Impact of Frailty on Hippocampal Volume in Patients with Chronic Obstructive Pulmonary Disease
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Clinical Assessments
2.3. Neuroimaging Analysis
2.4. Statistics
3. Results
3.1. Association between QOL and Frailty and Depressive Symptoms
3.2. Association between Frailty and Depressive Symptoms
3.3. Association between Volume of Hippocampal Subfields and Frailty and Depressive Symptoms
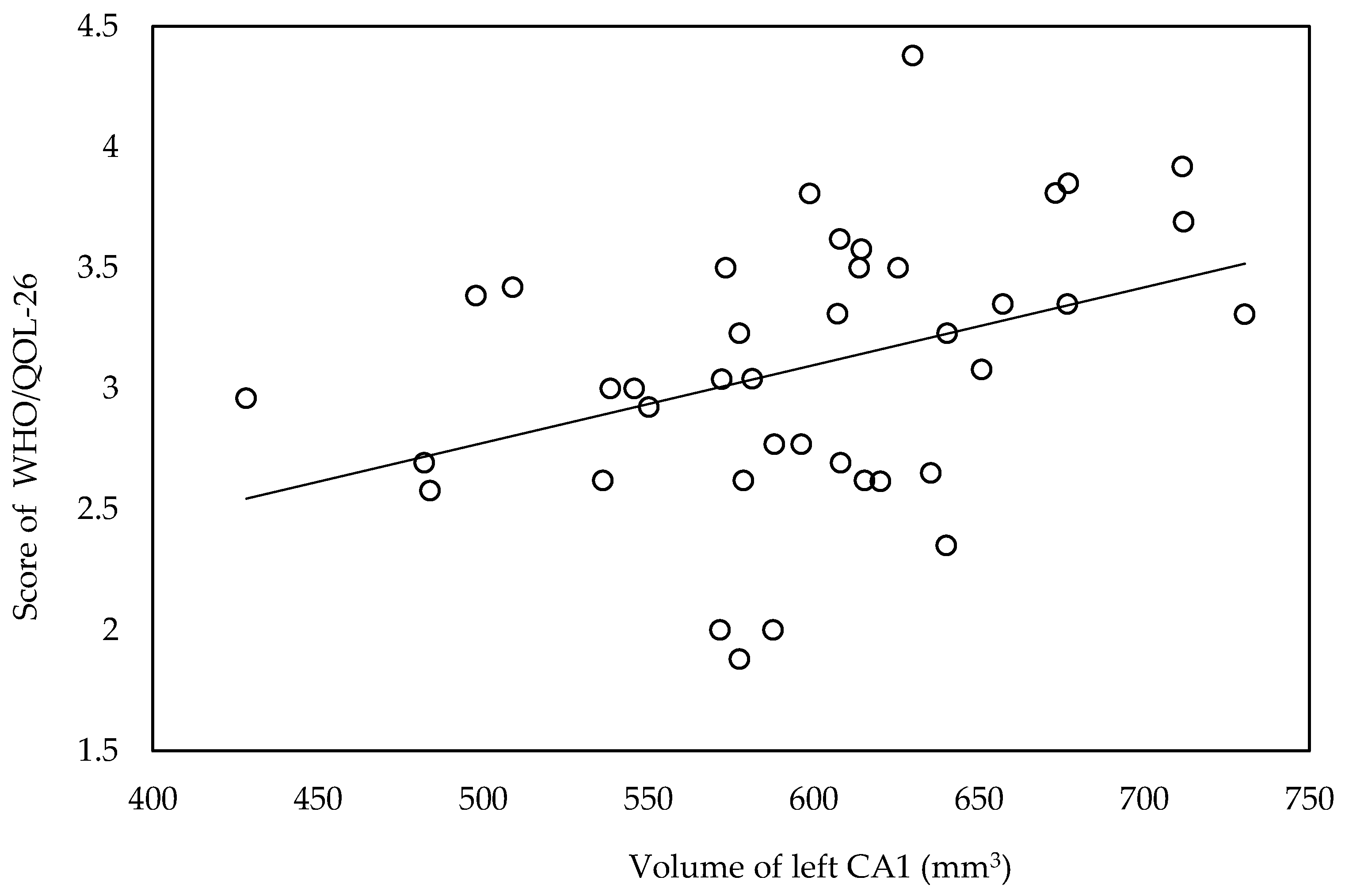
3.4. Association between Hippocampal Subfield Volume and QOL
3.5. Association between Respiratory Values with QOL, Frailty, Depressive Symptoms and Hippocampal Subfield Volume
3.6. Step-Wise Multiple Regression Analyses for the Correlated Factors
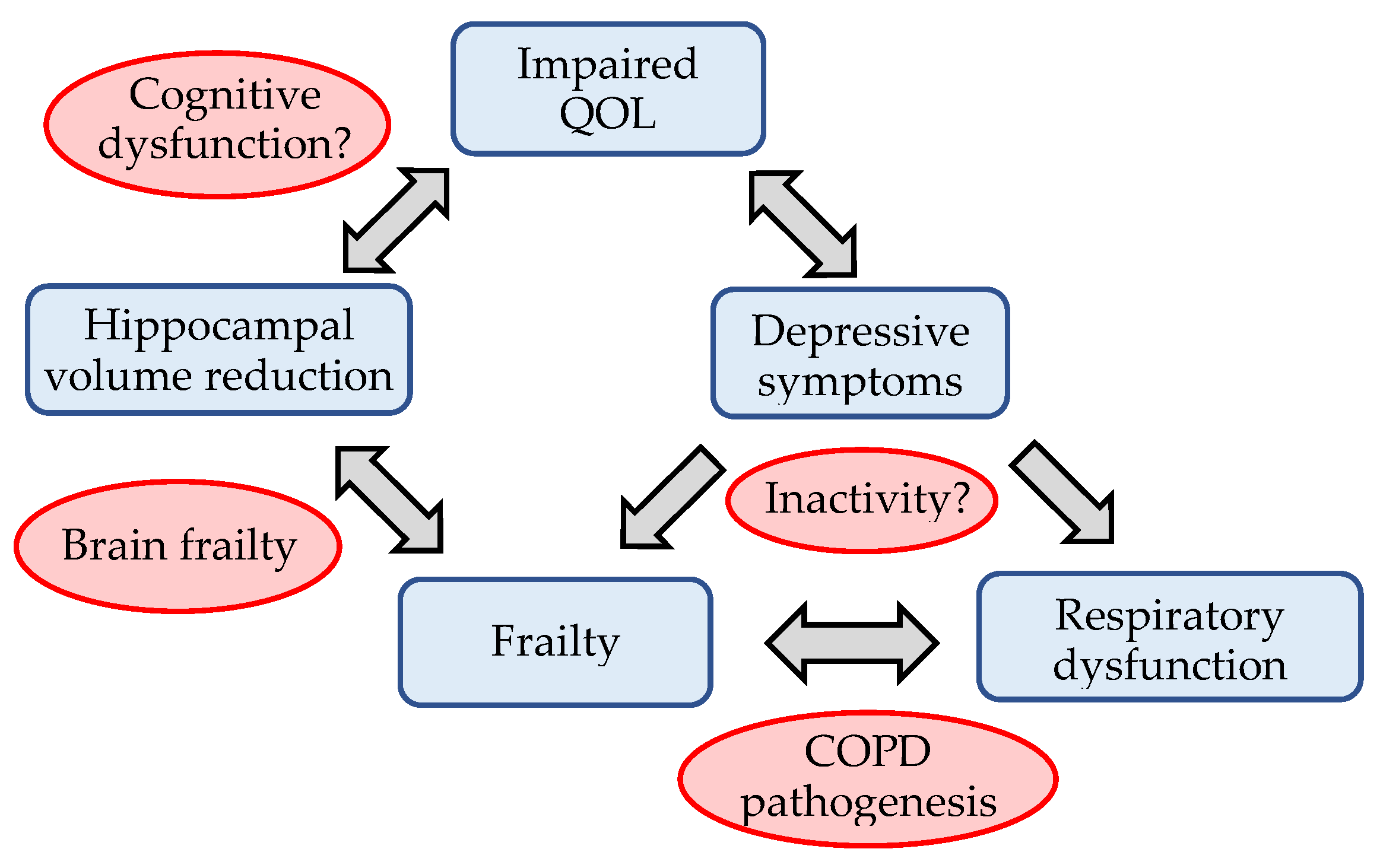
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rabe, K.F.; Watz, H. Chronic obstructive pulmonary disease. Lancet 2017, 389, 1931–1940. [Google Scholar] [CrossRef]
- Yorgancioglu, A.; Havlucu, Y.; Celik, P.; Dinc, G.; Saka, A. Relation between quality of life and morbidity and mortality in COPD patients: Two-year follow-up study. COPD 2010, 7, 248–253. [Google Scholar] [CrossRef]
- Agusti, A.; Soriano, J.B. COPD as a systemic disease. COPD 2008, 5, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Decramer, M.; Janssens, W.; Miravitlles, M. Chronic obstructive pulmonary disease. Lancet 2012, 379, 1341–1351. [Google Scholar] [CrossRef]
- Hirano, T.; Doi, K.; Matsunaga, K.; Takahashi, S.; Donishi, T.; Suga, K.; Oishi, K.; Yasuda, K.; Mimura, Y.; Harada, M.; et al. A novel role of growth differentiation factor (GDF)-15 in overlap with sedentary lifestyle and cognitive risk in COPD. J. Clin. Med. 2020, 9, 2737. [Google Scholar] [CrossRef] [PubMed]
- Matsunaga, K.; Harada, M.; Suizu, J.; Oishi, K.; Asami-Noyama, M.; Hirano, T. Comorbid conditions in chronic obstructive pulmonary disease: Potential therapeutic targets for unmet needs. J. Clin. Med. 2020, 9, 3078. [Google Scholar] [CrossRef]
- Oishi, K.; Matsunaga, K.; Harada, M.; Suizu, J.; Murakawa, K.; Chikumoto, A.; Ohteru, Y.; Matsuda, K.; Uehara, S.; Hamada, K.; et al. A new dyspnea evaluation system focusing on patients’ perceptions of dyspnea and their living disabilities: The linkage between COPD and frailty. J. Clin. Med. 2020, 9, 3580. [Google Scholar] [CrossRef]
