Regional Diversities in Fibrogenesis Weighed as a Key Determinant for Atrial Arrhythmogenesis
Abstract
:1. Introduction
1.1. Abnormal Distribution of Fibrotic Tissue in Atrial Electrical Coupling and Arrhythmogenesis
1.2. Fibrosis-Related Impairment of Biomechanical–Electrical Properties
1.3. Enhancement of Atrial Arrhythmogenesis by Paracrine Signaling from Fibrosis
2. Diversity in Atrial Fibrogenesis and Arrhythmogenesis: Clinical Evidence
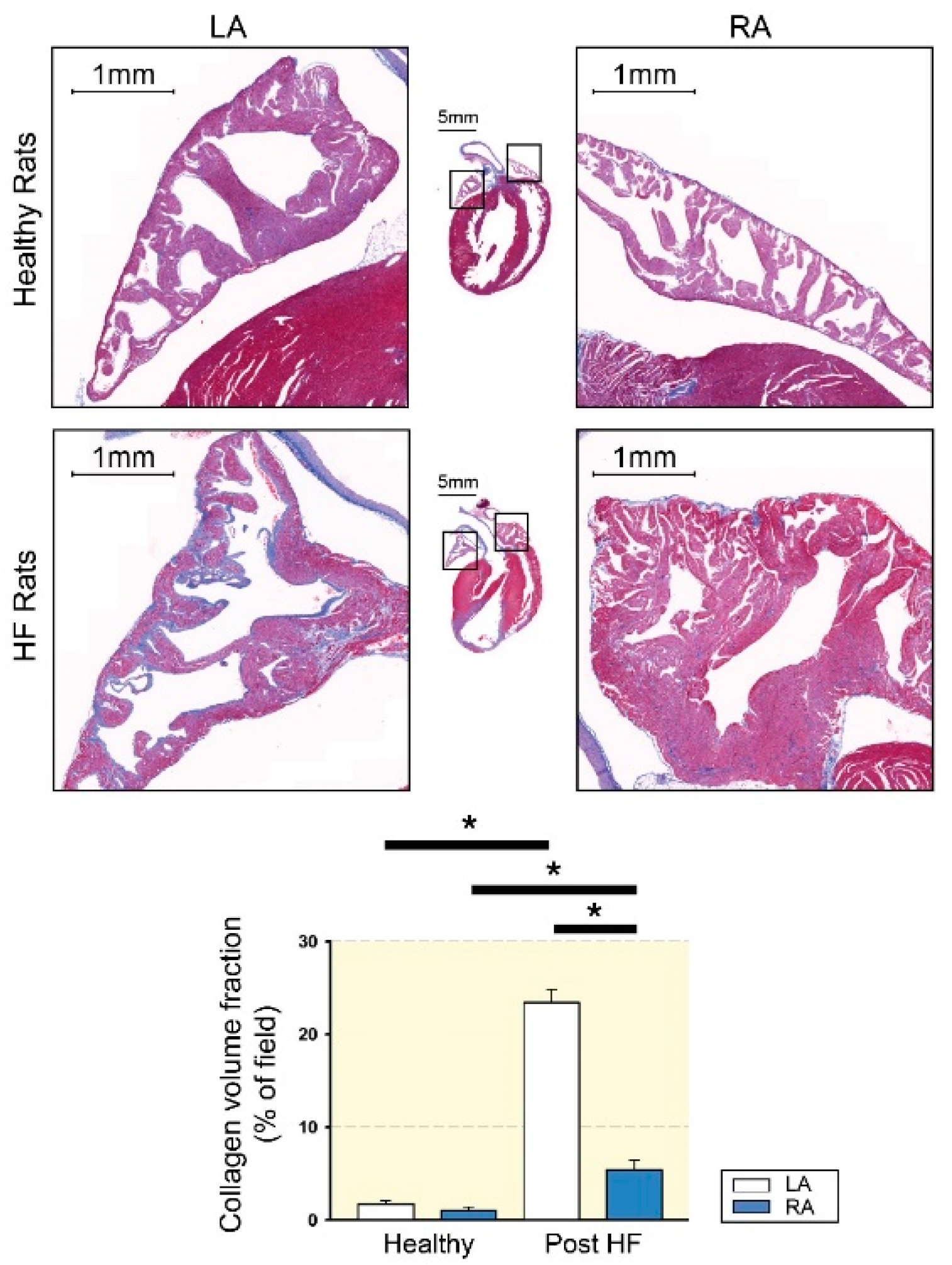
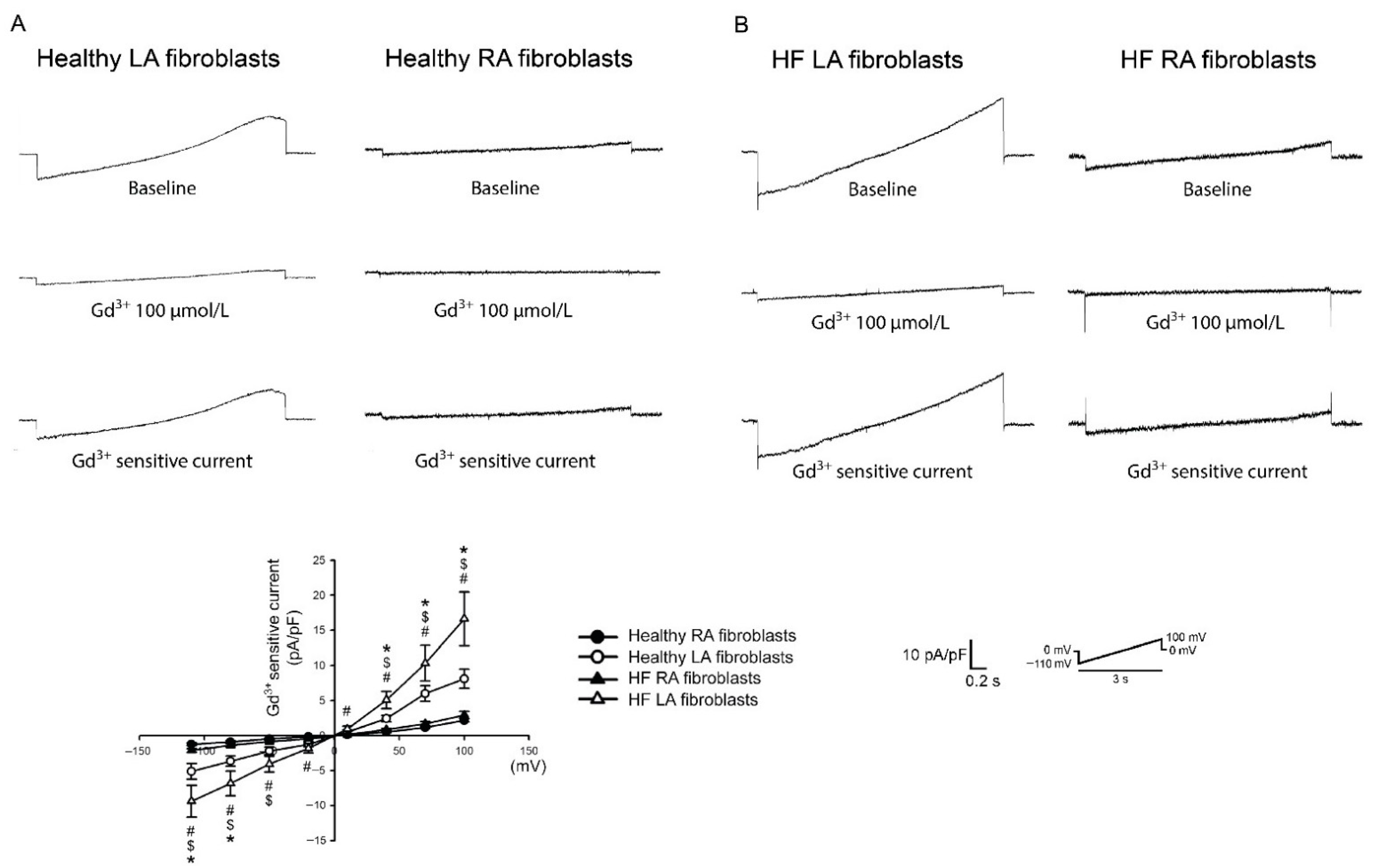
Laboratory Evidence of Diversity in Atrial Fibrogenesis and Arrhythmogenesis
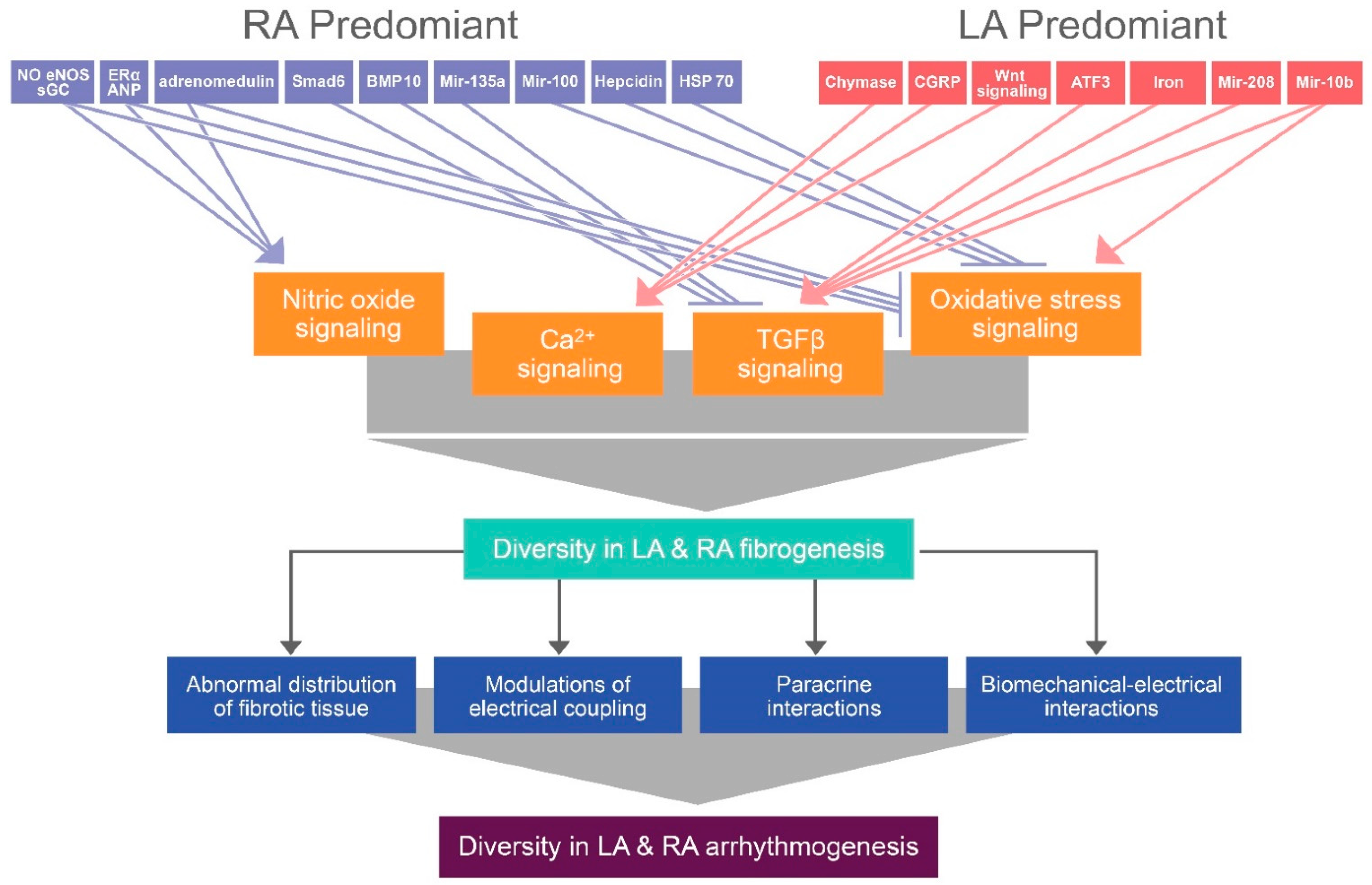
3. Mechanisms Contributing to the Regional Diversities of Atrial Fibrogenesis
3.1. NO and Ca2+ Signaling Modulation
3.2. TGF-β Paracrine Effect
3.3. Oxidative Stress Signaling
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Kainuma, S.; Masai, T.; Yoshitatsu, M.; Miyagawa, S.; Yamauchi, T.; Takeda, K.; Morii, E.; Sawa, Y. Advanced left-atrial fibrosis is associated with unsuccessful maze operation for valvular atrial fibrillation. Eur. J. Cardiothorac. Surg. 2011, 40, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Oakes, R.S.; Badger, T.J.; Kholmovski, E.G.; Akoum, N.; Burgon, N.S.; Fish, E.N.; Blauer, J.J.E.; Rao, S.N.; DiBella, E.V.R.; Segerson, N.M.; et al. Detection and quantification of left atrial structural remodeling with delayed-enhancement magnetic resonance imaging in patients with atrial fibrillation. Circulation 2009, 119, 1758–1767. [Google Scholar] [CrossRef] [Green Version]
- Ohtani, K.; Yutani, C.; Nagata, S.; Koretsune, Y.; Hori, M.; Kamada, T. High prevalence of atrial fibrosis in patients with dilated cardiomyopathy. J. Am. Coll. Cardiol. 1995, 25, 1162–1169. [Google Scholar] [CrossRef] [Green Version]
- Swedberg, K.; Zannad, F.; McMurray, J.J.V.; Krum, H.; van Veldhuisen, D.J.; Shi, H.; Vincent, J.; Pitt, B. Eplerenone and atrial fibrillation in mild systolic heart failure: Results from the EMPHASIS-HF (Eplerenone in Mild Patients Hospitalization and SurvIval Study in Heart Failure) study. J. Am. Coll. Cardiol. 2012, 59, 1598–1603. [Google Scholar] [CrossRef] [Green Version]
- Xu, J.; Cui, G.; Esmailian, F.; Plunkett, M.; Marelli, D.; Ardehali, A.; Odim, J.; Laks, H.; Sen, L. Atrial extracellular matrix remodeling and the maintenance of atrial fibrillation. Circulation 2004, 109, 363–368. [Google Scholar] [CrossRef] [Green Version]
- Park, J.H.; Lee, J.S.; Ko, Y.G.; Lee, S.H.; Lee, B.S.; Kang, S.M.; Chang, B.C.; Pak, H.N. Histological and biochemical comparisons between right atrium and left atrium in patients with mitral valvular atrial fibrillation. Korean Circ. J. 2014, 44, 233–242. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Swartz, M.F.; Fink, G.W.; Lutz, C.J.; Taffet, S.M.; Berenfeld, O.; Vikstrom, K.L.; Kasprowicz, K.; Bhatta, L.; Puskas, F.; Kalifa, J.; et al. Left versus right atrial difference in dominant frequency, K(+) channel transcripts, and fibrosis in patients developing atrial fibrillation after cardiac surgery. Heart Rhythm 2009, 6, 1415–1422. [Google Scholar] [CrossRef] [Green Version]
- Swartz, M.F.; Fink, G.W.; Sarwar, M.F.; Hicks, G.L.; Yu, Y.; Hu, R.; Lutz, C.J.; Taffet, S.M.; Jalife, J. Elevated pre-operative serum peptides for collagen I and III synthesis result in post-surgical atrial fibrillation. J. Am. Coll. Cardiol. 2012, 60, 1799–1806. [Google Scholar] [CrossRef] [Green Version]
- Smorodinova, N.; Lantová, L.; Bláha, M.; Melenovský, V.; Hanzelka, J.; Pirk, J.; Kautzner, J.; Kučera, T. Bioptic Study of Left and right atrial interstitium in cardiac patients with and without atrial fibrillation: Interatrial but not rhythm-based differences. PLoS ONE 2015, 10, e0129124. [Google Scholar]
- Marrouche, N.F.; Wilber, D.; Hindricks, G.; Jais, P.; Akoum, N.; Marchlinski, F.; Kholmovski, E.; Burgon, N.; Hu, N.; Mont, L.; et al. Association of atrial tissue fibrosis identified by delayed enhancement MRI and atrial fibrillation catheter ablation: The DECAAF study. JAMA 2014, 311, 498–506. [Google Scholar] [CrossRef] [PubMed]
- Akoum, N.; McGann, C.; Vergara, G.; Badger, T.; Ranjan, R.; Mahnkopf, C.; Kholmovski, E.; Macleod, R.; Marrouche, N. Atrial fibrosis quantified using late gadolinium enhancement MRI is associated with sinus node dysfunction requiring pacemaker implant. J. Cardiovasc. Electrophysiol. 2012, 23, 44–50. [Google Scholar] [CrossRef] [Green Version]
- Skanes, A.C.; Mandapati, R.; Berenfeld, O.; Davidenko, J.M.; Jalife, J. Spatiotemporal periodicity during atrial fibrillation in the isolated sheep heart. Circulation 1998, 98, 1236–1248. [Google Scholar] [CrossRef]
- Berenfeld, O.; Mandapati, R.; Dixit, S.; Skanes, A.C.; Chen, J.; Mansour, M.; Jalife, J. Spatially distributed dominant excitation frequencies reveal hidden organization in atrial fibrillation in the Langendorff-perfused sheep heart. J. Cardiovasc. Electrophysiol. 2000, 11, 869–879. [Google Scholar] [CrossRef]
