Role of SpO2/FiO2 Ratio and ROX Index in Predicting Early Invasive Mechanical Ventilation in COVID-19. A Pragmatic, Retrospective, Multi-Center Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Settings
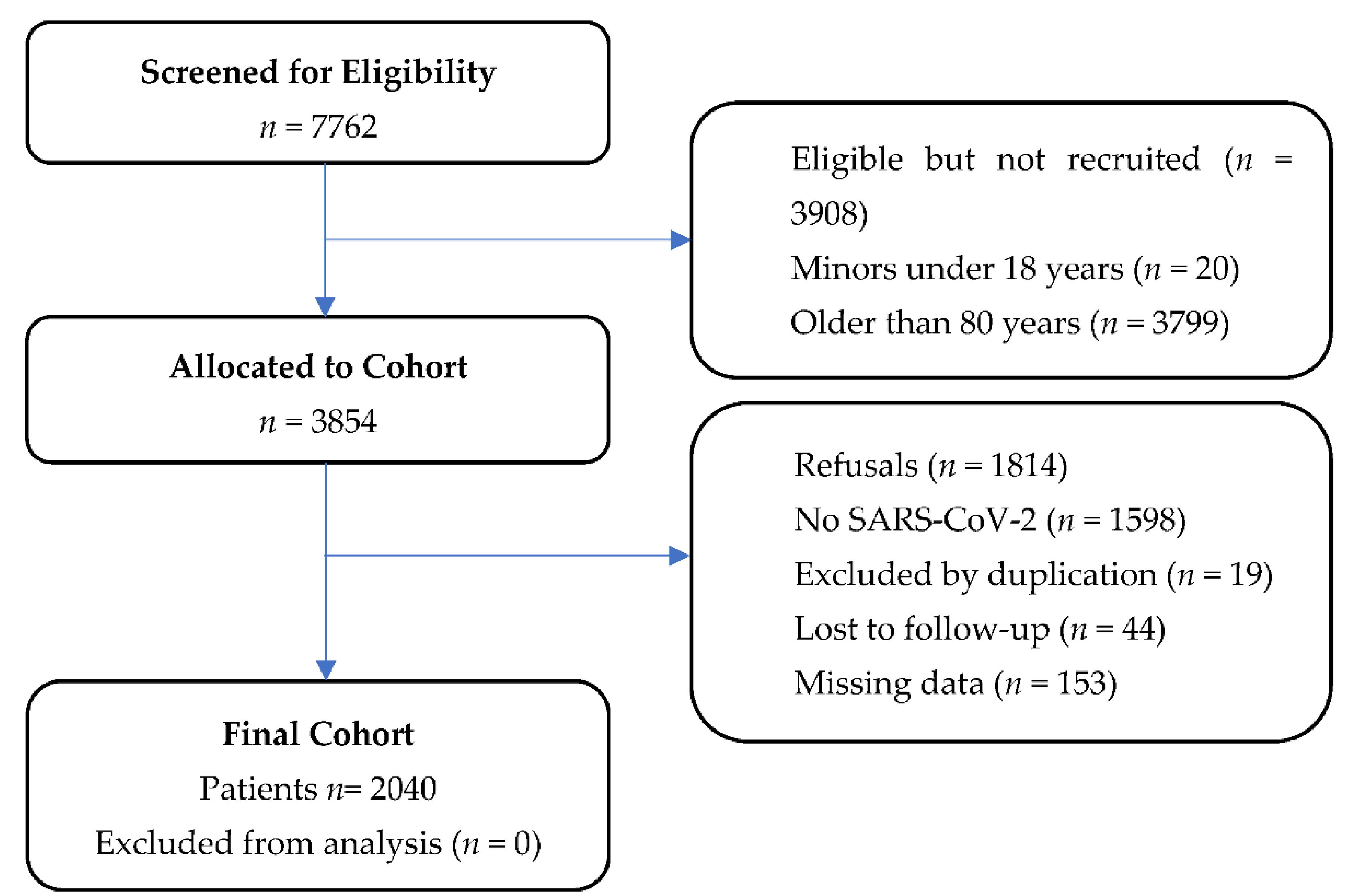
2.2. Population
2.3. Outcome
2.4. Measures and Data Abstraction
2.5. Primary Data Analysis
2.6. Statistical Analyses
3. Results
3.1. Cohort Overview
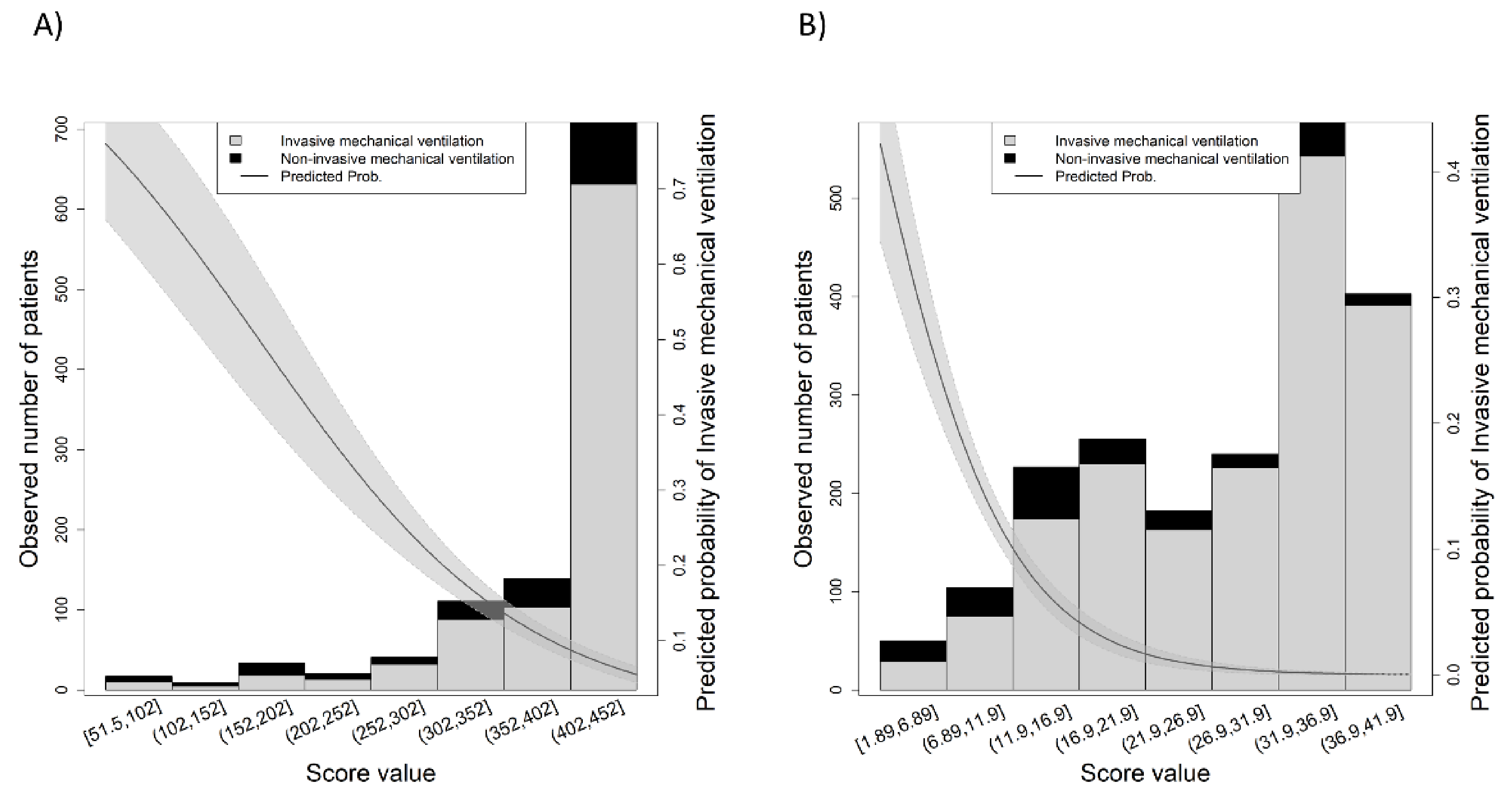
3.2. SpO2/FiO2 Ratio and ROX Index Discrimination
3.3. SpO2/FiO2 Ratio and Age Association
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rubio, O.; Estella, A.; Cabre, L.; Saralegui-Reta, I.; Martin, M.C.; Zapata, L.; Esquerda, M.; Ferrer, R.; Castellanos, A.; Trenado, J.; et al. Ethical recommendations for a difficult decision-making in intensive care units due to the exceptional situation of crisis by the COVID-19 pandemia: A rapid review & consensus of experts. Med. Intensiv. 2020, 44, 439–445. [Google Scholar]
- Escudero-Acha, P.; Leizaola, O.; Lázaro, N.; Cordero, M.; Gomez-Acebo, I.; González-Castro, A. Age as a limiting factor of admission to an intensive care unit. Med. Intensiv. 2020. Online ahead of print. [Google Scholar] [CrossRef]
- Griffin, K.M.; Karas, M.G.; Ivascu, N.S.; Lief, L. Hospital Preparedness for COVID-19: A Practical Guide from a Critical Care Perspective. Am. J. Respir. Crit. Care Med. 2020, 201, 1337–1344. [Google Scholar] [CrossRef] [Green Version]
- Lentz, T.; Groizard, C.; Colomes, A.; Ozguler, A.; Baer, M.; Loeb, T. Collective Critical Care Ambulance: An innovative transportation of critical care patients by bus in COVID-19 pandemic response. Scand. J. Trauma Resusc. Emerg. Med. 2021, 29, 78. [Google Scholar] [CrossRef] [PubMed]
- Ferron, R.; Agarwal, G.; Cooper, R.; Munkley, D. The effect of COVID-19 on emergency medical service call volumes and patient acuity: A cross-sectional study in Niagara, Ontario. BMC Emerg. Med. 2021, 21, 39. [Google Scholar] [CrossRef] [PubMed]
- Grasselli, G.; Greco, M.; Zanella, A.; Albano, G.; Antonelli, M.; Bellani, G.; Bonanomi, E.; Cabrini, L.; Carlesso, E.; Castelli, G.; et al. Risk Factors Associated with Mortality among Patients with COVID-19 in Intensive Care Units in Lombardy, Italy. JAMA Intern. Med. 2020, 180, 1345–1355. [Google Scholar] [CrossRef] [PubMed]
