The Role of Ubiquitination and Deubiquitination in the Pathogenesis of Acute Kidney Injury: Progress in Research
Abstract
1. Introduction
2. Overview of Ubiquitination and Ubiquitin-like Modifications
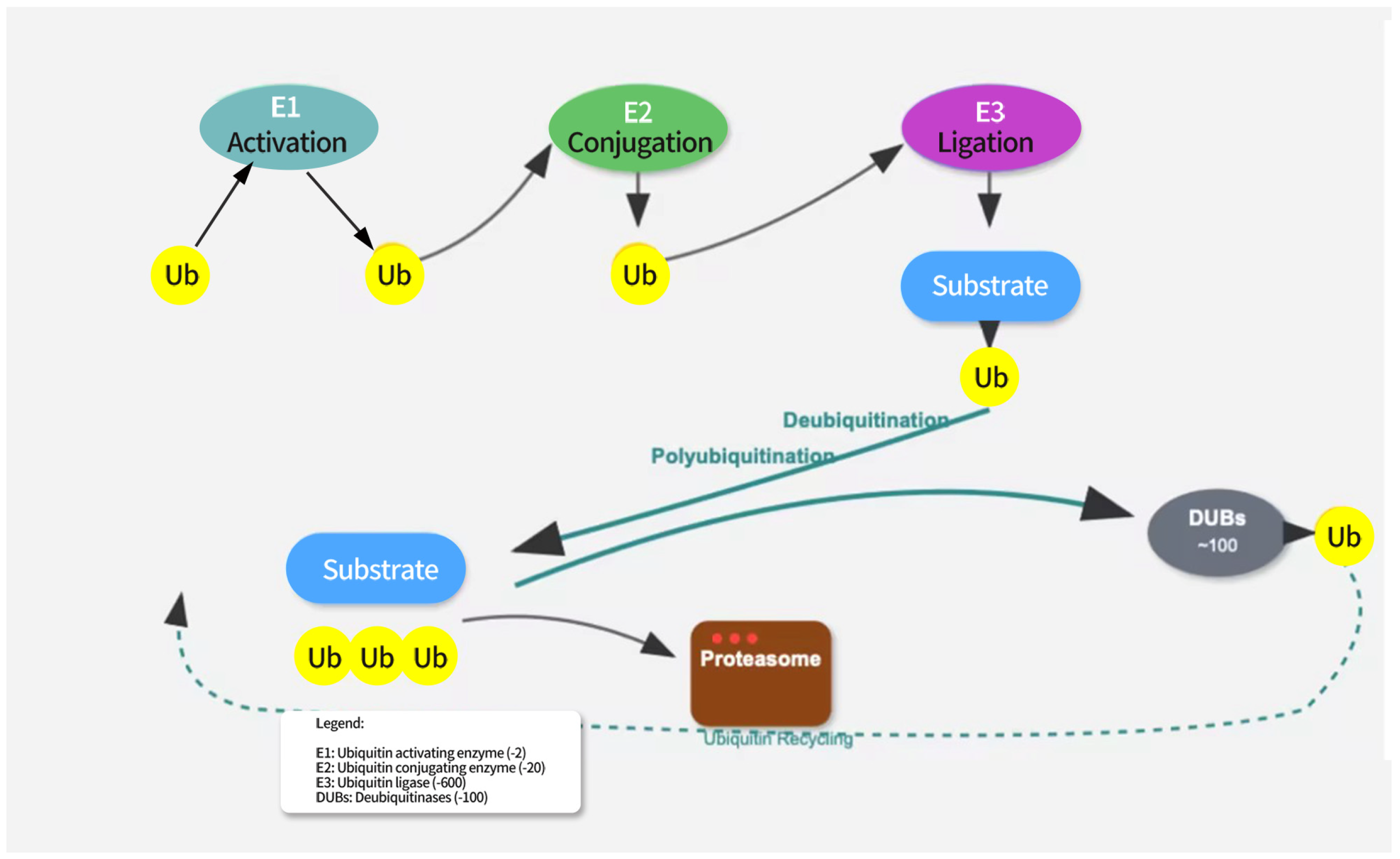
2.1. Mechanism of Ubiquitination
2.2. Deubiquitination
2.3. Ubiquitin-like Modifications, UBLs
2.3.1. SUMOylation
2.3.2. Neddylation
2.3.3. ISGylation
2.3.4. UFMylation
2.3.5. FATylation
2.3.6. Urmylation
3. Role of Ubiquitination and UBLs in the Pathology of AKI
3.1. Integrated Regulatory Networks in AKI
3.2. Ubiquitination and Inflammation: K63 vs. K48 Chain Specificity
3.3. Ubiquitination and Endoplasmic Reticulum Stress (ER Stress)
3.4. Ubiquitination and Apoptosis
3.5. Ubiquitination and Tubular Repair
3.6. Ubiquitination and Mitochondrial Function
4. Deubiquitinating Enzymes (DUBs) in AKI
4.1. DUB-Mediated Inflammation and Cytoprotection
4.2. DUBs Influence Tubular Repair
4.3. DUBs as Potential Therapeutic Targets
5. Spatio-Temporal Dynamics of Ubiquitin Ligases/DUBs in AKI
5.1. Renal Compartment-Specific Dynamics
5.2. Etiology-Specific Dynamics
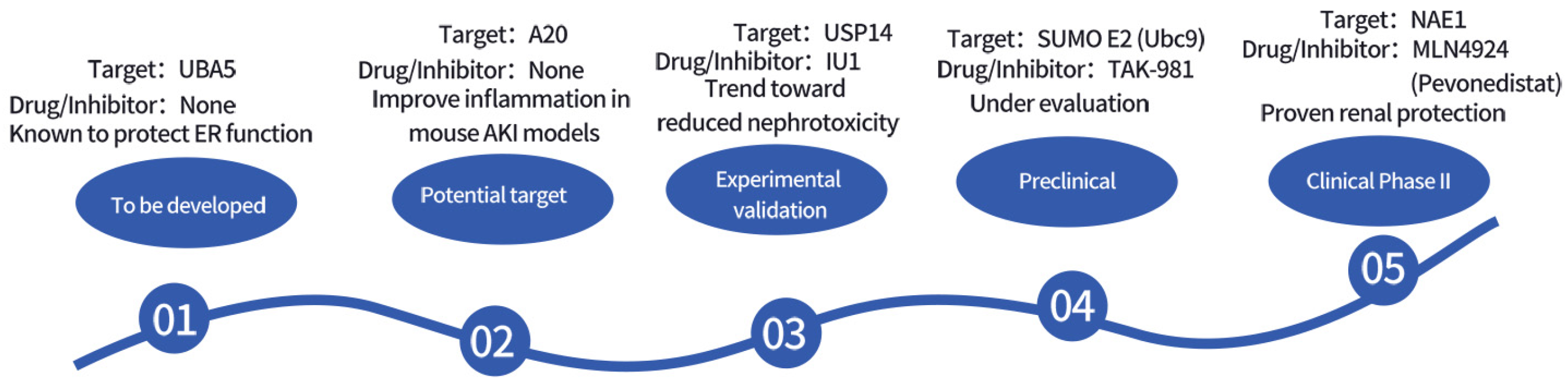
6. Ubiquitination and UBLs as Therapeutic Targets in AKI
6.1. Targeting E3 Ligases for Therapy
6.2. Intervening in AKI with DUBs
6.3. UBLs as Therapeutic Targets
6.4. Multi-Pathway Combined Targeting Strategy
6.5. Future Research Directions
7. Future Research Directions and Translational Challenges
7.1. Specific Testable Research Hypotheses
7.2. Technological Applications: CRISPR-Cas9 and PROTACs in AKI Research
7.3. Translational Challenges and Opportunities
8. Conclusions and Outlook
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AKI | Acute Kidney Injury |
| UPS | Ubiquitin-Proteasome System |
| UBLs | Ubiquitin-Like Modifiers |
| DUBs | Deubiquitinating Enzymes |
| NF-κB | Nuclear Factor-κB |
| NLRP3 | NOD-Like Receptor Pyrin Domain-Containing Protein 3 |
| SUMO | Small Ubiquitin-Like Modifier |
| NEDD8 | Neural Precursor Cell-Expressed Developmentally Downregulated 8 |
| ISG15 | Interferon-Stimulated Gene 15 |
| UFM1 | Ubiquitin-Fold Modifier 1 |
| FAT10 | HLA-F-Adjacent Transcript 10 |
| URM1 | Ubiquitin-Related Modifier 1 |
| USP | Ubiquitin-Specific Proteases |
| OTU | Otubain |
| UCH | Ubiquitin Carboxyl-Terminal Hydrolases |
| JAMM | JAB1/MPN/Mov34 Metalloenzymes |
| SAE | SUMO-Activating Enzyme |
| UBC9 | Ubiquitin-Conjugating Enzyme 9 |
| PIAS | Protein Inhibitor of Activated STAT |
| NAE | NEDD8-Activating Enzyme |
| UBE2M | Ubiquitin-Conjugating Enzyme E2M |
| UBE2F | Ubiquitin-Conjugating Enzyme E2F |
| RBX | RING-Box Protein |
| DCNL | Deneddylase-Like Protein |
| MDM2 | Murine Double Minute 2 |
| UbE1L | Ubiquitin-Activating Enzyme E1-Like |
| UbcH8 | Ubiquitin-Conjugating Enzyme H8 |
| HERC5 | HECT and RLD Domain-Containing E3 Ubiquitin Protein Ligase 5 |
| TRIM25 | Tripartite Motif Containing 25 |
| USP18 | Ubiquitin-Specific Peptidase 18 |
| UBA5 | Ubiquitin-Like Modifier Activating Enzyme 5 |
| UFC1 | UFM1-Conjugating Enzyme 1 |
| UFL1 | UFM1-Specific Ligase 1 |
| UFSP2 | UFM1-Specific Protease 2 |
| ER | Endoplasmic Reticulum |
| UPR | Unfolded Protein Response |
| TNF-α | Tumor Necrosis Factor-α |
| IFN-γ | Interferon-γ |
| UBA6 | Ubiquitin-Activating Enzyme 6 |
| USE1 | Ubiquitin-Conjugating Enzyme E2S1 |
| CKD | Chronic Kidney Disease |
| Wnt | Wingless-Type MMTV Integration Site Family |
| SOD2 | Superoxide Dismutase 2 |
| ROS | Reactive Oxygen Species |
| IRI | Ischemia–Reperfusion Injury |
| ERAD | ER-Associated Degradation |
| Bcl-2 | B-Cell Lymphoma 2 |
| MCL-1 | Myeloid Cell Leukemia 1 |
| Caspase | Cysteinyl Aspartate-Specific Protease |
| USP7 | Ubiquitin-Specific Peptidase 7 |
| CDKs | Cyclin-Dependent Kinases |
| PI3K/AKT | Phosphoinositide 3-Kinase/Protein Kinase B |
| CRLs | Cullin-RING E3 Ubiquitin Ligases |
| PINK1 | PTEN-Induced Kinase 1 |
| NDP52 | Nuclear Dot Protein 52 kDa |
| LC3B | Microtubule-Associated Protein 1 Light Chain 3 Beta |
| OPTN | Optineurin |