- Tai, C.T.; Lo, L.W.; Lin, Y.J.; Chen, S.A. Arrhythmogenic difference between the left and right atria in a canine ventricular pacing-induced heart failure model of atrial fibrillation. Pacing Clin. Electrophysiol. 2012, 35, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Rohr, S. Arrhythmogenic Implications of Fibroblast-Myocyte Interactions. Circ. Arrhythm. Electrophysiol. 2012, 5, 442–452. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pellman, J.; Zhang, J.; Sheikh, F. Myocyte-fibroblast communication in cardiac fibrosis and arrhythmias: Mechanisms and model systems. J. Mol. Cell Cardiol. 2016, 94, 22–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chapeau, C.; Gutkowska, J.; Schiller, P.W.; Milne, R.W.; Thibault, G.; Garcia, R.; Genest, J.; Cantin, M. Localization of immunoreactive synthetic atrial natriuretic factor (ANF) in the heart of various animal species. J. Histochem. Cytochem. 1985, 33, 541–550. [Google Scholar] [CrossRef] [Green Version]
- Kahr, P.C.; Piccini, I.; Fabritz, L.; Greber, B.; Schöler, H.; Scheld, H.H.; Hoffmeier, A.; Brown, N.A.; Kirchhof, P. Systematic analysis of gene expression differences between left and right atria in different mouse strains and in human atrial tissue. PLoS ONE 2011, 6, e26389. [Google Scholar] [CrossRef]
- Tabibiazar, R.; Wagner, R.A.; Liao, A.; Quertermous, T. Transcriptional profiling of the heart reveals chamber-specific gene expression patterns. Circ. Res. 2003, 93, 1193–1201. [Google Scholar] [CrossRef]
- Hsu, J.; Hanna, P.; Van Wagoner, D.R.; Barnard, J.; Serre, D.; Chung, M.K.; Smith, J.D. Whole genome expression differences in human left and right atria ascertained by RNA sequencing. Circ. Cardiovasc. Genet. 2012, 5, 327–335. [Google Scholar] [CrossRef] [Green Version]
- Spach, M.S.; Miller, W.T., 3rd; Dolber, P.C.; Kootsey, J.M.; Sommer, J.R.; Mosher, C.E., Jr. The functional role of structural complexities in the propagation of depolarization in the atrium of the dog. Cardiac conduction disturbances due to discontinuities of effective axial resistivity. Circ. Res. 1982, 50, 175–191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ashihara, T.; Haraguchi, R.; Nakazawa, K.; Namba, T.; Ikeda, T.; Nakazawa, Y.; Ozawa, T.; Ito, M.; Horie, M.; Trayanova, N.A. The role of fibroblasts in complex fractionated electrograms during persistent/permanent atrial fibrillation: Implications for electrogram-based catheter ablation. Circ. Res. 2012, 110, 275–284. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palacio, L.C.; Ugarte, J.P.; Saiz, J.; Tobón, C. The effects of fibrotic cell type and its density on atrial fibrillation dynamics: An in silico study. Cells 2021, 10, 2769. [Google Scholar] [CrossRef]
- Tanaka, K.; Zlochiver, S.; Vikstrom, K.L.; Yamazaki, M.; Moreno, J.; Klos, M.; Zaitsev, A.V.; Vaidyanathan, R.; Auerbach, D.S.; Landas, S.; et al. Spatial distribution of fibrosis governs fibrillation wave dynamics in the posterior left atrium during heart failure. Circ. Res. 2007, 101, 839–847. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Callegari, S.; Macchi, E.; Monaco, R.; Magnani, L.; Tafuni, A.; Croci, S.; Nicastro, M.; Garrapa, V.; Banchini, A.; Becchi, G.; et al. Clinicopathological bird’s-eye view of left atrial myocardial fibrosis in 121 patients with persistent atrial fibrillation: Developing architecture and main cellular players. Circ. Arrhythm. Electrophysiol. 2020, 13, e007588. [Google Scholar] [CrossRef]
- Hsieh, M.H.; Lin, Y.J.; Wang, H.H.; Lo, L.W.; Chang, S.L.; Yan, Y.L.; Chou, T.Y.; Chen, S.A.; Yeh, H.I. Functional characterization of atrial electrograms in a pacing-induced heart failure model of atrial fibrillation: Importance of regional atrial connexin40 remodeling. J. Cardiovasc. Electrophysiol. 2013, 24, 573–582. [Google Scholar] [CrossRef]
- Poulet, C.; Künzel, S.; Büttner, E.; Lindner, D.; Westermann, D.; Ravens, U. Altered physiological functions and ion currents in atrial fibroblasts from patients with chronic atrial fibrillation. Physiol. Rep. 2016, 4, e12681. [Google Scholar] [CrossRef] [Green Version]
- Maleckar, M.M.; Greenstein, J.L.; Giles, W.R.; Trayanova, N.A. Electrotonic coupling between human atrial myocytes and fibroblasts alters myocyte excitability and repolarization. Biophys. J. 2009, 97, 2179–2190. [Google Scholar] [CrossRef] [Green Version]
- Kamkin, A.; Kiseleva, I.; Wagner, K.D.; Lammerich, A.; Bohm, J.; Persson, P.B.; Günther, J. Mechanically induced potentials in fibroblasts from human right atrium. Exp. Physiol. 1999, 84, 347–356. [Google Scholar] [CrossRef]
- Zhan, H.; Xia, L. Excitation-contraction coupling between human atrial myocytes with fibroblasts and stretch activated channel current: A simulation study. Comput Math. Methods Med. 2013, 2013, 238676. [Google Scholar] [CrossRef] [Green Version]
- Yoon, Y.E.; Kim, H.J.; Kim, S.A.; Kim, S.H.; Park, J.H.; Park, K.H.; Choi, S.; Kim, M.K.; Kim, H.S.; Cho, G.Y. Left atrial mechanical function and stiffness in patients with paroxysmal atrial fibrillation. J. Cardiovasc. Ultrasound 2012, 20, 140–145. [Google Scholar] [CrossRef] [Green Version]
- Musa, H.; Kaur, K.; O’Connell, R.; Klos, M.; Guerrero-Serna, G.; Avula, U.M.R.; Herron, T.J.; Kalifa, J.; Anumonwo, J.M.B.; Jalife, J. Inhibition of platelet-derived growth factor-AB signaling prevents electromechanical remodeling of adult atrial myocytes that contact myofibroblasts. Heart Rhythm 2013, 10, 1044–1051. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramos-Mondragón, R.; Vega, A.V.; Avila, G. Long-term modulation of Na+ and K+ channels by TGF-β1 in neonatal rat cardiac myocytes. Pflugers Arch 2011, 461, 235–247. [Google Scholar] [CrossRef] [PubMed]
