Pediatric Psoriasis: From New Insights into Pathogenesis to Updates on Treatment
Abstract
:1. Introduction
2. Clinical Presentation of Pediatric Psoriasis
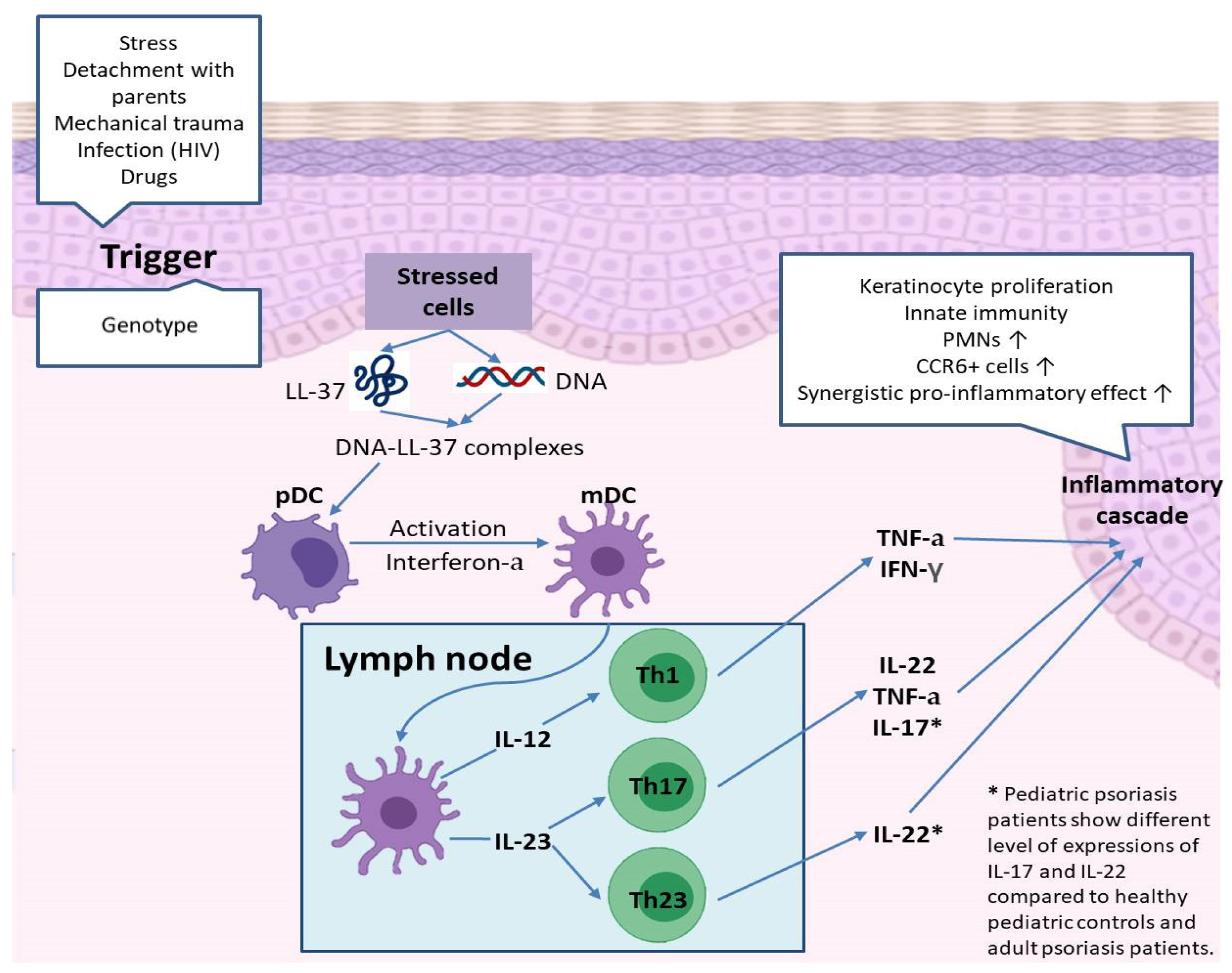
3. Etiopathogenesis of Pediatric Psoriasis
4. Treatments of Pediatric Psoriasis
4.1. Topical Treatments
4.1.1. Emollients and Keratolytics
4.1.2. Topical Corticosteroids
4.1.3. Topical Calcineurin Inhibitors (TCI)
4.1.4. Topical Vitamin D Analogues
4.1.5. Other Topical Agents
4.2. Phototherapy
4.3. Systemic Treatments
4.3.1. Methotrexate
4.3.2. Cyclosporine
4.3.3. Systemic Retinoids
4.3.4. Systemic Fumaric Acid Esters
4.3.5. Other Systemic Agents
4.4. Biologic Therapy
4.4.1. Etanercept
4.4.2. Adalimumab
4.4.3. Ustekinumab
4.4.4. Infliximab
4.4.5. Secukinumab
4.4.6. Ixekizumab
4.4.7. Guselkumab
4.4.8. Risankizumab
4.4.9. Tofacitinib
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| IL | Interleukin |
| Th | T helper cell |
| INF-a | Interferon alpha |
| TNF-a | Tumor necrosis factor alpha |
| HPA | Hypothalamic–Pituitary–Adrenal |
| FDA | US Food and Drug Administration |
| PASI | Psoriasis Area and Severity Index |
| CDLQI | Children’s Dermatology Life Quality Index |
| AhR | Aryl hydrocarbon receptor |
| NB-UVB | Narrow band ultraviolet-B |
| UVA | Ultraviolet-A |
| MTX | Methotrexate |
| IBD | Inflammatory bowel disease |
| PGA | Physician global assessment |
| SC | Subcutaneous |
| EMA | European Medicines Association |
| JAK | Janus kinase |
References
- Bronckers, I.M.; Paller, A.S.; van Geel, M.J.; van de Kerkhof, P.C.; Seyger, M.M. Psoriasis in Children and Adolescents: Diagnosis, Management and Comorbidities. Paediatr. Drugs 2015, 17, 373–384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tollefson, M.M.; Crowson, C.S.; McEvoy, M.T.; Maradit Kremers, H. Incidence of psoriasis in children: A population-based study. J. Am. Acad. Dermatol. 2010, 62, 979–987. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parisi, R.; Symmons, D.P.; Griffiths, C.E.; Ashcroft, D.M. Identification and Management of Psoriasis and Associated ComorbidiTy (IMPACT) project team. Global epidemiology of psoriasis: A systematic review of incidence and prevalence. J. Investig. Dermatol. 2013, 133, 377–385. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pietrzak, A.; Grywalska, E.; Walankiewicz, M.; Lotti, T.; Roliński, J.; Myśliński, W.; Chabros, P.; Piekarska-Myślińska, D.; Reich, K. Psoriasis and metabolic syn-drome in children: Current data. Clin. Exp. Dermatol. 2017, 42, 131–136. [Google Scholar] [CrossRef]
- Becker, L.; Tom, W.L.; Eshagh, K.; Benjamin, L.T.; Paller, A.S. Excess adiposity preceding pediatric psoriasis. JAMA Dermatol. 2014, 150, 573–574. [Google Scholar] [CrossRef] [Green Version]
- Jensen, P.; Zachariae, C.; Christensen, R.; Geiker, N.R.W.; Schaadt, B.K.; Stender, S.; Hansen, P.R.; Astrup, A.; Skov, L. Effect of weight loss on the severity of psoriasis: A randomized clinical study. JAMA Dermatol. 2013, 149, 795–801. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.T.; Yeh, H.M.; Liu, S.Y.; Chen, K.T. Psoriatic arthritis: Epidemiology, diagnosis, and treatment. World J. Orthop. 2014, 5, 537–543. [Google Scholar] [CrossRef] [PubMed]
- Chiam, L.Y.; de Jager, M.E.; Giam, Y.C.; de Jong, E.M.; van de Kerkhof, P.C.; Seyger, M.M. Juvenile psoriasis in European and Asian children: Similarities and differences. Br. J. Dermatol. 2011, 164, 1101–1103. [Google Scholar] [CrossRef]
- Griffiths, C.E.; Barker, J.N. Pathogenesis and clinical features of psoriasis. Lancet 2007, 370, 263–271. [Google Scholar] [CrossRef]
- Farber, E.M.; Nall, M.L. The natural history of psoriasis in 5600 patients. Dermatologica 1974, 148, 1–18. [Google Scholar] [CrossRef]
- Romiti, R.; Maragno, L.; Arnone, M.; Takahashi, M.D. Psoriasis in childhood and adolescence. An. Bras. Dermatol. 2009, 84, 9–20. [Google Scholar] [CrossRef] [Green Version]