| GABARAP | Gamma-Aminobutyric Acid Receptor-Associated Protein |
| p62/SQSTM1 | Sequestosome 1 |
| TRAF6 | TNF Receptor-Associated Factor 6 |
| RIP1 | Receptor-Interacting Protein 1 |
| IκBα | Inhibitor of NF-κB Alpha |
| IKK | IκB Kinase |
| NEMO | NF-κB Essential Modulator |
| FBXL2 | F-Box and Leucine-Rich Repeat Protein 2 |
| TLR4 | Toll-Like Receptor 4 |
| NOX4 | NADPH Oxidase 4 |
| TGFβR1 | Transforming Growth Factor Beta Receptor 1 |
| CYLD | Cylindromatosis |
| USP13 | Ubiquitin-Specific Peptidase 13 |
| USP22 | Ubiquitin-Specific Peptidase 22 |
| SIRT1 | Sirtuin 1 |
| USP14 | Ubiquitin-Specific Peptidase 14 |
| USP9X | Ubiquitin-Specific Peptidase 9 X-Linked |
| USP8 | Ubiquitin-Specific Peptidase 8 |
| EGFR | Epidermal Growth Factor Receptor |
| USP10 | Ubiquitin-Specific Peptidase 10 |
| UCH-L1 | Ubiquitin C-Terminal Hydrolase L1 |
| MLN4924 | Pevonedistat |
| Cbl-b | Casitas B-Lineage Lymphoma Proto-Oncogene B |
| nephrin | Nephrin |
| SCFβ-TrCP | Skp1-Cullin-F-box Beta-Transducin Repeat-Containing Protein |
| Nrf2 | Nuclear Factor Erythroid 2-Related Factor 2 |
| SENPs | SUMO-Specific Proteases |
| HIF-1α | Hypoxia-Inducible Factor 1 Alpha |
| CRISPR-Cas9 | Clustered Regularly Interspaced Short Palindromic Repeats-CRISPR-Associated Protein 9 |
| PROTACs | Proteolysis-Targeting Chimeras |
| AAV | Adeno-Associated Virus |
| UUO | Unilateral Ureteral Obstruction |
| α-SMA | Alpha-Smooth Muscle Actin |
| FOXO4 | Forkhead Box O4 |
References
- Kellum, J.A.; Ronco, C.; Bellomo, R. Conceptual advances and evolving terminology in acute kidney disease. Nat. Rev. Nephrol. 2021, 17, 493–502. [Google Scholar] [CrossRef] [PubMed]
- Kellum, J.A.; Romagnani, P.; Ashuntantang, G.; Ronco, C.; Zarbock, A.; Anders, H.J. Acute kidney injury. Nat. Rev. Dis. Primers 2021, 7, 52. [Google Scholar] [CrossRef] [PubMed]
- Oh, D.J. A long journey for acute kidney injury biomarkers. Ren. Fail. 2020, 42, 154–165. [Google Scholar] [CrossRef] [PubMed]
- Deng, F.; Sharma, I.; Dai, Y.; Yang, M.; Kanwar, Y.S. Myo-inositol oxygenase expression profile modulates pathogenic ferroptosis in the renal proximal tubule. J. Ofclinical Investig. 2019, 129, 5033–5049. [Google Scholar] [CrossRef]
- Deng, F.; Zheng, X.; Sharma, I.; Dai, Y.; Wang, Y.; Kanwar, Y.S. Regulated cell death in cisplatin-induced AKI: Relevance of myo-inositol metabolism. Am. J. Physiol. Physiol. 2021, 320, F578–F595. [Google Scholar] [CrossRef]
- Chen, C.; Qiu, R.; Yang, J.; Zhang, Q.; Sun, G.; Gao, X.; Hei, Z.; Ji, H. Lipoxin A4 Restores Septic Renal Function via Blocking Crosstalk Between Inflammation and Premature Senescence. Front. Immunol. 2021, 12, 637753. [Google Scholar] [CrossRef]
- Yuan, D.; Li, X.; Luo, C.; Li, X.; Cheng, N.; Ji, H.; Qiu, R.; Luo, G.; Chen, C.; Hei, Z. Inhibition of gap junction composed of Cx43prevents against acute kidney injury following liver transplantation. Cell Death Dis. 2019, 10, 767. [Google Scholar] [CrossRef]
- Wu, S.W.; Lee, C.Y.; Lee, S.S.; Chen, W.Y.; Chen, C.J.; Tseng, C.C.; Chiang, C.Y.; Kuan, Y.H. Visnagin mitigates acute kidney injury caused by lipopolysaccharide administration by inhibiting the NF-κB and pyroptosis pathways. Biomed. Pharmacother. 2025, 192, 118578. [Google Scholar] [CrossRef]
- Apriamashvili, G.; Vredevoogd, D.W.; Krijgsman, O.; Bleijerveld, O.B.; Ligtenberg, M.A.; de Bruijn, B.; Boshuizen, J.; Traets, J.J.H.; D’Empaire Altimari, D.; van Vliet, A.; et al. Ubiquitin ligase STUB1 destabilizes IFNγ-receptor complex to suppress tumor IFNγ signaling. Nat. Commun. 2022, 13, 1923. [Google Scholar] [CrossRef]
- Magri, S.; Nanetti, L.; Gellera, C.; Sarto, E.; Rizzo, E.; Mongelli, A.; Ricci, B.; Fancellu, R.; Sambati, L.; Cortelli, P.; et al. Digenic inheritance of STUB1variants and TBP polyglutamine expansions explains the incomplete penetrance of SCA17 and SCA48. Genet. Med. Off. J. Am. Med. Genet. 2022, 24, 29–40. [Google Scholar]