- Verheule, S.; Sato, T.; Everett, T.t.; Engle, S.K.; Otten, D.; Rubart-von der Lohe, M.; Nakajima, H.O.; Nakajima, H.; Field, L.J.; Olgin, J.E. Increased vulnerability to atrial fibrillation in transgenic mice with selective atrial fibrosis caused by overexpression of TGF-beta1. Circ. Res. 2004, 94, 1458–1465. [Google Scholar] [CrossRef] [Green Version]
- Choi, E.K.; Chang, P.C.; Lee, Y.S.; Lin, S.F.; Zhu, W.; Maruyama, M.; Fishbein, M.C.; Chen, Z.; Rubart-von der Lohe, M.; Field, L.J.; et al. Triggered firing and atrial fibrillation in transgenic mice with selective atrial fibrosis induced by overexpression of TGF-β1. Circ. J. 2012, 76, 1354–1362. [Google Scholar] [CrossRef] [Green Version]
- Chung, C.C.; Kao, Y.H.; Yao, C.J.; Lin, Y.K.; Chen, Y.J. A comparison of left and right atrial fibroblasts reveals different collagen production activity and stress-induced mitogen-activated protein kinase signalling in rats. Acta Physiol. 2017, 220, 432–445. [Google Scholar] [CrossRef] [PubMed]
- Tao, H.; Shi, K.H.; Yang, J.J.; Huang, C.; Liu, L.P.; Li, J. Epigenetic regulation of cardiac fibrosis. Cell Signal. 2013, 25, 1932–1938. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhatia, H.; Verma, G.; Datta, M. miR-107 orchestrates ER stress induction and lipid accumulation by post-transcriptional regulation of fatty acid synthase in hepatocytes. Biochim. Biophys. Acta 2014, 1839, 334–343. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, W.J.; Lin, F.M.; Huang, H.D.; Wang, H. Investigating microRNA-target interaction-supported tissues in human cancer tissues based on miRNA and target gene expression profiling. PLoS ONE 2014, 9, e95697. [Google Scholar] [CrossRef] [Green Version]
- Li, S.; Gao, Y.; Liu, Y.; Li, J.; Yang, X.; Hu, R.; Liu, J.; Zhang, Y.; Zuo, K.; Li, K.; et al. Myofibroblast-derived exosomes contribute to development of a susceptible substrate for atrial fibrillation. Cardiology 2020, 145, 324–332. [Google Scholar] [CrossRef]
- Zhou, Y.; Xu, W.; Han, R.; Zhou, J.; Pan, Z.; Rong, H.; Li, J.; Xu, C.; Qiao, G.; Lu, Y. Matrine inhibits pacing induced atrial fibrillation by modulating I(KM3) and I(Ca-L). Int. J. Biol Sci. 2012, 8, 150–158. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karam, B.S.; Chavez-Moreno, A.; Koh, W.; Akar, J.G.; Akar, F.G. Oxidative stress and inflammation as central mediators of atrial fibrillation in obesity and diabetes. Cardiovasc. Diabetol. 2017, 16, 120. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Zhao, J.; Qiu, J.; Li, J.; Liang, X.; Zhang, Z.; Zhang, X.; Fu, H.; Korantzopoulos, P.; Letsas, K.P.; et al. Xanthine oxidase inhibitor allopurinol prevents oxidative stress-mediated atrial remodeling in alloxan-induced diabetes mellitus rabbits. J. Am. Heart Assoc. 2018, 7, e008807. [Google Scholar] [CrossRef] [PubMed]
- Cai, B.; Pan, Z.; Liu, Y.; Chen, N.; Lu, Y. Arrhythmogenic potential of oxidative stress in atrial myocytes. Int. J. Cardiol. 2011, 150, 219–221. [Google Scholar] [CrossRef]
- Tsai, C.T.; Tseng, C.D.; Hwang, J.J.; Wu, C.K.; Yu, C.C.; Wang, Y.C.; Chen, W.P.; Lai, L.P.; Chiang, F.T.; Lin, J.L. Tachycardia of atrial myocytes induces collagen expression in atrial fibroblasts through transforming growth factor β1. Cardiovasc. Res. 2011, 89, 805–815. [Google Scholar] [CrossRef] [Green Version]
- Moreira, L.M.; Takawale, A.; Hulsurkar, M.; Menassa, D.A.; Antanaviciute, A.; Lahiri, S.K.; Mehta, N.; Evans, N.; Psarros, C.; Robinson, P.; et al. Paracrine signalling by cardiac calcitonin controls atrial fibrogenesis and arrhythmia. Nature 2020, 587, 460–465. [Google Scholar] [CrossRef]
- Zheng, Y.; Xia, Y.; Carlson, J.; Kongstad, O.; Yuan, S. Atrial average conduction velocity in patients with and without paroxysmal atrial fibrillation. Clin. Physiol. Funct Imaging 2017, 37, 596–601. [Google Scholar] [CrossRef]
- Nitta, T.; Ishii, Y.; Miyagi, Y.; Ohmori, H.; Sakamoto, S.; Tanaka, S. Concurrent multiple left atrial focal activations with fibrillatory conduction and right atrial focal or reentrant activation as the mechanism in atrial fibrillation. J. Thorac Cardiovasc. Surg. 2004, 127, 770–778. [Google Scholar] [CrossRef] [Green Version]
- Sanders, P.; Berenfeld, O.; Hocini, M.; Jaïs, P.; Vaidyanathan, R.; Hsu, L.F.; Garrigue, S.; Takahashi, Y.; Rotter, M.; Sacher, F.; et al. Spectral analysis identifies sites of high-frequency activity maintaining atrial fibrillation in humans. Circulation 2005, 112, 789–797. [Google Scholar] [CrossRef] [Green Version]
- Berenfeld, O. Quantifying activation frequency in atrial fibrillation to establish underlying mechanisms and ablation guidance. Heart Rhythm 2007, 4, 1225–1234. [Google Scholar] [CrossRef]
- Sarmast, F.; Kolli, A.; Zaitsev, A.; Parisian, K.; Dhamoon, A.S.; Guha, P.K.; Warren, M.; Anumonwo, J.M.; Taffet, S.M.; Berenfeld, O.; et al. Cholinergic atrial fibrillation: I(K,ACh) gradients determine unequal left/right atrial frequencies and rotor dynamics. Cardiovasc. Res. 2003, 59, 863–873. [Google Scholar] [CrossRef] [Green Version]
- Jeyaratnam, J.; Umapathy, K.; Masse, S.; Nair, K.; Farid, T.; Krishnan, S.; Nanthakumar, K. Relating spatial heterogeneities to rotor formation in studying human ventricular fibrillation. In Proceedings of the 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Societ, Boston, MA, USA, 30 August–3 September 2011; Volume 2011, pp. 231–234. [Google Scholar]