- Gudjonsson, J.E.; Thorarinsson, A.M.; Sigurgeirsson, B.; Kristinsson, K.G.; Valdimarsson, H. Streptococcal throat in-fections and exacerbation of chronic plaque psoriasis: A prospective study. Br. J. Dermatol. 2003, 149, 530–534. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Lorenzo, R.; Zambrano-Zaragoza, J.F.; Saul, A.; Jiménez-Zamudio, L.; Reyes-Maldonado, E.; García-Latorre, E. Autoantibodies to autologous skin in guttate and plaque forms of psoriasis and cross-reaction of skin antigens with streptococcal antigens. Int. J. Dermatol. 1998, 37, 524–531. [Google Scholar] [CrossRef]
- Silverberg, N.B. Update on pediatric psoriasis, part 1: Clinical features and demographics. Cutis 2010, 86, 118–124. [Google Scholar]
- Silverberg, N.B. Update on pediatric psoriasis. Cutis 2015, 95, 147–152. [Google Scholar] [CrossRef] [Green Version]
- Thorleifsdottir, R.H.; Sigurdardottir, S.L.; Sigurgeirsson, B.; Olafsson, J.H.; Petersen, H.; Sigurdsson, M.I.; Gudjonsson, J.E.; Johnston, A.; Valdimarsson, H. HLA-Cw6 homozygosity in plaque psoriasis is associated with streptococcal throat infections and pronounced improvement after tonsillectomy: A prospective case series. J. Am. Acad. Dermatol. 2016, 75, 889–896. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ji, Y.Z.; Liu, S.R. Koebner phenomenon leading to the formation of new psoriatic lesions: Evidences and mechanisms. Biosci. Rep. 2019, 39, BSR20193266. [Google Scholar] [CrossRef] [Green Version]
- Chiricozzi, A.; Romanelli, P.; Volpe, E.; Borsellino, G.; Romanelli, M. Scanning the Immunopathogenesis of Psoriasis. Int. J. Mol. Sci. 2018, 19, 179. [Google Scholar] [CrossRef] [Green Version]
- Albanesi, C.; Madonna, S.; Gisondi, P.; Girolomoni, G. The Interplay Between Keratinocytes and Immune Cells in the Pathogenesis of Psoriasis. Front. Immunol. 2018, 9, 1549. [Google Scholar] [CrossRef] [Green Version]
- Ogawa, E.; Sato, Y.; Minagawa, A.; Okuyama, R. Pathogenesis of psoriasis and development of treatment. J. Dermatol. 2018, 45, 264–272. [Google Scholar] [CrossRef] [Green Version]
- Baliwag, J.; Barnes, D.H.; Johnston, A. Cytokines in psoriasis. Cytokine 2015, 73, 342–350. [Google Scholar] [CrossRef] [Green Version]
- Nussbaum, L.; Chen, Y.L.; Ogg, G.S. Role of regulatory T cells in psoriasis pathogenesis and treatment. Br. J. Dermatol. 2021, 184, 14–24. [Google Scholar] [CrossRef]
- Tsoi, L.C.; Stuart, P.E.; Tian, C.; Gudjonsson, J.E.; Das, S.; Zawistowski, M.; Ellinghaus, E.; Barker, J.N.; Chandran, V.; Dand, N.; et al. Large scale meta-analysis characterizes genetic architecture for common psoriasis associated variants. Nat. Commun. 2017, 8, 15382. [Google Scholar] [CrossRef] [Green Version]
- Liu, Y.; Helms, C.; Liao, W.; Zaba, L.C.; Duan, S.; Gardner, J.; Wise, C.; Miner, A.; Malloy, M.J.; Pullinger, C.R.; et al. A genome-wide association study of psoriasis and psoriatic arthritis identifies new disease loci. PLoS Genet. 2008, 4, e1000041. [Google Scholar] [CrossRef] [PubMed]
- Andressen, C.; Henseler, T. Erblichkeit der Psoriasis. Eine Analyse von 2035 Familienanamnesen [Inheritance of pso-riasis. Analysis of 2035 family histories]. Hautarzt 1982, 33, 214–217. [Google Scholar]
- Kim, J.C.; Kim, S.M.; Soh, B.W.; Lee, E.S. Comparison of Cytokine Expression in Paediatric and Adult Psoriatic Skin. Acta Derm. Venereol. 2020, 100, adv00058. [Google Scholar] [CrossRef] [PubMed]
