Potential Therapeutic Applications of Synthetic Conotoxin s-cal14.2b, Derived from Californiconus californicus, for Treating Type 2 Diabetes
Abstract
:1. Introduction
2. Materials and Methods
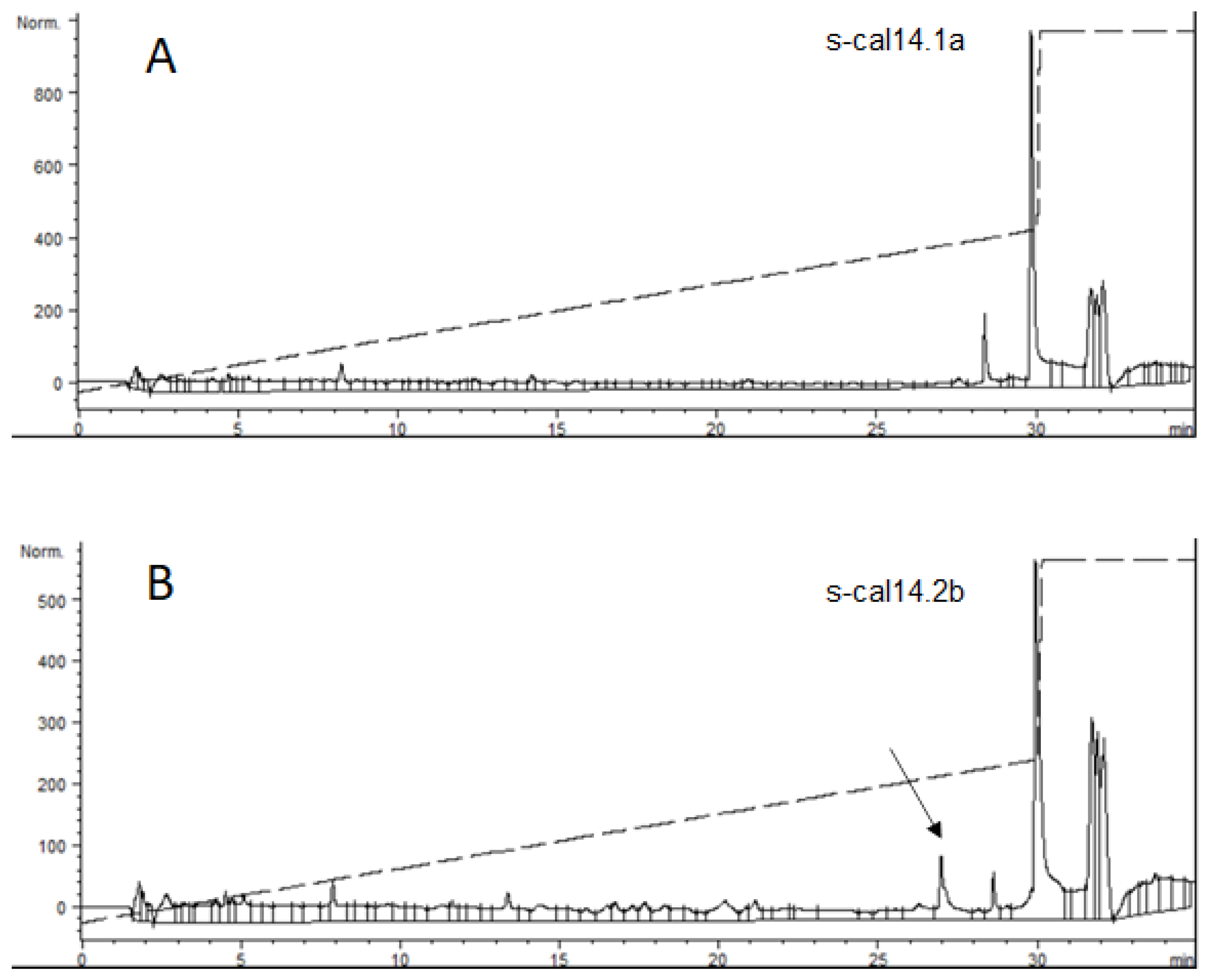
2.1. Conotoxin cal14.2b
2.2. Isolation and Primary Culture of Metabolic Cells and NIT-1 Cell Culture
2.3. Evaluation of s-cal14.2b Cytotoxicity in NIT-1 and Primary Cell Cultures
2.4. NIT-1 Insulin Secretion Assay
2.5. Isolation and Culture of Rat Pancreatic β-Cells
2.6. Electrophysiological Analysis