- Gibson, P.G.; Qin, L.; Puah, S.H. COVID-19 acute respiratory distress syndrome (ARDS): Clinical features and differences from typical pre-COVID-19 ARDS. Med. J. Aust. 2020, 213, 54–56.e1. [Google Scholar] [CrossRef]
- Gattinoni, L.; Chiumello, D.; Rossi, S. COVID-19 pneumonia: ARDS or not? Crit. Care 2020, 24, 154. [Google Scholar] [CrossRef] [Green Version]
- De Vita, N.; Scotti, L.; Cammarota, G.; Racca, F.; Pissaia, C.; Maestrone, C.; Colombo, D.; Olivieri, C.; Della Corte, F.; Barone-Adesi, F.; et al. Predictors of intubation in COVID-19 patients treated with out-of-ICU continuous positive airway pressure. Pulmonology 2021. Online ahead of print. [Google Scholar] [CrossRef]
- Gianstefani, A.; Farina, G.; Salvatore, V.; Alvau, F.; Artesiani, M.L.; Bonfatti, S.; Campinoti, F.; Caramella, I.; Ciordinik, M.; Lorusso, A.; et al. Role of ROX index in the first assessment of COVID-19 patients in the emergency department. Intern. Emerg. Med. 2021. Online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Goh, K.J.; Chai, H.Z.; Ong, T.H.; Sewa, D.W.; Phua, G.C.; Tan, Q.L. Early prediction of high flow nasal cannula therapy outcomes using a modified ROX index incorporating heart rate. J. Intensiv. Care 2020, 8, 41. [Google Scholar] [CrossRef]
- Suliman, L.A.; Abdelgawad, T.T.; Farrag, N.S.; Abdelwahab, H.W. Validity of ROX index in prediction of risk of intubation in patients with COVID-19 pneumonia. Adv. Respir. Med. 2021, 89, 1–7. [Google Scholar] [CrossRef]
- Marraro, G.A.; Li, Z.; Piga, M.A. Searching for Biomarkers With Predictive Value in Pediatric Acute Lung Injury: Can SpO2/FIO2 Be Used Instead of PaO2/FIO2 as an Index to Predict Outcome? Pediatr. Crit. Care Med. 2018, 18, 294–296. [Google Scholar] [CrossRef] [PubMed]
- Roca, O.; Caralt, B.; Messika, J.; Samper, M.; Sztrymf, B.; Hernández, G.; García-de-Acilu, M.; Frat, J.-P.; Masclans, J.R.; Ricard, J.-D. An Index Combining Respiratory Rate and Oxygenation to Predict Outcome of Nasal High-Flow Therapy. Am. J. Respir. Crit. Care Med. 2019, 199, 1368–1376. [Google Scholar] [CrossRef] [PubMed]
- Prower, E.; Grant, D.; Bisquera, A.; Breen, C.P.; Camporota, L.; Gavrilovski, M.; Ponting, M.; Douirih, A.; Gloveri, G.W. The ROX index has greater predictive validity than NEWS2 for deterioration in Covid-19. EClinicalMedicine 2021, 35, 100828. [Google Scholar] [CrossRef] [PubMed]