- Mamun, M.M.A.; Khan, M.R.; Zhu, Y.; Zhang, Y.; Zhou, S.; Xu, R.; Bukhari, I.; Thorne, R.F.; Li, J.; Zhang, X.D.; et al. Stub1 maintains proteostasis of master transcription factors in embryonic stem cells. Cell Rep. 2022, 39, 110919. [Google Scholar] [CrossRef] [PubMed]
- Kodroń, A.; Mussulini, B.H.; Pilecka, I.; Chacińska, A. The ubiquitin-proteasome system and its crosstalk with mitochondria as therapeutic targets in medicine. Pharmacol. Res. 2021, 163, 105248. [Google Scholar] [CrossRef]
- Zhang, Z.; Yue, P.; Lu, T.; Wang, Y.; Wei, Y.; Wei, X. Role of lysosomes in physiological activities, diseases, and therapy. J. Hematol. Oncol. 2021, 14, 79. [Google Scholar] [CrossRef]
- Goodall, E.A.; Kraus, F.; Harper, J.W. Mechanisms underlying ubiquitin-driven selective mitochondrial and bacterial autophagy. Mol. Cell 2022, 82, 1501–1513. [Google Scholar] [CrossRef]
- Toma-Fukai, S.; Shimizu, T. Structural diversity of ubiquitin E3 ligase. Molecules 2021, 26, 6682. [Google Scholar] [CrossRef]
- Gwon, Y.; Maxwell, B.A.; Kolaitis, R.M.; Zhang, P.; Kim, H.J.; Taylor, J.P. Ubiquitination of G3BP1 mediates stress granule disassembly in a context-specific manner. Science 2021, 372, eabf6548. [Google Scholar] [CrossRef]
- French, M.E.; Koehler, C.F.; Hunter, T. Emerging functions of branched ubiquitin chains. Cell Discov. 2021, 7, 6. [Google Scholar] [CrossRef]
- Horn-Ghetko, D.; Krist, D.T.; Prabu, J.R.; Baek, K.; Mulder, M.P.C.; Klügel, M.; Scott, D.C.; Ovaa, H.; Kleiger, G.; Schulman, B.A. Ubiquitin ligation to F-box protein targets by SCF–RBR E3–E3 super-assembly. Nature 2021, 590, 671–676. [Google Scholar] [CrossRef]
- Hanpanich, O.; Maruyama, A. Artificial chaperones: From materials designs to applications. Biomaterials 2020, 254, 120150. [Google Scholar] [CrossRef] [PubMed]
- Bard, J.A.M.; Goodall, E.A.; Greene, E.R.; Jonsson, E.; Dong, K.C.; Martin, A. Structure and Function of the 26S Proteasome. Annu. Rev. Biochem. 2018, 87, 697–724. [Google Scholar] [CrossRef] [PubMed]
- Kolla, S.D.D.; Ye, M.; Mark, K.G.; Rapé, M. Assembly and function of branched ubiquitin chains. Trends Biochem. Sci. 2022, 47, 759–771. [Google Scholar] [CrossRef] [PubMed]
- Pohl, C.; Dikic, I. Cellular quality control by the ubiquitin-proteasome system and autophagy. Science 2019, 366, 818–822. [Google Scholar] [CrossRef] [PubMed]
- Patwa, N.; Deep, S. Role of molecular and chemical chaperon in assisting refolding of BMP2 in E. coli. Int. J. Biol. 2022, 220, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Snyder, N.A.; Silva, G.M. Deubiquitinating enzymes (DUBs): Regulation, homeostasis, and oxidative stress response. J. Biol. Chem. 2021, 297, 101077. [Google Scholar] [CrossRef]
- Liu, B.; Ruan, J.; Chen, M.; Li, Z.; Manjengwa, G.; Schlüter, D.; Song, W.; Wang, X. Deubiquitinating enzymes (DUBs): Decipher underlying basis of neurodegenerative diseases. Mol. Psychiatry 2022, 27, 259–268. [Google Scholar] [CrossRef]
- Jolly, L.A.; Kumar, R.; Penzes, P.; Piper, M.; Gecz, J. The DUB club: Deubiquitinating enzymes and neurodevelopmental disorders. Biol. Psychiatry 2022, 92, 614–625. [Google Scholar] [CrossRef]
- Fang, Y.Z.; Jiang, L.; He, Q.; Cao, J.; Yang, B. Deubiquitination complex platform: A plausible mechanism for regulating the substrate specificity of deubiquitinating enzymes. Acta Pharm. Sin. B 2023, 13, 2955–2962. [Google Scholar] [CrossRef]
- Elu, N.; Osinalde, N.; Ramirez, J.; Presa, N.; Rodriguez, J.A.; Prieto, G.; Mayor, U. Identification of substrates for human deubiquitinating enzymes (DUBs): An up-to-date review and a case study for neurodevelopmental disorders. Semin. Cell Dev. Biol. 2022, 132, 120–131. [Google Scholar] [CrossRef]
- Trulsson, F.; Akimov, V.; Robu, M.; van Overbeek, N.; Berrocal, D.A.P.; Shah, R.G.; Cox, J.; Shah, G.M.; Blagoev, B.; Vertegaal, A.C.O. Deubiquitinating enzymes and the proteasome regulate preferential sets of ubiquitin substrates. Nat. Commun. 2022, 13, 2736. [Google Scholar] [CrossRef]
