Risk Factors for the Development of Early Onset Diabetes in the Population of Sindh Province, Pakistan
Abstract
1. Introduction
2. Materials and Methods
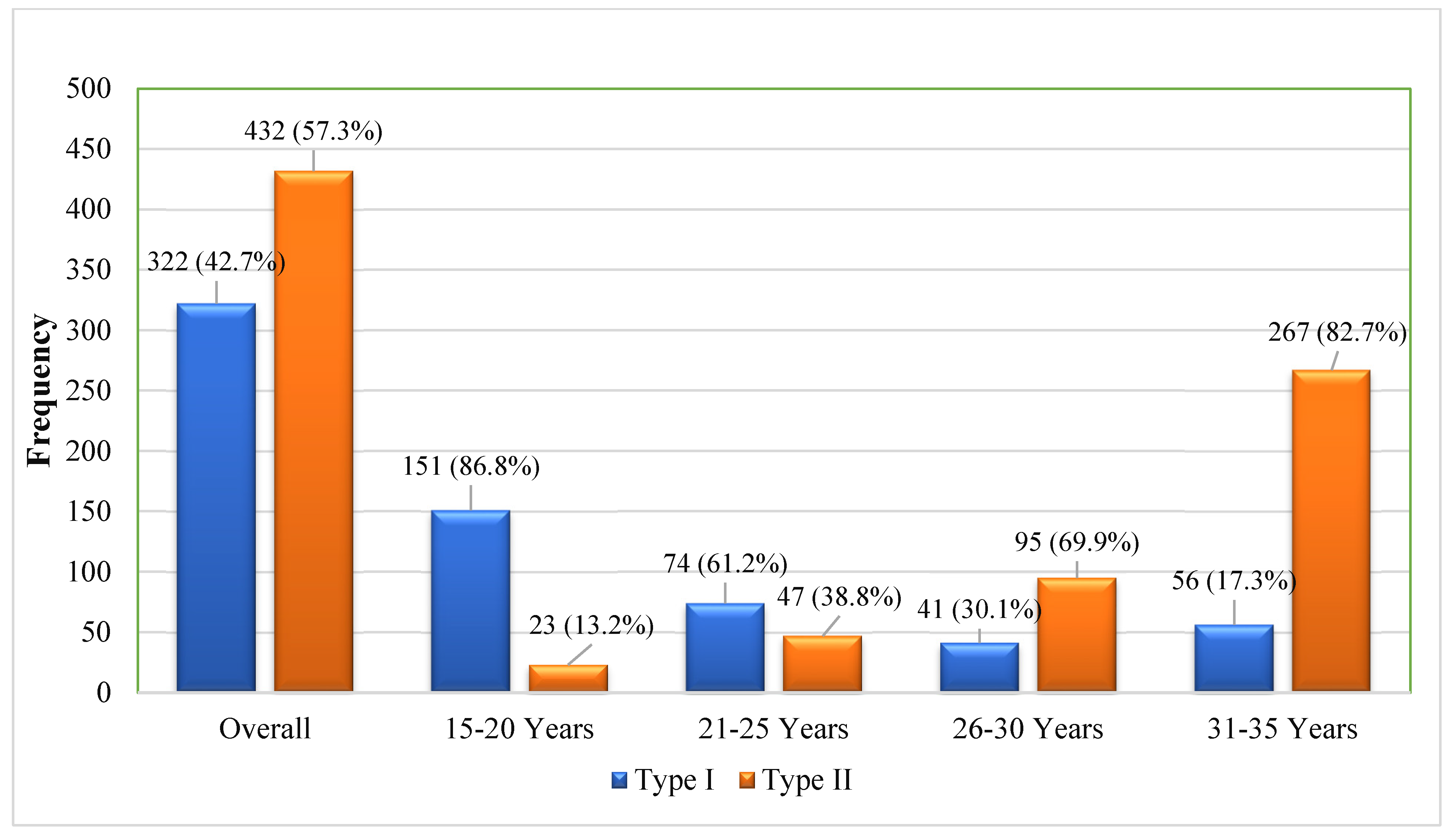
3. Results
4. Discussion
5. Conclusions and Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cloete, L. Diabetes mellitus: An overview of the types, symptoms, complications and management. Nurs. Stand. 2022, 37, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Gangwar, R.; Zargar, A.A.; Kumar, R.; Sharma, A. Prevalence of Diabetes in India: A Review of IDF Diabetes Atlas 10th Edition. Curr. Diabetes Rev. 2024, 20, e130423215752. [Google Scholar] [CrossRef] [PubMed]
- Kengne, A.P.; Ramachandran, A. Feasibility of prevention of type 2 diabetes in low- and middle-income countries. Diabetologia 2024, 67, 763–772. [Google Scholar] [CrossRef] [PubMed]
- Golovaty, I.; Ritchie, N.D.; Tuomilehto, J.; Mohan, V.; Ali, M.K.; Gregg, E.W.; Bergman, M.; Moin, T. Two decades of diabetes prevention efforts: A call to innovate and revitalize our approach to lifestyle change. Diabetes Res. Clin. Pract. 2023, 198, 110195. [Google Scholar] [CrossRef]
- Hossain, M.J.; Al-Mamun, M.; Islam, M.R. Diabetes mellitus, the fastest growing global public health concern: Early detection should be focused. Health Sci. Rep. 2024, 7, e2004. [Google Scholar] [CrossRef]
- Pan, J.; Jia, W. Early-onset diabetes: An epidemic in China. Front. Med. 2018, 12, 624–633. [Google Scholar] [CrossRef]