- Cordoro, K.M.; Hitraya-Low, M.; Taravati, K.; Sandoval, P.M.; Kim, E.; Sugarman, J.; Pauli, M.L.; Liao, W.; Rosenblum, M.D. Skin-infiltrating, interleukin-22-producing T cells differentiate pediatric psoriasis from adult psoriasis. J. Am. Acad. Dermatol. 2017, 77, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Li, Y.; Yang, X.; Wei, J.; Zhou, S.; Zhao, Z.; Cheng, J.; Duan, H.; Jia, T.; Lei, Q.; et al. Characterization of Th17 and FoxP3(+) Treg Cells in Paediatric Psoriasis Patients. Scand. J. Immunol. 2016, 83, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Cline, A.; Berg, A.; Bartos, G.J.; Strowd, L.C.; Feldman, S.R. Biologic Treatment Options for Pediatric Psoriasis and Atopic Dermatitis-A Review. J. Clin. Aesthet. Dermatol. 2020, 13, 33–38. [Google Scholar]
- Haulrig, M.B.; Zachariae, C.; Skov, L. Off-Label Treatments for Pediatric Psoriasis: Lessons for the Clinic. Psoriasis 2021, 11, 1–20. [Google Scholar] [CrossRef]
- Maul, J.T.; Anzengruber, F.; Conrad, C.; Cozzio, A.; Häusermann, P.; Jalili, A.; Kolios, A.G.A.; Laffitte, E.; Lapointe, A.-K.; Mainetti, C.; et al. Topical Treatment of Psoriasis Vulgaris: The Swiss Treatment Pathway. Dermatology 2021, 237, 166–178. [Google Scholar]
- Lamba, S.; Lebwohl, M. Combination therapy with vitamin D analogues. Br. J. Dermatol. 2001, 144 (Suppl. S58), 27–32. [Google Scholar] [CrossRef]
- Jacobi, A.; Mayer, A.; Augustin, M. Keratolytics and emollients and their role in the therapy of psoriasis: A systematic review. Dermatol. Ther. 2015, 5, 1–18. [Google Scholar] [CrossRef]
- Thomas, J.; Parimalam, K. Treating pediatric plaque psoriasis: Challenges and solutions. Pediatric Health Med. Ther. 2016, 7, 25–38. [Google Scholar] [CrossRef] [Green Version]
- Silverberg, N.B. Update on pediatric psoriasis, Part 2: Therapeutic management. Cutis 2010, 86, 172–176. [Google Scholar] [PubMed]
- Fluhr, J.W.; Cavallotti, C.; Berardesca, E. Emollients, moisturizers, and keratolytic agents in psoriasis. Clin. Dermatol. 2008, 26, 380–386. [Google Scholar] [CrossRef]
- Shah, K.N. Diagnosis and treatment of pediatric psoriasis: Current and future. Am. J. Clin. Dermatol. 2013, 14, 195–213. [Google Scholar] [CrossRef]
- Kimball, A.B.; Gold, M.H.; Zib, B.; Davis, M.W.; Clobetasol Propionate Emulsion Formulation Foam Phase III Clinical Study Group. Clobetasol propionate emulsion formulation foam 0.05%: Review of phase II open-label and phase III randomized controlled trials in steroid-responsive dermatoses in adults and adolescents. J. Am. Acad. Dermatol. 2008, 59, 448–454.e1. [Google Scholar] [CrossRef]
- Bhutani, T.; Kamangar, F.; Cordoro, K.M. Management of pediatric psoriasis. Pediatr. Ann. 2012, 41, e1–e7. [Google Scholar] [CrossRef] [Green Version]
- de Jager, M.E.; de Jong, E.M.; van de Kerkhof, P.C.; Seyger, M.M. Efficacy and safety of treatments for childhood psoriasis: A systematic literature review. J. Am. Acad. Dermatol. 2010, 62, 1013–1030. [Google Scholar] [CrossRef]
- Herz, G.; Blum, G.; Yawalkar, S. Halobetasol propionate cream by day and halobetasol propionate ointment at night for the treatment of pediatric patients with chronic, localized plaque psoriasis and atopic dermatitis. J. Am. Acad. Dermatol. 1991, 25, 1166–1169. [Google Scholar] [CrossRef]
- Wang, C.; Lin, A. Efficacy of topical calcineurin inhibitors in psoriasis. J. Cutan Med. Surg. 2014, 18, 8–14. [Google Scholar] [CrossRef]
- Steele, J.A.; Choi, C.; Kwong, P.C. Topical tacrolimus in the treatment of inverse psoriasis in children. J. Am. Acad. Dermatol. 2005, 53, 713–716. [Google Scholar] [CrossRef] [PubMed]
- Brune, A.; Miller, D.W.; Lin, P.; Cotrim-Russi, D.; Paller, A.S. Tacrolimus ointment is effective for psoriasis on the face and intertriginous areas in pediatric patients. Pediatr. Dermatol. 2007, 24, 76–80. [Google Scholar] [CrossRef] [PubMed]
- Carr, W.W. Topical calcineurin inhibitors for atopic dermatitis: Review and treatment recommendations. Paediatr. Drugs 2013, 15, 303–310. [Google Scholar] [CrossRef] [Green Version]
