Serum Perilipin 2 (PLIN2) Predicts Multiple Organ Dysfunction in Critically Ill Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Characteristics
2.2. PLIN2 Measurements
2.3. Assessment of Computed Tomography Scan Body Composition Markers
2.4. Statistical Analysis
3. Results
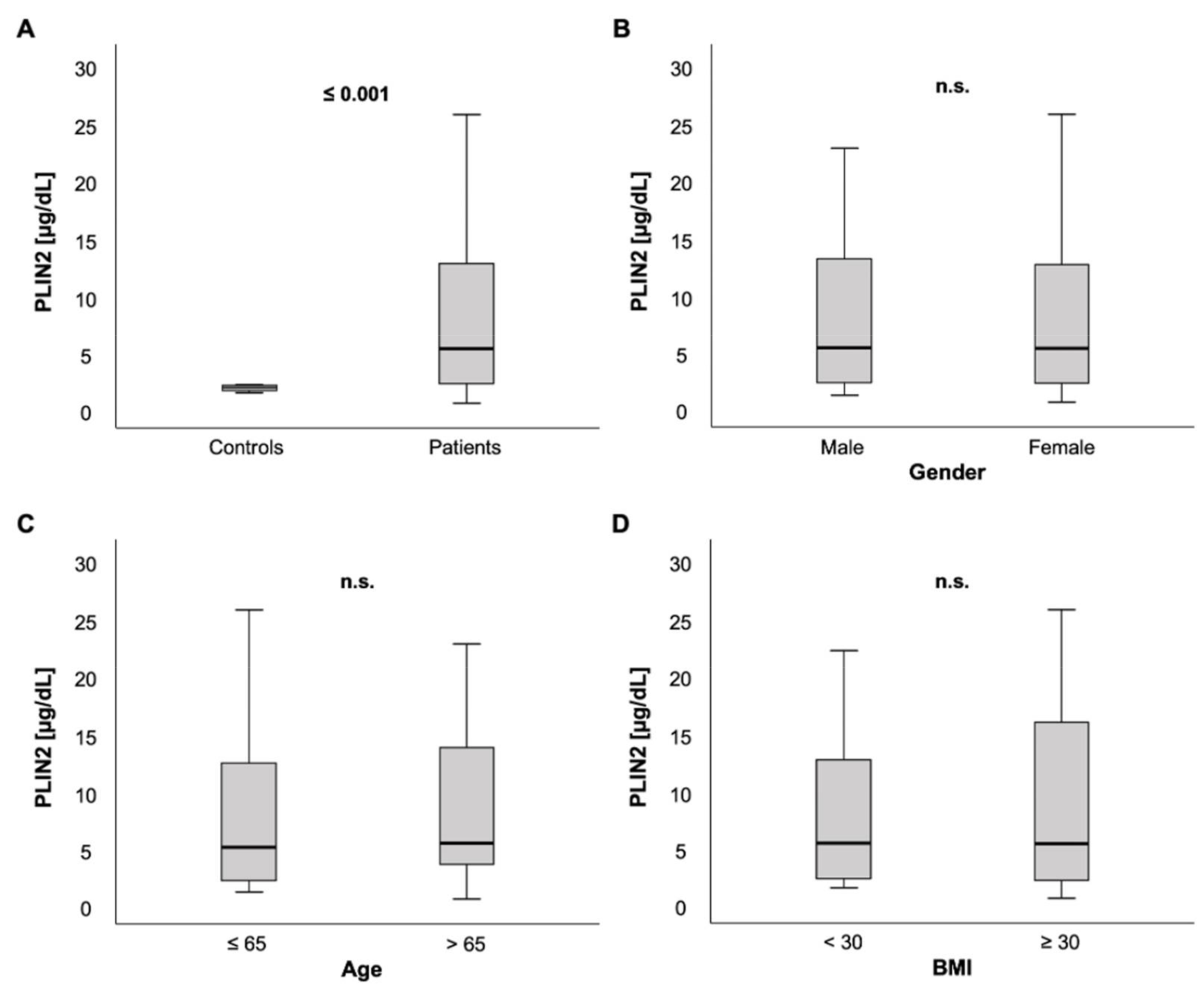
3.1. PLIN2 Serum Levels Were Significantly Elevated in Critically Ill Patients
3.2. Associations of PLIN2 Serum Concentrations with Clinical Data and Blood-Based Parameters
3.3. PLIN2 Levels Were Associated with Organ Failure and Disease Severity
3.4. PLIN2 Serum Levels and Association with CT Scan Body Composition Markers
3.5. Serum PLIN2 Concentrations May Predict ICU Mortality in Critically Ill Patients Older Than 65 Years
4. Discussion
- (i)
- Because of growing evidence suggesting sex differences in the pathophysiology of critical illness [49,50,51], we investigated whether PLIN2 concentrations show a different distribution based on sex. In contrast to recent data stating that PLIN2 levels were higher in women, especially in patients below 79 years [32], we did not detect any difference of serum PLIN2 in both sexes.
- (ii)
- (iii)
- As BMI and mortality act in a “J-shaped” dependence and, because overweight and moderate obesity appear to be protective factors in critically ill patients, called the “obesity paradox” [36,52,53], we correlated serum PLIN2 with BMI and analyzed PLIN2 in different BMI subgroups (underweight vs. normal vs. overweight vs. obese; data not shown). Serum PLIN2 did not show any significant differences in these analyses, which is in contrast to previously published data [32].
- (iv)
- PLIN2 acts as a regulator in lipid metabolism [5,7,15,16] and previous murine and human studies have shown that PLIN2 dysregulation can be associated with lipid storage malfunction diseases [7,14,17,18,19,20,21,22]. Surprisingly and despite PLIN’s function as a lipid droplet protein, we did not detect an association of serum PLIN2 with classical markers of lipid metabolism such as cholesterol, LDL or triglycerides. These results are not in line with experimental studies, which showed reduction of hepatic steatosis or lower triglycerides in serum and liver after knock-out or downregulation of PLIN2 expression [6,7,9,19,54].