- Kyrou, I.; Tsigos, C.; Mavrogianni, C.; Cardon, G.; Van Stappen, V.; Latomme, J.; Kivelä, J.; Wikström, K.; Tsochev, K.; Nanasi, A.; et al. Sociodemographic and lifestyle-related risk factors for identifying vulnerable groups for type 2 diabetes: A narrative review with emphasis on data from Europe. BMC Endocr. Disord. 2020, 20 (Suppl. 1), 134. [Google Scholar] [CrossRef]
- Serbis, A.; Giapros, V.; Kotanidou, E.P.; Galli-Tsinopoulou, A.; Siomou, E. Diagnosis, treatment and prevention of type 2 diabetes mellitus in children and adolescents. World J. Diabetes 2021, 12, 344–365. [Google Scholar] [CrossRef]
- Schnurr, T.M.; Jakupović, H.; Carrasquilla, G.D.; Ängquist, L.; Grarup, N.; Sørensen, T.I.A.; Tjønneland, A.; Overvad, K.; Pedersen, O.; Hansen, T.; et al. Obesity, unfavourable lifestyle and genetic risk of type 2 diabetes: A case-cohort study. Diabetologia 2020, 63, 1324–1332. [Google Scholar] [CrossRef]
- Negrato, C.A.; Martins, R.L.M.; Louro, M.D.; Medeiros, G.A.; Lanzarin, J.V.M.; Zajdenverg, L.; Lopes, L.C.P. Association between perinatal and obstetric factors and early age at diagnosis of type 1 diabetes mellitus: A cohort study. J. Pediatr. Endocrinol. Metab. 2024, 37, 673–679. [Google Scholar] [CrossRef]
- Azeem, S.; Khan, U.; Liaquat, A. The increasing rate of diabetes in Pakistan: A silent killer. Ann. Med. Surg. 2022, 79, 103901. [Google Scholar] [CrossRef] [PubMed]
- Internet. Available online: https://diabetesatlas.org/data/en/region/7/sea.html (accessed on 23 October 2024).
- International Diabetes Federation. IDF Diabetes Atlas, 10th ed.; IDF Diabetes Atlas: Brussels, Belgium, 2021; Available online: https://www.diabetesatlas.org (accessed on 15 January 2025).