- Marengoni, A.; Vetrano, D.L.; Manes-Gravina, E.; Bernabei, R.; Onder, G.; Palmer, K. The relationship between COPD and frailty: A systematic review and meta-analysis of observational studies. Chest 2018, 154, 21–40. [Google Scholar] [CrossRef]
- Matte, D.L.; Pizzichini, M.M.; Hoepers, A.T.; Diaz, A.P.; Karloh, M.; Dias, M.; Pizzichini, E. Prevalence of depression in COPD: A systematic review and meta-analysis of controlled studies. Respir Med. 2016, 117, 154–161. [Google Scholar] [CrossRef]
- Kennedy, C.C.; Novotny, P.J.; LeBrasseur, N.K.; Wise, R.A.; Sciurba, F.C.; Benzo, R.P. Frailty and clinical outcomes in chronic obstructive pulmonary disease. Ann. Am. Thorac. Soc. 2019, 16, 217–224. [Google Scholar] [CrossRef]
- Lahousse, L.; Ziere, G.; Verlinden, V.J.; Zillikens, M.C.; Uitterlinden, A.G.; Rivadeneira, F.; Tiemeier, H.; Joos, G.F.; Hofman, A.; Ikram, M.A.; et al. Risk of frailty in elderly with COPD: A population-based study. J. Gerontol. A Biol. Sci. Med. Sci. 2016, 71, 689–695. [Google Scholar] [CrossRef] [PubMed]
- Bernabeu-Mora, R.; Oliveira-Sousa, S.L.; Sánchez-Martínez, M.P.; García-Vidal, J.A.; Gacto-Sánchez, M.; Medina-Mirapeix, F. Frailty transitions and associated clinical outcomes in patients with stable COPD: A longitudinal study. PLoS ONE 2020, 15, e0230116. [Google Scholar] [CrossRef]
- Yohannes, A.M.; Willgoss, T.G.; Baldwin, R.C.; Connolly, M.J. Depression and anxiety in chronic heart failure and chronic obstructive pulmonary disease: Prevalence, relevance, clinical implications and management principles. Int. J. Geriatr. Psychiatry 2010, 25, 1209–1221. [Google Scholar] [CrossRef]
- Yohannes, A.M.; Alexopoulos, G.S. Depression and anxiety in patients with COPD. Eur Respir Rev. 2014, 23, 345–349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lou, P.; Chen, P.; Zhang, P.; Yu, J.; Wang, Y.; Chen, N.; Zhang, L.; Wu, H.; Zhao, J. Effects of smoking, depression, and anxiety on mortality in COPD patients: A prospective study. Respir. Care 2014, 59, 54–61. [Google Scholar] [CrossRef] [Green Version]
- Panagioti, M.; Scott, C.; Blakemore, A.; Coventry, P.A. Overview of the prevalence, impact, and management of depression and anxiety in chronic obstructive pulmonary disease. Int. J. Chron. Obstruct. Pulmon. Dis. 2014, 9, 1289–1306. [Google Scholar] [PubMed] [Green Version]
