Short-Term Diet Restriction but Not Alternate Day Fasting Prevents Cisplatin-Induced Nephrotoxicity in Mice
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Experimental Design
2.3. Histopathological Analysis
2.4. Biochemical Analysis
2.5. Western Blot
2.6. Statistical Analysis
3. Results
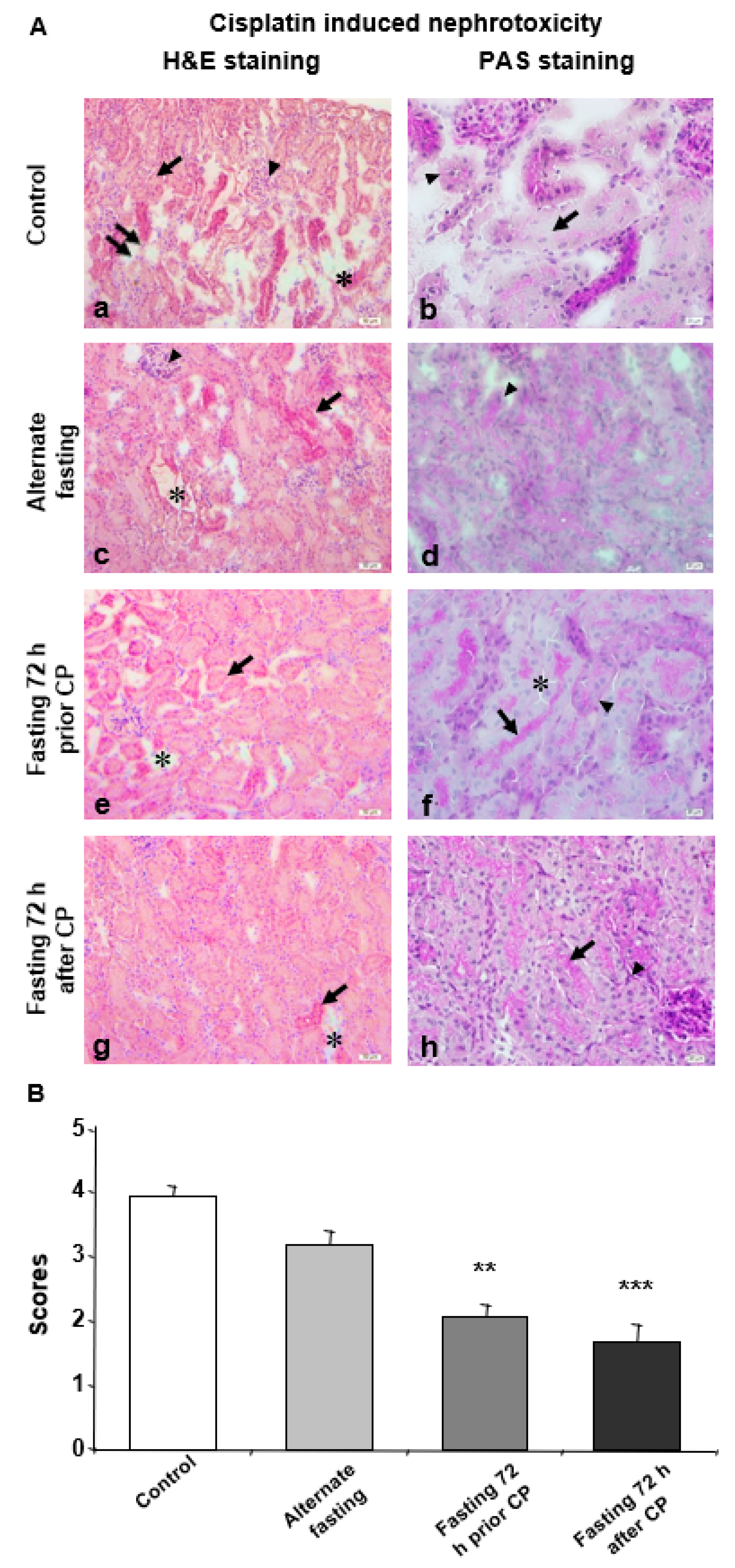
3.1. Prolonged Starvation Resulted in Conserved Morphology in Nephrotic Structures
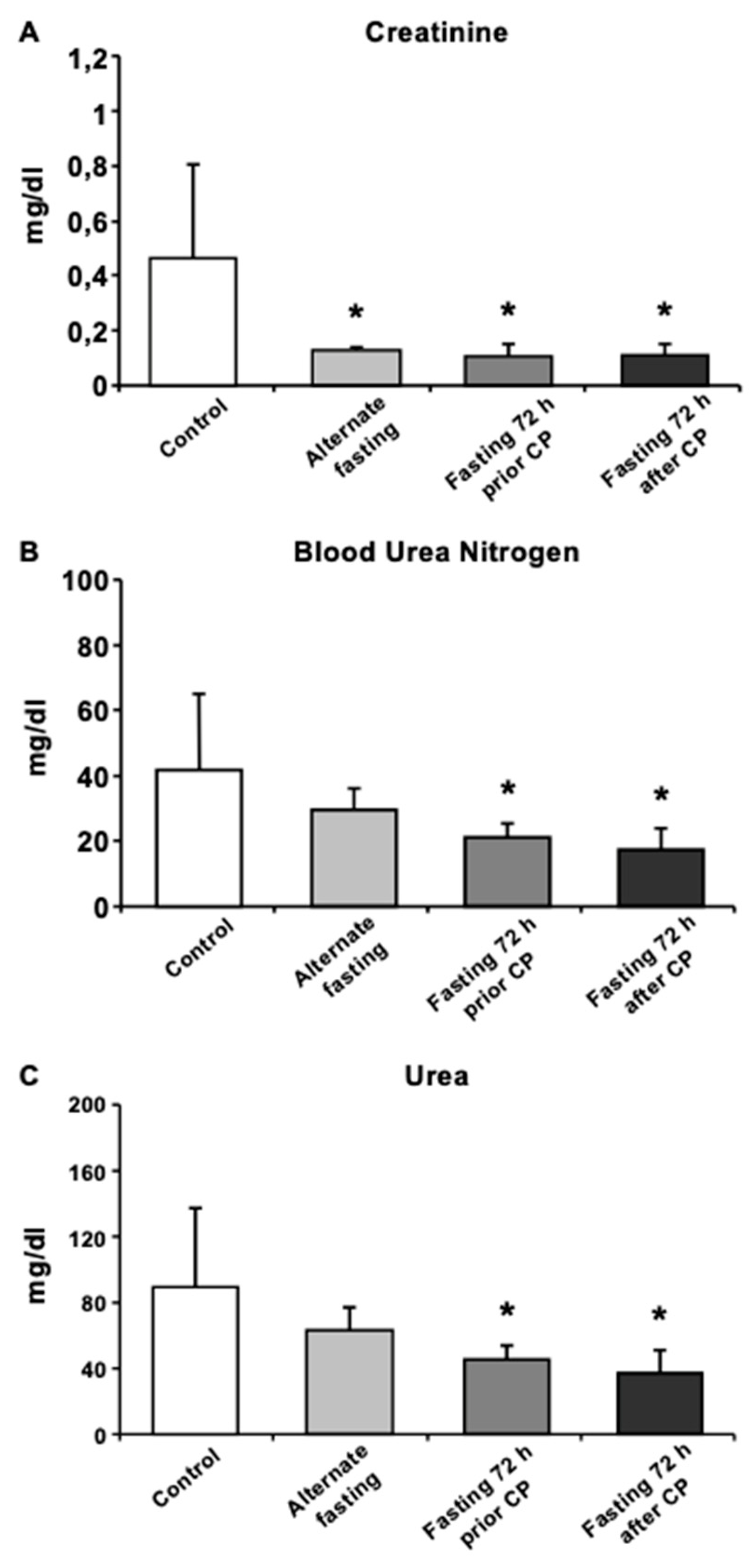
3.2. Biochemical Tests and Analysis of DNA Fragmentation Reveal that 72A Group Is Protected from CP-Induced Oxidative Stress
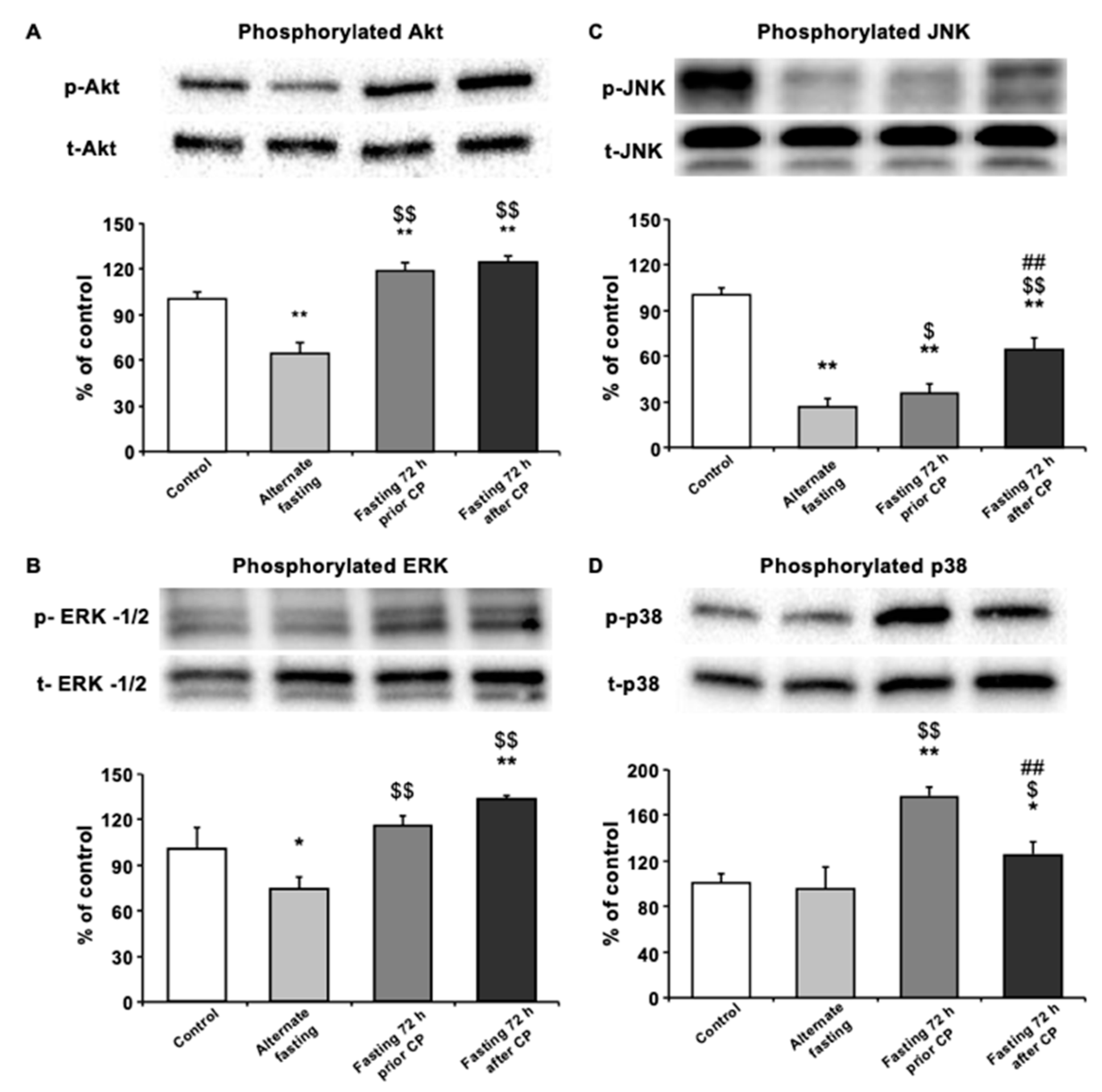
3.3. Seventy-Two Hours of Fasting Improves Cellular Survival via Regulating MAPK Pathway Elements in Kidney
3.4. Dietary Content Is Also a Rate-Limiting Factor in Expansion of AKI Followed by CP Administration
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- von der Maase, H.; Sengelov, L.; Roberts, J.T.; Ricci, S.; Dogliotti, L.; Oliver, T.; Moore, M.J.; Zimmermann, A.; Arning, M. Long-term-survival results of a randomized trial comparing gemcitabine plus cisplatin, with methotrexate, vinblastine, doxorubicin, plus cisplatin in patients with bladder cancer. J. Clin. Oncol. 2005, 23, 4602–4608. [Google Scholar] [CrossRef] [PubMed]
- Silver, D.P.; Richardson, A.L.; Eklund, A.C.; Wang, Z.C.; Szallasi, Z.; Li, Q.; Juul, N.; Leong, C.O.; Calogrias, D.; Buraimoh, A.; et al. Efficacy of neoadjuvant Cisplatin in triple-negative breast cancer. J. Clin. Oncol. 2010, 28, 1145–1153. [Google Scholar] [CrossRef] [PubMed]
- Pignon, J.P.; Tribodet, H.; Scagliotti, G.V.; Douillard, J.Y.; Shepherd, F.A.; Stephens, R.J.; Dunant, A.; Torri, V.; Rosell, R.; Seymour, L.; et al. Lung adjuvant cisplatin evaluation: a pooled analysis by the LACE Collaborative Group. J. Clin. Oncol. 2008, 26, 3552–3559. [Google Scholar] [CrossRef] [PubMed]