- Fink, D.L.; Goldman, N.R.; Cai, J.; El-Shakankery, K.H.; Sismey, G.E.; Gupta-Wright, A.; Tai, C.X. ROX Index to Guide Management of COVID-19 Pneumonia. Ann. Am. Thorac. Soc 2021. Online ahead of print. [Google Scholar] [CrossRef]
- Brown, S.M.; Grissom, C.K.; Moss, M.; Rice, T.W.; Schoenfeld, D.; Hou, P.C.; Thompson, B.T.; Brower, R.G.; NIH/NHLBI PETAL Network Collaborators. Nonlinear Imputation of Pao2/Fio2 from Spo2/Fio2 among Patients with Acute Respiratory Distress Syndrome. Chest 2016, 150, 307–313. [Google Scholar] [CrossRef] [Green Version]
- Martín-Rodríguez, F.; López-Izquierdo, R.; del Pozo Vegas, C.; Delgado-Benito, J.F.; Ortega, G.J.; Villamor, M.A.C.; Sanz-García, A. Association of Prehospital Oxygen Saturation to Inspired Oxygen Ratio with 1-, 2-, and 7-Day Mortality. JAMA Netw. Open 2021, 4, e215700. [Google Scholar] [CrossRef]
- Lu, X.; Jiang, L.; Chen, T.; Wang, Y.; Zhang, B.; Hong, Y. Continuously available ratio of SpO/FiO serves as a noninvasive prognostic marker for intensive care patients with COVID-19. Respir. Res. 2020, 21, 194. [Google Scholar] [CrossRef]
- Catoire, P.; Tellier, E.; de la Rivière, C.; Beauvieux, M.C.; Valdenaire, G.; Galinski, M.; Revel, P.; Combes, X.; Gil-Jardiné, C. Assessment of the SpO/FiO ratio as a tool for hypoxemia screening in the emergency department. Am. J. Emerg. Med. 2021, 44, 116–120. [Google Scholar] [CrossRef]
- Lemiale, V.; Dumas, G.; Demoule, A.; Pène, F.; Kouatchet, A.; Bisbal, M.; Nseir, S.; Argaud, L.; Kontar, L.; Klouche, K.; et al. Performance of the ROX index to predict intubation in immunocompromised patients receiving high-flow nasal cannula for acute respiratory failure. Ann. Intensiv. Care 2021, 11, 17. [Google Scholar] [CrossRef]
- Vega, M.L.; Dongilli, R.; Olaizola, G.; Colaianni, N.; Sayat, M.C.; Pisani, L.; Romagnoli, M.; Spoladore, G.; Prediletto, I.; Montiel, G.; et al. COVID-19 Pneumonia and ROX index: Time to set a new threshold for patients admitted outside the ICU. Pulmonology 2021. Online ahead of print. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Cook, T.M.; El-Boghdadly, K.; McGuire, B.; McNarry, A.F.; Patel, A.; Higgs, A. Consensus guidelines for managing the airway in patients with COVID-19: Guidelines from the Difficult Airway Society, the Association of Anaesthetists the Intensive Care Society, the Faculty of Intensive Care Medicine and the Royal College of Anaesthetist. Anaesthesia 2020, 75, 785–799. [Google Scholar] [CrossRef] [PubMed]
