Combined Serum IL-6 and CYFRA 21-1 as Potential Biomarkers for Radon-Associated Lung Cancer Risk: A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Area
2.2. Study Subjects and Sample Collection
2.3. Determination of Biomarker Serum Levels
2.4. Statistical Analyses
3. Results
3.1. Characteristics of the Participants
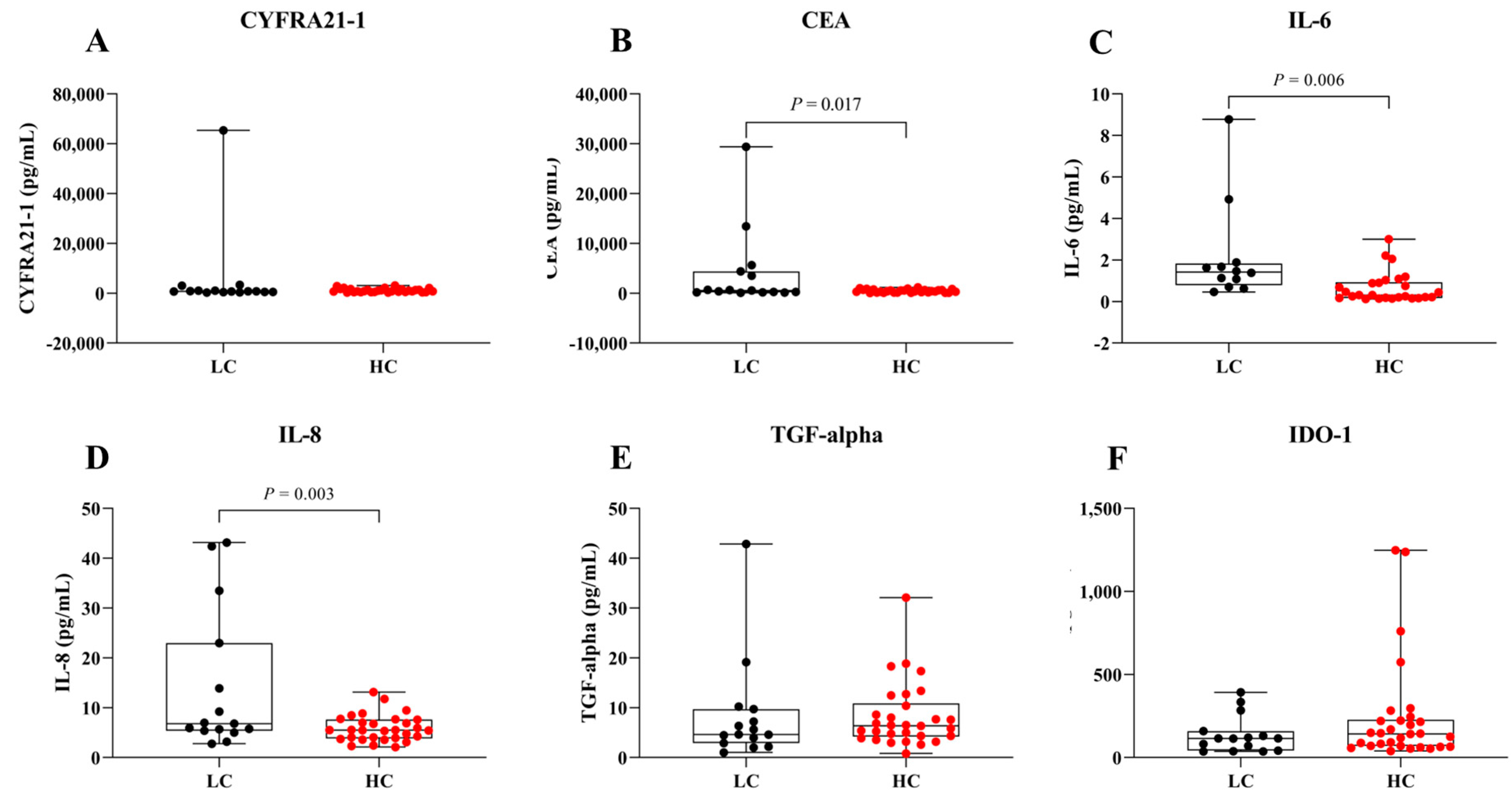
3.2. Comparative Serum Analyte Levels in LC Versus HC Groups
3.3. Comparative Levels of Serum Analytes Among LC, LR, and HR Groups
3.4. Evaluation of the Diagnostic Capability of Serum Biomarkers for LC Risk in HC and HR Groups
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AUC | Area under the curve |
| CEA | Carcinoembryonic antigen |
| CI | Confidence interval |
| CYFRA 21-1 | Cytokeratin 19 fragment |
| HC | Healthy controls |
| HR | High radon |
| IDO-1 | Indoleamine 2,3-dioxygenase 1 |
| IL-6 | Interleukin-6 |
| IL-8 | Interleukin-8 |
| LC | Lung cancer |
| LDCT | Low-dose computed tomography |
| LOD | Limit of detection |
| LR | Low radon |
| NSCLC | Non-small cell lung cancer |
| PM | Particulate matter |
| ROC | Receiver operating characteristic |
| SCLC | Small cell lung cancer |
| SD | Standard deviation |
| TGF-alpha | Transforming growth factor alpha |
References
- Bray, F.; Laversanne, M.; Sung, H.; Ferlay, J.; Siegel, R.L.; Soerjomataram, I.; Jemal, A. Global cancer statistics 2024: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2024, 74, 229–263. [Google Scholar]
- International Agency for Research on Cancer. Thailand Fact Sheet. GLOBOCAN 2020. Available online: https://gco.iarc.who.int/media/globocan/factsheets/populations/764-thailand-fact-sheet.pdf (accessed on 1 February 2025).
- Zappa, C.; Mousa, S.A. Non-small cell lung cancer: Current treatment and future advances. Transl. Lung Cancer Res. 2016, 5, 288–300. [Google Scholar] [CrossRef]
- American Cancer Society. 5-Year Survival Rates for Non-Small Cell Lung Cancer. Available online: https://www.cancer.org/cancer/types/lung-cancer/detection-diagnosis-staging/survival-rates.html (accessed on 1 February 2025).
- D’Antona, P.; Cattoni, M.; Dominioni, L.; Poli, A.; Moretti, F.; Cinquetti, R.; Gini, E.; Daffrè, E.; Noonan, D.M.; Imperatori, A.; et al. Serum miR-223: A validated biomarker for detection of early-stage non–small cell lung cancer. Cancer Epidemiol. Biomark. Prev. 2019, 28, 1926–1933. [Google Scholar] [CrossRef] [PubMed]
- Yuan, J.; Sun, Y.; Wang, K.; Wang, Z.; Li, D.; Fan, M.; Bu, X.; Chen, J.; Wu, Z.; Geng, H.; et al. Development and validation of reassigned CEA, CYFRA21-1 and NSE-based models for lung cancer diagnosis and prognosis prediction. BMC Cancer 2022, 22, 686. [Google Scholar] [CrossRef] [PubMed]