2.7. Insulinotropic Potential of s-cal14.2b In Vivo
2.7.1. In Vivo Glucose Modulation by s-cal14.2b
2.7.2. Radiolabeling of s-cal14.2b with Technetium-99m
2.7.3. In Vivo 99mTc-s-cal14.2b Biodistribution in Normal Rats
2.8. Statistical Analysis
3. Results
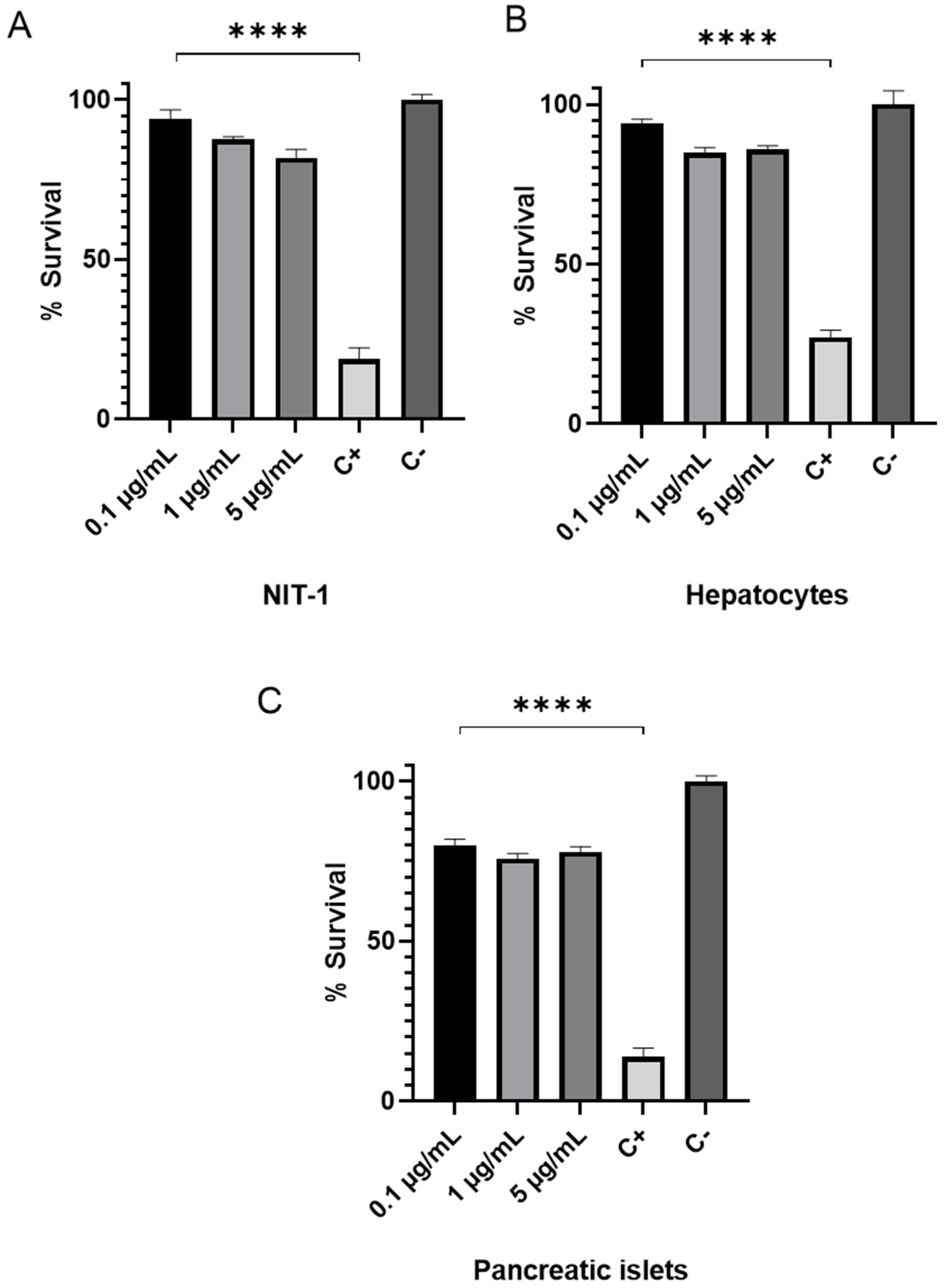
3.1. Cytotoxic Assesment of s-cal14.2b in NIT 1 Insulinoma and Primary Hepatic and Pancreatic Cells
3.2. Impact of s-cal14.2b on Insulin Secretion In Vitro
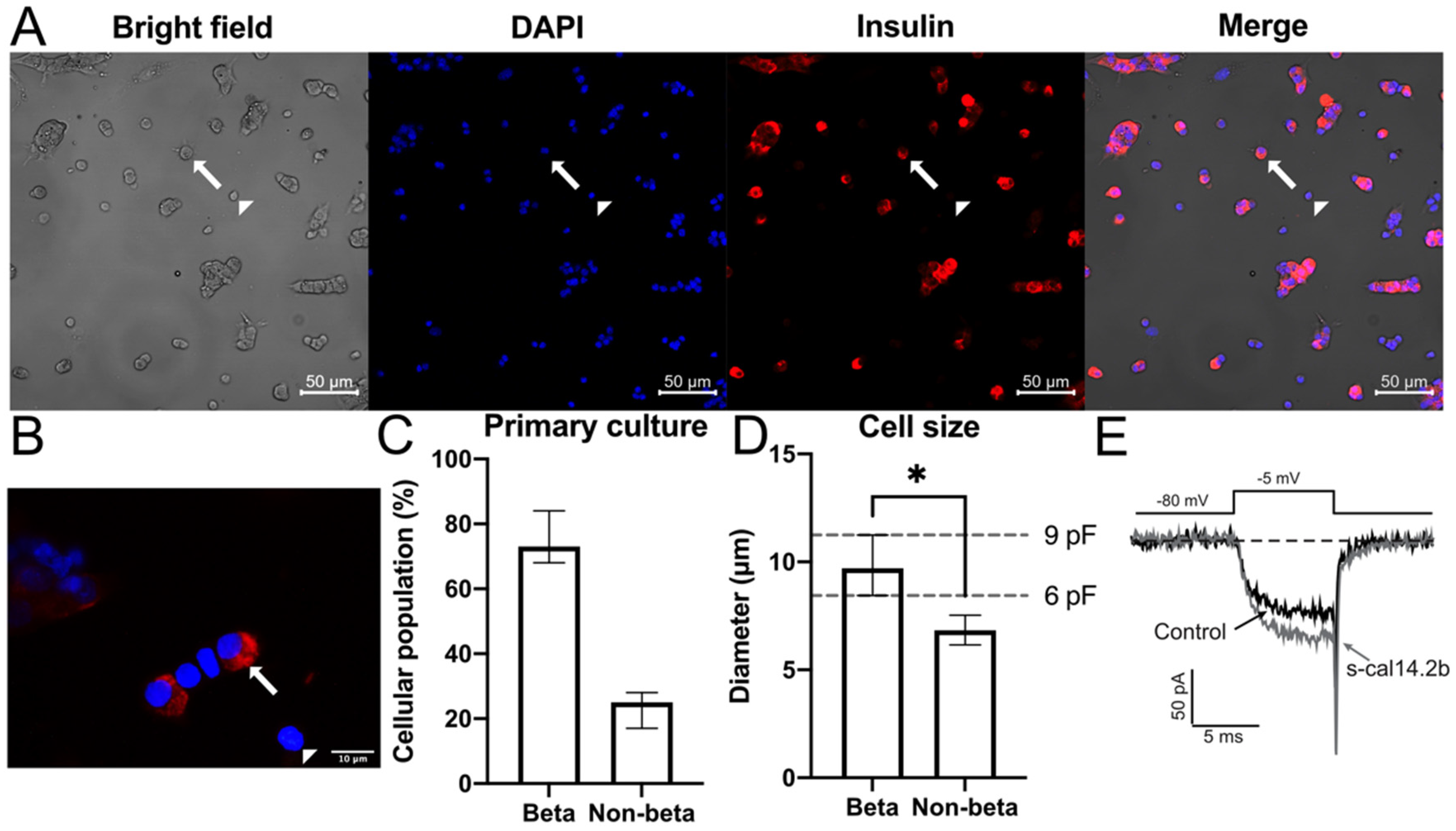
3.3. In Vitro Immunocytochemistry Identification of Insulin in Native Rat Pancreatic β-Cells