- Miller, R.P.; Tadagavadi, R.K.; Ramesh, G.; Reeves, W.B. Mechanisms of Cisplatin nephrotoxicity. Toxins 2010, 2, 2490–2518. [Google Scholar] [CrossRef] [PubMed]
- Oh, G.S.; Kim, H.J.; Shen, A.; Lee, S.B.; Khadka, D.; Pandit, A.; So, H.S. Cisplatin-induced Kidney Dysfunction and Perspectives on Improving Treatment Strategies. Electrolyte Blood Press. 2014, 12, 55–65. [Google Scholar] [CrossRef]
- Mattson, M.P.; Longo, V.D.; Harvie, M. Impact of intermittent fasting on health and disease processes. Ageing Res. Rev. 2017, 39, 46–58. [Google Scholar] [CrossRef]
- Estrela, G.R.; Wasinski, F.; Batista, R.O.; Hiyane, M.I.; Felizardo, R.J.; Cunha, F.; de Almeida, D.C.; Malheiros, D.M.; Camara, N.O.; Barros, C.C.; et al. Caloric Restriction Is More Efficient than Physical Exercise to Protect from Cisplatin Nephrotoxicity via PPAR-Alpha Activation. Front Physiol. 2017, 8, 116. [Google Scholar] [CrossRef]
- Raffaghello, L.; Safdie, F.; Bianchi, G.; Dorff, T.; Fontana, L.; Longo, V.D. Fasting and differential chemotherapy protection in patients. Cell Cycle 2010, 9, 4474–4476. [Google Scholar] [CrossRef]
- Shi, Y.; Felley-Bosco, E.; Marti, T.M.; Orlowski, K.; Pruschy, M.; Stahel, R.A. Starvation-induced activation of ATM/Chk2/p53 signaling sensitizes cancer cells to cisplatin. BMC Cancer 2012, 12, 571. [Google Scholar] [CrossRef]
- van Niekerk, G.; Hattingh, S.M.; Engelbrecht, A.M. Enhanced Therapeutic Efficacy in Cancer Patients by Short-term Fasting: The Autophagy Connection. Front Oncol. 2016, 6, 242. [Google Scholar] [CrossRef]
- Smith, N.J.G.; Caldwell, J.L.; van der Merwe, M.; Sharma, S.; Butawan, M.; Puppa, M.; Bloomer, R.J. A Comparison of Dietary and Caloric Restriction Models on Body Composition, Physical Performance, and Metabolic Health in Young Mice. Nutrients 2019, 11, 350. [Google Scholar] [CrossRef] [PubMed]