- Basit, A.; Mustafa, N.; Waris, N.; Askari, S.; Fawwad, A.; NDSP members. Predicting the risk of type 2 diabetes through anthropometric indices in Pakistani adults- A sub-analysis of second National diabetes survey of Pakistan 2016–2017 (NDSP-07). Diabetes Metab. Syndr. 2021, 15, 543–547. [Google Scholar] [CrossRef] [PubMed]
- Condie, A.M.; Allen, T.V.; Ogle, G.D. Incidence and characteristics of childhood- and youth-onset diabetes in the Qalandarabad area in northern Pakistan. Diabetes Res. Clin. Pract. 2020, 163, 108155. [Google Scholar] [CrossRef]
- Greenwood, S.; Newland-Jones, P.; Hicks, D.; Yousef, Z.; Moore, J.; Kelly, B.; Davies, S.; Dashora, U. Risk Prediction of the Diabetes Missing Million: Identifying Individuals at High Risk of Diabetes and Related Complications. Diabetes Ther. 2021, 12, 87–105. [Google Scholar] [CrossRef]
- Cao, L.; Zhou, J.; Chen, Y.; Wu, Y.; Wang, Y.; Liu, T.; Fu, C. Effects of Body Mass Index, Waist Circumference, Waist-to-Height Ratio and Their Changes on Risks of Dyslipidemia among Chinese Adults: The Guizhou Population Health Cohort Study. Int. J. Environ. Res. Public Health 2021, 19, 341. [Google Scholar] [CrossRef]
- World Health Organization. BMI-for-Age (5–19 Years). Available online: https://www.who.int/tools/growth-reference-data-for-5to19-years/indicators/bmi-for-age (accessed on 15 January 2025).
- Alzahrani, N.; Alouffi, S.; Almutairi, K.; Almutairi, M.; Almutairi, T.; Alwan, I.A.; Otaibi, N.; Tamimi, W. Can Fasting Blood Sugar be Used as an Indicator of Long-Term Diabetic Control Instead of Estimated Average Glucose? Clin. Lab. 2020, 66. [Google Scholar] [CrossRef]
- Dildar, S.; Imran, S.; Naz, F. Method comparison of Particle Enhanced Immunoturbidimetry (PEIT) with High Performance Liquid Chromatography (HPLC) for glycated hemoglobin (HbA1c) analysis. Clin. Diabetes Endocrinol. 2021, 7, 10. [Google Scholar] [CrossRef]
- Weir, C.B.; Jan, A. BMI Classification Percentile and Cut Off Points. [Updated 26 June 2023]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK541070/ (accessed on 19 January 2025).
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2018, 71, e127–e248. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. 6. Glycemic Goals and Hypoglycemia: Standards of Care in Diabetes—2024. Diabetes Care 2024, 47 (Suppl. S1), S111–S125. [Google Scholar] [CrossRef]
- World Health Organization. Physical Activity. Available online: https://www.who.int/initiatives/behealthy/physical-activity (accessed on 31 January 2025).
- World Health Organization. Increasing Fruit and Vegetable Consumption to Reduce the Risk of Noncommunicable Diseases. Last Updated: 9 August 2023. Available online: https://www.who.int/tools/elena/interventions/fruit-vegetables-ncds (accessed on 31 January 2025).