- Liu, F.; Chen, J.; Li, K.; Li, H.; Zhu, Y.; Zhai, Y.; Lu, B.; Fan, Y.; Liu, Z.; Chen, X.; et al. Ubiquitination and deubiquitination in cancer: From mechanisms to novel therapeutic approaches. Mol. Cancer 2024, 23, 148. [Google Scholar] [CrossRef]
- Ge, F.; Li, Y.; Yuan, T.; Wu, Y.; He, Q.; Yang, B.; Zhu, H. Deubiquitinating enzymes: Promising targets for drug resistance. Drug Discov. Today 2022, 27, 2603–2613. [Google Scholar] [CrossRef] [PubMed]
- Qin, B.; Chen, X.; Wang, F.; Wang, Y. DUBs in Alzheimer’s disease: Mechanisms and therapeutic implications. Cell Death Discov. 2024, 10, 475. [Google Scholar] [CrossRef] [PubMed]
- Dagar, G.; Kumar, R.; Yadav, K.K.; Singh, M.; Pandita, T.K. Ubiquitination and deubiquitination: Implications on cancer therapy. Biochim. Biophys. Acta (BBA)-Gene Regul. Mech. 2023, 1866, 194979. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Ma, Y.; Zhang, T.; Liu, R.; Chang, F.; Yan, X.; Yu, T.; Wu, P.; Li, Q.; Xu, L.; et al. The deubiquitinating enzyme USP4 regulates BRCA1 stability and function. npj Breast Cancer 2024, 1, 35. [Google Scholar] [CrossRef]
- Hromas, R.; Srinivasan, G.; Yang, M.; Jaiswal, A.; Totterdale, T.A.; Phillips, L.; Kirby, A.; Khodayari, N.; Brantley, M.; Williamson, E.A.; et al. BRCA1 mediates protein homeostasis through the ubiquitination of PERK and IRE1. iScience 2022, 25, 105626. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Inagi, R.; Ishimoto, Y.; Nangaku, M. Proteostasis in endoplasmic reticulum—New mechanisms in kidney disease. Nat. Rev. Nephrol. 2014, 10, 369–378. [Google Scholar] [CrossRef]
- Jiang, X.; Chen, Z.J. The role of ubiquitylation in immune defence and pathogen evasion. Nat. Rev. Immunol. 2011, 12, 35–48. [Google Scholar] [CrossRef]
- Liao, Y.; Yang, M.; Wang, K.; Wang, Y.; Zhong, B.; Jiang, N. Deubiquitinating enzyme OTUB1 in immunity and cancer: Good player or bad actor? Cancer Lett. 2022, 526, 248–258. [Google Scholar] [CrossRef]
- Karin, M.; Ben-Neriah, Y. Phosphorylation meets ubiquitination: The control of NF-κB activity. Annu. Rev. Immunol. 2000, 18, 621–663. [Google Scholar] [CrossRef]
- Kategaya, L.; Di Lello, P.; Rougé, L.; Pastor, R.; Clark, K.R.; Drummond, J.; Kleinheinz, T.; Lin, E.; Upton, J.P.; Prakash, S.; et al. USP7 small-molecule inhibitors interfere with ubiquitin binding. Nature 2017, 550, 534–538. [Google Scholar] [CrossRef]
- Kawakami, T.; Ren, S.; Duffield, J.S. Wnt signalling in kidney diseases: Dual roles in renal injury and repair. J. Pathol. 2013, 229, 221–231. [Google Scholar] [CrossRef]
- Ma, X.-N.; Li, M.-Y.; Qi, G.-Q.; Wei, L.-N.; Zhang, D.-K. SUMOylation at the crossroads of gut health: Insights into physiology and pathology. Cell Commun. Signal. 2024, 22, 404. [Google Scholar] [CrossRef] [PubMed]
- Celen, A.B.; Sahin, U. Sumoylation on its 25th anniversary: Mechanisms, pathology, and emerging concepts. FEBS J. 2020, 287, 3110–3140. [Google Scholar] [CrossRef] [PubMed]
- Chatzikalil, E.; Arvanitakis, K.; Filippatos, F.; Diamantopoulos, P.T.; Koufakis, T. Diagnostic and therapeutic implications of the SUMOylation pathway in acute myeloid leukemia. Cancers 2023, 17, 631. [Google Scholar] [CrossRef]
- Lu, J.; Zhang, X.; Wu, Y.; Sheng, Y.; Li, W.; Wang, W. Energy landscape remodeling mechanism of Hsp70-chaperone-accelerated protein folding. Biophys. J. 2021, 120, 1971–1983. [Google Scholar] [CrossRef] [PubMed]
- Burslem, G.M.; Crews, C.M. Proteolysis-targeting chimeras as therapeutics and tools for biological discovery. Cell 2020, 181, 102–114. [Google Scholar] [CrossRef]
- Zhang, S.; Yu, Q.; Li, Z.; Zhao, Y.; Sun, Y. Protein neddylation and its role in health and diseases. Signal Transduct. Target. Ther. 2024, 9, 85. [Google Scholar] [CrossRef]
- Fu, Z.; Liao, W.; Ma, H.; Wang, Z.; Jiang, M.; Feng, X.; Zhang, W. Inhibition of neddylation plays protective role in lipopolysaccharide-induced kidney damage through CRL-mediated NF-κB pathways. Am. J. Transl. Res. 2019, 11, 2830. [Google Scholar]