- Descamps, O.; Riondel, J.; Ducros, V.; Roussel, A.M. Mitochondrial production of reactive oxygen species and incidence of age-associated lymphoma in OF1 mice: effect of alternate-day fasting. Mech. Ageing Dev. 2005, 126, 1185–1191. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, E.A.; Chai, C.M.; Hellerstein, M.K. Effects of caloric restriction on cell proliferation in several tissues in mice: role of intermittent feeding. Am J. Physiol. Endocrinol. Metab. 2005, 288, E965–E972. [Google Scholar] [CrossRef] [PubMed]
- Rocha, N.S.; Barbisan, L.F.; de Oliveira, M.L.; de Camargo, J.L. Effects of fasting and intermittent fasting on rat hepatocarcinogenesis induced by diethylnitrosamine. Teratog. Carcinog. Mutagen. 2002, 22, 129–138. [Google Scholar] [CrossRef]
- Siegel, I.; Liu, T.L.; Nepomuceno, N.; Gleicher, N. Effects of short-term dietary restriction on survival of mammary ascites tumor-bearing rats. Cancer Invest. 1988, 6, 677–680. [Google Scholar] [CrossRef]
- Wan, R.; Camandola, S.; Mattson, M.P. Intermittent fasting and dietary supplementation with 2-deoxy-D-glucose improve functional and metabolic cardiovascular risk factors in rats. Faseb J. 2003, 17, 1133–1134. [Google Scholar] [CrossRef]
- Yakar, S.; Leroith, D.; Brodt, P. The role of the growth hormone/insulin-like growth factor axis in tumor growth and progression: Lessons from animal models. Cytokine Growth Factor Rev. 2005, 16, 407–420. [Google Scholar] [CrossRef]
- Cheng, C.W.; Adams, G.B.; Perin, L.; Wei, M.; Zhou, X.; Lam, B.S.; Da Sacco, S.; Mirisola, M.; Quinn, D.I.; Dorff, T.B.; et al. Pro-longed fasting reduces IGF-1/PKA to promote hematopoietic stem-cell-based regeneration and reverse immunosuppression. Cell Stem Cell 2014, 14, 810–823. [Google Scholar] [CrossRef]