- Pan, J.; Zhuang, W.; Xia, Y.; Huang, Z.; Zheng, Y.; Wang, X.; Huang, Y. Combined detection of serum IL-6 and CEA contributes to the diagnosis of lung adenocarcinoma in situ. PeerJ 2024, 12, e17141. [Google Scholar] [CrossRef]
- Okamura, K.; Takayama, K.; Izumi, M.; Harada, T.; Furuyama, K.; Nakanishi, Y. Diagnostic value of CEA and CYFRA 21-1 tumor markers in primary lung cancer. Lung Cancer 2013, 80, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Boutsikou, E.; Hardavella, G.; Fili, E.; Bakiri, A.; Gaitanakis, S.; Kote, A.; Samitas, K.; Gkiozos, I. The role of biomarkers in lung cancer screening. Cancers 2024, 16, 1980. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Wiwatanadate, P. Lung cancer related to environmental and occupational hazards and epidemiology in Chiang Mai, Thailand. Genes Environ. 2011, 33, 120–127. [Google Scholar] [CrossRef]
- Riudavets, M.; de Herreros, M.G.; Besse, B.; Mezquita, L. Radon and lung cancer: Current trends and future perspectives. Cancers 2022, 14, 3142. [Google Scholar] [CrossRef]
- International Agency for Research on Cancer. Radon. IARC Monogr. Eval. Carcinog. Risks Hum. 1988, 43, 173–259. [Google Scholar]
- Autsavapromporn, N.; Krandrod, C.; Klunklin, P.; Kritsananuwat, R.; Jaikang, C.; Kittidachanan, K.; Chitapanarux, I.; Fugkeaw, S.; Hosoda, M.; Tokonami, S. Health effects of natural environmental radiation during burning season in Chiang Mai, Thailand. Life 2022, 12, 853. [Google Scholar] [CrossRef]
- Autsavapromporn, N.; Klunklin, K.; Chitapanarux, I.; Jaikang, C.; Chewaskulyong, B.; Sripan, P.; Hosoda, M.; Tokonami, S. A potential serum biomarker for screening lung cancer risk in high level environmental radon areas: A pilot study. Life 2021, 11, 1273. [Google Scholar] [CrossRef]
- Tokonami, S.; Takahashi, H.; Kobayashi, Y.; Zhuo, W.; Hulber, E. Up-to-date radon-thoron discriminative detector for a large scale survey. Rev. Sci. Instrum. 2005, 76, 113505. [Google Scholar] [CrossRef]
- Autsavapromporn, N.; Kranrod, C.; Kritsananuwat, R.; Sola, P.; Klunklin, P.; Chitapanarux, I.; Jaikang, C.; Monum, T.; Hosoda, M.; Tokonami, S. Health impacts of natural background radiation in high air pollution area of Thailand. Toxics 2024, 12, 428. [Google Scholar] [CrossRef]
- Autsavapromporn, N.; Duangya, A.; Klunklin, P.; Chitapanarux, I.; Kranrod, C.; Jaikang, C.; Monum, T.; Paemanee, A.; Tokonami, S. Serum metabolomics study to screen potential biomarkers of lung cancer risk in high natural background radiation areas of Thailand: A pilot study. Cancers 2024, 16, 4182. [Google Scholar] [CrossRef]