- Galluzzi, L.; Vitale, I.; Aaronson, S.A.; Abrams, J.M.; Adam, D.; Agostinis, P.; Alnemri, E.S.; Altucci, L.; Amelio, I.; Andrews, D.W.; et al. Molecular mechanisms of cell death: Recommendations of the Nomenclature Committee on Cell Death 2018. Cell Death Differ. 2018, 25, 486–541. [Google Scholar] [CrossRef]
- Pu, Z.; Shen, C.; Zhang, W.; Xie, H.; Wang, W. Avenanthramide C from oats protects pyroptosis through dependent ROS-induced mitochondrial damage by PI3K ubiquitination and phosphorylation in pediatric pneumonia. J. Agric. Food Chem. 2022, 70, 2339–2353. [Google Scholar] [CrossRef]
- Rabb, H.; Griffin, M.D.; McKay, D.B.; Swaminathan, S.; Pickkers, P.; Rosner, M.H.; Kellum, J.A.; Ronco, C.; Acute Dialysis Quality Initiative Consensus XIII Work Group. Inflammation in AKI: Current understanding, key questions, and knowledge gaps. J. Am. Soc. Nephrol. 2016, 27, 371–379. [Google Scholar] [CrossRef] [PubMed]
- Kanarek, N.; Ben-Neriah, Y. Regulation of NF-κB by ubiquitination and degradation of the IκBs. Immunol. Rev. 2012, 246, 77–94. [Google Scholar] [CrossRef] [PubMed]
- Akizuki, Y.; Kaypee, S.; Ohtake, F.; Ikeda, F. The emerging roles of non-canonical ubiquitination in proteostasis and beyond. J. Cell Biol. 2024, 223, e202311171. [Google Scholar] [CrossRef]
- Gao, Y.; Lu, X.; Zhang, G.; Liu, C.; Sun, S.; Mao, W.; Jiang, G.; Zhou, Y.; Zhang, N.; Tao, S.; et al. DRD4 alleviates acute kidney injury by suppressing ISG15/NOX4 axis-associated oxidative stress. Redox Biol. 2024, 70, 103078. [Google Scholar] [CrossRef]
- Cui, N.; Liu, C.; Tang, X.; Song, L.; Xiao, Z.; Wang, C.; Wu, Y.; Zhou, Y.; Peng, C.; Liu, Y.; et al. ISG15 accelerates acute kidney injury and the subsequent AKI-to-CKD transition by promoting TGFβR1 ISGylation. Theranostics 2024, 14, 4536–4553. [Google Scholar] [CrossRef]
- Tandra, V.; Anderson, T.; Ayala, J.D.; Weintraub, N.L.; Singh, N.; Li, H.; Li, J. Ufmylation of UFBP1 Is Dispensable for Endoplasmic Reticulum Stress Response, Embryonic Development, and Cardiac and Intestinal Homeostasis. Cells 2023, 12, 1923. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, Y.; Zhang, M.; Wu, J.; Lei, G.; Li, H. Transcriptional Regulation of the Ufm1 Conjugation System in Response to Disturbance of the Endoplasmic Reticulum Homeostasis and Inhibition of Vesicle Trafficking. PLoS ONE 2012, 7, e48587. [Google Scholar] [CrossRef]
- Shao, Y.; Zhang, W.; Du, D.; Yu, Y.; Li, Q.; Peng, X. Ubiquitin-like protein FAT10 promotes renal fibrosis by stabilizing USP7 to prolong CHK1-mediated G2/M arrest in renal tubular epithelial cells. Aging 2022, 14, 7527–7546. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhou, T.; Yang, X.; Chen, Z.; Yang, Y.; Wang, X.; Cao, X.; Chen, C.; Han, C.; Tian, H.; Qin, A.; et al. Prussian blue nanoparticles stabilize SOD1 from ubiquitination-proteasome degradation to rescue intervertebral disc degeneration. Adv. Sci. 2022, 9, 2105466. [Google Scholar] [CrossRef]
- Sun, S.; Hou, H.; Ma, G.; Ma, Q.; Li, N.; Zhang, L.; Dong, C.; Cao, M.; Tam, K.Y.; Ying, Z.; et al. The interaction between E3 ubiquitin ligase Parkin and mitophagy receptor PHB2 links inner mitochondrial membrane ubiquitination to efficient mitophagy. J. Biol. Chem. 2022, 298, 102704. [Google Scholar] [CrossRef]
- Oshima, Y.; Cartier, E.; Boyman, L.; Verhoeven, N.; Polster, B.M.; Huang, W.; Kane, M.; Lederer, W.J.; Karbowski, M. Parkin-independent mitophagy via Drp1-mediated outer membrane severing and inner membrane ubiquitination. J. Cell Biol. 2021, 220, e202006043. [Google Scholar] [CrossRef]
- Hou, J.; Deng, Q.; Deng, X.; Zhong, W.; Liu, S.; Zhong, Z. MicroRNA-146a-5p alleviates lipopolysaccharide-induced NLRP3 inflammasome injury and pro-inflammatory cytokine production via the regulation of TRAF6 and IRAK1 in human umbilical vein endothelial cells (HUVECs). Ann. Transl. Med. 2021, 9, 1433. [Google Scholar] [CrossRef]
- Chen, Y.; Zhang, C.; Du, Y.; Yang, X.; Liu, M.; Yang, W.; Lei, G.; Wang, G. Exosomal transfer of microRNA-590-3p between renal tubular epithelial cells after renal ischemia-reperfusion injury regulates autophagy by targeting TRAF6. Chin. Med. J. 2022, 135, 2467–2477. [Google Scholar] [CrossRef]