- Longo, V.D.; Mattson, M.P. Fasting: molecular mechanisms and clinical applications. Cell Metab. 2014, 19, 181–192. [Google Scholar] [CrossRef]
- Jones, M.M.; Basinger, M.A.; Beaty, J.A.; Holscher, M.A. The relative nephrotoxicity of cisplatin, cis-[Pt(NH3)2(guanosine)2] 2+, and the hydrolysis product of cisplatin in the rat. Cancer Chemother. Pharm. 1991, 29, 29–32. [Google Scholar] [CrossRef]
- Saleh, S.; Ain-Shoka, A.A.; El-Demerdash, E.; Khalef, M.M. Protective effects of the angiotensin II receptor blocker losartan on cisplatin-induced kidney injury. Chemotherapy 2009, 55, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Marko, L.; Kassmann, M.; Zhu, Y.; Wu, K.; Gollasch, M. Role of TRPV1 channels in ischemia/reperfusion-induced acute kidney injury. PLoS ONE 2014, 9, e109842. [Google Scholar] [CrossRef] [PubMed]
- Pan, H.; Shen, K.; Wang, X.; Meng, H.; Wang, C.; Jin, B. Protective effect of metalloporphyrins against cisplatin-induced kidney injury in mice. PLoS ONE 2014, 9, e86057. [Google Scholar] [CrossRef] [PubMed]
- Spandou, E.; Tsouchnikas, I.; Karkavelas, G.; Dounousi, E.; Simeonidou, C.; Guiba-Tziampiri, O.; Tsakiris, D. Erythropoietin attenuates renal injury in experimental acute renal failure ischaemic/reperfusion model. Nephrol. Dial. Transpl. 2006, 21, 330–336. [Google Scholar] [CrossRef] [PubMed]
- Kelland, L. The resurgence of platinum-based cancer chemotherapy. Nat. Rev. Cancer 2007, 7, 573–584. [Google Scholar] [CrossRef] [PubMed]
- Karbownik, A.; Szalek, E.; Urjasz, H.; Gleboka, A.; Mierzwa, E.; Grzeskowiak, E. The physical and chemical stability of cisplatin (Teva) in concentrate and diluted in sodium chloride 0.9%. Wspolczesna Onkol. 2012, 16, 435–439. [Google Scholar] [CrossRef]
- Dasari, S.; Tchounwou, P.B. Cisplatin in cancer therapy: Molecular mechanisms of action. Eur. J. Pharm. 2014, 740, 364–378. [Google Scholar] [CrossRef]