- Nakamura, T.; Kiuchi, K.; Fukuzawa, K.; Takami, M.; Watanabe, Y.; Izawa, Y.; Suehiro, H.; Akita, T.; Takemoto, M.; Sakai, J.; et al. Late-gadolinium enhancement properties associated with atrial fibrillation rotors in patients with persistent atrial fibrillation. J. Cardiovasc. Electrophysiol. 2021, 32, 1005–1013. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.; Rillig, A.; Bucur, T.; Metzner, A.; Mathew, S.; Wissner, E.; Wohlmuth, P.; Kuck, K.H.; Ouyang, F.; Tilz, R.R. Focal impulse and rotor modulation using the novel 64-electrode basket catheter: Electrogram characteristics of human rotors. Europace 2015, 17, 1791–1797. [Google Scholar] [CrossRef] [Green Version]
- Morillo, C.A.; Klein, G.J.; Jones, D.L.; Guiraudon, C.M. Chronic rapid atrial pacing. Structural, functional, and electrophysiological characteristics of a new model of sustained atrial fibrillation. Circulation 1995, 91, 1588–1595. [Google Scholar] [CrossRef] [PubMed]
- Mansour, M.; Mandapati, R.; Berenfeld, O.; Chen, J.; Samie, F.H.; Jalife, J. Left-to-right gradient of atrial frequencies during acute atrial fibrillation in the isolated sheep heart. Circulation 2001, 103, 2631–2636. [Google Scholar] [CrossRef] [Green Version]
- Li, B.; Luo, F.; Luo, X.; Li, B.; Qi, L.; Zhang, D.; Tang, Y. Effects of atrial fibrosis induced by mitral regurgitation on atrial electrophysiology and susceptibility to atrial fibrillation in pigs. Cardiovasc. Pathol. 2019, 40, 32–40. [Google Scholar] [CrossRef]
- Ali, S.R.; Ranjbarvaziri, S.; Talkhabi, M.; Zhao, P.; Subat, A.; Hojjat, A.; Kamran, P.; Müller, A.M.S.; Volz, K.S.; Tang, Z.; et al. Developmental heterogeneity of cardiac fibroblasts does not predict pathological proliferation and activation. Circ. Res. 2014, 115, 625–635. [Google Scholar] [CrossRef] [Green Version]
- Chung, C.C.; Lin, Y.K.; Chen, Y.C.; Kao, Y.H.; Yeh, Y.H.; Chen, Y.J. Calcium regulation on the atrial regional difference of collagen production activity in atrial fibrogenesis. Biomedicines 2021, 9, 686. [Google Scholar] [CrossRef] [PubMed]
- Chung, C.C.; Lin, Y.K.; Chen, Y.C.; Kao, Y.H.; Yeh, Y.H.; Chen, Y.J. Factor Xa inhibition by rivaroxaban regulates fibrogenesis in human atrial fibroblasts with modulation of nitric oxide synthesis and calcium homeostasis. J. Mol. Cell Cardiol. 2018, 123, 128–138. [Google Scholar] [CrossRef]
- Brahmajothi, M.V.; Campbell, D.L. Heterogeneous expression of NO-activated soluble guanylyl cyclase in mammalian heart: Implications for NO- and redox-mediated indirect versus direct regulation of cardiac ion channel function. Channels 2007, 1, 353–365. [Google Scholar] [CrossRef] [Green Version]
- Hao, S.L.; Yu, Z.H.; Qi, B.S.; Luo, J.Z.; Wang, W.P. The antifibrosis effect of adrenomedullin in human lung fibroblasts. Exp. Lung Res. 2011, 37, 615–626. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.; Nishiyama, A.; Guo, P.; Nagai, Y.; Zhang, G.X.; Fujisawa, Y.; Fan, Y.Y.; Kimura, S.; Hosomi, N.; Omori, K.; et al. Effects of adrenomedullin on cardiac oxidative stress and collagen accumulation in aldosterone-dependent malignant hypertensive rats. J. Pharmacol. Exp. Ther. 2006, 318, 1323–1329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jankowski, M.; Rachelska, G.; Donghao, W.; McCann, S.M.; Gutkowska, J. Estrogen receptors activate atrial natriuretic peptide in the rat heart. Proc. Natl. Acad. Sci. USA 2001, 98, 11765–11770. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fukuma, N.; Takimoto, E.; Ueda, K.; Liu, P.; Tajima, M.; Otsu, Y.; Kariya, T.; Harada, M.; Toko, H.; Koga, K.; et al. Estrogen receptor-α non-nuclear signaling confers cardioprotection and is essential to cGMP-PDE5 inhibition efficacy. JACC Basic Transl. Sci. 2020, 5, 282–295. [Google Scholar] [CrossRef]
- Hohmann, N.; Xia, N.; Steinkamp-Fenske, K.; Förstermann, U.; Li, H. Estrogen receptor signaling and the PI3K/Akt pathway are involved in betulinic acid-induced eNOS activation. Molecules 2016, 21, 973. [Google Scholar] [CrossRef] [Green Version]
- Thor, D.; Zhang, R.; Anderson, L.; Bose, D.D.; Dubé, G.P.; Rahimian, R. Effects of 17 β-estradiol on lipopolysacharride-induced intracellular adhesion molecule-1 mRNA expression and Ca²+ homeostasis alteration in human endothelial cells. Vascul Pharmacol. 2010, 53, 230–238. [Google Scholar] [CrossRef] [Green Version]
- Sribnick, E.A.; Del Re, A.M.; Ray, S.K.; Woodward, J.J.; Banik, N.L. Estrogen attenuates glutamate-induced cell death by inhibiting Ca2+ influx through L-type voltage-gated Ca2+ channels. Brain Res. 2009, 1276, 159–170. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guivarc’h, E.; Favre, J.; Guihot, A.L.; Vessières, E.; Grimaud, L.; Proux, C.; Rivron, J.; Barbelivien, A.; Fassot, C.; Briet, M.; et al. Nuclear activation function 2 estrogen receptor α attenuates arterial and renal alterations due to aging and hypertension in female mice. J. Am. Heart Assoc. 2020, 9, e013895. [Google Scholar] [CrossRef] [PubMed]
- Gutkowska, J.; Thibault, G.; Januszewicz, P.; Cantin, M.; Genest, J. Direct radioimmunoassay of atrial natriuretic factor. Biochem. Biophys. Res. Commun. 1984, 122, 593–601. [Google Scholar] [CrossRef]
- Tsunoda, K.; Hodsman, G.P.; Sumithran, E.; Johnston, C.I. Atrial natriuretic peptide in chronic heart failure in the rat: A correlation with ventricular dysfunction. Circ. Res. 1986, 59, 256–261. [Google Scholar] [CrossRef] [Green Version]