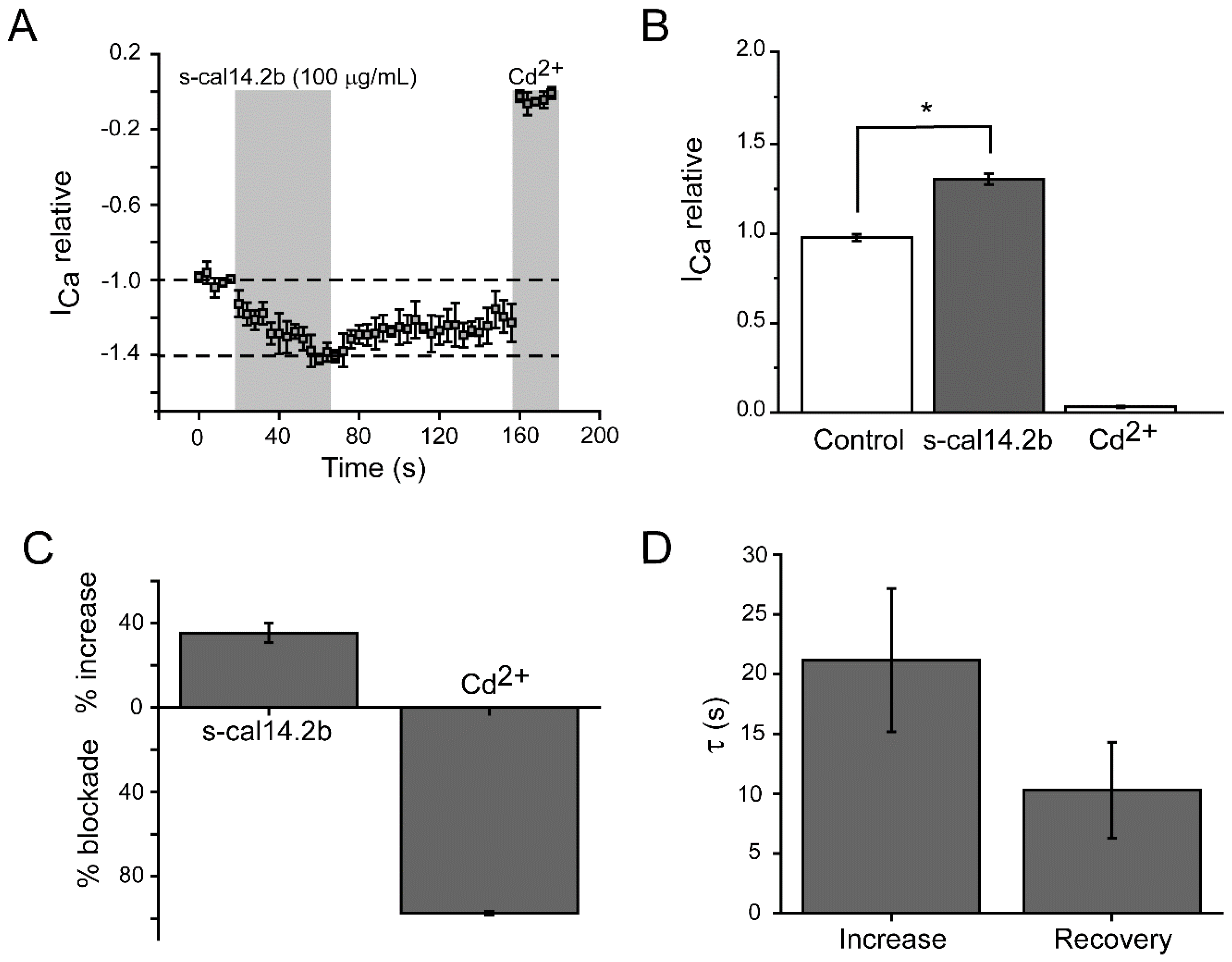
3.4. Electrophysiological Assessment of Pancreatic β-Cell Ca2+ Currents in Response to s-cal14.2b
3.5. Glucose Tolerance Curve in Mice Model after s-cal14.2b Administration
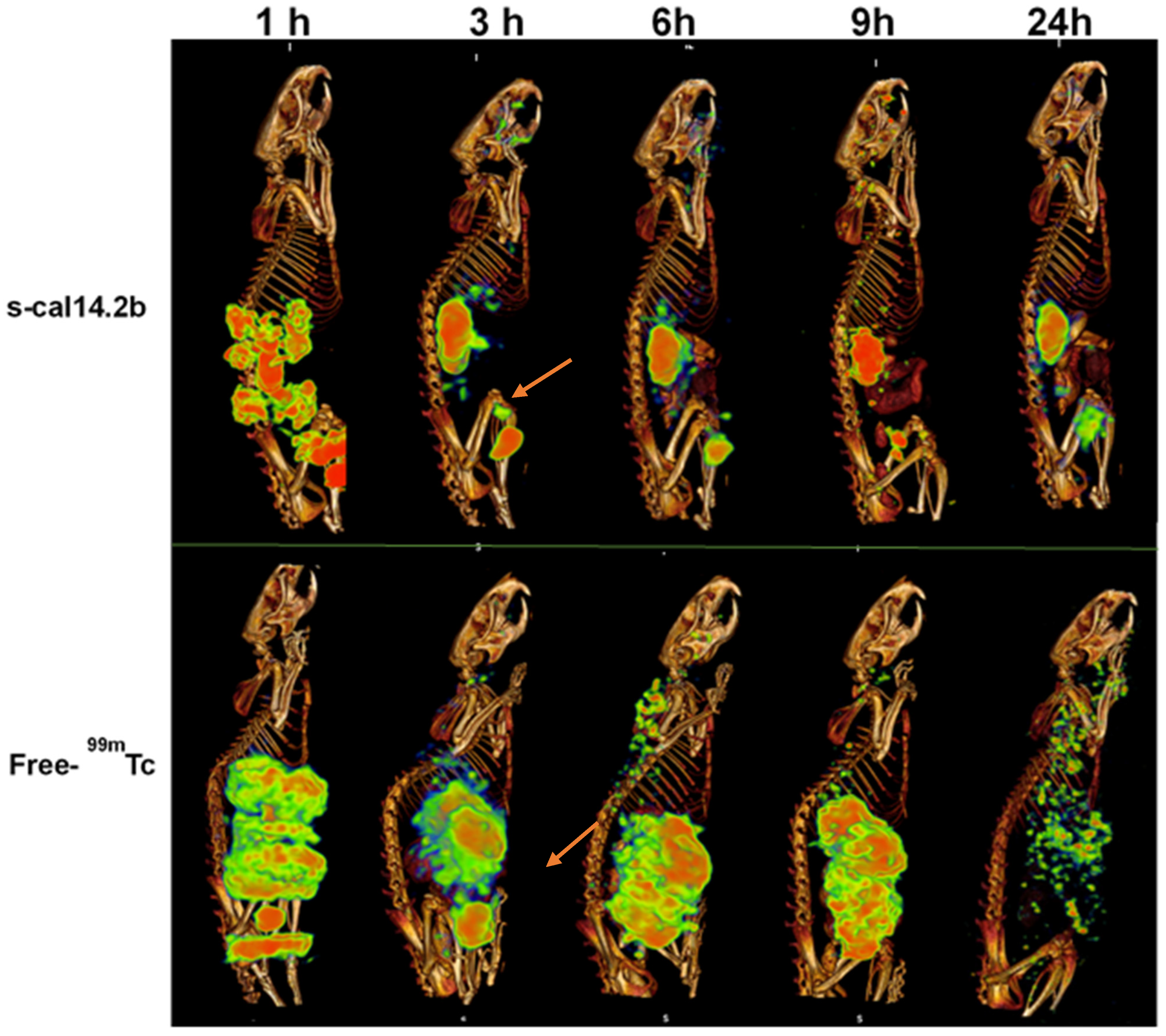
3.6. Biodistribution of Radiolabeled s-cal14.2b in Wistar Rats
4. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Danaei, G.; Finucane, M.M.; Lu, Y.; Singh, G.M.; Cowan, M.J.; Paciorek, C.J.; Lin, J.K.; Farzadfar, F.; Khang, Y.H.; Stevens, G.A.; et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: Systematic analysis of health examination surveys and epide-miological studies with 370 country-years and 2.7million participants. Lancet 2011, 378, 31–40. [Google Scholar] [CrossRef]
- International Diabetes Federation. Diabetes Atlas, 6th ed.; International Diabetes Federation: Brussels, Belgium, 2013; ISBN 2-930229-85-3. [Google Scholar]
- WHO. 10 Facts about Diabetes. Available online: http://www.whoint/features/factfiles/diabetes/facts/en/index.html (accessed on 15 April 2021).