- Boughton, A.J.; Krueger, S.; Fushman, D. Branching via K11 and K48 bestows ubiquitin chains with a unique interdomain interface and enhanced affinity for proteasomal subunit Rpn1. Structure 2020, 28, 29–43.e6. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Li, S.; Wu, H. Ubiquitination-Proteasome System (UPS) and Autophagy Two Main Protein Degradation Machineries in Response to Cell Stress. Cells 2022, 11, 851. [Google Scholar] [CrossRef] [PubMed]
- Wan, X.; Fan, L.; Hu, B.; Yang, J.; Li, X.; Chen, X.; Cao, C. Small interfering RNA targeting IKKβ prevents renal ischemia-reperfusion injury in rats. Am. J. Physiol.-Ren. Physiol. 2011, 300, F857–F863. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Hu, Y.; Huang, P.; Toleman, C.A.; Paterson, A.J.; Kudlow, J.E. Proteasome function is regulated by cyclic AMP-dependent protein kinase through phosphorylation of Rpt6. J. Biol. Chem. 2014, 282, 22460–22471. [Google Scholar] [CrossRef]
- Çetin, G.; Klafack, S.; Studencka-Turski, M.; Krüger, E.; Ebstein, F. The ubiquitin–proteasome system in immune cells. Biomolecules 2021, 11, 60. [Google Scholar] [CrossRef]
- Guo, C.; Dong, G.; Liang, X.; Dong, Z. Epigenetic regulation in AKI and kidney repair: Mechanisms and therapeutic implications. Nat. Rev. Nephrol. 2017, 13, 580–595. [Google Scholar] [CrossRef]
- Py, B.F.; Kim, M.S.; Vakifahmetoglu-Norberg, H.; Yuan, J. Deubiquitination of NLRP3 by BRCC3 critically regulates inflammasome activity. Mol. Cell 2013, 49, 331–338. [Google Scholar] [CrossRef]
- Han, S.; Jerome, J.A.; Gregory, A.D.; Mallampalli, R.K. Cigarette smoke destabilizes NLRP3 protein by promoting its ubiquitination. Respir. Res. 2015, 16, 2. [Google Scholar] [CrossRef] [PubMed]
- Jefferies, C.A. Regulating IRFs in IFN Driven Disease. Front. Immunol. 2019, 10, 325. [Google Scholar] [CrossRef] [PubMed]
- Perng, Y.C.; Lenschow, D.J. ISG15 in antiviral immunity and beyond. Nat. Rev. Microbiol. 2018, 16, 423–439. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Chen, X.; Shao, Y.; Deng, S.; Wang, C.; Chen, J.; Xie, Y.; Yuan, S.; Tang, L. Elevation of ISG15 promotes diabetic kidney disease by modulating renal tubular epithelial cell pyroptosis. Clin. Transl. Med. 2025, 15, e70337. [Google Scholar] [CrossRef]
- Sulkshane, P.; Ram, J.; Thakur, A.; Reis, N.; Kleifeld, O.; Glickman, M.H. Ubiquitination and receptor-mediated mitophagy converge to eliminate oxidation-damaged mitochondria during hypoxia. Redox Biol. 2021, 45, 102047. [Google Scholar] [CrossRef]
- Li, Z.; Liu, Z.; Luo, M.; Li, X.; Chen, H.; Gong, S.; Zhang, M.; Zhang, Y.; Liu, H.; Li, X. The pathological role of damaged organelles in renal tubular epithelial cells in the progression of acute kidney injury. Cell Death Discov. 2022, 8, 239. [Google Scholar] [CrossRef]
- Keuss, M.J.; Hjerpe, R.; Hsia, O.; Gourlay, R.; Burchmore, R.; Trost, M.; Kurz, T. Unanchored tri-NEDD8 inhibits PARP-1 to protect from oxidative stress-induced cell death. EMBO J. 2019, 38, e100024. [Google Scholar] [CrossRef]
- Tang, D.; Kang, R.; Berghe, T.V.; Vandenabeele, P.; Kroemer, G. The molecular machinery of regulated cell death. Cell Res. 2019, 29, 347–364. [Google Scholar] [CrossRef]
- Cui, Z.; Kang, H.; Grandis, J.R.; Johnson, D.E. CYLD Alterations in the Tumorigenesis and Progression of Human Papillomavirus–Associated Head and Neck Cancers. Mol. Cancer Res. 2021, 19, 14–24. [Google Scholar] [CrossRef]
- Bufalieri, F.; Lospinoso Severini, L.; Caimano, M.; Infante, P.; Di Marcotullio, L. DUBs Activating the Hedgehog Signaling Pathway: A Promising Therapeutic Target in Cancer. Cancers 2020, 12, 1518. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, Y.; Cai, J.; Tang, C.; Dong, Z. Mitophagy in acute kidney injury and kidney repair. Cells 2020, 9, 338. [Google Scholar] [CrossRef]