- (v)
- Insulin resistance and diabetes mellitus are important modulators of mortality and morbidity in critically ill patients [36]. Experimental research suggests that PLIN2 is involved in the pathophysiology of insulin resistance [12,13,14]. This encouraged us to analyze the relationship between pre-existent diabetes and PLIN2 serum levels. Of note, serum PLIN2 concentrations were independent of the presence of diabetes. Moreover, we did not observe a correlation between PLIN2 levels and HbA1c levels, but a non-significant trend towards a rather weak correlation with HOMA-IR. Interestingly, a recently published study reports similar results, with no observed association with DM, but a significant correlation between PLIN2 and HOMA-IR [32]. Another group described higher PLIN2 levels in diabetic patients with NAFLD compared to patients without NAFLD, and correlations with age, waist circumference, triglycerides and HOMA-IR. However, these results are difficult to compare to our study because we did not assess our patients for the presence of NAFLD.
- (a)
- There has been evidence of PLIN2 involvement in the development of age-related vascular disease, such as atherosclerosis [6,15,23,24,25,26,27]. Recent studies highlighted the importance of PLIN2 in cardiomyocyte lipid accumulation [28] and were able to connect PLIN2 to coronary microvascular obstruction and infarct size in patients with ST-elevation myocardial infarction and major adverse cardiovascular events during follow-up [55]. Intrigued by these findings, we investigated whether arterial hypertension or coronary artery disease are associated with altered PLIN2 serum levels. However, our results did not prove any obvious association between vascular diseases and PLIN2 levels.
- (b)
- Prompted by experimental research connecting changes in PLIN2 serum levels with hepatic diseases and alcohol consumption [20,21,54,56], we analyzed serum PLIN2 concentrations in ICU patients suffering from liver cirrhosis and patients with a history of alcohol abuse. However, we did not observe any connections between cirrhosis or alcohol abuse and PLIN2 levels. However, this may be due to missing statistical power because only 3.1% of our cohort had cirrhosis. Additionally, the majority of the mentioned studies assessed PLIN2 in NAFLD or non-alcoholic steatohepatitis (NASH) instead of cirrhosis, further reducing the comparability of the results.
- (c)
- PLIN2′s activation state is regulated by pancreatic hormones. While catecholamines permit lipolysis via phosphorylation and dissociation of PLIN2, insulin inhibits lipolysis via dephosphorylation of PLIN2, hindering hormone-sensitive lipases in accessing the lipid droplets [21]. Of note, we observed a strong negative correlation between PLIN2 and lipase. Correspondingly, patients admitted due to acute pancreatitis presented with decreased PLIN2 concentrations. However, serum PLIN2 was not able to discriminate a mortality difference in the small subgroup of patients with acute pancreatitis (n = 13; Figure S4A). To the best of our knowledge, associations with pancreatic markers or disease have not been previously described. Taking physiological mechanisms into consideration, the inverse association of PLIN2 with lipase raises the question of whether this is due to pancreatitis and its associated multiple organ dysfunction or rather an effect of higher PLIN2 metabolization of serum lipases. Importantly, serum PLIN2 levels were not associated with norepinephrine demand. Moreover, the logistic regression analyses of PLIN2 and SOFA score > 9 points remained significant after adjustment for the norepinephrine demand (Table 3).
- (d)
- Previous studies have demonstrated the role of PLIN2 as a tumor marker in different body fluids or in tumor tissue [6,57,58] for several malignant diseases, such as renal cell carcinoma [57,59,60,61], colorectal carcinoma [29] or lung adenocarcinoma [30]. In our ICU cohort, PLIN2 serum concentrations were elevated in patients with preexistent malignant disease. These consistent associations of serum PLIN2 with malignancy even during critical illness underline its potential capacity as a tumor marker for routine diagnostics.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jiang, H.P.; Serrero, G. Isolation and characterization of a full-length cDNA coding for an adipose differentiation-related protein. Proc. Natl. Acad. Sci. USA 1992, 89, 7856–7860. [Google Scholar] [CrossRef] [Green Version]
- Jiang, H.P.; Harris, S.E.; Serrero, G. Molecular cloning of a differentiation-related mRNA in the adipogenic cell line 1246. Cell Growth Differ. 1992, 3, 21–30. [Google Scholar]
- Brasaemle, D.L.; Barber, T.; Wolins, N.E.; Serrero, G.; Blanchette-Mackie, E.J.; Londos, C. Adipose differentiation-related protein is an ubiquitously expressed lipid storage droplet-associated protein. J. Lipid Res. 1997, 38, 2249–2263. [Google Scholar] [CrossRef]