- American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care 2013, 36, 1033–1046. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Breton, M.C.; Guenette, L.; Amiche, M.A.; Kayibanda, J.F.; Gregoire, J.P.; Moisan, J. Burden of diabetes on the ability to work: A systematic review. Diabetes Care 2013, 36, 740–749. [Google Scholar] [CrossRef] [Green Version]
- McEwen, L.N.; Casagrande, S.S.; Kuo, S.; Herman, W.H. Why Are Diabetes Medications So Expensive and What Can Be Done to Control Their Cost? Curr. Diabetes Rep. 2017, 17, 71. [Google Scholar] [CrossRef]
- Bhutani, J.; Bhutani, S. Worldwide burden of diabetes. Indian J. Endocrinol. Metab. 2014, 18, 868–870. [Google Scholar] [CrossRef]
- Sarwar, N.; Gao, P.; Seshasai, S.R.; Gobin, R.; Kaptoge, S.; Di Angelantonio, E.; Ingelsson, E.; Lawlor, D.A.; Selvin, E.; Stampfer, M.; et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: A collaborative meta-analysis of 102 prospective studies. Lancet 2010, 375, 2215–2222. [Google Scholar] [CrossRef]
- Barquera, S.; Hernández-Alcaraz, C.; Jáuregui, A.; Medina, C.; Mendoza-Herrera, K.; Pedroza-Tobias, A.; Tolentino Mayo, L.; Guillen Pineda, L.E.; López-Ridaura, R.; Aguilar Salinas, C.A. Diabetes awareness, treatment, and control among Mexico City residents. Diabetology 2021, 2, 2. [Google Scholar] [CrossRef]
- Weihrauch-Blüher, S.; Wiegand, S. Risk factors and implications of childhood obesity. Curr. Obes. Rep. 2017, 7, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Genuth, S.; Alberti, K.G.; Bennett, P.; Buse, J.; Defronzo, R.; Kahn, R.; Kitzmiller, J.; Knowler, W.C.; Lebovitz, H.; Lernmark, A.; et al. Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care 2003, 26, 3160–3167. [Google Scholar] [CrossRef] [Green Version]
- American Diabetes Association. Introduction: Standards of Medical Care in Diabetes—2021. Diabetes Care 2021, 44 (Suppl. 1), S1–S2. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2013, 32 (Suppl. 1), S62–S74. [Google Scholar] [CrossRef] [Green Version]
- Lingvay, I. Sodium glucose cotransporter 2 and dipeptidyl peptidase-4 inhibition: Promise of a dynamic duo. Endocr. Pract. 2017, 23, 831–840. [Google Scholar] [CrossRef] [PubMed]
- Kalra, S.; Kesavadev, J.; Chadha, M.; Kumar, G.V. Sodium-glucose Cotransporter-2 Inhibitors in Combination with Other Glucose-lowering Agents for the Treatment of Type 2 Diabetes Mellitus. Indian J. Endocrinol. Metab. 2018, 22, 827–836. [Google Scholar] [CrossRef] [PubMed]
- Lajara, R. Combination therapy with SGLT-2 inhibitors and GLP-1 receptor agonists as complementary agents that address multi-organ defects in type 2 diabetes. Postgrad. Med. 2019, 131, 555–565. [Google Scholar] [CrossRef] [Green Version]
- Chaudhury, A.; Duvoor, C.; Reddy Dendi, V.S.; Kraleti, S.; Chada, A.; Ravilla, R.; Marco, A.; Shekhawat, N.S.; Montales, M.T.; Kuriakose, K.; et al. Clinical review of antidiabetic drugs: Implications for Type 2 Diabetes Mellitus management. Front. Endocrinol. 2017, 8, 6. [Google Scholar] [CrossRef] [Green Version]
- Westermeier, F.; Holyoak, T.; Asenjo, J.L.; Gatica, R.; Nualart, F.; Burbulis, I.; Bertinat, R. Gluconeogenic enzymes in β-Cells: Pharmacological targets for improving insulin secretion. Trends Endocrinol. Metab. 2019, 30, 520–531. [Google Scholar] [CrossRef]
- Khunti, K.; Gomes, M.B.; Pocock, S.; Shestakova, M.V.; Pintat, S.; Fenici, P.; Hammar, N.; Medina, J. Therapeutic inertia in the treatment of hyperglycaemia in patients with type 2 diabetes: A systematic review. Diabetes Obes. Metab. 2018, 20, 427–437. [Google Scholar] [CrossRef] [Green Version]
- DeFronzo, R.A.; Ratner, R.E.; Han, J.; Kim, D.D.; Fineman, B.S.; Baron, A.D. Effects of exenatide (exendin-4) on glycemic control and weight over 30 weeks in metformin-treated patients with type 2 diabetes. Diabetes Care 2005, 28, 1092–1100. [Google Scholar] [CrossRef] [Green Version]
- Li, Z.; Zhou, Z.; Huang, G.; Hu, F.; Xiang, Y.; He, L. Exendin-4 protects mitochondria from reactive oxygen species induced apoptosis in pancreatic beta cells. PLoS ONE 2013, 8, e76172. [Google Scholar] [CrossRef]
- Yap, M.K.K.; Misuan, N. Exendin-4 from Heloderma suspectum venom: From discovery to its latest application as type II diabetes combatant. Basic Clin. Pharmacol. Toxicol. 2019, 124, 513–527. [Google Scholar] [CrossRef] [Green Version]