- Basit, A.; Fawwad, A.; Qureshi, H.; Shera, A.S.; NDSP Members. Prevalence of diabetes, pre-diabetes and associated risk factors: Second National Diabetes Survey of Pakistan (NDSP), 2016–2017. BMJ Open 2018, 8, e020961, Erratum in BMJ Open 2019, 8, e020961corr1. https://doi.org/10.1136/bmjopen-2017-020961corr1. [Google Scholar] [CrossRef]
- Mayer-Davis, E.J.; Lawrence, J.M.; Dabelea, D.; Divers, J.; Isom, S.; Dolan, L.; Imperatore, G.; Linder, B.; Marcovina, S.; Pettitt, D.J.; et al. Incidence Trends of Type 1 and Type 2 Diabetes among Youths, 2002–2012. N. Engl. J. Med. 2017, 376, 1419–1429. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Moran, M.; Guerrero-Romero, F.; Aradillas-García, C.; Violante, R.; Simental-Mendia, L.E.; Monreal-Escalante, E.; Mendoza Ede, L. Obesity and family history of diabetes as risk factors of impaired fasting glucose: Implications for the early detection of prediabetes. Pediatr. Diabetes 2010, 11, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Goodman, M.O.; Dashti, H.S.; Lane, J.M.; Windred, D.P.; Burns, A.; Jones, S.E.; Sofer, T.; Purcell, S.M.; Zhu, X.; Ollila, H.M.; et al. Causal Association Between Subtypes of Excessive Daytime Sleepiness and Risk of Cardiovascular Diseases. J. Am. Heart Assoc. 2023, 12, e030568. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Yeung, S.L.A.; Sharp, S.J.; Wang, M.; Jang, H.; Luo, S.; Brage, S.; Wijndaele, K. Genetic susceptibility, screen-based sedentary activities and incidence of coronary heart disease. BMC Med. 2022, 20, 188. [Google Scholar] [CrossRef]
| Parameters |
Overall n (%) | 15–19 Years | 20–24 Years | 25–29 Years | 30–35 Years | Chi Square/F Value | p-Value | |
|---|---|---|---|---|---|---|---|---|
|
Gender n (%) | Male | 390 (51.7) | 100 (57.5) | 62 (51.2) | 67 (49.3) | 161 (49.8) | 3.09 | 0.37 |
| Female | 364 (48.3) | 74 (42.5) | 59 (48.8) | 69 (50.7) | 162 (50.2) | |||
| Age of Diagnosis (Years) | Mean ± SD | 26.14 ± 6.53 | 16.79 ± 1.53 | 22.35 ± 1.81 | 28.63 ± 1.46 | 33.20 ± 1.41 | 4283.17 | <0.001 * |
|
Ethnicity n (%) | Baloch | 55 (7.3) | 12 (6.9) | 6 (5.0) | 10 (7.4) | 27 (8.4) | 12.50 | 0.64 |
| Hindko | 20 (2.7) | 3 (1.7) | 2 (1.7) | 3 (2.2) | 12 (3.7) | |||
| Pathan | 139 18.4) | 37 (21.3) | 20 16.5) | 28 (20.6) | 54 (16.7) | |||
| Punjabi | 103 (13.7) | 24 (13.8) | 20 (16.5) | 19 (14.0) | 40 (12.4) | |||
| Un Disclosed | 119 (15.8) | 29 (16.7) | 26 (21.5) | 15 (11.0) | 49 (15.2) | |||
| Sindhi | 318 (42.2) | 69 (39.7) | 47 38.8) | 61 (44.9) | 141 43.7) | |||
|
Highest Education n (%) | College/University Completed | 207 (27.5) | 47 (27.0) | 37 (30.6) | 43 (31.6) | 80 24.8) | 58.15 | <0.001 * |
| High School Completed | 192 (25.5) | 44 (25.3) | 28 (23.1) | 34 (25.0) | 86 26.6) | |||