- Malecic, N.; Young, H. Tacrolimus for the management of psoriasis: Clinical utility and place in therapy. Psoriasis 2016, 6, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Mansouri, P.; Farshi, S. Pimecrolimus 1 percent cream in the treatment of psoriasis in a child. Dermatol. Online J. 2006, 12, 7. [Google Scholar] [CrossRef] [PubMed]
- Oranje, A.P.; Marcoux, D.; Svensson, A.; Prendiville, J.; Krafchik, B.; Toole, J.; Rosenthal, D.; de Waard-van der Spek, F.B.; Molin, L.; Axelsen, M. Topical calcipotriol in childhood psoriasis. J. Am. Acad. Dermatol. 1997, 36, 203–208. [Google Scholar] [CrossRef]
- van Geel, M.J.; Mul, K.; Oostveen, A.M.; van de Kerkhof, P.C.; de Jong, E.M.; Seyger, M.M. Calcipotri-ol/betamethasone dipropionate ointment in mild-to-moderate paediatric psoriasis: Long-term daily clinical practice data in a prospective cohort. Br. J. Dermatol. 2014, 171, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Gooderham, M.; Debarre, J.M.; Keddy-Grant, J.; Xu, Z.; Kurvits, M.; Goodfield, M. Safety and efficacy of calcipotriol plus betamethasone dipropionate gel in the treatment of scalp psoriasis in adolescents 12–17 years of age. Br. J. Dermatol. 2014, 171, 1470–1477. [Google Scholar] [CrossRef]
- Menter, A.; Cordoro, K.M.; Davis, D.; Kroshinsky, D.; Paller, A.S.; Armstrong, A.W.; Connor, C.; Elewski, B.E.; Gelfand, J.M.; Gordon, K.B.; et al. Joint American Academy of Dermatology-National Psoriasis Foundation guidelines of care for the management and treatment of psoriasis in pediatric patients. J. Am. Acad. Dermatol. 2020, 82, 161–201. [Google Scholar] [CrossRef] [Green Version]
- Seyger, M.; Abramovits, W.; Liljedahl, M.; Hoejen, M.N.; Teng, J. Safety and efficacy of fixed-dose combination cal-cipotriol (50 μg/g) and betamethasone dipropionate (0.5 mg/g) cutaneous foam in adolescent patients (aged 12 to <17 years) with plaque psoriasis: Results of a phase II, open-label trial. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 2026–2034. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Diluvio, L.; Campione, E.; Paternò, E.J.; Mordenti, C.; El Hachem, M.; Chimenti, S. Childhood nail psoriasis: A useful treatment with tazarotene 0.05%. Pediatr. Dermatol. 2007, 24, 332–333. [Google Scholar] [CrossRef] [PubMed]
- de Jager, M.E.; van de Kerkhof, P.C.; de Jong, E.M.; Seyger, M.M. Dithranol therapy in childhood psoriasis: Unjustifiably on the verge of falling into oblivion. Dermatology 2010, 220, 329–332. [Google Scholar] [CrossRef]
- Zvulunov, A.; Anisfeld, A.; Metzker, A. Efficacy of short-contact therapy with dithranol in childhood psoriasis. Int. J. Dermatol. 1994, 33, 808–810. [Google Scholar] [CrossRef]
- Oostveen, A.M.; Beulens, C.A.; van de Kerkhof, P.C.; de Jong, E.M.; Seyger, M.M. The effectiveness and safety of short-contact dithranol therapy in paediatric psoriasis: A prospective comparison of regular day care and day care with telemedicine. Br. J. Dermatol. 2014, 170, 454–457. [Google Scholar] [CrossRef] [PubMed]
- Menter, M.A.; Whiting, D.A.; McWilliams, J. Resistant childhood psoriasis: An analysis of patients seen in a day-care center. Pediatr. Dermatol. 1984, 2, 8–12. [Google Scholar] [CrossRef]
- Kortuem, K.R.; Davis, M.D.; Witman, P.M.; McEvoy, M.T.; Farmer, S.A. Results of Goeckerman treatment for psoriasis in children: A 21-year retrospective review. Pediatr. Dermatol. 2010, 27, 518–524. [Google Scholar] [CrossRef]
- Borska, L.; Andrys, C.; Krejsek, J.; Palicka, V.; Chmelarova, M.; Hamakova, K.; Kremlacek, J.; Fiala, Z. Oxidative damage to nucleic acids and benzo(a)pyrene-7,8-diol-9,10-epoxide-DNA adducts and chromosomal aberration in children with psoriasis repeatedly exposed to crude coal tar ointment and UV radiation. Longev. OMAC 2014, 2014, 302528. [Google Scholar] [CrossRef] [Green Version]
- Smith, S.H.; Jayawickreme, C.; Rickard, D.J.; Nicodeme, E.; Bui, T.; Simmons, C.; Coquery, C.M.; Neil, J.; Pryor, W.M.; Mayhew, D.; et al. Tapinarof Is a Natural AhR Agonist that Resolves Skin Inflammation in Mice and Humans. J. Investig. Dermatol. Symp. Proc. 2017, 137, 2110–2119. [Google Scholar] [CrossRef] [Green Version]