- Sanggaard, K.W.; Dyrlund, T.F.; Thomsen, L.R.; Nielsen, T.A.; Brøndum, L.; Wang, T.; Thøgersen, I.B.; Enghild, J.J. Characterization of the gila monster (Heloderma suspectum suspectum) venom proteome. Data Br. 2015, 3, 137–142. [Google Scholar] [CrossRef]
- Nathan, D.M.; Buse, J.B.; Davidson, M.B.; Ferrannini, E.; Holman, R.R.; Sherwin, R.; Zinman, B. American Diabetes Association, European Association for Study of Diabetes. Medical management of hyperglycemia in type 2 diabetes: A consensus algorithm for the initiation and adjustment of therapy: A consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2009, 32, 193–203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davies, M.J.; D’Alessio, D.A.; Fradkin, J.; Kernan, W.N.; Mathieu, C.; Mingrone, G.; Rossing, P.; Tsapas, A.; Wexler, D.J.; Buse, J.B. Management of hyperglycemia in type 2 diabetes, (2018). A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2018, 41, 2669–2701. [Google Scholar] [CrossRef] [Green Version]
- Garber, A.J.; Abrahamson, M.J.; Barzilay, J.I.; Blonde, L.; Bloomgarden, Z.T.; Bush, M.A.; Dagogo-Jack, S.; DeFronzo, R.A.; Einhorn, D.; Fonseca, V.A.; et al. Consensus statement by the American association of clinical endocrinologists and American college of endocrinology on the comprehensive type 2 diabetes management algorithm—2019 executive summary. Endocr. Pract. 2019, 25, 69–100. [Google Scholar] [CrossRef] [Green Version]
- Kosiborod, M.; Cavender, M.A.; Fu, A.Z.; Wilding, J.P.; Khunti, K.; Holl, R.W.; Norhammar, A.; Birkeland, K.I.; Jørgensen, M.E.; Thuresson, M.; et al. CVD-REAL Investigators and Study Group. Lower risk of heart failure and death in patients initiated on sodium-glucose cotransporter-2 inhibitors versus other glucose-lowering drugs: The CVD-REAL study (comparative effectiveness of cardiovascular outcomes in new users of sodium-glucose cotransporter-2 inhibitors). Circulation 2017, 136, 249–259. [Google Scholar] [CrossRef]
- Guillausseau, P.J.; Meas, T.; Virally, M.; Laloi-Michelin, M.; Médeau, V.; Kevorkian, J.P. Abnormalities in insulin secretion in type 2 diabetes mellitus. Diabetes Metab. 2008, 34 (Suppl. 2), S43–S48. [Google Scholar] [CrossRef]
- McGivern, J.G. Ziconotide: A review of its pharmacology and use in the treatment of pain. Neuropsychiatr. Dis. Treat. 2007, 3, 69–85. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olivera, B.M.; McIntosh, J.M.; Cruz, L.J.; Luque, F.A.; Gray, W.R. Purification and sequence of a presynaptic peptide toxin from Conus geographus venom. Biochemistry 1984, 23, 5087–5090. [Google Scholar] [CrossRef]
- Olivera, B.M.; Rivier, J.; Clark, C.; Ramilo, C.A.; Corpuz, G.P.; Abogadie, F.C.; Mena, E.E.; Woodward, S.R.; Hillyard, D.R.; Cruz, L.J. Diversity of Conus neuropeptides. Science 1990, 249, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Olivera, B.M. Conus venom peptides, receptor and ion channel targets, and drug design: 50 million years of neuropharmacology. Mol. Biol. Cell 1997, 8, 2101–2109. [Google Scholar] [CrossRef] [Green Version]
- Biggs, J.S.; Watkins, M.; Puillandre, N.; Ownby, J.P.; Lopez-Vera, E.; Christensen, S.; Juárez-Moreno, K.; Bernaldez, J.; Licea-Navarro, A.; Corneli, P.S.; et al. Evolution of Conus Peptide Toxins: Analysis of Conus californicus Reeve, 1844. Mol. Phylogenet. Evol. 2010, 56, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Puillandre, N.; Duda, T.F.; Meyer, C.; Olivera, B.M.; Bouchet, P. One, four or 100 genera? A new classification of the cone snails. J. Molluscan Stud. 2015, 81, 1–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Craig, A.G.; Jimenez, E.C.; Dykert, J.; Nielsen, D.B.; Gulyas, J.; Abogadie, F.C.; Porter, J.; Rivier, J.E.; Cruz, L.J.; Olivera, B.M.; et al. A novel post translational modification involving bromination of tryptophan—identification of the residue, l-6-bromotryptophan, in peptides from Conus imperialis and Conus radiatus venom. J. Biol. Chem. 1997, 272, 4689–4698. [Google Scholar] [CrossRef] [Green Version]
- Terlau, H.; Olivera, B. Conus Venoms: A rich source of novel ion channel-targeted peptides. Physiol. Rev. 2004, 84, 41–68. [Google Scholar] [CrossRef] [Green Version]
- Olivera, B.M.; Teichert, R.W. Diversity of the neurotoxic Conus peptides: A model for concerted pharmacological discovery. Mol. Interv. 2007, 7, 251–260. [Google Scholar] [CrossRef] [PubMed]