| No Formal Schooling | 153 (20.3) | 20 (11.5) | 26 (21.5) | 27 (19.9) | 80 (24.8) | |||
| Post Graduate Degree | 38 (5.0) | 1 (0.6) | 3 (2.5) | 9 (6.6) | 25 (7.7) | |||
| Primary School Completed | 79 (10.5) | 30 (17.2) | 8 (6.6) | 11 (8.1) | 30 (9.3) | |||
| Un Disclosed | 9 (1.2) | 2 (1.1) | 4 (3.3) | 2 (1.5) | 1 0.3) | |||
| Secondary School Completed | 76 (10.1) | 30 (17.2) | 15 (12.4) | 10 (7.4) | 21 (6.5) | |||
|
Marital Status n (%) | Divorced | 3 (0.4) | 0 (0.0) | 1 (0.8) | 0 (0.0) | 2 (0.6) | 154.58 | <0.001 * |
| Married | 549 (72.8) | 72 (41.4) | 85 (70.2) | 115 (84.6) | 277 (85.8) | |||
| Unmarried | 191 (25.3) | 102 58.6) | 35 (28.9) | 19 (14.0) | 35 (10.8) | |||
| Widowed | 11 (1.5) | 0 (0.0) | 0 (0.0) | 2 (1.5) | 9 (2.8) | |||
|
Occupation n (%) | Government Employee | 14 (1.9) | 1 (0.6) | 3 (2.5) | 3 (2.2) | 7 (2.2) | 102.03 | <0.001 * |
| Non-Government Employee | 66 (8.8) | 23 (13.2) | 11 (9.1) | 10 (7.4) | 22 (6.8) | |||
| Self-Employed | 231 (30.6) | 48 (27.6) | 30 (24.8) | 46 (33.8) | 107 (33.1) | |||
| Student | 123 (16.3) | 66 (37.9) | 16 (13.2) | 13 (9.6) | 28 (8.7) | |||
| Un-Employed | 320 (42.4) | 36 (20.7) | 61 (50.4) | 64 (47.1) | 159 49.2) | |||
|
District n (%) | Karachi | 489 (64.9) | 120 (69.0) | 85 (70.2) | 90 (66.2) | 194 (60.1) | 15.193 | 0.08 |
| Hyderabad | 100 (13.3) | 24 (13.8) | 15 (12.4) | 16 (11.8) | 45 (13.9) | |||
| Larkana | 57 (7.6) | 12 (6.9) | 12 (9.9) | 11 (8.1) | 22 (6.8) | |||
| Sukkar | 108 (14.3) | 18 (10.3) | 9 (7.4) | 19 (14.0) | 62 (19.2) | |||
|
Family History of Diabetes n (%) | No History | 217 (28.8) | 56 (32.2) | 36 (29.8) | 35 (25.7) | 90 (27.9) | 9.50 | 0.023 * |
| One Generation | 62 (8.2) | 13 (7.5) | 8 (6.6) | 13 (9.6) | 28 (8.7) | |||
| Two Generations | 421 (55.8) | 86 (49.4) | 67 (55.4) | 79 (58.1) | 189 (58.5) | |||
| Three Generations | 54 (7.2) | 19 (10.9) | 10 (8.3) | 9 (6.6) | 16 (5.0) | |||
| Parameters |
Overall n (%) | Age of Diagnosis of Diabetes | Chi Square/Z | p-Value | ||||
|---|---|---|---|---|---|---|---|---|
| 15–19 Years | 20–25 Years | 26–30 Years | 31–35 Years | |||||
|
Smoking n (%) | Yes | 78 (10.0) | 15 (8.6) | 17 (14.0) | 15 (11.0) | 31 (9.6) | 2.612 | 0.45 |
| No | 676 (90.0) | 159 (91.4) | 104 (86.0) | 121 (89.0) | 292 (90.4) | |||
|
Smokeless Tobacco Use n (%) | Yes | 83 (11.0) | 21 (12.1) | 16 (13.2) | 15 (11.0) | 31 (9.6) | 1.46 | 0.69 |
| No | 671 (89.0) | 153 (87.9) | 105 (86.8) | 121 (89.0) | 292 (90.4) | |||
|
Former Smokers n (%) | Yes | 149 (19.8) | 27 (15.5) | 23 (19.0) | 27 (19.9) | 72 (22.3) | 3.32 | 0.34 |
| No | 605 (80.2) | 147 (84.5) | 98 (81.0) | 109 (80.9) | 251 (77.7) | |||
|
Physical Activity n (%) | Inadequate | 501 (66.4) | 117 (67.2) | 66 (54.5) | 86 (63.2) | 232 (71.8) | 12.558 | 0.006 * |
