The Impact of the COVID-19 Pandemic on Coronary Artery Bypass Grafting Surgery: A Single-Centre Retrospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Data Collection
2.2. Statistical Analysis
3. Results
3.1. Pre-Pandemic vs. Pandemic Group
3.1.1. Number of CABG Procedures and Basic Characteristics
3.1.2. Surgical Data
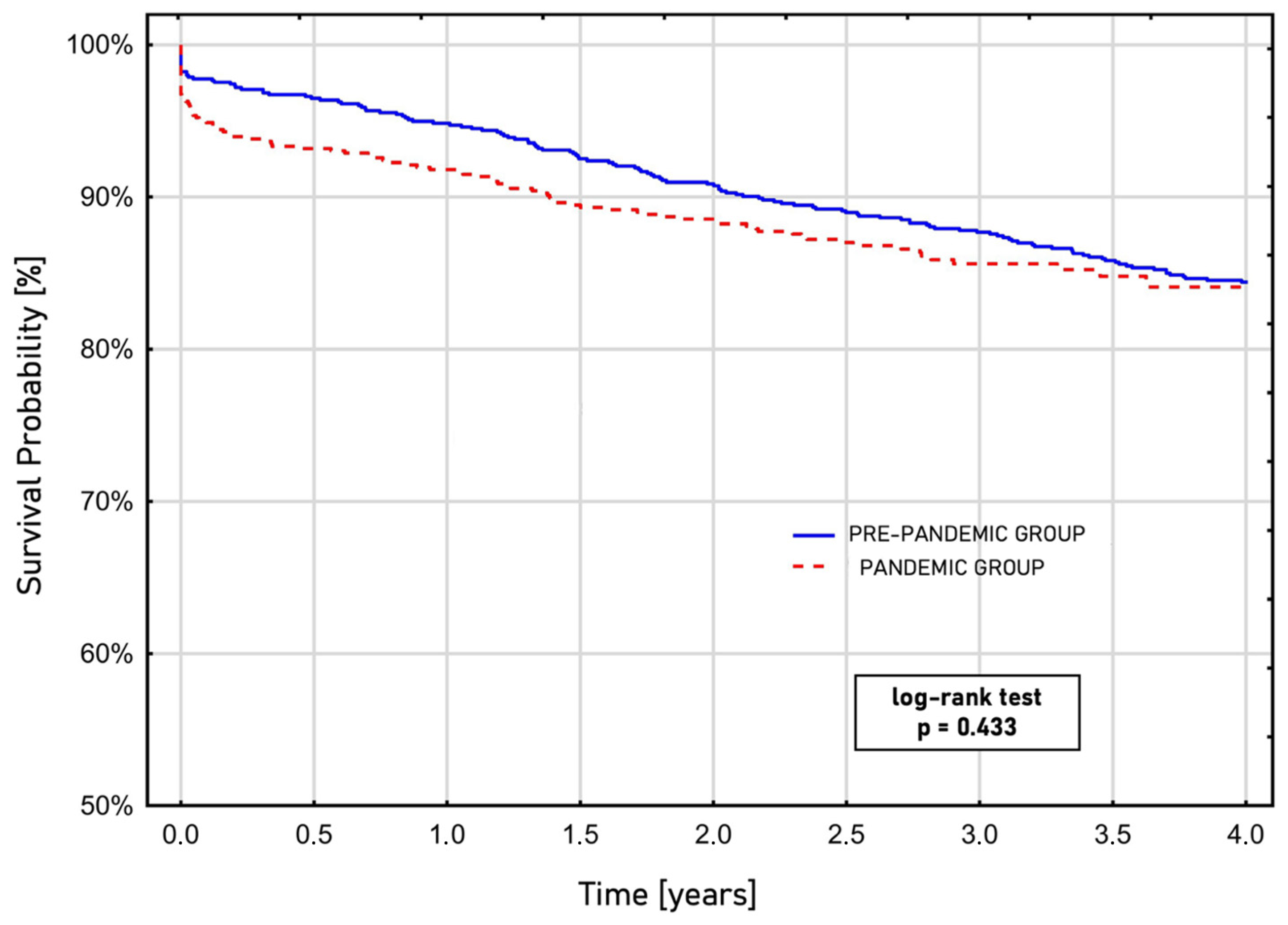
3.1.3. Outcome Data and Survival Analysis
3.2. The Three Waves of the COVID-19 Pandemic
3.2.1. Number of CABG Procedures and Basic Characteristics
3.2.2. Surgical Data
3.2.3. Outcome Data and Survival Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACS | Acute coronary syndrome |
| CABG | Coronary artery bypass grafting |
| CAD | Coronary artery disease |
| COVID-19 | The coronavirus disease 2019 |
| CPB | Cardiopulmonary bypass |
| CSS | Classifications of Canadian Cardiovascular Society |
| DM | Diabetes mellitus |
| EUROSCORE II | The European System for Cardiac Operative Risk Evaluation |
| FREEDOM | Future Revascularisation Evaluation in Patients with Diabetes Mellitus: Optimal Management of Multivessel Disease |
| HA | Artery hypertension |
| ICU | Intensive care unit |
| KROK | The Polish National Registry of Cardiac Surgical Operations database |
| MIDCAB | Minimally invasive coronary artery bypass |
| NYHA | New York Heart Association |
| OPCAB | Off-pump coronary artery bypass |
| PCI | Percutaneous coronary intervention |
| SARS-CoV-2 | Severe acute respiratory syndrome coronavirus 2 |
| SYNTAX | Synergy between PCI with Taxus and Cardiac Surgery |
| TVCAD | Triple vessel coronary artery disease |
References
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [CrossRef]
- Pinkas, J.; Jankowski, M.; Szumowski, Ł.; Lusawa, A.; Zgliczyński, W.S.; Raciborski, F.; Wierzba, W.; Gujski, M. Public Health Interventions to Mitigate Early Spread of SARS-CoV-2 in Poland. Med. Sci. Monit. 2020, 26, e924730-1. [Google Scholar] [CrossRef]
- Bociąga-Jasik, M.; Wojciechowska, W.; Terlecki, M.; Wizner, B.; Rajzer, M.; Garlicki, A.; Sładek, K.; Krzanowska, K.; Wordliczek, J.; Krzanowski, M.; et al. Comparison between COVID-19 Outcomes in the First Three Waves of Pandemic: A Reference Hospital Report. Pol. Arch. Intern. Med. 2022, 132, 16286. [Google Scholar] [CrossRef]