- Severgnini, M.; Sherman, J.; Sehgal, A.; Jayaprakash, N.K.; Aubin, J.; Wang, G.; Zhang, L.; Peng, C.G.; Yucius, K.; Butler, J.; et al. A rapid two-step method for isolation of functional primary mouse hepatocytes: Cell characterization and asialoglycoprotein receptor-based assay development. Cytotechnology 2012, 64, 187–195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Szot, G.L.; Koudria, P.; Bluestone, J.A. Transplantation of pancreatic islets into the kidney capsule of diabetic mice. J. Vis. Exp. 2007, 9, e404. [Google Scholar] [CrossRef]
- Hamaguchi, K.; Gaskins, H.R.; Leiter, E.H. NIT-1, a pancreatic beta-cell line established from a transgenic NOD/Lt mouse. Diabetes 1991, 40, 842–849. [Google Scholar] [CrossRef]
- Wu, Y.J.; Wu, Y.B.; Fang, Z.H.; Chen, M.Q.; Wang, Y.F.; Wu, C.Y.; Lv, M.A. Danzhi Jiangtang capsule mediates NIT-1 Insulinoma cell proliferation and apoptosis by GLP-1/Akt signaling pathway. Evid. Based Complement. Altern. Med. 2019, 5356825. [Google Scholar] [CrossRef]
- Najjar, A.; Alawi, M.; AbuHeshmeh, N.; Sallam, A. A rapid, isocratic HPLC method for determination of insulin and its degradation product. Adv. Pharm. 2014, 6. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.; Yoon, H.J.; Kang, M.G.; Kim, G.J.; Shin, S.Y.; Baek, S.H.; Lee, J.G.; Bai, J.; Lee, S.Y.; Choi, M.J.; et al. Identification and evaluation of cytotoxicity of peptide liposome incorporated citron extracts in an in vitro system. Int. J. Mol. Sci. 2018, 19, 626. [Google Scholar] [CrossRef] [Green Version]
- Lee, H.S.; Jeong, J.; Lee, K.J. Characterization of vesicles secreted from insulinoma NIT-1 cells. J. Proteome Res. 2009, 8, 2851–2862. [Google Scholar] [CrossRef]
- Andrikopoulos, S.; Blair, A.R.; Deluca, N.; Fam, B.C.; Proietto, J. Evaluating the glucose tolerance test in mice. Am. J. Physiol. Endocrinol. Metab. 2008, 295, E1323–E1332. [Google Scholar] [CrossRef] [Green Version]
- Geskovski, N.; Kuzmanovska, S.; Simonoska Crcarevska, M.; Calis, S.; Dimchevska, S.; Petrusevska, M.; Zdravkovski, P.; Goracinova, K. Comparative biodistribution studies of technetium-99 m radiolabeled amphiphilic nanoparticles using three different reducing agents during the labeling procedure. J. Label. Comp. Radiopharm. 2013, 56, 689–695. [Google Scholar] [CrossRef] [PubMed]
- Hiriart, M.; Vidaltamayo, R.; Sánchez-Soto, M.C. Nerve and fibroblast growth factors as modulators of pancreatic beta cell plasticity and insulin secretion. Isr. Med. Assoc. J. 2001, 3, 114–116. [Google Scholar]
- de la Cruz, L.; Puente, E.I.; Reyes-Vaca, A.; Arenas, I.; Garduño, J.; Bravo-Martínez, J.; Garcia, D.E. PIP2 in pancreatic β-cells regulates voltage-gated calcium channels by a voltage-independent pathway. Am. J. Physiol. Cell Physiol. 2016, 311, C630–C640. [Google Scholar] [CrossRef] [PubMed]
- Kahn, S.E. The importance of β-cell failure in the development and progression of type 2 diabetes. Int. J. Clin. Endocrinol. Metab. 2001, 86, 4047–4058. [Google Scholar] [CrossRef] [Green Version]
- Molina, J.; Rodriguez-Diaz, R.; Fachado, A.; Jacques-Silva, M.C.; Berggren, P.O.; Caicedo, A. Control of insulin secretion by cholinergic signaling in the human pancreatic islet. Diabetes 2014, 63, 2714–2726. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klonoff, D.C.; Buse, J.B.; Nielsen, L.L.; Guan, X.; Bowlus, C.L.; Holcombe, J.H.; Wintle, M.E.; Maggs, D.G. Exenatide effects on diabetes, obesity, cardiovascular risk factors and hepatic biomarkers in patients with type 2 diabetes treated for at least 3 years. Curr. Med. Res. Opin. 2008, 24, 275–286. [Google Scholar] [CrossRef] [PubMed]
- Henquin, J.C. Paracrine and autocrine control of insulin secretion in human islets: Evidence and pending questions. Am. J. Physiol. Endocrinol. Metab. 2021, 320, E78–E86. [Google Scholar] [CrossRef] [PubMed]
- Hiriart, M.; Aguilar-Bryan, L. Channel regulation of glucose sensing in the pancreatic β-cell. Am. J. Physiol. Endocrinol. Metab. 2008, 295, E1298–E1306. [Google Scholar] [CrossRef] [Green Version]
- Suga, S.; Kanno, T.; Nakano, K.; Takeo, T.; Dobashi, Y.; Wakui, M. GLP-I (7–36) amide augments Ba2+ current through L-type Ca2+ channel of rat pancreatic beta-cell in a cAMP-dependent manner. Diabetes 1997, 46, 1755–1760. [Google Scholar] [CrossRef] [PubMed]