- Leclerc, T.; Donat, N.; Donat, A.; Pasquier, P.; Libert, N.; Schaeffer, E.; D’Aranda, E.; Cotte, J.; Fontaine, B.; Perrigault, P.-F.; et al. Prioritisation of ICU treatments for critically ill patients in a COVID-19 pandemic with scarce resources. Anaesth. Crit. Care Pain Med. 2020, 39, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Karagiannidis, C.; Mostert, C.; Hentschker, C.; Voshaar, T.; Malzahn, J.; Schillinger, G.; Klauber, J.; Janssens, U.; Marx, G.; Weber-Carstens, S.; et al. Case characteristics, resource use, and outcomes of 10,021 patients with COVID-19 admitted to 920 German hospitals: An observational study. Lancet Respir. Med. 2020, 8, 853–862. [Google Scholar] [CrossRef]
- Emanuel, E.J.; Persad, G.; Upshur, R.; Thome, B.; Parker, M.; Glickman, A.; Zhang, C.; Boyle, C.; Smith, M.; Phillips, J.P. Fair Allocation of Scarce Medical Resources in the Time of Covid-19. N. Engl. J. Med. 2020, 382, 2049–2055. [Google Scholar] [CrossRef] [PubMed]
- Shashikumar, S.P.; Wardi, G.; Paul, P.; Carlile, M.; Brenner, L.N.; Hibbert, K.A.; North, C.M.; Mukerji, S.S.; Robbins, G.K.; Shao, Y.-P.; et al. Development and Prospective Validation of a Deep Learning Algorithm for Predicting Need for Mechanical Ventilation. Chest 2021, 159, 2264–2273. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Tong, Z.; Guan, X.; Du, B.; Qiu, H.; Slutsky, A.S. Critical care crisis and some recommendations during the COVID-19 epidemic in China. Intensiv. Care Med. 2020, 46, 837–840. [Google Scholar] [CrossRef] [Green Version]
- Zucman, N.; Mullaert, J.; Roux, D.; Roca, O.; Ricard, J.D. Prediction of outcome of nasal high flow use during COVID-19-related acute hypoxemic respiratory failure. Intensiv. Care Med. 2020, 46, 1924–1926. [Google Scholar] [CrossRef]
- Chen, W.L.; Lin, W.T.; Kung, S.C.; Lai, C.C.; Chao, C.M. The value of oxygenation saturation index in predicting the outcomes of patients with acute respiratory distress syndrome. J. Clin. Med. 2018, 7, 205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frat, J.P.; Marie, D.; Thille, A.W. Acute respiratory failure:non intubation assist methods for the acutely deteriorating patient. Curr. Opin. Crit. Care 2019, 25, 591–596. [Google Scholar] [CrossRef] [PubMed]