- Smith, S.H.; McHale, K.; Creech, K.; Rickard, D.; Jayawickreme, C.; Wu, D.; Rastinejad, F.; Rubenstein, D. Differential ligand binding distinguishes therapeutic from pathologic aryl hydrocarbon receptor (AhR) modulating agents: Implications for inflammatory skin disease. J. Investig. Dermatol. 2020, 140, S81. [Google Scholar] [CrossRef]
- Bissonnette, R.; Bolduc, C.; Maari, C.; Nigen, S.; Webster, J.M.; Tang, L. Efficacy and safety of topical WBI-1001 in patients with mild to moderate psoriasis: Results from a randomized double-blind placebo-controlled, phase II trial. J. Eur. Acad. Dermatol. Venereol. 2012, 26, 1516–1521. [Google Scholar] [CrossRef]
- Paller, A.S.; Stein Gold, L.; Soung, J.; Tallman, A.M.; Rubenstein, D.S.; Gooderham, M. Efficacy and patient-reported outcomes from a phase 2b, randomized clinical trial of tapinarof cream for the treatment of adolescents and adults with atopic dermatitis. J. Am. Acad. Dermatol. 2021, 84, 632–638. [Google Scholar] [CrossRef]
- Walters, I.B.; Burack, L.H.; Coven, T.R.; Gilleaudeau, P.; Krueger, J.G. Suberythemogenic narrow-band UVB is markedly more effective than conventional UVB in treatment of psoriasis vulgaris. J. Am. Acad. Dermatol. 1999, 40, 893–900. [Google Scholar] [CrossRef]
- Ersoy-Evans, S.; Altaykan, A.; Sahin, S.; Kölemen, F. Phototherapy in childhood. Pediatr. Dermatol. 2008, 25, 599–605. [Google Scholar] [CrossRef]
- Jain, V.K.; Aggarwal, K.; Jain, K.; Bansal, A. Narrow-band UV-B phototherapy in childhood psoriasis. Int. J. Dermatol. 2007, 46, 320–322. [Google Scholar] [CrossRef]
- Bronckers, I.; Seyger, M.; West, D.P.; Lara-Corrales, I.; Tollefson, M.; Tom, W.L.; Hogeling, M.; Belazarian, L.; Zachariae, C.; Mahe, E.; et al. Safety of Systemic Agents for the Treatment of Pediatric Psoriasis. JAMA Dermatol. 2017, 153, 1147–1157. [Google Scholar] [CrossRef] [PubMed]
- Lara-Corrales, I.; Ramnarine, S.; Lansang, P. Treatment of childhood psoriasis with phototherapy and photochemo-therapy. Clin. Med. Insights Pediatr. 2013, 7, 25–33. [Google Scholar]
- Kaur, I.; Dogra, S.; De, D.; Kanwar, A.J. Systemic methotrexate treatment in childhood psoriasis: Further experience in 24 children from India. Pediatr. Dermatol. 2008, 25, 184–188. [Google Scholar] [CrossRef]
- Warren, R.B.; Chalmers, R.J.; Griffiths, C.E.; Menter, A. Methotrexate for psoriasis in the era of biological therapy. Clin. Exp. Dermatol. 2008, 33, 551–554. [Google Scholar] [CrossRef]
- Herfarth, H.H.; Kappelman, M.D.; Long, M.D.; Isaacs, K.L. Use of Methotrexate in the Treatment of Inflammatory Bowel Diseases. Inflamm. Bowel. Dis. 2016, 22, 224–233. [Google Scholar] [CrossRef] [Green Version]
- Ergun, T.; Seckin Gencosmanoglu, D.; Alpsoy, E.; Bulbul-Baskan, E.; Saricam, M.H.; Salman, A.; Onsun, N.; Sarioz, A. Efficacy, safety and drug survival of conventional agents in pediatric psoriasis: A multicenter, cohort study. J. Dermatol. 2017, 44, 630–634. [Google Scholar] [CrossRef]
- van Geel, M.J.; Mul, K.; de Jager, M.E.; van de Kerkhof, P.C.; de Jong, E.M.; Seyger, M.M. Systemic treatments in paediatric psoriasis: A systematic evidence-based update. J. Eur. Acad. Dermatol. Venereol. 2015, 29, 425–437. [Google Scholar] [CrossRef] [PubMed]
- Rendon, A.; Schäkel, K. Psoriasis Pathogenesis and Treatment. Int. J. Mol. Sci. 2019, 20, 1475. [Google Scholar] [CrossRef] [Green Version]
- Kiliç, S.S.; Hacimustafaoğlu, M.; Celebi, S.; Karadeniz, A.; Ildirim, I. Low dose cyclosporin A treatment in generalized pustular psoriasis. Pediatr. Dermatol. 2001, 18, 246–248. [Google Scholar] [CrossRef]
- Cyclosporine [Package Insert]; Novartis Pharmaceutical Corporation: East Hanover, NJ, USA, 2015.