- Robakowski, P.; Synoweć, J. Poland’s health policy—What has changed in the era of COVID-19. Political Stud. 2020, 48, 85–106. (In Polish) [Google Scholar] [CrossRef]
- Kanecki, K.; Nitsch-Osuch, A.; Goryński, P.; Wojtyniak, B.; Juszczyk, G.; Magdalena, B.; Kosińska, I.; Tyszko, P. Hospitalizations for COVID-19 in Poland: A study based on data from a national hospital register. Pol. Arch. Intern. Med. 2021, 131, 535–540. [Google Scholar] [CrossRef]
- El-Andari, R.; Fialka, N.M.; Nagendran, J. The impact of resource allocation during the COVID-19 pandemic on cardiac surgical practice and patient outcomes: A systematic review. Eur. J. Cardiothorac. Surg. 2023, 63, ezad230. [Google Scholar] [CrossRef] [PubMed]
- Aranda-Michel, E.; Serna-Gallegos, D.; Arnaoutakis, G.; Kilic, A.; Brown, J.A.; Dai, Y.; Dunn-Lewis, C.; Sultan, I. The Effect of COVID-19 on Cardiac Surgical Volume and its Associated Costs. Semin. Thorac. Cardiovasc. Surg. 2023, 35, 508–515. [Google Scholar] [CrossRef]
- Bonalumi, G.; Giambuzzi, I.; Buratto, B.; Barili, F.; Garatti, A.; Pilozzi Casado, A.; Di Mauro, M.; Parolari, A. The day after tomorrow: Cardiac surgery and coronavirus disease-2019. J. Cardiovasc. Med. 2022, 23, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Gaudino, M.; Chikwe, J.; Hameed, I.; Robinson, N.B.; Fremes, S.E.; Ruel, M. Response of Cardiac Surgery Units to COVID-19: An Internationally-Based Quantitative Survey. Circulation 2020, 142, 300–302. [Google Scholar] [CrossRef]
- Archer, J.E.; Odeh, A.; Ereidge, S.; Salem, H.K.; Jones, G.P.; Gardner, A.; Tripathi, S.S.; Gregg, A.; Jeganathan, R.; Siddique, M.H.; et al. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: An international cohort study. Lancet 2020, 396, 27–38. [Google Scholar] [CrossRef]
- Kirkley, K.; Benedetto, U.; Caputo, M.; Angelini, G.D.; Vohra, H.A. The Ongoing Impact of COVID-19 on Adult Cardiac Surgery and Suggestions for Safe Continuation throughout the Pandemic: A Review of Expert Opinions. Perfusion 2021, 37, 340–349. [Google Scholar] [CrossRef] [PubMed]