- Peres, L.A.; da Cunha, A.D., Jr. Acute nephrotoxicity of cisplatin: molecular mechanisms. J. Bras. Nefrol. 2013, 35, 332–340. [Google Scholar] [CrossRef]
- Raffaghello, L.; Lee, C.; Safdie, F.M.; Wei, M.; Madia, F.; Bianchi, G.; Longo, V.D. Starvation-dependent differential stress resistance protects normal but not cancer cells against high-dose chemotherapy. Proc. Natl. Acad. Sci. USA 2008, 105, 8215–8220. [Google Scholar] [CrossRef]
- Bauersfeld, S.P.; Kessler, C.S.; Wischnewsky, M.; Jaensch, A.; Steckhan, N.; Stange, R.; Kunz, B.; Bruckner, B.; Sehouli, J.; Michalsen, A. The effects of short-term fasting on quality of life and tolerance to chemotherapy in patients with breast and ovarian cancer: a randomized crossover pilot study. BMC Cancer 2018, 18, 476. [Google Scholar] [CrossRef]
- Kilic, U.; Caglayan, A.B.; Beker, M.C.; Gunal, M.Y.; Caglayan, B.; Yalcin, E.; Kelestemur, T.; Gundogdu, R.Z.; Yulug, B.; Yilmaz, B.; et al. Particular phosphorylation of PI3K/Akt on Thr308 via PDK-1 and PTEN mediates melatonin’s neuroprotective activity after focal cerebral ischemia in mice. Redox Biol. 2017, 12, 657–665. [Google Scholar] [CrossRef] [PubMed]
- Kilic, U.; Kilic, E.; Soliz, J.; Bassetti, C.I.; Gassmann, M.; Hermann, D.M. Erythropoietin protects from axotomy-induced degeneration of retinal ganglion cells by activating ERK-1/-2. Faseb J. 2005, 19, 249–251. [Google Scholar] [CrossRef] [PubMed]
- Feliers, D.; Kasinath, B.S. Erk in kidney diseases. J. Signal Transduct. 2011, 2011, 768512. [Google Scholar] [CrossRef] [PubMed]
- di Mari, J.F.; Davis, R.; Safirstein, R.L. MAPK activation determines renal epithelial cell survival during oxidative injury. Am J. Physiol. 1999, 277, F195–F203. [Google Scholar] [CrossRef] [PubMed]
