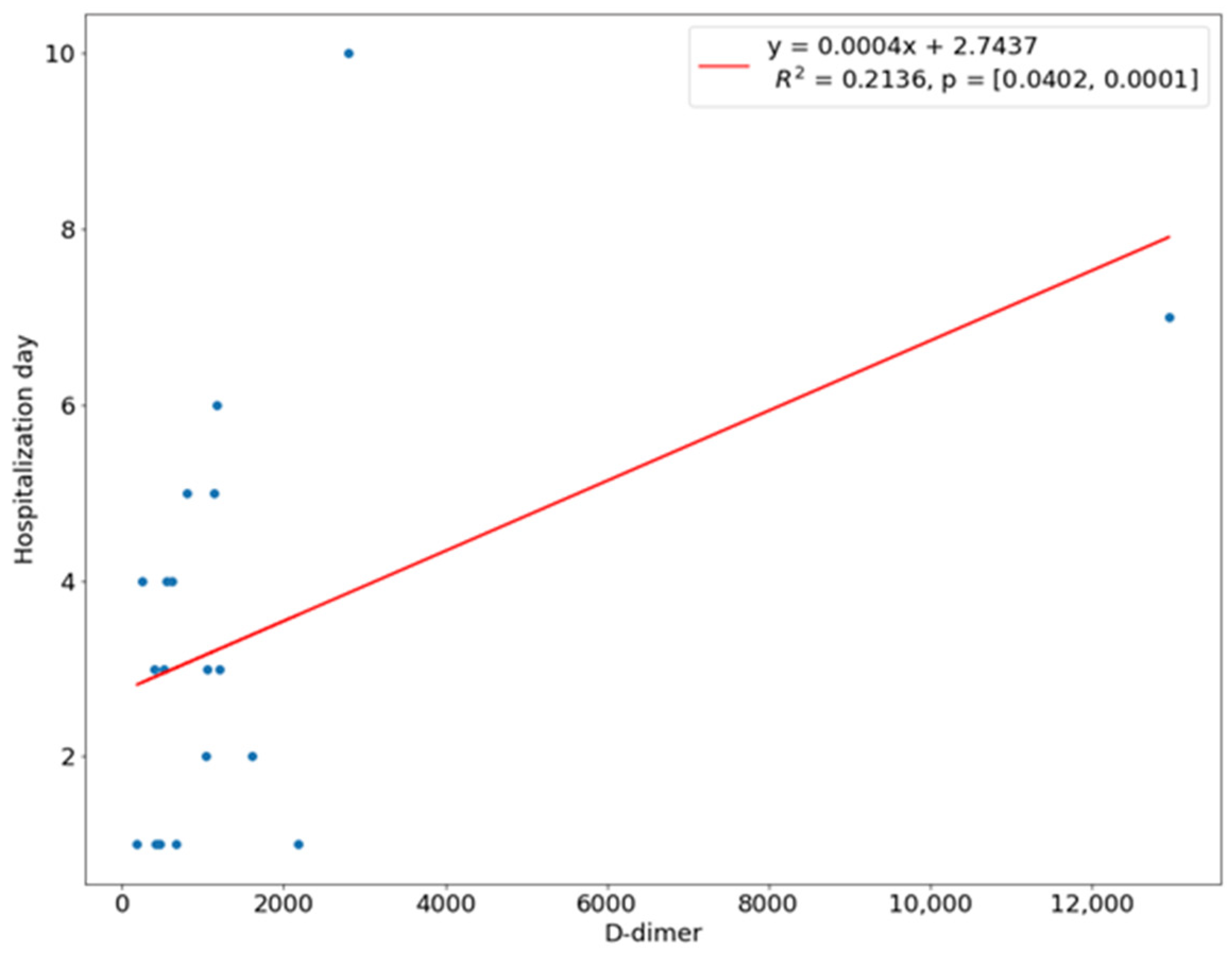
| D-dimer | −0.44 * | 0.7 * | 0.44 (0.055) | 0.64 * |
| Prealbumin | 0.19 | −0.29 | −0.15 | −0.08 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Słotwińska-Pawlaczyk, A.; Orzechowska-Wylęgała, B.; Latusek, K.; Roszkowska, A.M. Analysis of Clinical Symptoms and Biochemical Parameters in Odontogenic Cellulitis of the Head and Neck Region in Children. Children 2023, 10, 172. https://doi.org/10.3390/children10010172
Słotwińska-Pawlaczyk A, Orzechowska-Wylęgała B, Latusek K, Roszkowska AM. Analysis of Clinical Symptoms and Biochemical Parameters in Odontogenic Cellulitis of the Head and Neck Region in Children. Children. 2023; 10(1):172. https://doi.org/10.3390/children10010172
Chicago/Turabian StyleSłotwińska-Pawlaczyk, Adrianna, Bogusława Orzechowska-Wylęgała, Katarzyna Latusek, and Anna Maria Roszkowska. 2023. "Analysis of Clinical Symptoms and Biochemical Parameters in Odontogenic Cellulitis of the Head and Neck Region in Children" Children 10, no. 1: 172. https://doi.org/10.3390/children10010172
APA StyleSłotwińska-Pawlaczyk, A., Orzechowska-Wylęgała, B., Latusek, K., & Roszkowska, A. M. (2023). Analysis of Clinical Symptoms and Biochemical Parameters in Odontogenic Cellulitis of the Head and Neck Region in Children. Children, 10(1), 172. https://doi.org/10.3390/children10010172