- Patel, V.; Jimenez, E.; Cornwell, L.; Tran, T.; Paniagua, D.; Denktas, A.E.; Chou, A.; Hankins, S.J.; Bozkurt, B.; Rosengart, T.K.; et al. Cardiac Surgery during the Coronavirus Disease 2019 Pandemic: Perioperative Considerations and Triage Recommendations. J. Am. Heart Assoc. 2020, 9, e017042. [Google Scholar] [CrossRef]
- Haft, J.W.; Atluri, P.; Ailawadi, G.; Engelman, D.T.; Grant, M.C.; Hassan, A.; Legare, J.-F.; Whitman, G.J.R.; Arora, R.C. Adult Cardiac Surgery During the COVID-19 Pandemic: A Tiered Patient Triage Guidance Statement. Ann. Thorac. Surg. 2020, 110, 697–700. [Google Scholar] [CrossRef]
- Goel, A.; Malik, A.H.; Bandyopadhyay, D.; Isath, A.; Gupta, R.; Hajra, A.; Shrivastav, R.; Virani, S.S.; Fonarow, G.C.; Lavie, C.J.; et al. Impact of COVID-19 on Outcomes of Patients Hospitalized With STEMI: A Nationwide Propensity-matched Analysis. Curr. Probl. Cardiol. 2023, 48, 101547. [Google Scholar] [CrossRef]
- Gustafson, D.; Ngai, M.; Wu, R.; Hou, H.; Schoffel, A.C.; Erice, C.; Mandla, S.; Billia, F.; Wilson, M.D.; Radisic, M.; et al. Cardiovascular Signatures of COVID-19 Predict Mortality and Identify Barrier Stabilizing Therapies. eBioMedicine 2022, 78, 103982. [Google Scholar] [CrossRef]
- Cierpiszewska, K.; Ciechanowicz, S.; Górecki, M.; Kupidłowski, P.; Puślecki, M.; Perek, B. Changes in treatment of aortic valve diseases for acute and elective indications during the COVID-19 pandemic: A retrospective single-center analysis from 2019 to 2020. Adv. Clin. Exp. Med. 2022, 31, 1043–1048. [Google Scholar] [CrossRef] [PubMed]
- Perek, B.; Olasinska-Wisniewska, A.; Misterski, M.; Puslecki, M.; Grygier, M.; Buczkowski, P.; Lesiak, M.; Stankowski, T.; Szarpak, Ł.; Ruetzler, K.; et al. How the COVID-19 pandemic changed treatment of severe aortic stenosis: A single cardiac center experience. J. Thorac. Dis. 2021, 13, 906–917. [Google Scholar] [CrossRef]
- Ordinance of the Minister of Health of 12 May 2022 Amending the Revocation of the State of Epidemic in the Territory of the Republic of Poland. Available online: https://sip.lex.pl/akty-prawne/dzu-dziennik-ustaw/odwolanie-na-obszarze-rzeczypospolitej-polskiej-stanu-epidemii-19240388 (accessed on 29 June 2025). (In Polish).