- Heid, H.W.; Moll, R.; Schwetlick, I.; Rackwitz, H.R.; Keenan, T.W. Adipophilin is a specific marker of lipid accumulation in diverse cell types and diseases. Cell Tissue Res. 1998, 294, 309–321. [Google Scholar] [CrossRef]
- Imamura, M.; Inoguchi, T.; Ikuyama, S.; Taniguchi, S.; Kobayashi, K.; Nakashima, N.; Nawata, H. ADRP stimulates lipid accumulation and lipid droplet formation in murine fibroblasts. Am. J. Physiol. Endocrinol. Metab. 2002, 283, E775–E783. [Google Scholar] [CrossRef] [Green Version]
- Conte, M.; Franceschi, C.; Sandri, M.; Salvioli, S. Perilipin 2 and Age-Related Metabolic Diseases: A New Perspective. Trends Endocrinol. Metab. 2016, 27, 893–903. [Google Scholar] [CrossRef]
- Imai, Y.; Varela, G.M.; Jackson, M.B.; Graham, M.J.; Crooke, R.M.; Ahima, R.S. Reduction of hepatosteatosis and lipid levels by an adipose differentiation-related protein antisense oligonucleotide. Gastroenterology 2007, 132, 1947–1954. [Google Scholar] [CrossRef]
- Listenberger, L.L.; Ostermeyer-Fay, A.G.; Goldberg, E.B.; Brown, W.J.; Brown, D.A. Adipocyte differentiation-related protein reduces the lipid droplet association of adipose triglyceride lipase and slows triacylglycerol turnover. J. Lipid Res. 2007, 48, 2751–2761. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Imai, Y.; Boyle, S.; Varela, G.M.; Caron, E.; Yin, X.; Dhir, R.; Dhir, R.; Graham, M.J.; Ahima, R.S. Effects of perilipin 2 antisense oligonucleotide treatment on hepatic lipid metabolism and gene expression. Physiol. Genom. 2012, 44, 1125–1131. [Google Scholar] [CrossRef] [Green Version]
- Sztalryd, C.; Brasaemle, D.L. The perilipin family of lipid droplet proteins: Gatekeepers of intracellular lipolysis. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2017, 1862, 1221–1232. [Google Scholar] [CrossRef] [PubMed]
- Sztalryd, C.; Kimmel, A.R. Perilipins: Lipid droplet coat proteins adapted for tissue-specific energy storage and utilization, and lipid cytoprotection. Biochimie 2014, 96, 96–101. [Google Scholar] [CrossRef] [Green Version]
- Varela, G.M.; Antwi, D.A.; Dhir, R.; Yin, X.; Singhal, N.S.; Graham, M.J.; Crooke, R.M.; Ahima, R.S. Inhibition of ADRP prevents diet-induced insulin resistance. Am. J. Physiol.-Gastrointest. Liver Physiol. 2008, 295, G621–G628. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bosma, M.; Hesselink, M.K.; Sparks, L.M.; Timmers, S.; Ferraz, M.J.; Mattijssen, F.; van Beurden, D.; Schaart, G.; de Baets, M.H.; Verheyen, F.K.; et al. Perilipin 2 improves insulin sensitivity in skeletal muscle despite elevated intramuscular lipid levels. Diabetes 2012, 61, 2679–2690. [Google Scholar] [CrossRef] [Green Version]
- Chang, B.H.; Li, L.; Saha, P.; Chan, L. Absence of adipose differentiation related protein upregulates hepatic VLDL secretion, relieves hepatosteatosis, and improves whole body insulin resistance in leptin-deficient mice. J. Lipid Res. 2010, 51, 2132–2142. [Google Scholar] [CrossRef] [Green Version]
- Larigauderie, G.; Cuaz-Pérolin, C.; Younes, A.B.; Furman, C.; Lasselin, C.; Copin, C.; Jaye, M.; Fruchart, J.C.; Rouis, M. Adipophilin increases triglyceride storage in human macrophages by stimulation of biosynthesis and inhibition of beta-oxidation. FEBS J. 2006, 273, 3498–3510. [Google Scholar] [CrossRef]
- Ducharme, N.A.; Bickel, P.E. Lipid droplets in lipogenesis and lipolysis. Endocrinology 2008, 149, 942–949. [Google Scholar] [CrossRef] [Green Version]
- Chang, B.H.; Li, L.; Paul, A.; Taniguchi, S.; Nannegari, V.; Heird, W.C.; Chan, L. Protection against fatty liver but normal adipogenesis in mice lacking adipose differentiation-related protein. Mol. Cell Biol. 2006, 26, 1063–1076. [Google Scholar] [CrossRef] [Green Version]
- Fan, H.; Diao, H.; Lu, Y.; Xie, J.; Cheng, X. The relation between serum adipose differentiation-related protein and non-alcoholic fatty liver disease in type 2 diabetes mellitus. Ther. Adv. Endocrinol. Metab. 2020, 11. [Google Scholar] [CrossRef] [PubMed]
- McManaman, J.L.; Bales, E.S.; Orlicky, D.J.; Jackman, M.; MacLean, P.S.; Cain, S.; Crunk, A.E.; Mansur, A.; Graham, C.E.; Bowman, T.A.; et al. Perilipin-2-null mice are protected against diet-induced obesity, adipose inflammation, and fatty liver disease. J. Lipid Res. 2013, 54, 1346–1359. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Motomura, W.; Inoue, M.; Ohtake, T.; Takahashi, N.; Nagamine, M.; Tanno, S.; Kohgo, Y.; Okumura, T. Up-regulation of ADRP in fatty liver in human and liver steatosis in mice fed with high fat diet. Biochem. Biophys. Res. Commun. 2006, 340, 1111–1118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Straub, B.K.; Stoeffel, P.; Heid, H.; Zimbelmann, R.; Schirmacher, P. Differential pattern of lipid droplet-associated proteins and de novo perilipin expression in hepatocyte steatogenesis. Hepatology 2008, 47, 1936–1946. [Google Scholar] [CrossRef]