- Seymour, C.W.; Liu, V.X.; Iwashyna, T.J.; Brunkhorst, F.M.; Rea, T.D.; Scherag, A.; Rubenfeld, G.; Kahn, J.M.; Shankar-Hari, M.; Singer, M.; et al. Assessment of clinical criteria for sepsis: For the third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA 2016, 315, 762. [Google Scholar] [CrossRef] [Green Version]
- García-Gordillo, J.A.; Camiro-Zúñiga, A.; Aguilar-Soto, M.; Cuenca, D.; Cadena-Fernández, A.; Khouri, L.S.; Rayek, J.N.; Mercado, M.; The ARMII Study Group. COVID-IRS: A novel predictive score for risk of invasive mechanical ventilation in patients with COVID-19. PLoS ONE 2021, 16, e0248357. [Google Scholar] [CrossRef]
- Tobin, M.J.; Laghi, F.; Jubran, A. Why COVID-19 Silent Hypoxemia Is Baffling to Physicians. Am. J. Respir. Crit. Care Med. 2020, 202, 356–360. [Google Scholar] [CrossRef] [PubMed]
- Bickler, P.E.; Feiner, J.R.; Lipnick, M.S.; McKleroy, W. “Silent” Presentation of Hypoxemia and Cardiorespiratory Compensation in COVID-19. Anesthesiology 2021, 134, 262–269. [Google Scholar] [CrossRef]
- Quaresima, V.; Ferrari, M. COVID-19: Efficacy of prehospital pulse oximetry for early detection of silent hypoxemia. Crit. Care 2020, 24, 501. [Google Scholar] [CrossRef]
- Fang, X.; Li, S.; Yu, H.; Wang, P.; Zhang, Y.; Chen, Z.; Li, Y.; Cheng, L.; Li, W.; Jia, H.; et al. Epidemiological, comorbidity factors with severity and prognosis of COVID-19: A systematic review and meta-analysis. Aging 2020, 12, 12493–12503. [Google Scholar] [CrossRef]
- Chen, Y.; Klein, S.L.; Garibaldi, B.T.; Li, H.; Wu, C.; Osevala, N.M.; Li, T.; Margolick, J.B.; Pawelec, G.; Leng, S.X. Aging in COVID-19: Vulnerability, immunity and intervention. Ageing Res. Rev. 2021, 65, 101205. [Google Scholar] [CrossRef]
- Meng, L.; Qiu, H.; Wan, L.; Ai, Y.; Xue, Z.; Guo, Q.; Deshpande, R.; Zhang, L.; Meng, J.; Tong, C.; et al. Intubation and Ventilation amid the COVID-19 Outbreak: Wuhan’s Experience. Anesthesiology 2020, 132, 1317–1332. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Variable 1 | Total | IMV | Non-IMV | p Value 2 |
|---|---|---|---|---|
| No. (%) with data | 2040 (100) | 207 (10.1) | 1833 (89.9) | NA |
| Age, year | 67 (55–75) | 68 (62–75) | 66 (54–75) | <0.001 |
| Age, group, year | ||||
| <40 | 165 (8.1) | 4 (1.9) | 161 (8.8) | |
| 41–55 | 367 (18) | 25 (12.1) | 342 (18.7) | 0.003 |