- Nashef, S.A.M.; Roques, F.; Sharples, L.D.; Nilsson, J.; Smith, C.; Goldstone, A.R.; Lockowandt, U. EuroSCORE II. Eur. J. Cardiothorac. Surg. 2012, 41, 734–745. [Google Scholar] [CrossRef] [PubMed]
- Khalil, K.H.; Sá, M.P.B.O.; Vervoort, D.; Roever, L.; Pires, M.A.D.A.; Lima, J.M.D.O.; de Salles, F.B.; Khalil, G.M.; Nicz, P.F.G.; Mejía, O.A.V.; et al. Impact of the COVID-19 pandemic on coronary artery bypass graft surgery in Brazil: A nationwide perspective. J. Card. Surg. 2021, 36, 3289–3293. [Google Scholar] [CrossRef]
- Parcha, V.; Kalra, R.; Glenn, A.M.; Davies, J.E.; Kuranz, S.; Arora, G.; Arora, P. Coronary artery bypass graft surgery outcomes in the United States: Impact of the coronavirus disease 2019 (COVID-19) pandemic. JTCVS Open 2021, 6, 132–143. [Google Scholar] [CrossRef]
- Ivert, T.; Dalén, M.; Friberg, Ö. Effect of COVID-19 on cardiac surgery volumes in Sweden. Scand. Cardiovasc. J. 2023, 57, 2166102. [Google Scholar] [CrossRef]
- Mejia, O.A.V.; Borgomoni, G.B.; Silveira, L.M.V.; Guerreiro, G.P.; Falcão Filho, A.T.G.; Goncharov, M.; Dallan, L.R.P.; Oliveira, M.A.P.; de Sousa, A.G.; Nakazone, M.A.; et al. The arrival of COVID-19 in Brazil and the impact on coronary artery bypass surgery. J. Card. Surg. 2021, 36, 3070–3077. [Google Scholar] [CrossRef]
- Nader, J.; Anselmi, A.; Tomasi, J.; Martin, A.; Aymami, M.; Rouze, S.; Corbineau, H.; Langanay, T.; Flecher, E.; Nesseler, N.; et al. Adult cardiac surgery during COVID-19 lockdown: Impact on activity and outcomes in a high-volume centre. Arch. Cardiovasc. Dis. 2021, 114, 364–370. [Google Scholar] [CrossRef] [PubMed]
- Mafham, M.M.; Spata, E.; Goldacre, R.; Gair, D.; Curnow, P.; Bray, M.; Hollings, S.; Roebuck, C.; Gale, C.P.; Mamas, M.A.; et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet 2020, 396, 381–389. [Google Scholar] [CrossRef]
- Bychowski, J.; Michalski, T.; Sobiczewski, W.; Jaguszewski, M.; Gruchała, M. The impact of the COVID-19 pandemic on ST-segment elevation myocardial infarction treatment strategy and outcomes. Front. Cardiovasc. Med. 2025, 12, 1522661. [Google Scholar] [CrossRef]
- Jankowska-Sanetra, J.; Sanetra, K.; Konopko, M.; Kutowicz, M.; Synak, M.; Kaźmierczak, P.; Milewski, K.; Kołtowski, Ł.; Buszman, P.P. Incidence and course of acute coronary syndrome cases after the first wave of the COVID-19 pandemic. Kardiol. Pol. 2023, 81, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Rubino, A.S.; De Santo, L.S.; Pisano, A.; Mauro, M.D.; Benussi, S.; Borghetti, V.; Castiglioni, A.; Chiariello, L.; Colli, A.; De Bellis, A.; et al. Cardiac surgery practice during the COVID-19 outbreak: A multicentre national survey. Eur. J. Cardiothorac. Surg. 2021, 59, 901–907. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.M.I.; Bin Zafar, M.D.; Yasmin, F.; Ghazi, E.M.; Jatoi, H.N.; Jawed, A.; Nadeem, A.; Khan, Z.; Anas, Z.; Siddiqui, S.A. Exploring the impact of the COVID-19 pandemic on cardiac surgical services: A scoping review. J. Card. Surg. 2021, 36, 3354–3363. [Google Scholar] [CrossRef]
- Hassan, A.; Arora, R.C.; Lother, S.A.; Adams, C.; Bouchard, D.; Cook, R.; Gunning, D.; Lamarche, Y.; Malas, T.; Moon, M.; et al. Ramping up the delivery of cardiac surgery during the COVID-19 pandemic: A guidance statement from the Canadian Society of Cardiac Surgeons. Can. J. Cardiol. 2020, 36, 1139–1143. [Google Scholar] [CrossRef]
- Polish Society of Cardiothoracic Surgeons. The Statement of the Polish Society of Cardiothoracic Surgeons Regarding Treatment During the SARS-CoV-2 Pandemic. Available online: https://ptkt.pl/wp-content/uploads/2020/12/Wytyczne-PTKT-COVID-19.pdf (accessed on 29 June 2025). (In Polish).