- Liu, F.; Wang, C.; Zhang, L.; Xu, Y.; Jang, L.; Gu, Y.; Cao, X.; Zhao, X.; Ye, J.; Li, Q. Metformin prevents hepatic steatosis by regulating the expression of adipose differentiation-related protein. Int. J. Mol. Med. 2014, 33, 51–58. [Google Scholar] [CrossRef] [Green Version]
- Larigauderie, G.; Furman, C.; Jaye, M.; Lasselin, C.; Copin, C.; Fruchart, J.C.; Castro, G.; Rouis, M. Adipophilin enhances lipid accumulation and prevents lipid efflux from THP-1 macrophages: Potential role in atherogenesis. Arterioscler. Thromb. Vasc. Biol. 2004, 24, 504–510. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paul, A.; Chan, L.; Bickel, P.E. The PAT family of lipid droplet proteins in heart and vascular cells. Curr. Hypertens. Rep. 2008, 10, 461–466. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paul, A.; Chang, B.H.; Li, L.; Yechoor, V.K.; Chan, L. Deficiency of adipose differentiation-related protein impairs foam cell formation and protects against atherosclerosis. Circ. Res. 2008, 102, 1492–1501. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Son, S.H.; Goo, Y.H.; Choi, M.; Saha, P.K.; Oka, K.; Chan, L.C.; Paul, A. Enhanced atheroprotection and lesion remodelling by targeting the foam cell and increasing plasma cholesterol acceptors. Cardiovasc. Res. 2016, 109, 294–304. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, B.; Zhao, H.; Wang, S.; Sun, X.; Qin, X. Increased ADRP expression in human atherosclerotic lesions correlates with plaque instability. Int. J. Clin. Exp. Med. 2015, 8, 5414–5421. [Google Scholar]
- Mardani, I.; Tomas Dalen, K.; Drevinge, C.; Miljanovic, A.; Ståhlman, M.; Klevstig, M.; Scharin Täng, M.; Fogelstrand, P.; Levin, M.; Ekstrand, M.; et al. Plin2-deficiency reduces lipophagy and results in increased lipid accumulation in the heart. Sci. Rep. 2019, 9, 6909. [Google Scholar] [CrossRef] [Green Version]
- Matsubara, J.; Honda, K.; Ono, M.; Sekine, S.; Tanaka, Y.; Kobayashi, M.; Jung, G.; Sakuma, T.; Nakamori, S.; Sata, N.; et al. Identification of adipophilin as a potential plasma biomarker for colorectal cancer using label-free quantitative mass spectrometry and protein microarray. Cancer Epidemiol. Prev. Biomark. 2011, 20, 2195–2203. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.D.; Li, W.; Zhang, N.; Hou, Y.L.; Niu, Z.Q.; Zhong, Y.J.; Zhang, Y.P.; Yang, S.Y. Identification of adipophilin as a potential diagnostic tumor marker for lung adenocarcinoma. Int. J. Clin. Exp. Med. 2014, 7, 1190–1196. [Google Scholar]
- Conte, M.; Armani, A.; Conte, G.; Serra, A.; Franceschi, C.; Mele, M.; Sandri, M.; Salvioli, S. Muscle-specific Perilipin2 down-regulation affects lipid metabolism and induces myofiber hypertrophy. J. Cachexia Sarcopenia Muscle 2019, 10, 95–110. [Google Scholar] [CrossRef] [Green Version]
- Conte, M.; Santoro, A.; Collura, S.; Martucci, M.; Battista, G.; Bazzocchi, A.; Morsiani, C.; Sevini, F.; Capri, M.; Monti, D.; et al. Circulating perilipin 2 levels are associated with fat mass, inflammatory and metabolic markers and are higher in women than men. Aging 2021, 13, 7931–7942. [Google Scholar] [CrossRef]
- Conte, M.; Vasuri, F.; Bertaggia, E.; Armani, A.; Santoro, A.; Bellavista, E.; Degiovanni, A.; D’Errico-Grigioni, A.; Trisolino, G.; Capri, M.; et al. Differential expression of perilipin 2 and 5 in human skeletal muscle during aging and their association with atrophy-related genes. Biogerontology 2015, 16, 329–340. [Google Scholar] [CrossRef] [PubMed]
- Conte, M.; Vasuri, F.; Trisolino, G.; Bellavista, E.; Santoro, A.; Degiovanni, A.; Martucci, E.; D’Errico-Grigioni, A.; Caporossi, D.; Capri, M.; et al. Increased Plin2 Expression in Human Skeletal Muscle Is Associated with Sarcopenia and Muscle Weakness. PLoS ONE 2013, 8, e73709. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ouchi, N.; Parker, J.L.; Lugus, J.J.; Walsh, K. Adipokines in inflammation and metabolic disease. Nat. Rev. Immunol. 2011, 11, 85–97. [Google Scholar] [CrossRef] [PubMed]
- Schetz, M.; De Jong, A.; Deane, A.M.; Druml, W.; Hemelaar, P.; Pelosi, P.; Pickkers, P.; Reintam-Blaser, A.; Roberts, J.; Sakr, Y.; et al. Obesity in the critically ill: A narrative review. Intensive Care Med. 2019, 45, 757–769. [Google Scholar] [CrossRef]
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef]
- Knaus, W.; Draper, E.A.; Wagner, D.P.; Zimmerman, J.E. APACHE II: A severity of disease classification system. Crit. Care Med. 1985, 13, 818–829. [Google Scholar] [CrossRef]
- Cloud-Clone Corp: ELISA Kit for Adipose Differentiation Related Protein (ADRP). Available online: http://www.cloud-clone.com/products/SEB350Hu.html (accessed on 28 August 2021).