| 56–70 | 687 (33.7) | 91 (44) | 596 (32.5) | 0.041 |
| >71 | 821 (40.2) | 87 (42) | 734 (40) | 0.113 |
| Sex | ||||
| Female | 883 (43.3) | 152 (73.4) | 828 (45.2) | |
| Male | 1157 (56.7) | 55 (22.6) | 1005 (54.8) | <0.001 |
| Nursing homes | 288 (14.1) | 6 (2.9) | 282 (5.4) | <0.001 |
| Zone, urban | 1117 (54.1) | 113 (54.9) | 1004 (54.8) | 0.960 |
| Triage ED evaluation | ||||
| Respiratory rate, bpm | 14 (12–24) | 24 (13–28) | 14 (12–21) | <0.001 |
| Pulse oximetry saturation, % | 95 (91–97) | 89 (83–93) | 95 (82–97) | <0.001 |
| Fraction of inspired oxygen, % | 0.21 (0.21–0.21) | 0.21 (0.21–0.24) | 0.21 (0.21–0.21) | <0.001 |
| Systolic arterial pressure, mmHg | 126 (113–143) | 122 (110−139) | 126 (113–141) | 0.047 |
| Diastolic arterial pressure, mmHg | 76 (67–84) | 72 (64–82) | 76 (68–84) | 0.009 |
| Heart rate, bpm | 90 (78–101) | 90 (79–105) | 90 (78–101) | 0.482 |
| Temperature, °C | 36.7 (36.2–37.3) | 37 (36.2–37.8) | 36.7 (36.2–37.3) | 0.006 |
| Glasgow coma scale, point | 15 (15–15) | 15 (15–15) | 15 (15–15) | 0.421 |
| Outcomes | ||||
| SpO2/FiO2 ratio | 448 (424–462) | 405 (319–438) | 452 (429–462) | <0.001 |
| ROX index | 31.3 (18.2–35.9) | 16.9 (11.9–30.9) | 32.1 (19.5–36.2) | <0.001 |
| Hospital-inpatient | 1453 (71.2) | 207 (100) | 1246 (68) | <0.001 |
| Hospitalization time, day | 9 (5–16) | 26 (14–46) | 8 (5–13) | <0.001 |
| Intensive care unit-admission | 225 (11) | 197 (95.2) | 28 (1.5) | <0.001 |
| Intensive care unit time, day | 16 (7–30) | 15 (7–30) | 10 (5–64) | <0.001 |
| In-hospital mortality | 251 (12.3) | 73 (35.3) | 178 (9.7) | <0.001 |
| Out-hospital mortality | 58 (2.8) | 7 (3.4) | 51 (2.8) | 0.623 |
| Aggregate mortality | 309 (15.1) | 80 (38.6) | 229 (12.5) | <0.001 |
| CCI, point | 1 (0–2) | 1 (0–2) | 1 (0–2) | 0.733 |
| AIDS | 3 (0.1) | 0 | 3 (0.2) | NA |
| Solid tumor metastatic | 30 (1.5) | 2 (1) | 28 (1.5) | 0.525 |
| Liver disease severe | 54 (2.6) | 4 (1.9) | 50 (2.7) | 0.499 |
| Lymphoma | 11 (0.5) | 0 | 11 (0.6) | NA |
| Leukemia | 22 (1.1) | 2 (1) | 20 (1.1) | 0.869 |
| Solid tumor localized | 233 (11.4) | 22 (10.6) | 211 (11.5) | 0.705 |
| DM end organ damage | 88 (4.3) | 14 (6.8) | 74 (4) | 0.067 |
| Severe chronic kidney disease | 168 (8.2) | 21 (10.1) | 147 (8) | 0.292 |
| Hemiplegia | 48 (2.4) | 1 (0.5) | 47 (2.6) | 0.061 |