| Adequate | 232 (33.6) | 57 (32.8) | 55 (45.5) | 50 (36.8) | 91 (28.2) | |||
|
Consumption of sugar-added beverages? n (%) | Never | 370 (49.1) | 79 (45.4) | 66 (54.5) | 62 (45.6) | 163 (50.5) | 16.04 | 0.379 |
| Daily | 62 (8.2) | 14 (8.0) | 10 (8.3) | 7 (5.1) | 31 (9.6) | |||
| One a Month | 46 (6.1) | 11 (6.3) | 6 (5.0) | 11 (8.1) | 18 (5.6) | |||
| One a Week | 18 (2.1) | 2 1.1) | 4 (3.3) | 2 (1.5) | 10 (3.1) | |||
| Rarely | 9 (1.2) | 0 (0.0) | 2 (1.7) | 2 (1.5) | 5 (1.5) | |||
| Twice a Week | 249 (33.0) | 68 (39.1) | 33 (27.3) | 52 (38.2) | 96 (29.7) | |||
|
Fruit intake n (%) | Adequate | 445 (59.0) | 99 (56.9) | 73 (60.3) | 82 (60.3) | 191 (59.1) | 0.50 | 0.91 |
| Inadequate | 309 (41.0) | 75 (43.1) | 48 (39.7) | 54 (39.7) | 132 (40.9) | |||
|
Vegetable intake n (%) | Adequate | 480 (63.7) | 111 (63.8) | 84 (69.4) | 81 (59.6) | 204 63.2) | 2.76 | 0.43 |
| Inadequate | 274 (36.3) | 63 (36.2) | 37 (30.6) | 55 (40.4) | 119 (36.8) | |||
|
Consumption of Junk food n (%) | Daily | 165 (21.9) | 37 (21.3) | 28 (23.1) | 25 (18.4) | 75 (23.2) | 14.02 | 0.524 |
| Never | 123 (16.3) | 37 (21.3) | 17 (14.0) | 20 (14.7) | 49 (15.2) | |||
| One a Month | 106 (14.1) | 26 (14.9) | 21 (17.4) | 22 (16.2) | 37 (11.5) | |||
| One a Week | 150 (19.9) | 33 (19.0) | 25 (20.7) | 25 (18.4) | 67 (20.7) | |||
| Rarely | 117 (15.5) | 25 (14.4) | 20 (16.5) | 21 (15.4) | 51 (15.8) | |||
| Twice a Week | 93 (12.3) | 16 (9.2) | 10 (8.3) | 23 (16.9) | 44 13.6) | |||
|
Sleep Duration n (%) | 6–8 h | 548 (72.7) | 118 (67.8) | 74 (61.2) | 97 (71.3) | 259 (80.2) | 20.23 | 0.003 * |
| >8 h | 106 (14.1) | 29 (16.7) | 22 (18.2) | 20 (14.7) | 35 (10.8) | |||
| <6 h | 100 (13.3) | 27 (15.5) | 25 (20.7) | 19 (14.0) | 29 (9.0) | |||
| Parameters | Overall n (%) | Age of Diagnosis of Diabetes | Chi Square/Z | p-Value | ||||
|---|---|---|---|---|---|---|---|---|
| 15–19 Years | 20–25 Years | 26–30 Years | 31–35 Years | |||||
|
BMI Levels, n (%) | Underweight | 80 (10.6) | 39 (22.4) | 15 (12.4) | 12 (8.8) | 14 (4.3) | 113.3 | <0.001 * |
| Normal weight | 255 (33.8) | 86 (49.4) | 54 (44.6) | 35 (25.7) | 80 (24.8) | |||
| Overweight | 225 (29.8) | 37 (21.3) | 29 (24.0) | 47 (34.6) | 112 34.7) | |||
| Obese | 194 (25.7) | 12 (6.9) | 23 (19.0) | 42 (30.9) | 117 (36.2) | |||
|
Blood Pressure, n (%) | Normal | 290 (38.5) | 92 (52.9) | 56 (46.3) | 44 (32.4) | 98 (30.3) | 33.41 | <0.001 * |
| Elevated | 309 (41.0) | 53 (30.5) | 43 (35.5) | 60 (44.1) | 153 (47.4) | |||
| Stage-I hypertension | 144 (19.1) | 28 (16.1) | 21 (17.4) | 31 (22.8) | 64 19.8) | |||
| Stage-II hypertension | 11 (1.5) | 11 (1.5) | 1 (0.6) | 1 (0.8) | 1 (0.7) | |||
|
Hypercholesterolemia n (%) | Yes | 365 (48.4) | 83 (49.4) | 72 (58.0) | 61 (44.9) | 149 (46.2) | 4.95 | 0.17 |