- Connolly, M.J.; Yohannes, A.M. The impact of depression in older patients with chronic obstructive pulmonary disease and asthma. Maturitas 2016, 92, 9–14. [Google Scholar] [CrossRef]
- Rivera, C.M.; Galicia, J.C.; Navarrete, B.A.; Garcia-Polo, C.; Iturriaga, L.A.R.; Herrejón, A.; Lucas, J.A.R.; García-Sidro, P.; Tirado-Conde, G.; López-Campos, J.L.; et al. Factors associated with depression in COPD: A multicenter study. Lung 2016, 194, 335–343. [Google Scholar] [CrossRef]
- Atlantis, E.; Fahey, P.; Cochrane, B.; Smith, S. Bidirectional associations between clinically relevant depression or anxiety and COPD: A systematic review and meta-analysis. Chest 2013, 144, 766–777. [Google Scholar] [CrossRef]
- Soysal, P.; Veronese, N.; Thompson, T.; Kahl, K.G.; Fernandes, B.S.; Prina, A.M.; Solmi, M.; Schofield, P.; Koyanagi, A.; Tseng, P.T.; et al. Relationship between depression and frailty in older adults: A systematic review and meta-analysis. Ageing Res. Rev. 2017, 36, 78–87. [Google Scholar] [CrossRef] [Green Version]
- Lahousse, L.; Tiemeier, H.; Ikram, M.A.; Brusselle, G.G. Chronic obstructive pulmonary disease and cerebrovascular disease: A comprehensive review. Respir. Med. 2015, 109, 1371–1380. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yin, M.; Wang, H.; Hu, X.; Li, X.; Fei, G.; Yu, Y. Patterns of brain structural alteration in COPD with different levels of pulmonary function impairment and its association with cognitive deficits. BMC Pulm. Med. 2019, 19, 203. [Google Scholar] [CrossRef] [Green Version]
- Kim, E.J.; Pellman, B.; Kim, J.J. Stress effects on the hippocampus: A critical review. Learn. Mem. 2015, 22, 411–416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Esser, R.W.; Stoeckel, M.C.; Kirsten, A.; Watz, H.; Taube, K.; Lehmann, K.; Petersen, S.; Magnussen, H.; von Leupoldt, A. Structural Brain Changes in Patients With COPD. Chest 2016, 149, 426–434. [Google Scholar] [CrossRef]
- Li, J.; Fei, G.H. The unique alterations of hippocampus and cognitive impairment in chronic obstructive pulmonary disease. Respir. Res. 2013, 14, 140. [Google Scholar] [CrossRef] [Green Version]
- Chen, W.T.; Chou, K.H.; Liu, L.K.; Lee, P.L.; Lee, W.J.; Chen, L.K.; Wang, P.N.; Lin, C.P. Reduced cerebellar gray matter is a neural signature of physical frailty. Hum. Brain Mapp. 2015, 36, 3666–3676. [Google Scholar] [CrossRef]