- Bonalumi, G.; Pilozzi Casado, A.; Barbone, A.; Garatti, A.; Colli, A.; Giambuzzi, I.; Torracca, L.; Ravenni, G.; Folesani, G.; Murara, G.; et al. Prognostic value of SARS-CoV-2 on patients undergoing cardiac surgery. J. Card. Surg. 2022, 37, 165–173. [Google Scholar] [CrossRef]
- Katsiampoura, A.; Perozo, C.; Varkaris, A.; Vellayappan, S.; Tam, M.Z.; Vellayappan, U.; Agnihotri, A.; Tam, S. Covid-19 positivity affects outcome of cardiac surgical patients. J. Card. Surg. 2020, 35, 3650–3652. [Google Scholar] [CrossRef] [PubMed]
- Doenst, T.; Haverich, A.; Serruys, P.; Bonow, R.O.; Kappetein, P.; Falk, V.; Velazquez, E.; Diegeler, A.; Sigusch, H. PCI and CABG for Treating Stable Coronary Artery Disease: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2019, 73, 964–976. [Google Scholar] [CrossRef]
- Neumann, F.-J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.-P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef] [PubMed]
- Serruys, P.W.; Morice, M.-C.; Kappetein, A.P.; Colombo, A.; Holmes, D.R.; Mack, M.J.; Ståhle, E.; Feldman, T.E.; van den Brand, M.; Bass, E.J.; et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N. Engl. J. Med. 2009, 360, 961–972. [Google Scholar] [CrossRef] [PubMed]
- Farkouh, M.E.; Domanski, M.; Sleeper, L.A.; Siami, F.S.; Dangas, G.; Mack, M.; Yang, M.; Cohen, D.J.; Rosenberg, Y.; Solomon, S.D.; et al. Strategies for multivessel revascularization in patients with diabetes. N. Engl. J. Med. 2012, 367, 2375–2384. [Google Scholar] [CrossRef]
- Baigent, C.; Windecker, S.; Andreini, D.; Arbelo, E.; Barbato, E.; Bartorelli, A.L.; Baumbach, A.; Behr, E.R.; Berti, S.; Bueno, H.; et al. ESC guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic: Part 2-care pathways, treatment, and follow-up. Eur. Heart J. 2022, 43, 1059–1103. [Google Scholar] [CrossRef]
- Taxiarchi, P.; Kontopantelis, E.; Kinnaird, T.; Kinnaird, T.; Curzen, N.; Banning, A.; Ludman, P.; Shoaib, A.; Rashid, M.; Martin, G.P.; et al. Adoption of same day discharge following elective left main stem percutaneous coronary intervention. Int. J. Cardiol. 2020, 321, 38–47. [Google Scholar] [CrossRef]
- Kite, T.A.; Ladwiniec, A.; Owens, C.G.; Chase, A.B.; Shaukat, A.; Mozid, A.; O’Kane, P.; Routledge, H.; Perera, D.; Jain, A.; et al. Outcomes following PCI in CABG candidates during the COVID-19 pandemic: The prospective multicentre UK-ReVasc registry. Catheter. Cardiovasc. Interv. 2022, 99, 305–313. [Google Scholar] [CrossRef]
- Wang, X.; Gao, H.; Zhang, Z.; Deng, C.; Yan, Y.; Shi, T. Effect of the COVID-19 pandemic on complications and mortality of patients with cardiac surgery. J. Cardiothorac. Surg. 2021, 16, 361. [Google Scholar] [CrossRef]
| Pre-Pandemic N = 853 | Pandemic N = 646 | p-Value | |
|---|---|---|---|
| Sex, men, N (%) | 626 (73.4) | 499 (77.2) | 0.088 |
| Age, years | 67.3 [61.3; 72.4] | 67.1 [61.7; 72.6] | 0.670 |
| Body mass index, kg/m2 | 28.7 [25.8; 31.5] | 28.4 [25.4; 31.7] | 0.789 |
| Diabetes mellitus, N% | 360 (42.2) | 321 (49.7) | 0.004 |