- Saha, S.; Mahalanobish, S.; Dutta, S.; Sil, P.C. Mangiferin ameliorates collateral neuropathy in tBHP induced apoptotic nephropathy by inflammation mediated kidney to brain crosstalk. Food Funct. 2019, 10, 5981–5999. [Google Scholar] [CrossRef] [PubMed]
- Wei, Q.J.; Zhao, J.J.; Zhou, X.G.; Yu, L.L.; Liu, Z.H.; Chang, Y.L. Propofol can suppress renal ischemia-reperfusion injury through the activation of PI3K/AKT/mTOR signal pathway. Gene 2019, 708, 14–20. [Google Scholar] [CrossRef]
- Winograd-Katz, S.E.; Levitzki, A. Cisplatin induces PKB/Akt activation and p38(MAPK) phosphorylation of the EGF receptor. Oncogene 2006, 25, 7381–7390. [Google Scholar] [CrossRef]
- Jo, S.K.; Cho, W.Y.; Sung, S.A.; Kim, H.K.; Won, N.H. MEK inhibitor, U0126, attenuates cisplatin-induced renal injury by decreasing inflammation and apoptosis. Kidney Int. 2005, 67, 458–466. [Google Scholar] [CrossRef]
- Mukherjee, S.; Dash, S.; Lohitesh, K.; Chowdhury, R. The dynamic role of autophagy and MAPK signaling in determining cell fate under cisplatin stress in osteosarcoma cells. PLoS ONE 2017, 12, e0179203. [Google Scholar] [CrossRef]
- Sen, Z.; Jie, M.; Jingzhi, Y.; Dongjie, W.; Dongming, Z.; Xiaoguang, C. Total Coumarins from Hydrangea paniculata Protect against Cisplatin-Induced Acute Kidney Damage in Mice by Suppressing Renal Inflammation and Apoptosis. Evid. Based Complement Altern. Med. 2017, 2017, 5350161. [Google Scholar] [CrossRef]
- Ramesh, G.; Reeves, W.B. p38 MAP kinase inhibition ameliorates cisplatin nephrotoxicity in mice. Am J. Physiol. Ren. Physiol. 2005, 289, F166–F174. [Google Scholar] [CrossRef] [PubMed]
- Mishima, K.; Baba, A.; Matsuo, M.; Itoh, Y.; Oishi, R. Protective effect of cyclic AMP against cisplatin-induced nephrotoxicity. Free Radic. Biol. Med. 2006, 40, 1564–1577. [Google Scholar] [CrossRef] [PubMed]