- Nishita, Y.; Nakamura, A.; Kato, T.; Otsuka, R.; Iwata, K.; Tange, C.; Ando, F.; Ito, K.; Shimokata, H.; Arai, H. Links Between Physical Frailty and Regional Gray Matter Volumes in Older Adults: A Voxel-Based Morphometry Study. J. Am. Med. Dir. Assoc. 2019, 20, 1587–1592. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Videbech, P.; Ravnkilde, B. Hippocampal volume and depression: A meta-analysis of MRI studies. Am. J. Psychiatry 2004, 161, 1957–1966. [Google Scholar] [CrossRef]
- Sewo Sampaio, P.Y.; Sampaio, R.A.; Yamada, M.; Arai, H. Systematic review of the Kihon Checklist: Is it a reliable assessment of frailty? Geriatr. Gerontol. Int. 2016, 16, 893–902. [Google Scholar] [CrossRef] [PubMed]
- Kusunose, M.; Oga, T.; Nakamura, S.; Hasegawa, Y.; Nishimura, K. Frailty and patient-reported outcomes in subjects with chronic obstructive pulmonary disease: Are they independent entities? BMJ Open Respir. Res. 2017, 4, e000196. [Google Scholar] [CrossRef] [Green Version]
- Guan, C.; Niu, H. Frailty assessment in older adults with chronic obstructive respiratory diseases. Clin. Interv. Aging 2018, 13, 1513–1524. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hirai, K.; Tanaka, A.; Homma, T.; Kaneko, K.; Uno, T.; Sato, H.; Manabe, R.; Ohta, S.; Kusumoto, S.; Yamaguchi, F.; et al. Comparison of three frailty models and a sarcopenia model in elderly patients with chronic obstructive pulmonary disease. Geriatr. Gerontol. Int. 2019, 19, 896–901. [Google Scholar] [CrossRef]
- Satake, S.; Senda, K.; Hong, Y.J.; Miura, H.; Endo, H.; Sakurai, T.; Kondo, I.; Toba, K. Validity of the Kihon Checklist for assessing frailty status. Geriatr. Gerontol. Int. 2016, 16, 709–715. [Google Scholar] [CrossRef]
- Kugaya, A.; Akechi, T.; Okuyama, T.; Okamura, H.; Uchitomi, Y. Screening for psychological distress in Japanese cancer patients. Jpn. J. Clin. Oncol. 1998, 28, 333–338. [Google Scholar] [CrossRef]
- Park, S.K.; Richardson, C.R.; Holleman, R.G.; Larson, J.L. Frailty in people with COPD, using the National Health and Nutrition Evaluation Survey dataset (2003-2006). Heart Lung 2013, 42, 163–170. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Mara, S. The subiculum: What it does, what it might do, and what neuroanatomy has yet to tell us. J. Anat. 2005, 207, 271–282. [Google Scholar] [CrossRef]