| DM uncomplicated | 345 (16.9) | 42 (20.3) | 303 (16.5) | 0.172 |
| Liver disease mild | 63 (3.1) | 8 (3.9) | 55 (3) | 0.496 |
| Peptic ulcer disease | 54 (2.6) | 9 (4.3) | 45 (2.5) | 0.108 |
| Connective disease | 69 (3.3) | 7 (3.4) | 61 (3.3) | 0.967 |
| COPD | 174 (8.5) | 20 (9.7) | 154 (8.4) | 0.539 |
| Dementia | 154 (7.5) | 1 (0.5) | 153 (8.3) | <0.001 |
| Cerebrovascular disease | 112 (5.5) | 11 (5.3) | 101 (5.5) | 0.907 |
| Peripheral vascular disease | 140 (6.9) | 22 (10.6) | 118 (6.4) | 0.024 |
| Congestive heart failure | 107 (5.2) | 14 (6.8) | 93 (5.1) | 0.302 |
| Myocardial infarction | 136 (6.7) | 20 (9.7) | 116 (6.3) | 0.068 |
| Variable 1 | <40 | 41–55 | 56–70 | >70 | p Value 2 |
|---|---|---|---|---|---|
| No. (%) with data | 165 (8.1) | 367 (18) | 687 (33.7) | 821 (40.2) | NA |
| Age, y | 32 (26–38) | 50 (45–53) | 64 (60–67) | 76 (73–78) | NA |
| Sex, female | |||||
| Female | 98 (59.4) | 176 (48) | 262 (38.1) | 346 (42.3) | <0.001 |
| Male | 67 (40.6) | 191 (52) | 425 (61.9) | 474 (57.7) | <0.001 |
| Nursing homes | 3 (1.8) | 14 (3.8) | 76 (11.1) | 195 (23.8) | <0.001 |
| Zone, urban | 99 (60) | 188 (51.2) | 378 (55) | 452 (55.1) | 0.293 |
| Triage ED evaluation | |||||
| Respiratory rate, bpm | 13 (12–15) | 14 (12–20) | 14 (12–24) | 14 (13–25) | <0.001 |
| Pulse oximetry saturation, % | 97 (95–99) | 96 (93–98) | 94 (91–96) | 93 (89–96) | <0.001 |
| FiO2, % | 0.21 (0.21–0.21) | 0.21 (0.21–0.21) | 0.21 (0.21–0.21) | 0.21 (0.21–0.21) | <0.001 |
| SAP, mmHg | 120 (111–134) | 125 (114–138) | 127 (115–143) | 127 (111–144) | 0.008 |
| DAP, mmHg | 77 (70–85) | 80 (71–88) | 77 (68–84) | 72 (64–80) | <0.001 |
| Heart rate, bpm | 94 (82–106) | 92 (81–103) | 90 (80–100) | 87 (75–101) | <0.001 |
| Temperature, °C | 36.6 (36.2–37.1) | 36.8 (36.3–37.3) | 36.7 (36.2–37.4) | 36.6 (36.2–37.3) | 0.149 |
| Glasgow coma scale, point | 15 (15–15) | 15 (15–15) | 15 (15–15) | 15 (15–15) | 0.233 |
| Outcomes | |||||
| SpO2/FiO2 ratio | 462 (452–471) | 457 (443–467) | 448 (424–457) | 438 (405–452) | <0.001 |
| ROX index | 35.3 (30.3–38.2) | 32.6 (22.2–36.6) | 31.2 (18.3–35.9) | 28.8 (16.8–34.8) | <0.001 |
| IMV | 4 (2.4) | 25 (6.8) | 91 (13.2) | 87 (10.6) | <0.001 |
| Hospital-inpatient | 54 (32.7) | 203 (55.3) | 518 (75.4) | 678 (82.6) | <0.001 |
| Hospitalization time, day | 6 (3–10) | 8 (5–13) | 9 (6–16) | 9 (5–17) | <0.001 |