- Wilcox, J.N.; Augustine, A.; Goeddel, D.V.; Lowe, D.G. Differential regional expression of three natriuretic peptide receptor genes within primate tissues. Mol. Cell Biol. 1991, 11, 3454–3462. [Google Scholar]
- Onuoha, G.N.; Alpar, E.K.; Nicholls, D.P.; Buchanan, K.D. Calcitonin gene-related peptide, neuropeptide Y and atrial natriuretic peptide distribution in guinea pig heart from paraffin wax-embedded and formalin-cryoprotected tissues. Histochem. J. 1999, 31, 617–621. [Google Scholar] [CrossRef]
- Osman, A.H.; Yuge, S.; Hyodo, S.; Sato, S.; Maeda, S.; Marie, H.; Caceci, T.; Birukawa, N.; Urano, A.; Naruse, K.; et al. Molecular identification and immunohistochemical localization of atrial natriuretic peptide in the heart of the dromedary camel (Camelus dromedarius). Comp. Biochem. Physiol. A Mol. Integr. Physiol. 2004, 139, 417–424. [Google Scholar] [CrossRef]
- Chen, W.; Oberwinkler, H.; Werner, F.; Gaßner, B.; Nakagawa, H.; Feil, R.; Hofmann, F.; Schlossmann, J.; Dietrich, A.; Gudermann, T.; et al. Atrial natriuretic peptide-mediated inhibition of microcirculatory endothelial Ca2+ and permeability response to histamine involves cGMP-dependent protein kinase I and TRPC6 channels. Arterioscler. Thromb. Vasc. Biol. 2013, 33, 2121–2129. [Google Scholar] [CrossRef]
- Jung, S.M.; Lee, J.H.; Park, J.; Oh, Y.S.; Lee, S.K.; Park, J.S.; Lee, Y.S.; Kim, J.H.; Lee, J.Y.; Bae, Y.S.; et al. Smad6 inhibits non-canonical TGF-β1 signalling by recruiting the deubiquitinase A20 to TRAF6. Nat. Commun. 2013, 4, 2562. [Google Scholar] [CrossRef]
- Lin, H.; Dolmatova, E.V.; Morley, M.P.; Lunetta, K.L.; McManus, D.D.; Magnani, J.W.; Margulies, K.B.; Hakonarson, H.; del Monte, F.; Benjamin, E.J.; et al. Gene expression and genetic variation in human atria. Heart Rhythm 2014, 11, 266–271. [Google Scholar] [CrossRef] [Green Version]
- Morrell, N.W.; Bloch, D.B.; ten Dijke, P.; Goumans, M.J.T.H.; Hata, A.; Smith, J.; Yu, P.B.; Bloch, K.D. Targeting BMP signalling in cardiovascular disease and anaemia. Nat. Rev. Cardiol. 2016, 13, 106–120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, Y.K.; Lai, M.S.; Chen, Y.C.; Cheng, C.C.; Huang, J.H.; Chen, S.A.; Chen, Y.J.; Lin, C.I. Hypoxia and reoxygenation modulate the arrhythmogenic activity of the pulmonary vein and atrium. Clin. Sci. 2012, 122, 121–132. [Google Scholar] [CrossRef] [Green Version]
- Hsiao, C.C.; Lee, C.H.; Yang, R.C.; Chen, J.Y.; Su, T.C.; Chang, Y.J.; Lin, C.Y.; Tsai, Y.G. Heat shock protein-70 levels are associated with a state of oxidative damage in the development of bronchopulmonary dysplasia. Front. Pediatr. 2021, 9, 616452. [Google Scholar] [CrossRef] [PubMed]
- Bayraktar, A.; Erbaş, D.; Akarca Dizakar, S.; Göktaş, T.; Ömeroğlu, S.; Öz Oyar, E. The effect of hepcidin on cardiac ischemia-reperfusion injury. J. Investig. Surg. 2020, 33, 813–821. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Liu, Y.; Pan, Y.; Lu, C.; Xu, H.; Wang, X.; Liu, T.; Feng, K.; Tang, Y. MicroRNA-135a inhibits cardiac fibrosis induced by isoproterenol via TRPM7 channel. Biomed. Pharmacother. 2018, 104, 252–260. [Google Scholar] [CrossRef] [PubMed]
- Cooley, N.; Cowley, M.J.; Lin, R.C.; Marasco, S.; Wong, C.; Kaye, D.M.; Dart, A.M.; Woodcock, E.A. Influence of atrial fibrillation on microRNA expression profiles in left and right atria from patients with valvular heart disease. Physiol. Genomics. 2012, 44, 211–219. [Google Scholar] [CrossRef]
- Li, X.; Wang, Y.; Cai, Z.; Zhou, Q.; Li, L.; Fu, P. Exosomes from human umbilical cord mesenchymal stem cells inhibit ROS production and cell apoptosis in human articular chondrocytes via the miR-100-5p/NOX4 axis. Cell Biol. Int. 2021, 45, 2096–2106. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Varagic, J.; Nagata, S.; Kon, N.D.; Ahmad, S.; VonCannon, J.L.; Wright, K.N.; Sun, X.; Deal, D.; Groban, L.; et al. Differential expression of the angiotensin-(1-12)/chymase axis in human atrial tissue. J. Surg. Res. 2020, 253, 173–184. [Google Scholar] [CrossRef]
- Chang, Y.; Stover, S.R.; Hoover, D.B. Regional localization and abundance of calcitonin gene-related peptide receptors in guinea pig heart. J. Mol. Cell Cardiol. 2001, 33, 745–754. [Google Scholar] [CrossRef]
- Thomas, A.M.; Cabrera, C.P.; Finlay, M.; Lall, K.; Nobles, M.; Schilling, R.J.; Wood, K.; Mein, C.A.; Barnes, M.R.; Munroe, P.B.; et al. Differentially expressed genes for atrial fibrillation identified by RNA sequencing from paired human left and right atrial appendages. Physiol. Genomics 2019, 51, 323–332. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Chandrasekaran, G.; Li, W.; Kim, D.Y.; Jeong, I.Y.; Lee, S.H.; Liang, T.; Bae, J.Y.; Choi, I.; Kang, H.; et al. Wnt-PLC-IP3-Connexin-Ca2+ axis maintains ependymal motile cilia in zebrafish spinal cord. Nat. Commun. 2020, 11, 1860. [Google Scholar] [CrossRef] [PubMed]
- Hasin, T.; Elhanani, O.; Abassi, Z.; Hai, T.; Aronheim, A. Angiotensin II signaling up-regulates the immediate early transcription factor ATF3 in the left but not the right atrium. Basic Res. Cardiol. 2011, 106, 175–187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saito, K.; Ishizaka, N.; Aizawa, T.; Sata, M.; Iso-o, N.; Noiri, E.; Mori, I.; Ohno, M.; Nagai, R. Iron chelation and a free radical scavenger suppress angiotensin II-induced upregulation of TGF-beta1 in the heart. Am. J. Physiol Heart Circ. Physiol. 2005, 288, H1836–H1843. [Google Scholar] [CrossRef]