- Autsavapromporn, N.; Duangya, A.; Klunklin, P.; Chitapanarux, I.; Kranrod, C.; Jaikang, C.; Monum, T.; Paemanee, A.; Tokonami, S. Serum biomarkers associated with health impacts of high residential radon exposure: A metabolomic pilot study. Sci. Rep. 2025, 15, 5099. [Google Scholar] [CrossRef]
- Günther, A.; Becker, M.; Göpfert, J.; Joos, T.; Schneiderhan-Marra, N. Comparison of bead-based fluorescence versus planar electrochemiluminescence multiplex immunoassays for measuring cytokines in human plasma. Front. Immunol. 2020, 11, 572634. [Google Scholar] [CrossRef]
- Lesbek, A.; Omori, Y.; Bakhtin, M.; Kazymbet, P.; Tokonami, S.; Altaeva, N.; Ibrayeva, D.; Kashkinbayev, Y. Systematic review and meta-analysis of inflammatory biomarkers in individuals exposed to radon. Biomedicines 2025, 13, 499. [Google Scholar] [CrossRef]
- Qu, Z.; Sun, F.; Zhou, J.; Li, L.; Shapiro, S.D.; Xiao, G. Interleukin-6 prevents the initiation but enhances the progression of lung cancer. Cancer Res. 2015, 75, 3209–3215. [Google Scholar] [CrossRef]
- Briukhovetska, D.; Dörr, J.; Endres, S.; Libby, P.; Dinarello, C.A.; Kobold, S. Interleukins in cancer: From biology to therapy. Nat. Rev. Cancer 2021, 21, 481–499. [Google Scholar] [CrossRef]
- Vilotić, A.; Nacka-Aleksić, M.; Pirković, A.; Bojić-Trbojević, Ž.; Dekanski, D.; Jovanović Krivokuća, M. IL-6 and IL-8: An overview of their roles in healthy and pathological pregnancies. Int. J. Mol. Sci. 2022, 23, 14574. [Google Scholar] [CrossRef]
- Yang, Y.; Xu, M.; Huang, H.; Jiang, X.; Gong, K.; Liu, Y.; Kuang, X.; Yang, X. Serum carcinoembryonic antigen elevation in benign lung diseases. Sci. Rep. 2021, 11, 19044. [Google Scholar] [CrossRef]
- Grunnet, M.; Sorensen, J.B. Carcinoembryonic antigen (CEA) as tumor marker in lung cancer. Lung Cancer 2012, 76, 138–143. [Google Scholar] [CrossRef]
- Wieskopf, B.; Demangeat, C.; Purohit, A.; Stenger, R.; Gries, P.; Kreisman, H.; Quoix, E. Cyfra 21-1 as a biologic marker of non-small cell lung cancer. Evaluation of sensitivity, specificity, and prognostic role. Chest 1995, 108, 163–169. [Google Scholar] [CrossRef]
- Minamibata, A.; Kono, Y.; Arimoto, T.; Marunaka, Y.; Takayama, K. Variability of serum CYFRA 21 − 1 and its susceptibility to clinical characteristics in individuals without cancer: A 4-year retrospective analysis. BMC Pulm. Med. 2023, 23, 344. [Google Scholar] [CrossRef]
- Normanno, N.; De Luca, A.; Bianco, C.; Strizzi, L.; Mancino, M.; Maiello, M.R.; Carotenuto, A.; De Feo, G.; Caponigro, F.; Salomon, D.S. Epidermal growth factor receptor (EGFR) signaling in cancer. Gene 2006, 366, 2–16. [Google Scholar] [CrossRef]