- Faron, A.; Luetkens, J.A.; Schmeel, F.C.; Kuetting, D.L.R.; Thomas, D.; Sprinkart, A.M. Quantification of fat and skeletal muscle tissue at abdominal computed tomography: Associations between single-slice measurements and total compartment volumes. Abdom. Radiol. 2019, 44, 1907–1916. [Google Scholar] [CrossRef]
- Wirtz, T.H.; Loosen, S.H.; Schulze-Hagen, M.; Weiskirchen, R.; Buendgens, L.; Abu Jhaisha, S.; Brozat, J.F.; Puengel, T.; Vucur, M.; Paffenholz, P.; et al. CT-based determination of excessive visceral adipose tissue is associated with an impaired survival in critically ill patients. PLoS ONE 2021, 16, e0250321. [Google Scholar] [CrossRef]
- Loosen, S.H.; Schulze-Hagen, M.; Püngel, T.; Bündgens, L.; Wirtz, T.; Kather, J.N.; Vucur, M.; Paffenholz, P.; Demir, M.; Bruners, P.; et al. Skeletal Muscle Composition Predicts Outcome in Critically Ill Patients. Crit. Care Explor. 2020, 2, e0171. [Google Scholar] [CrossRef]
- Fedorov, A.; Beichel, R.; Kalpathy-Cramer, J.; Finet, J.; Fillion-Robin, J.C.; Pujol, S.; Bauer, C.; Jennings, D.; Fennessy, F.; Sonka, M.; et al. 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magn. Reson. Imaging 2012, 30, 1323–1341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bickel, P.E.; Tansey, J.T.; Welte, M.A. PAT proteins, an ancient family of lipid droplet proteins that regulate cellular lipid stores. Biochim. Biophys. Acta 2009, 1791, 419–440. [Google Scholar] [CrossRef] [Green Version]
- Loosen, S.H.; Koch, A.; Tacke, F.; Roderburg, C.; Luedde, T. The Role of Adipokines as Circulating Biomarkers in Critical Illness and Sepsis. Int. J. Mol. Sci. 2019, 20, 4820. [Google Scholar] [CrossRef] [Green Version]
- Alipoor, E.; Mohammad Hosseinzadeh, F.; Hosseinzadeh-Attar, M.J. Adipokines in critical illness: A review of the evidence and knowledge gaps. Biomed. Pharmacother. 2018, 108, 1739–1750. [Google Scholar] [CrossRef] [PubMed]
- Wirtz, T.H.; Loosen, S.H.; Buendgens, L.; Kurt, B.; Abu Jhaisha, S.; Hohlstein, P.; Brozat, J.F.; Weiskirchen, R.; Luedde, T.; Tacke, F.; et al. Low Myostatin Serum Levels Are Associated with Poor Outcome in Critically Ill Patients. Diagnostics 2020, 10, 574. [Google Scholar] [CrossRef] [PubMed]
- Rittig, N.; Bach, E.; Thomsen, H.H.; Pedersen, S.B.; Nielsen, T.S.; Jørgensen, J.O.; Jessen, N.; Møller, N. Regulation of Lipolysis and Adipose Tissue Signaling during Acute Endotoxin-Induced Inflammation: A Human Randomized Crossover Trial. PLoS ONE 2016, 11, e0162167. [Google Scholar] [CrossRef]
- Angele, M.K.; Pratschke, S.; Hubbard, W.J.; Chaudry, I.H. Gender differences in sepsis: Cardiovascular and immunological aspects. Virulence 2014, 5, 12–19. [Google Scholar] [CrossRef] [Green Version]
- Failla, K.R.; Connelly, C.D. Systematic Review of Gender Differences in Sepsis Management and Outcomes. J. Nurs. Scholarsh. 2017, 49, 312–324. [Google Scholar] [CrossRef]
- Nachtigall, I.; Tafelski, S.; Rothbart, A.; Kaufner, L.; Schmidt, M.; Tamarkin, A.; Kartachov, M.; Zebedies, D.; Trefzer, T.; Wernecke, K.D.; et al. Gender-related outcome difference is related to course of sepsis on mixed ICUs: A prospective, observational clinical study. Crit. Care 2011, 15, R151. [Google Scholar] [CrossRef] [Green Version]
- De Jong, A.; Wrigge, H.; Hedenstierna, G.; Gattinoni, L.; Chiumello, D.; Frat, J.P.; Ball, L.; Schetz, M.; Pickkers, P.; Jaber, S. How to ventilate obese patients in the ICU. Intensive Care Med. 2020, 46, 2423–2435. [Google Scholar] [CrossRef]
- Pepper, D.J.; Sun, J.; Welsh, J.; Cui, X.; Suffredini, A.F.; Eichacker, P.Q. Increased body mass index and adjusted mortality in ICU patients with sepsis or septic shock: A systematic review and meta-analysis. Crit. Care 2016, 20, 181. [Google Scholar] [CrossRef] [Green Version]
- Carr, R.M.; Peralta, G.; Yin, X.; Ahima, R.S. Absence of perilipin 2 prevents hepatic steatosis, glucose intolerance and ceramide accumulation in alcohol-fed mice. PLoS ONE 2014, 9, e97118. [Google Scholar] [CrossRef]
- Russo, M.; Montone, R.A.; D’Amario, D.; Camilli, M.; Canonico, F.; Santamaria, C.; Iannaccone, G.; Pedicino, D.; Pidone, C.; Galli, M.; et al. Role of perilipin 2 in microvascular obstruction in patients with ST-elevation myocardial infarction. Eur. Heart J. Acute Cardiovasc. Care 2020, 10, 633–642. [Google Scholar] [CrossRef]
- Najt, C.P.; Senthivinayagam, S.; Aljazi, M.B.; Fader, K.A.; Olenic, S.D.; Brock, J.R.; Lydic, T.A.; Jones, A.D.; Atshaves, B.P. Liver-specific loss of Perilipin 2 alleviates diet-induced hepatic steatosis, inflammation, and fibrosis. Am. J. Physiol. Gastrointest. Liver Physiol. 2016, 310, G726–G738. [Google Scholar] [CrossRef] [Green Version]