- Bulbul Baskan, E.; Yazici, S.; Tunali, S.; Saricaoglu, H. Clinical experience with systemic cyclosporine A treatment in severe childhood psoriasis. J. Dermatolog. Treat. 2016, 27, 328–331. [Google Scholar] [CrossRef]
- Dogra, S.; Mahajan, R.; Narang, T.; Handa, S. Systemic cyclosporine treatment in severe childhood psoriasis: A retro-spective chart review. J. Dermatol. Treat. 2017, 28, 18–20. [Google Scholar] [CrossRef] [PubMed]
- Lebwohl, M. Psoriasis. Ann. Intern. Med. 2018, 168, ITC49–ITC64. [Google Scholar] [CrossRef] [PubMed]
- Rosińska, D.; Wolska, H.; Jablonska, S.; Konca, I. Etretinate in severe psoriasis of children. Pediatr. Dermatol. 1988, 5, 266–272. [Google Scholar] [CrossRef]
- Napolitano, M.; Megna, M.; Balato, A.; Ayala, F.; Lembo, S.; Villani, A.; Balato, N. Systemic Treatment of Pediatric Psoriasis: A Review. J. Drugs Dermatol. 2016, 6, 125–142. [Google Scholar] [CrossRef] [Green Version]
- Popadic, S.; Nikolic, M. Pustular psoriasis in childhood and adolescence: A 20-year single-center experience. Pediatr. Dermatol. 2014, 31, 575–579. [Google Scholar] [CrossRef]
- Absorica (Isotretinoin) [Package Insert]; Galephar Pharmaceuticals Research, Inc.: Humaco, PR, USA, 2018.
- Halverstam, C.P.; Zeichner, J.; Lebwohl, M. Lack of significant skeletal changes after long-term, low-dose retinoid therapy: Case report and review of the literature. J. Cutan Med. Surg. 2006, 10, 291–299. [Google Scholar] [CrossRef]
- Marqueling, A.L.; Cordoro, K.M. Systemic treatments for severe pediatric psoriasis: A practical approach. Dermatol. Clin. 2013, 31, 267–288. [Google Scholar] [CrossRef]
- Mrowietz, U.; Barker, J.; Boehncke, W.H.; Iversen, L.; Kirby, B.; Naldi, L.; Reich, K.; Tanew, A.; van de Kerhok, P.C.M.; Warren, R.M. Clinical use of dimethyl fumarate in moderate-to-severe plaque-type psoriasis: A European expert consensus. J. Eur. Acad. Dermatol. Venereol. 2018, 32 (Suppl. S3), 3–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steinz, K.; Gerdes, S.; Domm, S.; Mrowietz, U. Systemic treatment with fumaric acid esters in six paediatric patients with psoriasis in a psoriasis centre. Dermatology 2014, 229, 199–204. [Google Scholar] [CrossRef]
- Paller, A.S.; Siegfried, E.C.; Langley, R.G.; Gottlieb, A.B.; Pariser, D.; Landells, I.; Herbert, A.A.; Eichenfield, L.F.; Patel, V.; Creamer, K.; et al. Etanercept treatment for children and adolescents with plaque psoriasis. N. Engl. J. Med. 2008, 358, 241–251. [Google Scholar] [CrossRef] [Green Version]
- Aslam, N.; Saleem, H.; Murtazaliev, S.; Quazi, S.J.; Khan, S. FDA Approved Biologics: Can Etanercept and Ustekinumab be Considered a First-Line Systemic Therapy for Pediatric/Adolescents in Moderate to Severe Psoriasis? A Systematic Review. Cureus 2020, 12, e9812. [Google Scholar]
- Langley, R.G.; Paller, A.S.; Hebert, A.A.; Creamer, K.; Weng, H.H.; Jahreis, A.; Globe, D.; Patel, V.; Orlow, S.J. Patient-reported outcomes in pediatric patients with psoriasis undergoing etanercept treatment: 12-week results from a phase III randomized controlled trial. J. Am. Acad. Dermatol. 2011, 64, 64–70. [Google Scholar] [CrossRef]
- Fabrizi, G.; Guerriero, C.; Pagliarello, C. Etanercept in infants: Suberythrodermic, recalcitrant psoriasis in a 22 month-old child successfully treated with etanercept. Eur. J. Dermatol. 2007, 17, 245. [Google Scholar] [PubMed]
- Paller, A.S.; Siegfried, E.C.; Eichenfield, L.F.; Pariser, D.; Langley, R.G.; Creamer, K.; Kricorian, G. Long-term etanercept in pediatric patients with plaque psoriasis. J. Am. Acad. Dermatol. 2010, 63, 762–768. [Google Scholar] [CrossRef]