- Wu, W.; O’Reilly, M.S.; Langley, R.R.; Tsan, R.Z.; Baker, C.H.; Bekele, N.; Tang, X.M.; Onn, A.; Fidler, I.J.; Herbst, R.S. Expression of epidermal growth factor (EGF)/transforming growth factor-alpha by human lung cancer cells determines their response to EGF receptor tyrosine kinase inhibition in the lungs of mice. Mol. Cancer Ther. 2007, 6, 2652–2663. [Google Scholar] [CrossRef]
- Prendergast, G.C.; Malachowski, W.J.; Mondal, A.; Scherle, P.; Muller, A.J. Indoleamine 2,3-dioxygenase and its therapeutic inhibition in cancer. Int. Rev. Cell Mol. Biol. 2018, 336, 175–203. [Google Scholar]
- Liu, M.; Wang, X.; Wang, L.; Ma, X.; Gong, Z.; Zhang, S.; Li, Y. Targeting the IDO1 pathway in cancer: From bench to bedside. J. Hematol. Oncol. 2018, 11, 100. [Google Scholar] [CrossRef]
- Munn, D.H.; Mellor, A.L. Indoleamine 2,3-dioxygenase and tumor-induced tolerance. J. Clin. Investig. 2007, 117, 1147–1154. [Google Scholar] [CrossRef]
- Meireson, A.; Devos, M.; Brochez, L. IDO expression in cancer: Different compartment, different functionality? Front. Immunol. 2020, 11, 531491. [Google Scholar] [CrossRef]
- Yan, X.; Han, L.; Zhao, R.; Fatima, S.; Zhao, L.; Gao, F. Prognosis value of IL-6, IL-8, and IL-1β in serum of patients with lung cancer: A fresh look at interleukins as a biomarker. Heliyon 2022, 8, e09953. [Google Scholar] [CrossRef]
- Gaur, P.; Bhattacharya, S.; Kant, S.; Kushwaha, R.A.; Garg, R.; Singh, G.; Pandey, S. Association of inflammatory biomarkers with lung cancer in North Indian population. Afr. Health Sci. 2019, 19, 2147–2155. [Google Scholar] [CrossRef]
- Stephens, E.K.H.; Sigcha, J.G.; Lopez-Loo, K.; Yang, I.A.; Marshall, H.M.; Fong, K.M. Biomarkers of lung cancer for screening and in never-smokers—A narrative review. Transl. Lung Cancer Res. 2023, 12, 2129–2145. [Google Scholar] [CrossRef]
- Leng, S.; Thomas, C.L.; Snider, A.M.; Picchi, M.A.; Chen, W.; Willis, D.G.; Carr, T.G.; Krzeminski, J.; Desai, D.; Shantu, A.; et al. Radon exposure, IL-6 promoter variants, and lung squamous cell carcinoma in former uranium miners. Environ. Health Perspect. 2016, 124, 445–451. [Google Scholar] [CrossRef]
- Alsulami, S.; Jung, Y.S.; Li, L.; Banzon, T. Radon exposure induces IL-6-mediated airway inflammation in non-sensitized children with asthma. J. Allergy Clin. Immunol. 2025, 155, AB112. [Google Scholar] [CrossRef]
- Lin, M.; Li, Y.; Wang, S.; Cao, B.; Li, C.; Li, G. Sphingolipid metabolism and signaling in lung cancer: A potential therapeutic target. J. Oncol. 2022, 2022, 9099612. [Google Scholar] [CrossRef]