- Quintanilha, J.C.F.; de Sousa, V.M.; Visacri, M.B.; Amaral, L.S.; Santos, R.M.M.; Zambrano, T.; Salazar, L.A.; Moriel, P. Involvement of cytochrome P450 in cisplatin treatment: implications for toxicity. Cancer Chemother. Pharm. 2017, 80, 223–233. [Google Scholar] [CrossRef] [PubMed]
- Cangemi, A.; Fanale, D.; Rinaldi, G.; Bazan, V.; Galvano, A.; Perez, A.; Barraco, N.; Massihnia, D.; Castiglia, M.; Vieni, S.; et al. Dietary restriction: could it be considered as speed bump on tumor progression road? Tumour. Biol. 2016, 37, 7109–7118. [Google Scholar] [CrossRef] [PubMed]

© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gunebakan, E.; Yalcin, E.; Cikler Dulger, E.; Yigitbasi, A.; Ates, N.; Caglayan, A.; Beker, M.C.; Sahin, K.; Korkaya, H.; Kilic, E. Short-Term Diet Restriction but Not Alternate Day Fasting Prevents Cisplatin-Induced Nephrotoxicity in Mice. Biomedicines 2020, 8, 23. https://doi.org/10.3390/biomedicines8020023
Gunebakan E, Yalcin E, Cikler Dulger E, Yigitbasi A, Ates N, Caglayan A, Beker MC, Sahin K, Korkaya H, Kilic E. Short-Term Diet Restriction but Not Alternate Day Fasting Prevents Cisplatin-Induced Nephrotoxicity in Mice. Biomedicines. 2020; 8(2):23. https://doi.org/10.3390/biomedicines8020023
Chicago/Turabian StyleGunebakan, Evrin, Esra Yalcin, Esra Cikler Dulger, Ahmet Yigitbasi, Nilay Ates, Aysun Caglayan, Mustafa C. Beker, Kazim Sahin, Hasan Korkaya, and Ertugrul Kilic. 2020. "Short-Term Diet Restriction but Not Alternate Day Fasting Prevents Cisplatin-Induced Nephrotoxicity in Mice" Biomedicines 8, no. 2: 23. https://doi.org/10.3390/biomedicines8020023
APA StyleGunebakan, E., Yalcin, E., Cikler Dulger, E., Yigitbasi, A., Ates, N., Caglayan, A., Beker, M. C., Sahin, K., Korkaya, H., & Kilic, E. (2020). Short-Term Diet Restriction but Not Alternate Day Fasting Prevents Cisplatin-Induced Nephrotoxicity in Mice. Biomedicines, 8(2), 23. https://doi.org/10.3390/biomedicines8020023