- Morrissey, J.J.; Mellnick, V.M.; Luo, J.; Siegel, M.J.; Figenshau, R.S.; Bhayani, S.; Kharasch, E.D. Evaluation of Urine Aquaporin-1 and Perilipin-2 Concentrations as Biomarkers to Screen for Renal Cell Carcinoma: A Prospective Cohort Study. JAMA Oncol. 2015, 1, 204–212. [Google Scholar] [CrossRef] [PubMed]
- Morrissey, J.J.; Kharasch, E.D. The specificity of urinary aquaporin 1 and perilipin 2 to screen for renal cell carcinoma. J. Urol. 2013, 189, 1913–1920. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morrissey, J.J.; Mobley, J.; Figenshau, R.S.; Vetter, J.; Bhayani, S.; Kharasch, E.D. Urine aquaporin 1 and perilipin 2 differentiate renal carcinomas from other imaged renal masses and bladder and prostate cancer. Mayo Clin. Proc. 2015, 90, 35–42. [Google Scholar] [CrossRef] [Green Version]
- Morrissey, J.J.; Mobley, J.; Song, J.; Vetter, J.; Luo, J.; Bhayani, S.; Figenshau, R.S.; Kharasch, E.D. Urinary concentrations of aquaporin-1 and perilipin-2 in patients with renal cell carcinoma correlate with tumor size and stage but not grade. Urology 2014, 83, 256.e9–256.e14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cao, Q.; Ruan, H.; Wang, K.; Song, Z.; Bao, L.; Xu, T.; Xiao, H.; Wang, C.; Cheng, G.; Tong, J.; et al. Overexpression of PLIN2 is a prognostic marker and attenuates tumor progression in clear cell renal cell carcinoma. Int. J. Oncol. 2018, 53, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Files, D.C.; Sanchez, M.A.; Morris, P.E. A conceptual framework: The early and late phases of skeletal muscle dysfunction in the acute respiratory distress syndrome. Crit. Care 2015, 19, 266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Muscaritoli, M.; Anker, S.D.; Argilés, J.; Aversa, Z.; Bauer, J.M.; Biolo, G.; Boirie, Y.; Bosaeus, I.; Cederholm, T.; Costelli, P.; et al. Consensus definition of sarcopenia, cachexia and pre-cachexia: Joint document elaborated by Special Interest Groups (SIG) “cachexia-anorexia in chronic wasting diseases” and “nutrition in geriatrics”. Clin. Nutr. 2010, 29, 154–159. [Google Scholar] [CrossRef]
- Aro, R.; Mäkäräinen-Uhlbäck, E.; Ämmälä, N.; Rautio, T.; Ohtonen, P.; Saarnio, J.; Meriläinen, S. The impact of sarcopenia and myosteatosis on postoperative outcomes and 5-year survival in curatively operated colorectal cancer patients—A retrospective register study. Eur. J. Surg. Oncol. 2020, 46, 1656–1662. [Google Scholar] [CrossRef]
- Bredella, M.A.; Ghomi, R.H.; Thomas, B.J.; Torriani, M.; Brick, D.J.; Gerweck, A.V.; Misra, M.; Klibanski, A.; Miller, K.K. Comparison of DXA and CT in the assessment of body composition in premenopausal women with obesity and anorexia nervosa. Obesity 2010, 18, 2227–2233. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coletta, A.M.; Klopp, A.H.; Fogelman, D.; Parikh, A.M.; Li, Y.; Garg, N.; Basen-Engquist, K. Dual-Energy X-Ray Absorptiometry Compared to Computed Tomography for Visceral Adiposity Assessment Among Gastrointestinal and Pancreatic Cancer Survivors. Sci. Rep. 2019, 9, 11500. [Google Scholar] [CrossRef] [PubMed]
- Ninomiya, G.; Fujii, T.; Yamada, S.; Yabusaki, N.; Suzuki, K.; Iwata, N.; Kanda, M.; Hayashi, M.; Tanaka, C.; Nakayama, G.; et al. Clinical impact of sarcopenia on prognosis in pancreatic ductal adenocarcinoma: A retrospective cohort study. Int. J. Surg. 2017, 39, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Stretch, C.; Aubin, J.M.; Mickiewicz, B.; Leugner, D.; Al-Manasra, T.; Tobola, E.; Salazar, S.; Sutherland, F.R.; Ball, C.G.; Dixon, E.; et al. Sarcopenia and myosteatosis are accompanied by distinct biological profiles in patients with pancreatic and periampullary adenocarcinomas. PLoS ONE 2018, 13, e0196235. [Google Scholar] [CrossRef]
- van Dijk, D.P.; Bakens, M.J.; Coolsen, M.M.; Rensen, S.S.; van Dam, R.M.; Bours, M.J.; Weijenberg, M.P.; Dejong, C.H.; Olde Damink, S.W. Low skeletal muscle radiation attenuation and visceral adiposity are associated with overall survival and surgical site infections in patients with pancreatic cancer. J. Cachexia Sarcopenia Muscle 2017, 8, 317–326. [Google Scholar] [CrossRef] [PubMed]
- Tacke, F.; Spehlmann, M.E.; Vucur, M.; Benz, F.; Luedde, M.; Cardenas, D.V.; Roy, S.; Loosen, S.; Hippe, H.J.; Frey, N.; et al. miR-155 Predicts Long-Term Mortality in Critically Ill Patients Younger than 65 Years. Mediators. Inflamm. 2019, 2019, 6714080. [Google Scholar] [CrossRef]
- van Engelen, T.S.R.; Wiersinga, W.J.; Scicluna, B.P.; van der Poll, T. Biomarkers in Sepsis. Crit. Care Clin. 2018, 34, 139–152. [Google Scholar] [CrossRef]