- Yan, T.; Wang, X.; Wei, G.; Li, H.; Hao, L.; Liu, Y.; Yu, X.; Zhu, W.; Liu, P.; Zhu, Y.; et al. Exosomal miR-10b-5p mediates cell communication of gastric cancer cells and fibroblasts and facilitates cell proliferation. J. Cancer 2021, 12, 2140–2150. [Google Scholar] [CrossRef]
- Fang, C.Y.; Yu, C.C.; Liao, Y.W.; Hsieh, P.L.; Ohiro, Y.; Chu, P.M.; Huang, Y.C.; Yu, C.H.; Tsai, L.L. miR-10b regulated by Twist maintains myofibroblasts activities in oral submucous fibrosis. J. Formos Med. Assoc. 2020, 119, 1167–1173. [Google Scholar] [CrossRef]
- Ruan, Z.; Li, Y.; He, R.; Li, X. Inhibition of microRNA-10b-5p up-regulates HOXD10 to attenuate Alzheimer’s disease in rats via the Rho/ROCK signalling pathway. J. Drug Target. 2021, 29, 531–540. [Google Scholar] [CrossRef]
- Novak, J.; Sana, J.; Stracina, T.; Novakova, M.; Slaby, O. Doxorubicin and liposomal doxorubicin differentially affect expression of miR-208a and let-7g in rat ventricles and atria. Cardiovasc. Toxicol. 2017, 17, 355–359. [Google Scholar] [CrossRef]
- Shyu, K.G.; Wang, B.W.; Wu, G.J.; Lin, C.M.; Chang, H. Mechanical stretch via transforming growth factor-β1 activates microRNA208a to regulate endoglin expression in cultured rat cardiac myoblasts. Eur. J. Heart Fail. 2013, 15, 36–45. [Google Scholar] [CrossRef] [Green Version]
- Kazakov, A.; Hall, R.; Jagoda, P.; Bachelier, K.; Müller-Best, P.; Semenov, A.; Lammert, F.; Böhm, M.; Laufs, U. Inhibition of endothelial nitric oxide synthase induces and enhances myocardial fibrosis. Cardiovasc. Res. 2013, 100, 211. [Google Scholar] [CrossRef] [Green Version]
- Wang, D.; Yu, X.; Brecher, P. Nitric oxide and N-acetylcysteine inhibit the activation of mitogen-activated protein kinases by angiotensin II in rat cardiac fibroblasts. J. Biol. Chem. 1998, 273, 33027–33034. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mookerjee, I.; Hewitson, T.D.; Halls, M.L.; Summers, R.J.; Mathai, M.L.; Bathgate, R.A.D.; Tregear, G.W.; Samuel, C.S. Relaxin inhibits renal myofibroblast differentiation via RXFP1, the nitric oxide pathway, and Smad2. FASEB J. 2009, 23, 1219–1229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Y.Q.; Jiang, Y.F.; Hong, L.; Yang, H.J.; Zhang, J.Y.; Zhou, Y.F. Role of Endothelial nitric oxide synthase polymorphisms in atrial fibrillation: A PRISMA-compliant meta-analysis. Med. Sci. Monit. 2019, 25, 2687–2694. [Google Scholar] [CrossRef]
- Hamid, S.A.; Totzeck, M.; Drexhage, C.; Thompson, I.; Fowkes, R.C.; Rassaf, T.; Baxter, G.F. Nitric oxide/cGMP signalling mediates the cardioprotective action of adrenomedullin in reperfused myocardium. Basic Res. Cardiol. 2010, 105, 257–266. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Jiang, J.; Yue, Z.; Liu, S.; Ma, Y.; Yu, N.; Gao, Y.; Sun, S.; Chen, S.; Liu, P. Store-operated Ca2+ entry (SOCE) contributes to angiotensin II-induced cardiac fibrosis in cardiac fibroblasts. J. Pharmacol. Sci. 2016, 132, 171–180. [Google Scholar] [CrossRef] [Green Version]
- Yang, S.; Huang, X.Y. Ca2+ influx through L-type Ca2+ channels controls the trailing tail contraction in growth factor-induced fibroblast cell migration. J. Biol. Chem. 2005, 280, 27130–27137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ikeda, K.; Nakajima, T.; Yamamoto, Y.; Takano, N.; Tanaka, T.; Kikuchi, H.; Oguri, G.; Morita, T.; Nakamura, F.; Komuro, I. Roles of transient receptor potential canonical (TRPC) channels and reverse-mode Na+/Ca2+ exchanger on cell proliferation in human cardiac fibroblasts: Effects of transforming growth factor β1. Cell Calcium. 2013, 54, 213–225. [Google Scholar] [CrossRef]
- Murata, N.; Ito, S.; Furuya, K.; Takahara, N.; Naruse, K.; Aso, H.; Kondo, M.; Sokabe, M.; Hasegawa, Y. Ca2+ influx and ATP release mediated by mechanical stretch in human lung fibroblasts. Biochem. Biophys. Res. Commun. 2014, 453, 101–105. [Google Scholar] [CrossRef] [PubMed]
- Lang, Y.D.; Chang, S.F.; Wang, L.F.; Chen, C.M. Chymase mediates paraquat-induced collagen production in human lung fibroblasts. Toxicol. Lett. 2010, 193, 19–25. [Google Scholar] [CrossRef]
- Saito, K.; Muto, T.; Tomimori, Y.; Maruoka, H.; Tanaka, T.; Fukuda, Y. Human chymase stimulates Ca2+ signaling in human polymorphonuclear cells. Immunol. Lett. 2003, 89, 161–165. [Google Scholar] [CrossRef]
- Al-Rubaiee, M.; Gangula, P.R.; Millis, R.M.; Walker, R.K.; Umoh, N.A.; Cousins, V.M.; Jeffress, M.A.; Haddad, G.E. Inotropic and lusitropic effects of calcitonin gene-related peptide in the heart. Am. J. Physiol Heart Circ. Physiol. 2013, 304, H1525–H1537. [Google Scholar] [CrossRef] [Green Version]
- Grohé, C.; Kahlert, S.; Löbbert, K.; Stimpel, M.; Karas, R.H.; Vetter, H.; Neyses, L. Cardiac myocytes and fibroblasts contain functional estrogen receptors. FEBS Lett. 1997, 416, 107–112. [Google Scholar] [CrossRef]
- Watanabe, T.; Akishita, M.; He, H.; Miyahara, Y.; Nagano, K.; Nakaoka, T.; Yamashita, N.; Kozaki, K.; Ouchi, Y. 17 beta-estradiol inhibits cardiac fibroblast growth through both subtypes of estrogen receptor. Biochem. Biophys. Res. Commun. 2003, 311, 454–459. [Google Scholar] [CrossRef]
- Dworatzek, E.; Mahmoodzadeh, S.; Schriever, C.; Kusumoto, K.; Kramer, L.; Santos, G.; Fliegner, D.; Leung, Y.-K.; Ho, S.M.; Zimmermann, W.H.; et al. Sex-specific regulation of collagen I and III expression by 17β-Estradiol in cardiac fibroblasts: Role of estrogen receptors. Cardiovasc. Res. 2019, 115, 315–327. [Google Scholar] [CrossRef]