- Guo, C.; Wei, Q.; Su, Y.; Dong, Z. SUMOylation occurs in acute kidney injury and plays a cytoprotective role. Biochim. Biophys. Acta. 2015, 1852, 482–489. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Xie, H.; Wang, Y.; Zhang, H.; Fan, Q.; Dai, D. Tubular epithelial C1orf54 mediates protection and recovery from acute kidney injury. J. Cell. Mol. Med. 2021, 25, 4759–4770. [Google Scholar] [CrossRef]
- Buetow, L.; Huang, D.T. Structural insights into the catalysis and regulation of E3 ubiquitin ligases. Nat. Rev. Mol. Cell Biol. 2016, 17, 626–642. [Google Scholar] [CrossRef] [PubMed]
- Kwon, Y.T.; Ciechanover, A. The Ubiquitin Code in the Ubiquitin-Proteasome System and Autophagy. Trends Biochem. Sci. 2017, 42, 873–886. [Google Scholar] [CrossRef] [PubMed]
- Karbowski, M.; Oshima, Y.; Verhoeven, N. Mitochondrial proteotoxicity: Implications and ubiquitin-dependent quality control mechanisms. Cell. Mol. Life Sci. 2022, 79, 574. [Google Scholar] [CrossRef] [PubMed]
- Seo, B.A.; Kim, D.; Hwang, H.; Kim, M.S.; Ma, S.X.; Kwon, S.H.; Kweon, S.H.; Wang, H.; Yoo, J.M.; Choi, S.; et al. TRIP12 ubiquitination of glucocerebrosidase contributes to neurodegeneration in Parkinson’s disease. Neuron 2021, 109, 3758–3774.e11. [Google Scholar] [CrossRef]
- Zhou, Q.; Zheng, Y.; Sun, Y. Neddylation regulation of mitochondrial structure and functions. Cell Biosci. 2021, 11, 55. [Google Scholar] [CrossRef]
- Zeng, S.; Zhao, Z.; Zheng, S.; Wu, M.; Song, X.; Li, Y.; Zheng, Y.; Liu, B.; Chen, L.; Gao, C.; et al. The E3 ubiquitin ligase TRIM31 is involved in cerebral ischemic injury by promoting degradation of TIGAR. Redox Biol. 2021, 45, 102058. [Google Scholar] [CrossRef]
- Sun, Y.; Yang, Y.M.; Hu, Y.Y.; Ouyang, L.; Sun, Z.H.; Yin, X.F.; Li, N.; He, Q.Y.; Wang, Y. Inhibition of nuclear deacetylase Sirtuin-1 induces mitochondrial acetylation and calcium overload leading to cell death. Redox Biol. 2022, 53, 102334. [Google Scholar] [CrossRef]
- Cao, Y.; Zheng, J.; Wan, H.; Sun, Y.; Fu, S.; Liu, S.; He, B.; Cai, G.; Cao, Y.; Huang, H.; et al. A mitochondrial SCF-FBXL4 ubiquitin E3 ligase complex degrades BNIP3 and NIX to restrain mitophagy and prevent mitochondrial disease. EMBO J. 2023, 42, e113033. [Google Scholar] [CrossRef]
- Harrigan, J.A.; Jacq, X.; Martin, N.M.; Jackson, S.P. Deubiquitylating enzymes and drug discovery: Emerging opportunities. Nat. Rev. Drug Discov. 2018, 17, 57–78. [Google Scholar] [CrossRef]
- Abdul Rehman, S.A.; Kristariyanto, Y.A.; Choi, S.Y.; Nkosi, P.J.; Weidlich, S.; Labib, K.; Hofmann, K.; Kulathu, Y. MINDY-1 Is a Member of an Evolutionarily Conserved and Structurally Distinct New Family of Deubiquitinating Enzymes. Mol. Cell 2016, 63, 146–155. [Google Scholar] [CrossRef] [PubMed]
- Rogers, N.M.; Zammit, N.; Nguyen-Ngo, D.; Souilmi, Y.; Minhas, N.; Meijles, D.N.; Self, E.; Walters, S.N.; Warren, J.; Cultrone, D.; et al. The impact of the cytoplasmic ubiquitin ligase TNFAIP3 gene variation on transcription factor NF-κB activation in acute kidney injury. Kidney Int. 2023, 103, 1105–1119. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Mooney, E.C.; Holden, S.E.; Xia, X.J.; Cohen, D.J.; Walsh, S.W.; Ma, A.; Sahingur, S.E. A20 Orchestrates Inflammatory Response in the Oral Mucosa through Restraining NF-κB Activity. J. Immunol. 2019, 202, 2044–2056. [Google Scholar] [CrossRef]
- Jiang, W.; Deng, M.; Gan, C.; Wang, L.; Mao, H.; Li, Q. A novel missense mutation in TNFAIP3 causes haploinsufficiency of A20. Cell. Immunol. 2022, 371, 104453. [Google Scholar] [CrossRef]
- Ke, B.; Shen, X.D.; Ji, H.; Kamo, N.; Gao, F.; Freitas, M.C.; Busuttil, R.W.; Kupiec-Weglinski, J.W. HO-1-STAT3 axis in mouse liver ischemia/reperfusion injury: Regulation of TLR4 innate responses through PI3K/PTEN signaling. J. Immunol. 2013, 190, 4981–4991. [Google Scholar] [CrossRef]
- Huang, Z.; Tan, Y. The potential of cylindromatosis (CYLD) as a therapeutic target in oxidative stress-associated pathologies: A comprehensive evaluation. Int. J. Mol. Sci. 2023, 24, 8368. [Google Scholar] [CrossRef]