| No | 389 (51.6) | 88 (50.6) | 52 (42.0) | 75 (55.1) | 174 53.9) | |||
| Cardiovascular Disease, n (%) | Yes | 118 (15.6) | 27 (15.5) | 30 (24.8) | 20 (14.7) | 41 (12.7) | 9.90 | 0.01 * |
| No | 636 (84.3) | 147 (84.5) | 91 (75.2) | 116 (85.3) | 282 87.3) | |||
|
FBS Level n (%) | Controlled | 176 (38.5) | 38 (36.2) | 17 (25.8) | 40 (47.1) | 81 (40.3) | 7.66 | 0.04 * |
| Uncontrolled | 281 (61.5) | 67 (63.8) | 49 (74.2) | 45 (52.9) | 120 (59.7) | |||
|
HbA1c Levels n (%) | Controlled | 65 (8.6) | 10 (5.7) | 9 (7.4) | 13 (9.6) | 33 (10.2) | 3.23 | 0.35 |
| Uncontrolled | 689 (91.4) | 164 (94.3) | 112 (92.6) | 123 (90.4) | 290 (89.8) | |||
| Risk Factors | Univariate Odds Ratio (95% CI) | Multivariate £ Odds Ratio (95% CI) |
|---|---|---|
| Male | 1.11 (0.83–1.48) | 0.82 (0.59–1.16) |
| Two Generations with Diabetes | 1.86 * (1.15–3.02) | 1.96 * (1.12–3.43) |
| In Adequate Physical Activity | 1.40 * (1.03–1.90) | 0.69 * (0.49–0.98) |
| Sugary Beverages | 1.93 * (1.89–1.98) | 1.94 * (1.89–1.99) |
| Sleep Duration > 8 h | 1.58 * (1.04–2.40) | 1.68 * (1.04–2.72) |
| Sleep Duration < 6 h | 1.86 * (1.21–2.85) | 1.84 * (1.14–2.97) |
| Elevated BP | 1.79 * (1.28–1.54) | 1.64 * (1.44–1.94) |
| Stage-I Hypertension | 1.81 * (1.34–1.77) | 1.70 (1.11–1.44) |
| Stage-II Hypertension | 1.78 * (1.03–1.85) | 1.64 (1.09–2.28) |
| Cardiovascular Disease | 1.88 * (1.12–3.16) | 1.38 (0.75–2.50) |
| Uncontrolled FBS | 1.52 * (1.03–2.25) | 0.83 (0.53–1.31) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abbas, E.; Fawwad, A.; Siddiqui, I.A.; Afzal, M.S.; Ansar, M.; Saqib, M.A.N.; Shahid, S.M. Risk Factors for the Development of Early Onset Diabetes in the Population of Sindh Province, Pakistan. Biomedicines 2025, 13, 1107. https://doi.org/10.3390/biomedicines13051107
Abbas E, Fawwad A, Siddiqui IA, Afzal MS, Ansar M, Saqib MAN, Shahid SM. Risk Factors for the Development of Early Onset Diabetes in the Population of Sindh Province, Pakistan. Biomedicines. 2025; 13(5):1107. https://doi.org/10.3390/biomedicines13051107
Chicago/Turabian StyleAbbas, Eraj, Asher Fawwad, Iftikhar Ahmed Siddiqui, Muhammad Sohail Afzal, Muhammad Ansar, Muhammad Arif Nadeem Saqib, and Syed M. Shahid. 2025. "Risk Factors for the Development of Early Onset Diabetes in the Population of Sindh Province, Pakistan" Biomedicines 13, no. 5: 1107. https://doi.org/10.3390/biomedicines13051107
APA StyleAbbas, E., Fawwad, A., Siddiqui, I. A., Afzal, M. S., Ansar, M., Saqib, M. A. N., & Shahid, S. M. (2025). Risk Factors for the Development of Early Onset Diabetes in the Population of Sindh Province, Pakistan. Biomedicines, 13(5), 1107. https://doi.org/10.3390/biomedicines13051107