| Hyperlipidaemia, N (%) | 658 (77.1) | 493 (76.3) | 0.755 |
| Arterial hypertension, N (%) | 726 (85.1) | 586 (90.7) | 0.001 |
| Active nicotine abuse, N (%) | 241 (29.4) | 157 (26.7) | 0.029 |
| Nicotine abuse in past, N (%) | 279 (32.7) | 171 (26.5) | 0.007 |
| Metabolic syndrome, N (%) | 109 (12.8) | 108 (16.7) | 0.032 |
| Chronic kidney disease, N (%) | 110 (12.9) | 96 (14.9) | 0.308 |
| Estimated glomerular filtration rate, mL/min/1.73 m2 | 77.2 [61.4; 91.5] | 75.2 [58.3; 90.3] | 0.134 |
| Pulmonary comorbidities, N (%) | 65 (7.6) | 54 (8.4) | 0.596 |
| Cerebrovascular comorbidities, N (%) | 102 (11.9) | 63 (9.8) | 0.177 |
| CCS I, N (%) | 36 (4.2) | 36 (5.6) | 0.176 |
| CCS II, N (%) | 358 (41.9) | 284 (43.9) | 0.188 |
| CCS III, N (%) | 224 (26.3) | 169 (26.2) | 0.751 |
| CCS IV, N (%) | 188 (22) | 82 (12.7) | 0.0001 |
| NYHA I, N (%) | 142 (16.6) | 186 (28.8) | 0.0001 |
| NYHA II, N (%) | 532 (62.4) | 351 (54.3) | 0.013 |
| NYHA III, N (%) | 163 (19.1) | 98 (15.2) | 0.085 |
| NYHA IV, N (%) | 16 (1.9) | 11 (1.7) | 0.867 |
| Critical preoperative state, N (%) | 209 (24.5) | 114 (17.6) | 0.001 |
| EUROSCORE II, % | 2.2 [1.2; 4.6] | 1.99 [1.2; 4.0] | 0.178 |
| Ejection fraction, % | 50 [43; 55] | 50 [42; 55] | 0.191 |
| Pre-Pandemic N = 853 | Pandemic N = 646 | p-Value | |
|---|---|---|---|
| Elective procedure, N (%) | 401 (47) | 261 (40.4) | 0.012 |
| Urgency procedure to 30 days, N (%) | 106 (12.5) | 67 (10.4) | 0.218 |
| Urgency procedure to 7 days, N (%) | 321 (37.6) | 282 (44) | 0.013 |
| Life-saving procedure, N (%) | 25 (2.9) | 34 (5.2) | 0.022 |
| Use of cardiopulmonary bypass, N (%) | 383 (44.9) | 470 (53.1) | 0.002 |
| Type of procedure, MIDCAB, N (%) | 46 (5.4) | 19 (2.9) | 0.021 |
| Type of procedure, OPCAB, N (%) | 424 (49.7) | 284 (44) | 0.027 |
| Duration of procedure, min | 279.7 [100; 635] | 315 [75; 632] | 0.0001 |
| Duration of cardiopulmonary bypass, min | 82 [67; 97] | 98 [80; 123] | 0.0001 |
| Number of bypass vessels, N (%) | 2 [2; 3] | 2 [2; 3] | 0.303 |
| TVCAD, N (%) | 411 (48.2) | 298 (46.1) | 0.462 |
| Elective procedure with TVCAD, N (%) | 184 (45.9) | 96 (36.8) | 0.025 |
| Urgency procedure to 30 days with TVCAD, N (%) | 49 (46.2) | 28 (49.8) | 0.678 |
| Urgency procedure to 7 days with TVCAD, N (%) | 168 (52.3) | 154 (54.6) | 0.634 |
| Life-saving procedure with TVCAD, N (%) | 10 (40) | 20 (58.8) | 0.244 |
| Pre-Pandemic N = 853 | Pandemic N = 646 | p-Value | |
|---|---|---|---|
| Perioperative myocardial infarction, N (%) | 6 (0.7) | 4 (0.6) | 0.843 |
| Postoperative low cardiac output syndrome, N (%) | 238 (27.9) | 194 (30) | 0.367 |
| Postoperative mechanical support, N (%) | 16 (1.9) | 12 (1.9) | 0.979 |
| Duration of mechanical ventilation, hours | 11 [9.3; 13.6] | 12 [9.6; 15] | 0.003 |
| Reintubation, N (%) | 10 (1.2) | 14 (2.2) | 0.129 |
| Postoperative atrial fibrillation, N (%) | 38 (4.5) | 31 (4.8) | 0.753 |
| Renal replacement therapy, N (%) | 6 (2.7) | 0 | 0.148 |