- Honda, Y.; Fururta, T. Multiple Patterns of Axonal Collateralization of Single Layer III Neurons of the Rat Presubiculum. Front. Neural. Circuits 2019, 13, 45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dalton, M.A.; Maguire, E.A. The pre/parasubiculum: A hippocampal hub for scene-based cognition? Curr. Opin. Behav. Sci. 2017, 17, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Campbell, S.; Macqueen, G. The role of the hippocampus in the pathophysiology of major depression. J. Psychiatry Neurosci. 2004, 29, 417–426. [Google Scholar]
- Roddy, D.W.; Farrell, C.; Doolin, K.; Roman, E.; Tozzi, L.; Frodl, T.; O’Keane, V.; O’Hanlon, E. The Hippocampus in Depression: More Than the Sum of Its Parts? Advanced Hippocampal Substructure Segmentation in Depression. Biol. Psychiatry 2019, 85, 487–497. [Google Scholar] [CrossRef]
- MacQueen, G.; Frodl, T. The hippocampus in major depression: Evidence for the convergence of the bench and bedside in psychiatric research? Mol. Psychiatry 2011, 16, 252–264. [Google Scholar] [CrossRef] [Green Version]
- Watanabe, R.; Kakeda, S.; Watanabe, K.; Liu, X.; Katsuki, A.; Umeno-Nakano, W.; Hori, H.; Abe, O.; Yoshimura, R.; Korogi, Y. Relationship between the hippocampal shape abnormality and serum cortisol levels in first-episode and drug-naïve major depressive disorder patients. Depress. Anxiety 2017, 34, 401–409. [Google Scholar] [CrossRef] [PubMed]
- Han, K.M.; Won, E.; Sim, Y.; Tae, W.S. Hippocampal subfield analysis in medication-naive female patients with major depressive disorder. J. Affect. Disord. 2016, 194, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Han, K.M.; Kim, A.; Kang, W.; Kang, Y.; Kang, J.; Won, E.; Tae, W.S.; Ham, B.J. Hippocampal subfield volumes in major depressive disorder and bipolar disorder. Eur. Psychiatry 2019, 57, 70–77. [Google Scholar] [CrossRef]
- Pumar, M.I.; Gray, C.R.; Walsh, J.R.; Yang, I.A.; Rolls, T.A.; Ward, D.L. Anxiety and depression-Important psychological comorbidities of COPD. J. Thorac. Dis. 2014, 6, 1615–1631. [Google Scholar] [PubMed]