- Terlizzi, M.; Colarusso, C.; Somma, P.; De Rosa, I.; Panico, L.; Pinto, A.; Sorrentino, R. S1P-induced TNF-α and IL-6 release from PBMCs exacerbates lung cancer-associated inflammation. Cells 2022, 11, 2524. [Google Scholar] [CrossRef]


| Characteristics | LC (n = 15) | LR (n = 15) | HR (n = 15) | p Value |
|---|---|---|---|---|
| Age in years, Mean (SD) | 62 (13.3) | 61.1 (11.2) | 61.3 (13) | 0.98 |
| Gender | 1 | |||
| Male | 8 | 8 | 8 | |
| Female | 7 | 7 | 7 | |
| Education | 0.91 | |||
| Middle school or lower | 9 | 10 | 9 | |
| High school or higher | 6 | 5 | 6 | |
| Alcohol consumption | 0.84 | |||
| Yes | 2 | 3 | 2 | |
| No | 13 | 12 | 13 | |
| Smoking status | 0.004 | |||
| Never smokers | 10 | 15 | 15 | |
| Former smokers | 5 | 0 | 0 | |
| Stage of lung cancer | - | |||
| I | 13 | 0 | 0 | |
| II | 2 | 0 | 0 | |
| Tumor histology | - | |||
| Adenocarcinoma | 10 | 0 | 0 | |
| Squamous cell carcinoma | 5 | 0 | 0 |
| Markers (pg/mL) | LC (n = 15) | HC (n = 30) | LR (n = 15) | HR (n = 15) |
|---|---|---|---|---|
| CYFRA 21-1 | ||||
| Mean | 5325.8 | 1132.5 | 752 | 1513.1 |
| SD | 16,631.1 | 766.2 | 470.5 | 827.3 |
| Min | 274.9 | 274.9 | 274.9 | 346.4 |
| Max | 65,353.5 | 3151.4 | 1321 | 3151.4 |
| Median | 778.1 | 876.4 | 609 | 1392.7 |
| CEA | ||||
| Mean | 3990 | 459.8 | 391.7 | 527.9 |
| SD | 7882.8 | 312.6 | 305.6 | 314.8 |
| Min | 121.2 | 62.2 | 62.2 | 107.6 |
| Max | 29,384.8 | 1174.9 | 1010.2 | 1174.9 |
| Median | 568.8 | 377.7 | 316.6 | 572.6 |
| IL-6 | ||||
| Mean | 2.2 | 0.7 | 0.5 | 0.9 |
| SD | 2.4 | 0.7 | 0.4 | 1 |
| Min | 0.5 | 0.1 | 0.1 | 0.1 |
| Max | 8.8 | 3 | 1.2 | 3 |
| Median | 1.4 | 0.3 | 0.3 | 0.3 |
| IL-8 | ||||
| Mean | 14.2 | 5.9 | 5.7 | 6.1 |
| SD | 14.2 | 2.7 | 2.6 | 2.8 |
| Min | 2.7 | 2.1 | 2.1 | 2.3 |
| Max | 43.1 | 13.1 | 11.8 | 13.1 |
| Median | 6.8 | 5.5 | 5.4 | 5.9 |
| TGF-alpha | ||||
| Mean | 8.5 | 8.3 | 7.4 | 9.2 |
| SD | 10.5 | 6.5 | 7.7 | 5.2 |
| Min | 1 | 0.8 | 0.8 | 4.4 |
| Max | 42.9 | 32.1 | 32.1 | 18.9 |
| Median | 4.7 | 6.4 | 5.3 | 7.6 |
| IDO-1 | ||||
| Mean | 138.3 | 243.4 | 252.9 | 233.8 |
| SD | 111.8 | 312.6 | 324.1 | 311.7 |
| Min | 37.2 | 39.9 | 39.9 | 54.8 |
| Max | 393.2 | 1248.1 | 1238.2 | 1248.1 |
| Median | 115.4 | 143.4 | 149.8 | 118.4 |
| Biomarkers | Cut-Off | AUC (95% CI) | Sensitivity (95% CI) | Specificity (95% CI) | Youden Index (95% CI) | p Value |
|---|---|---|---|---|---|---|
| CYFRA 21-1 | 1157.00 | 0.53 (0.35–0.72) | 0.40 (0.20–0.64) | 0.80 (0.63–0.90) | 0.20 (−0.17–0.55) | 0.72 |
| CEA | 149.20 | 0.62 (0.43–0.80) | 0.20 (0.07–0.45) | 0.93 (0.79–0.98) | 0.13 (−0.14–0.43) | 0.20 |
| IL-6 | 0.55 | 0.83 (0.70–0.96) | 0.62 (0.36–0.80) | 0.92 (0.79–0.98 | 0.53 (0.14–0.78) | 0.001 |