- Catterall, W.A. Voltage-gated calcium channels. Cold Spring Harb. Perspect. Biol. 2011, 3, a003947. [Google Scholar] [CrossRef]
- Henquin, J.C. Triggering and amplifying pathways of regulation of insulin secretion by glucose. Diabetes 2000, 49, 1751–1760. [Google Scholar] [CrossRef] [Green Version]
- Ashcroft, F.M.; Proks, P.; Smith, P.A.; Ammälä, C.; Bokvist, K.; Rorsman, P. Stimulus-secretion coupling in pancreatic beta cells. J. Cell. Biochem. 1994, 55, 54–65. [Google Scholar] [CrossRef]
- Gilbert, M.; Jung, S.-R.; Reed, B.J.; Sweet, I.R. Islet oxygen consumption and insulin secretion tightly coupled to calcium derived from L-type calcium channels but not from the endoplasmic reticulum. J. Biol. Chem. 2008, 283, 24334–24342. [Google Scholar] [CrossRef] [Green Version]
- Takahashi, N.; Hatakeyama, H.; Okado, H.; Noguchi, J.; Ohno, M.; Kasai, H. SNARE Conformational changes that prepare vesicles for exocytosis. Cell Metab. 2010, 12, 19–29. [Google Scholar] [CrossRef] [Green Version]
- Ashcroft, F.M.; Rorsman, P. Electrophysiology of the pancreatic beta-cell. Prog. Biophys. Mol. Biol. 1989, 54, 87–143. [Google Scholar] [CrossRef]
- Henquin, J.C. Pathways in beta-cell stimulus-secretion coupling as targets for therapeutic insulin secretagogues. Diabetes 2004, 53 (Suppl. 3), S48–S58. [Google Scholar] [CrossRef] [PubMed]
- Rutter, G.A.; Pullen, T.J.; Hodson, D.J.; Martinez-Sanchez, A. Pancreatic β-cell identity, glucose sensing and the control of insulin secretion. Biochem. J. 2015, 466, 203–218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Diabetes Association. 9. Pharmacologic Approaches to Glycemic Treatment: Standards of Medical Care in Diabetes—2021. Diabetes Care 2021, 44 (Suppl. 1), S111–S124. [Google Scholar] [CrossRef] [PubMed]
- Fatherazi, S.; Cook, D.L. Specificity of tetraethylammonium and quinine for three K channels in insulin-secreting cells. J. Membr. Biol. 1991, 120, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Donatsch, P.; Lowe, D.A.; Richardson, B.P.; Taylor, P. The functional significance of sodium channels in pancreatic beta-cell membranes. J. Physiol. 1977, 267, 357–376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silbering, A.F.; Benton, R. Ionotropic and metabotropic mechanisms in chemoreception: ‘chance or design’? EMBO Rep. 2010, 11, 173–179. [Google Scholar] [CrossRef] [Green Version]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lugo-Fabres, P.H.; Otero-Sastre, L.M.; Bernáldez-Sarabia, J.; Camacho-Villegas, T.A.; Sánchez-Campos, N.; Serrano-Bello, J.; Medina, L.A.; Muñiz-Hernández, S.; de la Cruz, L.; Arenas, I.; et al. Potential Therapeutic Applications of Synthetic Conotoxin s-cal14.2b, Derived from Californiconus californicus, for Treating Type 2 Diabetes. Biomedicines 2021, 9, 936. https://doi.org/10.3390/biomedicines9080936
Lugo-Fabres PH, Otero-Sastre LM, Bernáldez-Sarabia J, Camacho-Villegas TA, Sánchez-Campos N, Serrano-Bello J, Medina LA, Muñiz-Hernández S, de la Cruz L, Arenas I, et al. Potential Therapeutic Applications of Synthetic Conotoxin s-cal14.2b, Derived from Californiconus californicus, for Treating Type 2 Diabetes. Biomedicines. 2021; 9(8):936. https://doi.org/10.3390/biomedicines9080936
Chicago/Turabian StyleLugo-Fabres, Pavel H., Leslie M. Otero-Sastre, Johanna Bernáldez-Sarabia, Tanya A. Camacho-Villegas, Noemi Sánchez-Campos, Janeth Serrano-Bello, Luis A. Medina, Saé Muñiz-Hernández, Lizbeth de la Cruz, Isabel Arenas, and et al. 2021. "Potential Therapeutic Applications of Synthetic Conotoxin s-cal14.2b, Derived from Californiconus californicus, for Treating Type 2 Diabetes" Biomedicines 9, no. 8: 936. https://doi.org/10.3390/biomedicines9080936
APA StyleLugo-Fabres, P. H., Otero-Sastre, L. M., Bernáldez-Sarabia, J., Camacho-Villegas, T. A., Sánchez-Campos, N., Serrano-Bello, J., Medina, L. A., Muñiz-Hernández, S., de la Cruz, L., Arenas, I., Barajas-Martínez, A., Garcia, D. E., Nuñez-Garcia, L., González-Canudas, J., & Licea-Navarro, A. F. (2021). Potential Therapeutic Applications of Synthetic Conotoxin s-cal14.2b, Derived from Californiconus californicus, for Treating Type 2 Diabetes. Biomedicines, 9(8), 936. https://doi.org/10.3390/biomedicines9080936