- Langouche, L.; Vander Perre, S.; Frystyk, J.; Flyvbjerg, A.; Hansen, T.K.; Van den Berghe, G. Adiponectin, retinol-binding protein 4, and leptin in protracted critical illness of pulmonary origin. Crit. Care 2009, 13, R112. [Google Scholar] [CrossRef] [Green Version]
- Marques, M.B.; Langouche, L. Endocrine, metabolic, and morphologic alterations of adipose tissue during critical illness. Crit Care Med. 2013, 41, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Venkatesh, B.; Hickman, I.; Nisbet, J.; Cohen, J.; Prins, J. Changes in serum adiponectin concentrations in critical illness: A preliminary investigation. Crit. Care 2009, 13, R105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koch, A.; Sanson, E.; Voigt, S.; Helm, A.; Trautwein, C.; Tacke, F. Serum adiponectin upon admission to the intensive care unit may predict mortality in critically ill patients. J. Crit. Care 2011, 26, 166–174. [Google Scholar] [CrossRef]
- Koch, A.; Weiskirchen, R.; Kunze, J.; Dückers, H.; Bruensing, J.; Buendgens, L.; Matthes, M.; Luedde, T.; Trautwein, C.; Tacke, F. Elevated asymmetric dimethylarginine levels predict short- and long-term mortality risk in critically ill patients. J. Crit. Care 2013, 28, 947–953. [Google Scholar] [CrossRef]
- Koch, A.; Weiskirchen, R.; Bruensing, J.; Dückers, H.; Buendgens, L.; Kunze, J.; Matthes, M.; Luedde, T.; Trautwein, C.; Tacke, F. Regulation and prognostic relevance of symmetric dimethylarginine serum concentrations in critical illness and sepsis. Mediators. Inflamm. 2013, 2013, 413826. [Google Scholar] [CrossRef] [Green Version]
- Matsuguma, K.; Ueda, S.; Yamagishi, S.; Matsumoto, Y.; Kaneyuki, U.; Shibata, R.; Fujimura, T.; Matsuoka, H.; Kimoto, M.; Kato, S.; et al. Molecular mechanism for elevation of asymmetric dimethylarginine and its role for hypertension in chronic kidney disease. J. Am. Soc. Nephrol. 2006, 17, 2176–2183. [Google Scholar] [CrossRef] [Green Version]
- Böger, R.H.; Maas, R.; Schulze, F.; Schwedhelm, E. Asymmetric dimethylarginine (ADMA) as a prospective marker of cardiovascular disease and mortality--an update on patient populations with a wide range of cardiovascular risk. Pharmacol. Res. 2009, 60, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Sibal, L.; Agarwal, S.C.; Home, P.D.; Boger, R.H. The Role of Asymmetric Dimethylarginine (ADMA) in Endothelial Dysfunction and Cardiovascular Disease. Curr. Cardiol. Rev. 2010, 6, 82–90. [Google Scholar] [CrossRef]



| Parameters | r | p |
|---|---|---|
| Demographics | ||
| Age | 0.064 | 0.305 |
| Body mass index | −0.099 | 0.129 |
| FBC and markers of inflammation | ||
| MCHC | 0.166 | 0.007 * |
| Platelets | −0.135 | 0.030 * |
| WBC | −0.109 | 0.080 |
| C-reactive protein | 0.025 | 0.688 |
| Procalcitonin | −0.023 | 0.751 |
| Interleukin 6 | 0.050 | 0.486 |
| Interleukin 10 | 0.092 | 0.303 |
| TNF-α | −0.165 | 0.157 |
| Electrolytes and renal system | ||
| Sodium | −0.101 | 0.105 |
| Potassium | −0.143 | 0.021 * |
| Urea | 0.013 | 0.839 |
| Creatinine | −0.042 | 0.499 |
| HPB system | ||
| Albumin | −0.020 | 0.805 |
| INR | 0.004 | 0.955 |
| Bilirubin, total | −0.056 | 0.369 |
| γGT | −0.099 | 0.115 |
| AST | −0.072 | 0.263 |
| Lipase | −0.509 | <0.001 * |
| Cardiopulmonary system | ||
| NTproBNP | 0.024 | 0.785 |
| Norepinephrine demand at day 1 (µg/kg/min) | 0.066 | 0.322 |
| Horovitz quotient (PaO2/FiO2) | 0.202 | 0.052 |
| Ventilatory FiO2 demand | −0.224 | 0.026* |
| Metabolism and endocrinology | ||
| Glucose | 0.066 | 0.292 |
| HbA1c | −0.090 | 0.355 |
| Insulin | −0.035 | 0.720 |
| C-Peptide | −0.095 | 0.330 |
| HOMA IR | −0.173 | 0.077 |
| Cholesterol | −0.011 | 0.868 |
| HDL-cholesterol | 0.062 | 0.533 |
| LDL-cholesterol | 0.101 | 0.309 |
| Triglycerides | −0.094 | 0.170 |
| ICU parameters | ||
| Days on ICU | 0.132 | 0.034 * |
| SOFA day 1 | 0.149 | 0.113 |
| SOFA day 3 | 0.261 | 0.014 * |
| APACHE-II day 1 | −0.102 | 0.151 |
| APACHE-II day 3 | 0.240 | 0.020 * |
| Parameters | All Patients n = 259 | Non-Sepsis n = 93 | Sepsis n = 166 | p |
|---|---|---|---|---|
| Female (%) | 40.5% | 39.8% | 41% | n.s. |
| Age (years) | 63 (18–89) | 60 (18–85) | 64 (21–89) | n.s. |
| Body mass index (kg/m2) | 26 (15.9–86.5) | 25.8 (15.9–53.3) | 26.1 (17.1–86.5) | n.s. |
| Comorbidities | ||||
| Arterial Hypertension (%) | 23.9 | 26.9 | 22.3 | n.s. |
| Diabetes mellitus (%) | 31.3 | 32.3 | 30.7 | n.s. |
| Coronary artery disease (%) | 12.7 | 15.1 | 11.5 | n.s. |
| COPD (%) | 17.4 | 21.5 | 15.1 | n.s. |
| Liver cirrhosis (%) | 3.1 | 5.4 | 1.8 | n.s. |
| Malignant disease (%) | 11.2 | 7.5 | 13.3 | n.s. |
| Clinical parameters | ||||
| Mechanical ventilation demand at day 1 (%) | 72.2 | 64.5 | 76.5 | 0.039 |