- Tselebis, A.; Pachi, A.; Ilias, I.; Kosmas, E.; Bratis, D.; Moussas, G.; Tzanakis, N. Strategies to improve anxiety and depression in patients with COPD: A mental health perspective. Neuropsychiatr Dis Treat. 2016, 12, 297–328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Shair, K.; Kolsum, U.; Dockry, R.; Morris, J.; Singh, D.; Vestbo, J. Biomarkers of systemic inflammation and depression and fatigue in moderate clinically stable COPD. Respir. Res. 2011, 12, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eagan, T.M.; Ueland, T.; Wagner, P.D.; Hardie, J.A.; Mollnes, T.E.; Damås, J.K.; Aukrust, P.; Bakke, P.S. Systemic inflammatory markers in COPD: Results from the Bergen COPD Cohort Study. Eur. Respir. J. 2010, 35, 540–548. [Google Scholar] [CrossRef] [Green Version]
- Rybka, J.; Korte, S.M.; Czajkowska-Malinowska, M.; Wiese, M.; Kędziora-Kornatowska, K.; Kędziora, J. The links between chronic obstructive pulmonary disease and comorbid depressive symptoms: Role of IL-2 and IFN-gamma. Clin. Exp. Med. 2016, 16, 493–502. [Google Scholar] [CrossRef] [Green Version]
- Lu, Y.; Feng, L.; Feng, L.; Nyunt, M.S.; Yap, K.B.; Ng, T.P. Systemic inflammation, depression and obstructive pulmonary function: A population-based study. Respir. Res. 2013, 14, 53. [Google Scholar] [CrossRef] [Green Version]
- Xu, X.; Sun, Y.; Holmes, T.C.; López, A.J. Noncanonical connections between the subiculum and hippocampal CA1. J. Comp. Neurol. 2016, 524, 3666–3673. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, N.; Kitanishi, T.; Mizuseki, K. The subiculum: Unique hippocampal hub and more. Neurosci. Res. 2019, 143, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Al-Gamal, E. Quality of life, anxiety and depression among patients with chronic obstructive pulmonary disease and their spouses. Issues Ment Health Nurs. 2014, 35, 761–767. [Google Scholar] [CrossRef] [PubMed]
- Fan, V.S.; Curtis, J.R.; Tu, S.P.; McDonell, M.B.; Fihn, S.D.; Ambulatory Care Quality Improvement Project Investigators. Using quality of life to predict hospitalization and mortality in patients with obstructive lung diseases. Chest 2002, 122, 429–436. [Google Scholar] [CrossRef]
- Altenburg, W.A.; Bossenbroek, L.; de Greef, M.H.; Kerstjens, H.A.; ten Hacken, N.H.; Wempe, J.B. Functional and psychological variables both affect daily physical activity in COPD: A structural equations model. Respir. Med. 2013, 107, 1740–1747. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miravitlles, M.; Cantoni, J.; Naberan, K. Factors associated with a low level of physical activity in patients with chronic obstructive pulmonary disease. Lung 2014, 192, 259–265. [Google Scholar] [CrossRef] [PubMed]