- Kucich, U.; Rosenbloom, J.C.; Shen, G.; Abrams, W.R.; Hamilton, A.D.; Sebti, S.M.; Rosenbloom, J. TGF-beta1 stimulation of fibronectin transcription in cultured human lung fibroblasts requires active geranylgeranyl transferase I, phosphatidylcholine-specific phospholipase C, protein kinase C-delta, and p38, but not erk1/erk2. Arch. Biochem. Biophys. 2000, 374, 313–324. [Google Scholar] [CrossRef]
- Mukherjee, S.; Duan, F.; Kolb, M.R.; Janssen, L.J. Platelet derived growth factor-evoked Ca2+ wave and matrix gene expression through phospholipase C in human pulmonary fibroblast. Int. J. Biochem. Cell Biol. 2013, 45, 1516–1524. [Google Scholar] [CrossRef]
- Berridge, M.J.; Bootman, M.D.; Lipp, P. Calcium--a life and death signal. Nature 1998, 395, 645–648. [Google Scholar] [CrossRef] [PubMed]
- Wedel, B.; Boyles, R.R.; Putney, J.W., Jr.; Bird, G.S. Role of the store-operated calcium entry proteins Stim1 and Orai1 in muscarinic cholinergic receptor-stimulated calcium oscillations in human embryonic kidney cells. J. Physiol. 2007, 579, 679–689. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, T.; Obukhov, A.G.; Schaefer, M.; Harteneck, C.; Gudermann, T.; Schultz, G. Direct activation of human TRPC6 and TRPC3 channels by diacylglycerol. Nature 1999, 397, 259–263. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.-J.; Ma, N.; Su, F.; Liu, H.; Mei, J. Increased TRPM6 expression in atrial fibrillation patients contribute to atrial fibrosis. Exp. Mol. Pathol. 2015, 98, 486–490. [Google Scholar] [CrossRef]
- Harada, M.; Luo, X.; Qi, X.Y.; Tadevosyan, A.; Maguy, A.; Ordog, B.; Ledoux, J.; Kato, T.; Naud, P.; Voigt, N.; et al. Transient receptor potential canonical-3 channel-dependent fibroblast regulation in atrial fibrillation. Circulation 2012, 126, 2051–2064. [Google Scholar] [CrossRef] [PubMed]
- Essen, L.O.; Perisic, O.; Katan, M.; Wu, Y.; Roberts, M.F.; Williams, R.L. Structural mapping of the catalytic mechanism for a mammalian phosphoinositide-specific phospholipase C. Biochemistry 1997, 36, 1704–1718. [Google Scholar] [CrossRef]
- Moccia, F.; Dragoni, S.; Lodola, F.; Bonetti, E.; Bottino, C.; Guerra, G.; Laforenza, U.; Rosti, V.; Tanzi, F. Store-dependent Ca(2+) entry in endothelial progenitor cells as a perspective tool to enhance cell-based therapy and adverse tumour vascularization. Curr. Med. Chem. 2012, 19, 5802–5818. [Google Scholar] [CrossRef]
- Stathopulos, P.B.; Zheng, L.; Li, G.Y.; Plevin, M.J.; Ikura, M. Structural and mechanistic insights into STIM1-mediated initiation of store-operated calcium entry. Cell 2008, 135, 110–122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Mello, W.C. Atrial natriuretic factor reduces cell coupling in the failing heart, an effect mediated by cyclic GMP. J. Cardiovasc. Pharmacol. 1998, 32, 75–79. [Google Scholar] [CrossRef]
- Ma, L.; Wang, H.Y. Suppression of cyclic GMP-dependent protein kinase is essential to the Wnt/cGMP/Ca2+ pathway. J. Biol Chem. 2006, 281, 30990–31001. [Google Scholar] [CrossRef] [Green Version]
- Everett, T.H.T.; Olgin, J.E. Atrial fibrosis and the mechanisms of atrial fibrillation. Heart Rhythm 2007, 4, S24–S27. [Google Scholar] [CrossRef] [Green Version]
- Lin, X.; Wu, N.; Shi, Y.; Wang, S.; Tan, K.; Shen, Y.; Dai, H.; Zhong, J. Association between transforming growth factor β1 and atrial fibrillation in essential hypertensive patients. Clin. Exp. Hypertens 2015, 37, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Huang, Z.Y.; Wang, Z.H.; Li, C.P.; Meng, X.L.; Zhang, Y.J.; Su, F.; Ma, N. TGF-β1 and TIMP-4 regulate atrial fibrosis in atrial fibrillation secondary to rheumatic heart disease. Mol. Cell Biochem. 2015, 406, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Du, L.; Qin, M.; Yi, Y.; Chen, X.; Jiang, W.; Zhou, L.; Zhang, D.; Xu, K.; Yang, Y.; Li, C.; et al. Eplerenone prevents atrial fibrosis via the TGF-β signaling pathway. Cardiology 2017, 138, 55–62. [Google Scholar] [CrossRef]
- Seet, L.F.; Toh, L.Z.; Finger, S.N.; Chu, S.W.; Stefanovic, B.; Wong, T.T. Valproic acid suppresses collagen by selective regulation of Smads in conjunctival fibrosis. J. Mol. Med. 2016, 94, 321–334. [Google Scholar] [CrossRef] [Green Version]
- Qu, X.; Liu, Y.; Cao, D.; Chen, J.; Liu, Z.; Ji, H.; Chen, Y.; Zhang, W.; Zhu, P.; Xiao, D.; et al. BMP10 preserves cardiac function through its dual activation of SMAD-mediated and STAT3-mediated pathways. J. Biol. Chem. 2019, 294, 19877–19888. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.M.; Liu, X.M.; Wang, Y.; Chen, Z.Y. Activating transcription factor 3 (ATF3) regulates cell growth, apoptosis, invasion and collagen synthesis in keloid fibroblast through transforming growth factor beta (TGF-beta)/SMAD signaling pathway. Bioengineered 2021, 12, 117–126. [Google Scholar] [CrossRef]
- Zacharski, L.R.; McKernan, L.; Metzger, M.E.; Malone, M.G.; Samnotra, V.; Bhargava, A.; Steiner, P.R.; Rauwerdink, C.A.; Ornstein, D.L.; Cornell, C.J. Remission of paroxysmal atrial fibrillation with iron reduction in haemophilia A. Haemophilia 2010, 16, 726–730. [Google Scholar] [CrossRef]
- Saad, A.K.; Aladio, J.M.; Yamasato, F.; Volberg, V.I.; Gonzalez Ballerga, E.; Sordá, J.A.; Daruich, J.; Perez de la Hoz, R.A. Analysis of the left atrial function using two-dimensional strain in patients with recent diagnosis of hereditary hemochromatosis. Curr. Probl. Cardiol. 2021, 100903. [Google Scholar] [CrossRef]