- Paller, A.S.; Siegfried, E.C.; Pariser, D.M.; Rice, K.C.; Trivedi, M.; Iles, J.; Collier, D.H.; Kricorian, G.; Langley, R.G. Long-term safety and efficacy of etanercept in children and adolescents with plaque psoriasis. J. Am. Acad. Dermatol. 2016, 74, 277–280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Papp, K.; Thaçi, D.; Marcoux, D.; Weibel, L.; Philipp, S.; Ghislain, P.D.; Landells, I.; Hoeger, P.; Kotkin, C.; Unnebrink, K.; et al. Efficacy and safety of adalimumab every other week versus methotrexate once weekly in children and adolescents with severe chronic plaque psoriasis: A randomised, double-blind, phase 3 trial. Lancet 2017, 390, 40–49. [Google Scholar] [CrossRef]
- Xie, X.; Wang, Y.; Yao, S.; Xia, Y.; Luo, H.; Li, L.; Lu, C. Biologics recommendations for patients with psoriasis: A critical appraisal of clinical practice guidelines for psoriasis. J. Dermatolog Treat. 2021, 1–36. [Google Scholar] [CrossRef]
- Saeki, H.; Terui, T.; Morita, A.; Sano, S.; Imafuku, S.; Asahina, A.; Komine, M.; Etoh, T.; Igarashi, A.; Torii, H.; et al. Japanese guidance for use of biologics for pso-riasis (the 2019 version). J. Dermatol. 2020, 47, 201–222. [Google Scholar] [CrossRef] [PubMed]
- Landells, I.; Marano, C.; Hsu, M.C.; Li, S.; Zhu, Y.; Eichenfield, L.F.; Hoeger, P.H.; Menter, A.; Paller, A.S.; Taieb, A.; et al. Ustekinumab in adolescent patients age 12 to 17 years with moderate-to-severe plaque psoriasis: Results of the randomized phase 3 CADMUS study. J. Am. Acad. Dermatol. 2015, 73, 594–603. [Google Scholar] [CrossRef] [Green Version]
- Klufas, D.M.; Wald, J.M.; Strober, B.E. Treatment of Moderate to Severe Pediatric Psoriasis: A Retrospective Case Series. Pediatr. Dermatol. 2016, 33, 142–149. [Google Scholar] [CrossRef]
- Lim, H.; Lee, S.H.; Lee, H.T.; Lee, J.U.; Son, J.Y.; Shin, W.; Heo, Y.-S. Structural Biology of the TNFα Antagonists Used in the Treatment of Rheumatoid Arthritis. Int. J. Mol. Sci. 2018, 19, 768. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pinson, R.; Sotoodian, B.; Fiorillo, L. Psoriasis in children. Psoriasis 2016, 6, 121–129. [Google Scholar] [CrossRef] [Green Version]
- Bodemer, C.; Kaszuba, A.; Kingo, K.; Tsianakas, A.; Morita, A.; Rivas, E.; Papanastasiou, P.; Keefe, D.; Patekar, M.; Charef, P.; et al. Secukinumab demonstrates high effi-cacy and a favourable safety profile in paediatric patients with severe chronic plaque psoriasis: 52-week results from a Phase 3 double-blind randomized, controlled trial. J. Eur. Acad. Dermatol. Venereol. 2021, 35, 938–947. [Google Scholar] [CrossRef] [PubMed]
- Paller, A.S.; Seyger, M.; Alejandro Magariños, G.; Bagel, J.; Pinter, A.; Cather, J.; Keller, S.; Capriles, C.R.; Lima, R.G.; Gallo, G.; et al. Efficacy and safety of ixeki-zumab in a phase III, randomized, double-blind, placebo-controlled study in paediatric patients with moderate-to-severe plaque psoriasis (IXORA-PEDS). Br. J. Dermatol. 2020, 183, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Blauvelt, A.; Papp, K.A.; Griffiths, C.E.; Randazzo, B.; Wasfi, Y.; Shen, Y.K.; Li, S.; Kimball, A.B. Efficacy and safety of guselkumab, an anti-interleukin-23 monoclonal antibody, compared with adalimumab for the continuous treatment of patients with moderate to severe psoriasis: Results from the phase III, double-blinded, placebo- and active comparator-controlled VOYAGE 1 trial. J. Am. Acad. Dermatol. 2017, 76, 405–417. [Google Scholar]
- Papp, K.A.; Blauvelt, A.; Bukhalo, M.; Gooderham, M.; Krueger, J.G.; Lacour, J.P.; Menter, A.; Philipp, S.; Sofen, H.; Tyring, S.; et al. Risankizumab versus Ustekinumab for Moderate-to-Severe Plaque Psoriasis. N. Engl. J. Med. 2017, 376, 1551–1560. [Google Scholar] [CrossRef]
- Papp, K.A.; Menter, M.A.; Abe, M.; Elewski, B.; Feldman, S.R.; Gottlieb, A.B.; Langley, R.; Luger, T.; Thaci, D.; Buonanno, M.; et al. Tofacitinib, an oral Janus kinase inhibitor, for the treatment of chronic plaque psoriasis: Results from two randomized, placebo-controlled, phase III trials. Br. J. Dermatol. 2015, 173, 949–961. [Google Scholar] [CrossRef]