- Dueñas-Espín, I.; Demeyer, H.; Gimeno-Santos, E.; Polkey, M.I.; Hopkinson, N.S.; Rabinovich, R.A.; Dobbels, F.; Karlsson, N.; Troosters, T.; Garcia-Aymerich, J. Depression symptoms reduce physical activity in COPD patients: A prospective multicenter study. Int. J. Chron. Obstruct. Pulmon. Dis. 2016, 11, 1287–1295. [Google Scholar] [CrossRef] [Green Version]
- Feng, L.; Nyunt, M.S.; Feng, L.; Yap, K.B.; Ng, T.P. Frailty predicts new and persistent depressive symptoms among community-dwelling older adults: Findings from Singapore longitudinal aging study. J. Am. Med. Dir. Assoc. 2014, 15, 76.e7–76.e12. [Google Scholar] [CrossRef]
- Erickson, K.I.; Voss, M.W.; Prakash, R.S.; Basak, C.; Szabo, A.; Chaddock, L.; Kim, J.S.; Heo, S.; Alves, H.; White, S.M.; et al. Exercise training increases size of hippocampus and improves memory. Proc. Natl. Acad. Sci. USA 2011, 108, 3017–3022. [Google Scholar] [CrossRef] [Green Version]
- Erickson, K.I.; Leckie, R.L.; Weinstein, A.M. Physical activity, fitness, and gray matter volume. Neurobiol. Aging 2014, 35 (Suppl. 2), S20–S28. [Google Scholar] [CrossRef] [Green Version]
- Andenaes, R.; Moum, T.; Kalfoss, M.H.; Wahl, A.K. Changes in health status, psychological distress, and quality of life in COPD patients after hospitalization. Qual. Life Res. 2006, 15, 249–257. [Google Scholar] [CrossRef]
- Liang, W.M.; Chen, J.J.; Chang, C.H.; Chen, H.W.; Chen, S.L.; Hang, L.W.; Wang, J.D. An empirical comparison of the WHOQOL-BREF and the SGRQ among patients with COPD. Qual. Life Res. 2008, 17, 793–800. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akashiba, T.; Kawahara, S.; Akahoshi, T.; Omori, C.; Saito, O.; Majima, T.; Horie, T. Relationship between quality of life and mood or depression in patients with severe obstructive sleep apnea syndrome. Chest 2002, 122, 861–865. [Google Scholar] [CrossRef] [PubMed]
- Pauletto, P.; Réus, J.C.; Bolan, M.; Massignan, C.; Flores-Mir, C.; Maia, I.; Gozal, D.; Hallal, A.L.C.; Porporatti, A.L.; Canto, G.L. Association between obstructive sleep apnea and health-related quality of life in untreated adults: A systematic review. Sleep Breath 2021, in press. [Google Scholar] [CrossRef] [PubMed]