| Norepinephrine demand at day 1 (%) | 59.1 | 46.2 | 66.3 | <0.001 |
| Norepinephrine demand at day 1 (µg/kg/min) | 0 (0–2.4) | 0 (0–2.4) | 0.1 (0–1.5) | 0.001 |
| Renal replacement therapy demand at day 1 (%) | 27.4 | 18.3 | 32.5 | 0.010 |
| Renal replacement therapy (days) | 0 (0–37) | 0 (0–21) | 0 (0–37) | 0.006 |
| APACHE-II score at day 1 | 17 (2–43) | 14 (2–33) | 19 (3–43) | <0.001 |
| APACHE-II score at day 3 | 19 (0–36) | 12 (0–28) | 22 (6–36) | <0.001 |
| SOFA score at day 1 | 9 (0–19) | 7 (0–17) | 10 (3–19) | <0.001 |
| SOFA score at day 3 | 9 (0–18) | 6 (0–15) | 10 (1–18) | <0.001 |
| Days on ICU | 8 (2–137) | 6 (2–45) | 10 (2–137) | <0.001 |
| Death on ICU (%) | 24.7 | 17.2 | 28.9 | 0.036 |
| 180-day mortality (%) | 20.8 | 17.2 | 22.9 | n.s. |
| Observation period (days) | 137 (1–884) | 195.5 (1–883) | 110 (1–884) | n.s. |
| Overall mortality (%) | 47.5 | 34.0 | 54.8 | 0.002 |
| Laboratory data at day 1: | ||||
| WBC [×103/μL] | 12.7 (0–149) | 11.4 (1.8–29.6) | 13.1 (0–149) | 0.011 |
| C-reactive protein [mg/dL] | 97 (5–230) | 17 (5–230) | 161.5 (5–230) | <0.001 |
| Procalcitonin [ng/mL] | 0.8 (0–248) | 0.2 (0–100) | 2.7 (0.1–248) | <0.001 |
| Creatinine [mg/dL] | 1.4 (0.2–21.6) | 1 (0.2–15) | 1.6 (0.2–21.6) | 0.025 |
| Creatinine GFR [mL/min] | 54 (2–60) | 60 (6–60) | 38 (2–60) | 0.004 |
| INR [units] | 1.2 (0.9–6.7) | 1.2 (0.9–6.7) | 1.2 (0.9–4.6) | n.s. |
| Albumin [mg/dL] | 27 (1.6–61.4) | 30.1 (1.6–48.5) | 25.6 (5–61.4) | 0.005 |
| Lactate [mmol/l] | 1.6 (0.4–21.9) | 1.8 (0.6–18.1) | 1.5 (0.4–21.9) | 0.094 |
| PLIN2 [µg/dL] | 5.23 (0.48–59.5) | 4.86 (1.4–32.4) | 5.47 (0.48–59.5) | 0.021 |
| Sepsis occurrence at ICU admission | OR (95% CI) | p |
| Unadjusted | 1.72 (1.03–2.88) | 0.038 |
| Adjusted for age and DM | 1.71 (1.02–2.87) | 0.042 |
| Adjusted for CRP | 1.75 (0.94–3.28) | 0.079 |
| Adjusted for CRP and PCT | 2.07 (0.98–4.38) | 0.058 |
| Adjusted for norepinephrine demand | 1.73 (1.01–2.98) | 0.047 |
| SOFA > 9 points at ICU admission | OR (95% CI) | p |
| Unadjusted | 3.13 (1.36–7.20) | 0.007 |
| Adjusted for age and DM | 2.96 (1.27–6.88) | 0.012 |
| Adjusted for CRP | 3.07 (1.33–7.09) | 0.009 |
| Adjusted for CRP and PCT | 2.62 (0.67–10.24) | 0.166 |
| Adjusted for norepinephrine demand | 2.72 (1.08–6.89) | 0.035 |
| SOFA > 9 points at day 3 | OR (95% CI) | p |
| Unadjusted | 3.08 (1.25–7.60) | 0.015 |
| Adjusted for age and DM | 2.91 (1.16–7.29) | 0.023 |
| Adjusted for CRP | 2.93 (1.17–7.32) | 0.021 |
| Adjusted for CRP and PCT | 15.93 (2.85–88.93) | 0.002 |
| Adjusted for norepinephrine demand | 2.79 (1.05–7.42) | 0.040 |
| r|p | VAT [mm2] | SAT [mm2] | Skeletal Muscle [mm2] | Skeletal Muscle Mean HU | L3SMI |
|---|---|---|---|---|---|
| All patients | −0.004|0.983 | −0.160|0.353 | −0.152|0.377 | −0.213|0.213 | −0.095|0.592 |
| BMI < 30 kg/m2 | −0.015|0.942 | −0.214|0.305 | −0.002|0.991 | −0.261|0.208 | 0.033|0.875 |
| BMI ≥ 30 kg/m2 | −0.750|0.020 * | −0.517|0.154 | −0.567|0.112 | 0.259|0.500 | −0.533|0.139 |
| Age < 65 years | −0.030|0.898 | −0.156|0.500 | −0.138|0.552 | −0.152|0.510 | −0.072|0.770 |
| Age ≥ 65 years | 0.061|0.830 | −0.036|0.899 | −0.146|0.603 | −0.152|0.589 | −0.079|0.781 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kurt, B.; Buendgens, L.; Wirtz, T.H.; Loosen, S.H.; Schulze-Hagen, M.; Truhn, D.; Brozat, J.F.; Abu Jhaisha, S.; Hohlstein, P.; Koek, G.; et al. Serum Perilipin 2 (PLIN2) Predicts Multiple Organ Dysfunction in Critically Ill Patients. Biomedicines 2021, 9, 1210. https://doi.org/10.3390/biomedicines9091210
Kurt B, Buendgens L, Wirtz TH, Loosen SH, Schulze-Hagen M, Truhn D, Brozat JF, Abu Jhaisha S, Hohlstein P, Koek G, et al. Serum Perilipin 2 (PLIN2) Predicts Multiple Organ Dysfunction in Critically Ill Patients. Biomedicines. 2021; 9(9):1210. https://doi.org/10.3390/biomedicines9091210
Chicago/Turabian StyleKurt, Berkan, Lukas Buendgens, Theresa H. Wirtz, Sven H. Loosen, Maximilian Schulze-Hagen, Daniel Truhn, Jonathan F. Brozat, Samira Abu Jhaisha, Philipp Hohlstein, Ger Koek, and et al. 2021. "Serum Perilipin 2 (PLIN2) Predicts Multiple Organ Dysfunction in Critically Ill Patients" Biomedicines 9, no. 9: 1210. https://doi.org/10.3390/biomedicines9091210
APA StyleKurt, B., Buendgens, L., Wirtz, T. H., Loosen, S. H., Schulze-Hagen, M., Truhn, D., Brozat, J. F., Abu Jhaisha, S., Hohlstein, P., Koek, G., Weiskirchen, R., Trautwein, C., Tacke, F., Hamesch, K., & Koch, A. (2021). Serum Perilipin 2 (PLIN2) Predicts Multiple Organ Dysfunction in Critically Ill Patients. Biomedicines, 9(9), 1210. https://doi.org/10.3390/biomedicines9091210