- Bachelez, H.; van de Kerkhof, P.C.; Strohal, R.; Kubanov, A.; Valenzuela, F.; Lee, J.H.; Yakusevich, V.; Chimenti, S.; Papacharalambous, J.; Proulx, J.; et al. Tofacitinib versus etanercept or placebo in moderate-to-severe chronic plaque psoriasis: A phase 3 randomised non-inferiority trial. Lancet 2015, 386, 552–561. [Google Scholar] [CrossRef]
- AlMutairi, N.; Nour, T. Tofacitinib in Pediatric Psoriasis: An Open-Label Trial to Study Its Safety and Efficacy in Children. Dermatology 2020, 236, 191–198. [Google Scholar] [CrossRef] [PubMed]
| Systemic Treatments | Mechanism | Dosage | Side Effects |
|---|---|---|---|
| Methotrexate | Inhibition of RNA and DNA synthesis Cell cycle arrest Inhibition of inflammatory cytokines such as tumor necrosis factor (TNF) and interleukin (IL-6, and 8) | 0.2 to 0.7 mg/kg/week | Elevated liver enzymes Bone marrow suppression |
| Cyclosporine | Inhibition of T lymphocytes Prevention of the development of IL-2 and IFN-gamma | 1 to 5 mg/kg/d | Possible nephrotoxicity in prolonged usage High blood pressure |
| Retinoids | Modification of cellular metabolic pathways, cellular differentiation, and apoptosis | 0.1 to 1 mg/kg/d | Pruritus, cheilitis, hair loss, partial osteoporosis, elevated liver enzymes, hyperlipidemia, and paronychia |
| Fumaric acid esters | Small molecules with immunomodulatory effects | ≤720 mg/day | Gastrointestinal complains, lymphocytopenia, eosinophilia, and flush |
| Biologics | Mechanism | FDA/EMA Approval | Dosing | Safety |
|---|---|---|---|---|
| Etanercept | A fusion protein blocking TNF- from binding to its receptor | Approved in FDA for treatment of psoriasis in patients ≥4 years of age Approved in EMA for treatment of psoriasis in patients ≥6 years of age | SC injection of 0.8 mg/kg per week with a maximum of 50 mg per week | Upper respiratory tract infections, nasopharyngitis, streptococcal pharyngitis, sinusitis, headache, injection site reactions |
| Adalimumab | A fully human TNF- monoclonal antibody | Approved in EMA for treatment of psoriasis in patients ≥4 years of age | For patients 15 to 30 kg: SC injection of 20 mg at week 0 and then 20 mg every other week For patients >30 kg: SC injection of 40 mg at week 0 and then 40 mg every other week | Upper respiratory infections, uncomplicated infections, injection site reactions |
| Ustekinumab | A monoclonal antibody that targets the p40 subunit of IL-12 and IL-23 | Approved in FDA/EMA for treatment of psoriasis in patients ≥12 years of age | For patients < 60 kg: SC injection of 0.75 mg/kg at week 0, week 4, and then every 12 weeks For patients 60 kg to 100 kg: SC injection of 45 mg at week 0, week 4, and then every 12 weeks For >100 kg: SC injection of 90 mg at week 0, week 4, and then every 12 weeks | Upper respiratory tract infection, headache, injection site reaction |
| Infliximab | Chimeric monoclonal antibody that binds to human TNF-α | Not approved for pediatric psoriasis in FDA/EMA | IV infusion of 3.3–5 mg/ kg at weeks 0, 2, and 6, then once every 7-8 weeks | Infusion reactions, upper respiratory tract infection, headache, rash, and cough |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.O.; Kang, S.Y.; Kim, J.C.; Park, C.W.; Chung, B.Y. Pediatric Psoriasis: From New Insights into Pathogenesis to Updates on Treatment. Biomedicines 2021, 9, 940. https://doi.org/10.3390/biomedicines9080940
Kim HO, Kang SY, Kim JC, Park CW, Chung BY. Pediatric Psoriasis: From New Insights into Pathogenesis to Updates on Treatment. Biomedicines. 2021; 9(8):940. https://doi.org/10.3390/biomedicines9080940
Chicago/Turabian StyleKim, Hye One, Seok Young Kang, Jin Cheol Kim, Chun Wook Park, and Bo Young Chung. 2021. "Pediatric Psoriasis: From New Insights into Pathogenesis to Updates on Treatment" Biomedicines 9, no. 8: 940. https://doi.org/10.3390/biomedicines9080940
APA StyleKim, H. O., Kang, S. Y., Kim, J. C., Park, C. W., & Chung, B. Y. (2021). Pediatric Psoriasis: From New Insights into Pathogenesis to Updates on Treatment. Biomedicines, 9(8), 940. https://doi.org/10.3390/biomedicines9080940