| Reoperation, N (%) | 14 (6.3) | 6 (5.3) | 0.856 |
| Pulmonary complication, N (%) | 29 (3.4) | 28 (4.3) | 0.349 |
| Septic complication, N (%) | 18 (2.1) | 16 (2.5) | 0.637 |
| Neurologic complication, N (%) | 30 (3.5) | 26 (4) | 0.608 |
| Intensive care unit stay, days | 1.7 ± 2.5 | 1.9 ± 3.3 | 0.029 |
| Duration of hospitalization, N (%) | 8.5 ± 5.6 | 8.7 ± 9.6 | 0.249 |
| In-hospital mortality, N (%) | 15 (1.8) | 21 (3.3) | 0.089 |
| 30-day mortality, N (%) | 12 (1.4) | 21 (3.3) | 0.026 |
| 1st Wave N = 221 | 2nd Wave N = 114 | 3rd Wave N = 311 | p-Value | |
|---|---|---|---|---|
| Sex, men, N (%) | 162 (73.3) | 92 (80.7) | 245 (78.8) | 0.208 |
| Age, years | 67 [61.9; 72.7] | 66.3 [61.7; 71.8] | 67.3 [61.5; 72.8] | 0.624 |
| Body mass index, kg/m2 | 28.4 [25.1; 31.8] | 28.7 [25.4; 32.8] | 28.4 [25.5; 31.2] | 0.789 |
| Diabetes mellitus, N% | 110 (49.8) | 52 (45.6) | 159 (51.1) | 0.602 |
| Hyperlipidaemia, N (%) | 160 (72.4) | 82 (71.9) | 251 (80.7) | 0.041 |
| Arterial hypertension, N (%) | 203 (91.9) | 98 (85.9) | 288 (92.6) | 0.092 |
| Active nicotine abuse, N (%) | 45 (20.4) | 30 (26.3) | 82 (26.4) | 0.242 |
| Nicotine abuse in past, N (%) | 110 (49.8) | 50 (43.9) | 168 (54) | 0.167 |
| Metabolic syndrome, N (%) | 36 (16.3) | 14 (12.3) | 58 (18.6) | 0.294 |
| Chronic kidney disease, N (%) | 26 (11.8) | 14 (12.3) | 45 (14.5) | 0.631 |
| Estimated glomerular filtration rate, mL/min/1.73 m2 | 74.9 [60.1; 86.2] | 81.2 [61.6; 98.2] | 73.5 [55.6; 90.4] | 0.062 |
| Pulmonary comorbidities, N (%) | 21 (9.5) | 11 (9.6) | 22 (7.1) | 0.523 |
| Cerebrovascular comorbidities, N (%) | 25 (11.3) | 11 (9.6) | 27 (8.7) | 0.601 |
| CCS I, N (%) | 11 (4.9) | 5 (4.4) | 18 (5.8) | 0.825 |
| CCS II, N (%) | 103 (46.6) | 46 (40.4) | 135 (43.4) | 0.469 |
| CCS III, N (%) | 61 (27.6) | 32 (28.1) | 76 (24.4) | 0.803 |
| CCS IV, N (%) | 23 (10.4) | 20 (17.5) | 39 (12.5) | 0.177 |
| NYHA I, N (%) | 18 (8.1) | 8 (7) | 52 (16.7) | 0.002 |
| NYHA II, N (%) | 144 (65.2) | 61 (53.5) | 146 (46.9) | 0.001 |
| NYHA III, N (%) | 30 (13.6) | 20 (17.5) | 48 (15.4) | 0.359 |
| NYHA IV, N (%) | 2 (0.9) | 1 (0.9) | 7 (2.3) | 0.378 |
| Critical preoperative state, N (%) | 44 (19.9) | 24 (21.1) | 46 (14.8) | 0.179 |
| EUROSCORE II, % | 2.3 [1.3; 4.1] | 1.9 [1.2; 4.3] | 1.9 [1.2; 4] | 0.212 |
| Ejection fraction, % | 50 [42; 55] | 50 [42; 55] | 50 [40; 55] | 0.863 |
| 1st Wave N = 221 | 2nd Wave N = 114 | 3rd Wave N = 311 | p-Value | |
|---|---|---|---|---|
| Elective procedure, N (%) | 84 (38.1) | 30 (26.3) | 148 (47.6) | 0.0003 |
| Urgency procedure to 30 days, N (%) | 36 (16.2) | 10 (8.8) | 42 (13.5) | 0.164 |
| Urgency procedure to 7 days, N (%) | 95 (42.3) | 61 (53.5) | 128 (41.2) | 0.071 |
| Life-saving procedure, N (%) | 6 (2.7) | 13 (11.4) | 13 (4.2) | 0.003 |
| Use of cardiopulmonary bypass, N (%) | 97 (43.9) | 67 (58.8) | 184 (59.2) | 0.001 |
| Type of procedure, MIDCAB, N (%) | 7 (3.2) | 5 (4.4) | 7 (2.3) | 0.499 |
| Type of procedure, OPCAB, N (%) | 116 (52.5) | 42 (36.8) | 120 (38.6) | 0.002 |