| Intensive care unit-admission | 4 (2.4) | 31 (8.4) | 92 (13.4) | 98 (11.9) | <0.001 |
| Intensive care unit time, day | 14 (4–31) | 7 (4–15) | 15 (7–28) | 22 (11–40) | <0.001 |
| In-hospital mortality | 1 (0.6) | 10 (2.7) | 61 (8.9) | 179 (21.8) | <0.001 |
| Out-hospital mortality | 0 | 3 (0.8) | 18 (2.6) | 37 (4.5) | <0.001 |
| Aggregate mortality | 1 (0.6) | 13 (3.5) | 79 (11.5) | 216 (26.3) | <0.001 |
| CCI, point | 0 (0–0) | 0 (0–1) | 1 (0–2) | 1 (0–3) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alberdi-Iglesias, A.; Martín-Rodríguez, F.; Ortega Rabbione, G.; Rubio-Babiano, A.I.; Núñez-Toste, M.G.; Sanz-García, A.; del Pozo Vegas, C.; Castro Villamor, M.A.; Martín-Conty, J.L.; Jorge-Soto, C.; et al. Role of SpO2/FiO2 Ratio and ROX Index in Predicting Early Invasive Mechanical Ventilation in COVID-19. A Pragmatic, Retrospective, Multi-Center Study. Biomedicines 2021, 9, 1036. https://doi.org/10.3390/biomedicines9081036
Alberdi-Iglesias A, Martín-Rodríguez F, Ortega Rabbione G, Rubio-Babiano AI, Núñez-Toste MG, Sanz-García A, del Pozo Vegas C, Castro Villamor MA, Martín-Conty JL, Jorge-Soto C, et al. Role of SpO2/FiO2 Ratio and ROX Index in Predicting Early Invasive Mechanical Ventilation in COVID-19. A Pragmatic, Retrospective, Multi-Center Study. Biomedicines. 2021; 9(8):1036. https://doi.org/10.3390/biomedicines9081036
Chicago/Turabian StyleAlberdi-Iglesias, Ana, Francisco Martín-Rodríguez, Guillermo Ortega Rabbione, Ana I. Rubio-Babiano, María G. Núñez-Toste, Ancor Sanz-García, Carlos del Pozo Vegas, Miguel A. Castro Villamor, José L. Martín-Conty, Cristina Jorge-Soto, and et al. 2021. "Role of SpO2/FiO2 Ratio and ROX Index in Predicting Early Invasive Mechanical Ventilation in COVID-19. A Pragmatic, Retrospective, Multi-Center Study" Biomedicines 9, no. 8: 1036. https://doi.org/10.3390/biomedicines9081036
APA StyleAlberdi-Iglesias, A., Martín-Rodríguez, F., Ortega Rabbione, G., Rubio-Babiano, A. I., Núñez-Toste, M. G., Sanz-García, A., del Pozo Vegas, C., Castro Villamor, M. A., Martín-Conty, J. L., Jorge-Soto, C., & López-Izquierdo, R. (2021). Role of SpO2/FiO2 Ratio and ROX Index in Predicting Early Invasive Mechanical Ventilation in COVID-19. A Pragmatic, Retrospective, Multi-Center Study. Biomedicines, 9(8), 1036. https://doi.org/10.3390/biomedicines9081036