- Dusak, A.; Ursavas, A.; Hakyemez, B.; Gokalp, G.; Taskapilioglu, O.; Parlak, M. Correlation between hippocampal volume and excessive daytime sleepiness in obstructive sleep apnea syndrome. Eur. Rev. Med. Pharmacol. Sci. 2013, 17, 1198–1204. [Google Scholar] [PubMed]

| Measure | Mean | S.D. |
|---|---|---|
| Gender (male/female) | 39/1 | |
| Age (years) | 70.63 | 8.21 |
| BMI (kg/m2) | 23.26 | 3.29 |
| Smoking status (Cu/Ex/Non) | 12/28/0 | |
| Pack years | 46.60 | 25.49 |
| %VC (%) | 97.00 | 18.67 |
| %FVC (%) | 98.70 | 19.26 |
| %FEV1 (%) | 73.96 | 18.07 |
| %DLco/VA (%) | 77.84 | 24.10 |
| HADS | 12.83 | 7.09 |
| KCL | 8.30 | 5.08 |
| WHO/QOL-26 | 3.09 | 0.56 |
| WHO/QOL-26 | KCL | HADS | |
|---|---|---|---|
| WHO/QOL-26 | 1 | ||
| KCL | −0.596 * | 1 | |
| HADS | −0.723 * | 0.560 * | 1 |
| KCL | ||
|---|---|---|
| r | p | |
| Left whole hippocampus | −0.458 | 0.004 |
| Right whole hippocampus | −0.410 | 0.011 |
| Left subiculum | −0.518 | 0.001 |
| Left presubiculum | −0.401 | 0.013 |
| Right subiculum | −0.497 | 0.001 |
| Right presubiculum | −0.493 | 0.002 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Takahashi, S.; Hirano, T.; Yasuda, K.; Donishi, T.; Suga, K.; Doi, K.; Oishi, K.; Ohata, S.; Murata, Y.; Yamaji, Y.; et al. Impact of Frailty on Hippocampal Volume in Patients with Chronic Obstructive Pulmonary Disease. Biomedicines 2021, 9, 1103. https://doi.org/10.3390/biomedicines9091103
Takahashi S, Hirano T, Yasuda K, Donishi T, Suga K, Doi K, Oishi K, Ohata S, Murata Y, Yamaji Y, et al. Impact of Frailty on Hippocampal Volume in Patients with Chronic Obstructive Pulmonary Disease. Biomedicines. 2021; 9(9):1103. https://doi.org/10.3390/biomedicines9091103
Chicago/Turabian StyleTakahashi, Shun, Tsunahiko Hirano, Kasumi Yasuda, Tomohiro Donishi, Kazuyoshi Suga, Keiko Doi, Keiji Oishi, Shuichiro Ohata, Yoriyuki Murata, Yoshikazu Yamaji, and et al. 2021. "Impact of Frailty on Hippocampal Volume in Patients with Chronic Obstructive Pulmonary Disease" Biomedicines 9, no. 9: 1103. https://doi.org/10.3390/biomedicines9091103
APA StyleTakahashi, S., Hirano, T., Yasuda, K., Donishi, T., Suga, K., Doi, K., Oishi, K., Ohata, S., Murata, Y., Yamaji, Y., Asami-Noyama, M., Edakuni, N., & Matsunaga, K. (2021). Impact of Frailty on Hippocampal Volume in Patients with Chronic Obstructive Pulmonary Disease. Biomedicines, 9(9), 1103. https://doi.org/10.3390/biomedicines9091103