| Duration of procedure, min | 300 [255; 345] | 305 [260; 360] | 330 [285; 380] | 0.0001 |
| Duration of cardiopulmonary bypass, min | 92.5 [80; 121] | 98 [78; 128] | 102 [80; 125] | 0.469 |
| Number of bypass vessels, N (%) | 2 [2; 3] | 2 [2; 3] | 2 [2; 3] | 0.827 |
| TVCAD, N (%) | 97 (43.9) | 54 (47.4) | 147 (47.3) | 0.954 |
| Elective procedure with TVCAD, N (%) | 30 (13.6) | 9 (7.9) | 57 (18.3) | 0.107 |
| Urgency procedure to 30 days with TVCAD, N (%) | 15 (6.8) | 3 (2.6) | 10 (3.2) | 0.293 |
| Urgency procedure to 7 days with TVCAD, N (%) | 50 (22.6) | 35 (30.7) | 69 (22.2) | 0.462 |
| Life-saving procedure with TVCAD, N (%) | 2 (0.9) | 7 (6.1) | 11 (3.5) | 0.123 |
| 1st Wave N = 221 | 2nd Wave N = 114 | 3rd Wave N = 311 | p-Value | |
|---|---|---|---|---|
| Perioperative myocardial infarction, N (%) | 1 (0.47) | 0 | 4 (1.3) | 0.690 |
| Postoperative low cardiac output syndrome, N (%) | 63 (28.5) | 33 (28.9) | 99 (31.8) | 0.677 |
| Postoperative mechanical support, N (%) | 4 (1.8) | 3 (2.6) | 5 (1.6) | 0.975 |
| Duration of mechanical ventilation, hours | 11.5 [9.3; 15] | 11.9 [9.5; 15.5] | 11.8 [9.8; 14.9] | 0.535 |
| Reintubation, N (%) | 4 (1.8) | 2 (1.8) | 8 (2.6) | 0.792 |
| Postoperative atrial fibrillation, N (%) | 14 (6.3) | 4 (3.5) | 13 (4.2) | 0.769 |
| Renal replacement therapy, N (%) | 6 (2.7) | 0 | 4 (1.3) | 0.148 |
| Reoperation, N (%) | 14 (6.3) | 6 (5.3) | 21 (6.8) | 0.856 |
| Pulmonary complication, N (%) | 4 (1.8) | 8 (7) | 16 (5.1) | 0.053 |
| Septic complication, N (%) | 4 (1.8) | 4 (3.5) | 8 (2.6) | 0.631 |
| Neurologic complication, N (%) | 4 (1.8) | 7 (6.1) | 15 (4.8) | 0.098 |
| Intensive care unit stay, days | 2.6 ± 1.9 | 3.3 ± 3.5 | 2.7 ± 1.3 | 0.020 |
| Duration of hospitalization, N (%) | 8.5 ± 5.8 | 11.1 ± 19.2 | 7.9 ± 5.7 | 0.046 |
| In-hospital mortality, N (%) | 5 (2.3) | 5 (4.4) | 11 (3.5) | 0.539 |
| 30-day mortality, N (%) | 5 (2.3) | 5 (4.4) | 11 (3.5) | 0.539 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nadziakiewicz, P.; Wajda-Pokrontka, M. The Impact of the COVID-19 Pandemic on Coronary Artery Bypass Grafting Surgery: A Single-Centre Retrospective Cohort Study. Biomedicines 2025, 13, 2264. https://doi.org/10.3390/biomedicines13092264
Nadziakiewicz P, Wajda-Pokrontka M. The Impact of the COVID-19 Pandemic on Coronary Artery Bypass Grafting Surgery: A Single-Centre Retrospective Cohort Study. Biomedicines. 2025; 13(9):2264. https://doi.org/10.3390/biomedicines13092264
Chicago/Turabian StyleNadziakiewicz, Paweł, and Marta Wajda-Pokrontka. 2025. "The Impact of the COVID-19 Pandemic on Coronary Artery Bypass Grafting Surgery: A Single-Centre Retrospective Cohort Study" Biomedicines 13, no. 9: 2264. https://doi.org/10.3390/biomedicines13092264
APA StyleNadziakiewicz, P., & Wajda-Pokrontka, M. (2025). The Impact of the COVID-19 Pandemic on Coronary Artery Bypass Grafting Surgery: A Single-Centre Retrospective Cohort Study. Biomedicines, 13(9), 2264. https://doi.org/10.3390/biomedicines13092264