| IL-8 | 4.90 | 0.68 (0.50–0.85) | 0.40 (0.20–0.64) | 0.87 (0.70–0.95) | 0.27 (−0.10–0.59) | 0.06 |
| TGF-alpha | 10.31 | 0.58 (0.40–0.77) | 0.27 (0.11–0.52) | 0.87 (0.70–0.95) | 0.13 (−0.19–0.47) | 0.37 |
| IDO-1 | 136.40 | 0.61 (0.43–0.79) | 0.53 (0.30–0.75) | 0.73 (0.56–0.86) | 0.27 (−0.14–0.61) | 0.24 |
| IL-6 + IL-8 | 0.87 (0.76–0.99) | 0.41 (0.20–0.64) | 0.96 (0.83–0.99) | 0.37 (0.03–0.64) | 0.0003 |
| Biomarkers | Cut-Off | AUC (95% CI) | Sensitivity (95% CI) | Specificity (95% CI) | Youden Index (95% CI) | p Value |
|---|---|---|---|---|---|---|
| CYFRA 21-1 | 1157.00 | 0.66 (0.45–0.87) | 0.67 (0.42–0.85) | 0.80 (0.55–0.93) | 0.47 (−0.03–0.78) | 0.13 |
| CEA | 149.20 | 0.58 (0.37–0.79) | 0.20 (0.07–0.45) | 0.93 (0.70–0.99) | 0.13 (−0.23–0.44) | 0.47 |
| IL-6 | 0.54 | 0.75 (0.55–0.95) | 0.54 (0.30–0.75) | 0.92 (0.70–0.99) | 0.46 (0.00–0.74) | 0.03 |
| IL-8 | 4.54 | 0.64 (0.43–0.84) | 0.33 (0.15–0.58) | 0.87 (0.62–0.96) | 0.20 (−0.23–0.55) | 0.21 |
| TGF-alpha | 10.31 | 0.67 (0.47–0.87) | 0.33 (0.15–0.58) | 0.87 (0.62–0.96) | 0.20 (−0.23–0.55) | 0.11 |
| IDO-1 | 137.40 | 0.59 (0.38–0.79) | 0.47 (0.25–0.70) | 0.73 (0.48–0.89) | 0.20 (−0.27–0.59) | 0.42 |
| CYFRA21-1 + IL-6 | 0.81 (0.63–0.99) | 0.75 (0.48–0.89) | 0.85 (0.62–0.96) | 0.60 (0.10–0.85) | 0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Autsavapromporn, N.; Duangya, A.; Klunklin, P.; Chitapanarux, I.; Kranrod, C.; Jaikang, C.; Monum, T.; Tokonami, S. Combined Serum IL-6 and CYFRA 21-1 as Potential Biomarkers for Radon-Associated Lung Cancer Risk: A Pilot Study. Biomedicines 2025, 13, 2145. https://doi.org/10.3390/biomedicines13092145
Autsavapromporn N, Duangya A, Klunklin P, Chitapanarux I, Kranrod C, Jaikang C, Monum T, Tokonami S. Combined Serum IL-6 and CYFRA 21-1 as Potential Biomarkers for Radon-Associated Lung Cancer Risk: A Pilot Study. Biomedicines. 2025; 13(9):2145. https://doi.org/10.3390/biomedicines13092145
Chicago/Turabian StyleAutsavapromporn, Narongchai, Aphidet Duangya, Pitchayaponne Klunklin, Imjai Chitapanarux, Chutima Kranrod, Churdsak Jaikang, Tawachai Monum, and Shinji Tokonami. 2025. "Combined Serum IL-6 and CYFRA 21-1 as Potential Biomarkers for Radon-Associated Lung Cancer Risk: A Pilot Study" Biomedicines 13, no. 9: 2145. https://doi.org/10.3390/biomedicines13092145
APA StyleAutsavapromporn, N., Duangya, A., Klunklin, P., Chitapanarux, I., Kranrod, C., Jaikang, C., Monum, T., & Tokonami, S. (2025). Combined Serum IL-6 and CYFRA 21-1 as Potential Biomarkers for Radon-Associated Lung Cancer Risk: A Pilot Study. Biomedicines, 13(9), 2145. https://doi.org/10.3390/biomedicines13092145