- Correia, E.T.O.; Barbetta, L.; Silva, O.; Mesquita, E.T. Left atrial stiffness: A predictor of atrial fibrillation recurrence after radiofrequency catheter ablation—A systematic review and meta-aAnalysis. Arq Bras Cardiol. 2019, 112, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Wang, D.; Lucas, J.; Oparil, S.; Xing, D.; Cao, X.; Novak, L.; Renfrow, M.B.; Chen, Y.F. Atrial natriuretic peptide inhibits transforming growth factor beta-induced Smad signaling and myofibroblast transformation in mouse cardiac fibroblasts. Circ. Res. 2008, 102, 185–192. [Google Scholar] [CrossRef] [Green Version]
- Fang, L.; Ellims, A.H.; Moore, X.L.; White, D.A.; Taylor, A.J.; Chin-Dusting, J.; Dart, A.M. Circulating microRNAs as biomarkers for diffuse myocardial fibrosis in patients with hypertrophic cardiomyopathy. J. Transl. Med. 2015, 13, 314. [Google Scholar] [CrossRef] [PubMed]
- Satoh, M.; Minami, Y.; Takahashi, Y.; Tabuchi, T.; Nakamura, M. Expression of microRNA-208 is associated with adverse clinical outcomes in human dilated cardiomyopathy. J. Card Fail. 2010, 16, 404–410. [Google Scholar] [CrossRef]
- Samman Tahhan, A.; Sandesara, P.B.; Hayek, S.S.; Alkhoder, A.; Chivukula, K.; Hammadah, M.; Mohamed-Kelli, H.; O’Neal, W.T.; Topel, M.; Ghasemzadeh, N.; et al. Association between oxidative stress and atrial fibrillation. Heart Rhythm 2017, 14, 1849–1855. [Google Scholar] [CrossRef] [PubMed]
- Yeh, Y.H.; Kuo, C.T.; Chang, G.J.; Qi, X.Y.; Nattel, S.; Chen, W.J. Nicotinamide adenine dinucleotide phosphate oxidase 4 mediates the differential responsiveness of atrial versus ventricular fibroblasts to transforming growth factor-β. Circ. Arrhythmia Electrophysiol. 2013, 6, 790–798. [Google Scholar] [CrossRef] [Green Version]
- Li, P.F.; Dietz, R.; von Harsdorf, R. Superoxide induces apoptosis in cardiomyocytes, but proliferation and expression of transforming growth factor-β1 in cardiac fibroblasts. FEBS Lett. 1999, 448, 206–210. [Google Scholar] [CrossRef] [Green Version]
- Anupama, V.; George, M.; Dhanesh, S.B.; Chandran, A.; James, J.; Shivakumar, K. Molecular mechanisms in H2O2-induced increase in AT1 receptor gene expression in cardiac fibroblasts: A role for endogenously generated Angiotensin II. J. Mol. Cell Cardiol. 2016, 97, 295–305. [Google Scholar] [CrossRef]
- Zhou, L.; Liu, Y.; Wang, Z.; Liu, D.; Xie, B.; Zhang, Y.; Yuan, M.; Tse, G.; Li, G.; Xu, G.; et al. Activation of NADPH oxidase mediates mitochondrial oxidative stress and atrial remodeling in diabetic rabbits. Life Sci. 2021, 272, 119240. [Google Scholar] [CrossRef]
- Ganz, T. Hepcidin, a key regulator of iron metabolism and mediator of anemia of inflammation. Blood 2003, 102, 783–788. [Google Scholar] [CrossRef] [Green Version]
| Predominant Chamber | Molecules | Signaling That Induces Atrial Diversities | Effects of Molecules on the Signaling | References |
|---|---|---|---|---|
| RA | Nitric oxide | Nitric oxide signaling | + | [6,61] |
| eNOS | Nitric oxide signaling | + | [61] | |
| sGC | Nitric oxide signaling | + | [61] | |
| Adrenomedullin | Nitric oxide signaling | + | [18] | |
| TGF-β signaling | − | [62] | ||
| Oxidative stress signaling | − | [63] | ||
| Estrogen receptor-α | Nitric oxide signaling | + | [64,65,66] | |
| Ca2+ signaling | − | [67,68] | ||
| Oxidative stress signaling | − | [69] | ||
| ANP | Nitric oxide signaling | + | [17,64,70,71,72,73,74] | |
| Ca2+ signaling | − | [75] | ||
| Smad6 | TGF-β signaling | − | [76,77] | |
| BMP-10 | TGF-β signaling | − | [18,20,78] | |
| HSP-70 | Oxidative stress signaling | − | [79,80] | |
| Hepcidin | Oxidative stress signaling | − | [20,81] | |
| Mir-135a | Ca2+ signaling | − | [20,82] | |
| TGF-β signaling | − | [82] | ||
| Mir-100 | Oxidative stress signaling | − | [83,84] | |
| LA | Chymase | Ca2+ signaling | + | [85] |
| CGRP | Ca2+ signaling | + | [86] | |
| Wnt related gene | Ca2+ signaling | + | [87,88] | |
| ATF3 | TGF-β signaling | + | [89] | |
| Iron | TGF-β signaling | + | [7,90] | |
| Mir-10b | TGF-β signaling | + | [20,91,92] | |
| Oxidative stress signaling | + | [93] | ||
| Mir-208 | TGF-β signaling | + | [94,95] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chung, C.-C.; Chin, C.-G.; Lin, Y.-K.; Chen, Y.-C.; Cheng, W.-L.; Yeh, Y.-H.; Kao, Y.-H.; Chen, Y.-J. Regional Diversities in Fibrogenesis Weighed as a Key Determinant for Atrial Arrhythmogenesis. Biomedicines 2021, 9, 1900. https://doi.org/10.3390/biomedicines9121900
Chung C-C, Chin C-G, Lin Y-K, Chen Y-C, Cheng W-L, Yeh Y-H, Kao Y-H, Chen Y-J. Regional Diversities in Fibrogenesis Weighed as a Key Determinant for Atrial Arrhythmogenesis. Biomedicines. 2021; 9(12):1900. https://doi.org/10.3390/biomedicines9121900
Chicago/Turabian StyleChung, Cheng-Chih, Chye-Gen Chin, Yung-Kuo Lin, Yao-Chang Chen, Wan-Li Cheng, Yung-Hsin Yeh, Yu-Hsun Kao, and Yi-Jen Chen. 2021. "Regional Diversities in Fibrogenesis Weighed as a Key Determinant for Atrial Arrhythmogenesis" Biomedicines 9, no. 12: 1900. https://doi.org/10.3390/biomedicines9121900
APA StyleChung, C.-C., Chin, C.-G., Lin, Y.-K., Chen, Y.-C., Cheng, W.-L., Yeh, Y.-H., Kao, Y.-H., & Chen, Y.-J. (2021). Regional Diversities in Fibrogenesis Weighed as a Key Determinant for Atrial Arrhythmogenesis. Biomedicines, 9(12), 1900. https://doi.org/10.3390/biomedicines9121900