- Thuillier, R.; Dutheil, D.; Trieu, M.T.; Mallet, V.; Allain, G.; Rousselot, M.; Denizot, M.; Goujon, J.M.; Zal, F.; Hauet, T. Supplementation with a new therapeutic oxygen carrier reduces chronic fibrosis and organ dysfunction in kidney static preservation. Am. J. Transplant. 2017, 11, 1845–1860. [Google Scholar] [CrossRef]
- Wang, Q.; Cao, S.; Sun, Z.; Zhu, W.; Sun, L.; Li, Y.; Luo, D.; Huang, S.; Zhang, Y.; Xia, W.; et al. USP13 inhibition exacerbates mitochondrial dysfunction and acute kidney injury by acting on MCL-1. Biochim. Biophys. Acta (BBA)-Mol. Basis Dis. 2025, 1871, 167599. [Google Scholar] [CrossRef]
- Liu, J.; Livingston, M.J.; Dong, G.; Tang, C.; Su, Y.; Wu, G.; Yin, X.M.; Dong, Z. Histone deacetylase inhibitors protect against cisplatin-induced acute kidney injury by activating autophagy in proximal tubular cells. Cell Death Dis. 2018, 9, 322. [Google Scholar] [CrossRef]
- Yuan, J.; Zhang, Y.; Sheng, Y.; Fu, X.; Cheng, H.; Zhou, R. MYBL2 guides autophagy suppressor VDAC2 in the developing ovary to inhibit autophagy through a complex of VDAC2-BECN1-BCL2L1 in mammals. Mol. Cell 2015, 58, 989–1001. [Google Scholar] [CrossRef]
- Kabuta, T.; Mitsui, T.; Takahashi, M.; Fujiwara, Y.; Kabuta, C.; Konya, C.; Tsuchiya, Y.; Hatanaka, Y.; Uchida, K.; Hohjoh, H.; et al. Ubiquitin C-terminal Hydrolase L1 (UCH-L1) Acts as a Novel Potentiator of Cyclin-dependent Kinases to Enhance Cell Proliferation Independently of Its Hydrolase Activity. J. Biol. Chem. 2013, 288, 12615–12626. [Google Scholar] [CrossRef] [PubMed]
- Duff, S.; Irwin, R.; Cote, J.M.; Redahan, L.; McMahon, B.A.; Marsh, B.; Nichol, A.; Holden, S.; Doran, P.; Murray, P.T. Urinary biomarkers predict progression and adverse outcomes of acute kidney injury in critical illness. Nephrol. Dial. Transplant. 2022, 37, 1668–1678. [Google Scholar] [CrossRef] [PubMed]
- Mulay, S.R.; Thomasova, D.; Ryu, M.; Anders, H.J. MDM2 (murine double minute-2) links inflammation and tubular cell healing during acute kidney injury in mice. Kidney Int. 2012, 81, 1199–1211. [Google Scholar] [CrossRef] [PubMed]
- Lu, D.; Zhang, Y.; Zhu, P.; Wu, J.; Yuan, C.; Ni, L. The roles of the ubiquitin-proteasome system in renal disease. Int. J. Med. Sci. 2025, 22, 1791–1810. [Google Scholar] [CrossRef]
- Pontrelli, P.; Oranger, A.; Barozzino, M.; Divella, C.; Conserva, F.; Fiore, M.G.; Rossi, R.; Papale, M.; Castellano, G.; Simone, S.; et al. Deregulation of autophagy under hyperglycemic conditions is dependent on increased lysine 63 ubiquitination: A candidate mechanism in the progression of diabetic nephropathy. J. Mol. Med. 2018, 96, 645–659. [Google Scholar] [CrossRef]
- Kwasna, D.; Abdul Rehman, S.A.; Natarajan, J.; Matthews, S.; Madden, R.; De Cesare, V.; Weidlich, S.; Virdee, S.; Ahel, I.; Gibbs-Seymour, I.; et al. Discovery and Characterization of ZUFSP/ZUP1, a Distinct Deubiquitinase Class Important for Genome Stability. Mol. Cell 2018, 70, 150–164.e156. [Google Scholar] [CrossRef]
- Hughes, M.A.; Powley, I.R.; Jukes-Jones, R.; Horn, S.; Feoktistova, M.; Fairall, L.; Schwabe, J.W.; Leverkus, M.; Cain, K.; MacFarlane, M. Co-operative and Hierarchical Binding of c-FLIP and Caspase-8: A Unified Model Defines How c-FLIP Isoforms Differentially Control Cell Fate. Mol. Cell 2016, 61, 834–849. [Google Scholar] [CrossRef]
- Hsu, T.S.; Mo, S.T.; Hsu, P.N.; Lai, M.Z. c-FLIP is a target of the E3 ligase deltex1 in gastric cancer. Cell Death Dis. 2018, 9, 135. [Google Scholar] [CrossRef]
- Yao, D.; Zhang, S.; Hu, Z.; Luo, H.; Mao, C.; Fan, Y.; Tang, M.; Liu, F.; Shen, S.; Fan, L.; et al. CHIP ameliorates cerebral ischemia-reperfusion injury by attenuating necroptosis and inflammation. Aging 2021, 13, 25564–25577. [Google Scholar] [CrossRef]
- Sinha, S.; Dwivedi, N.; Woodgett, J.; Tao, S.; Howard, C.; Fields, T.A.; Jamadar, A.; Rao, R. Glycogen synthase kinase-3β inhibits tubular regeneration in acute kidney injury by a FoxM1-dependent mechanism. FASEB J. 2020, 34, 13597–13608. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zheng, W.; Guan, F.; Xu, G.; Yu, Y.; Xiao, J.; Huang, X. FAT10 Silencing Prevents Liver Fibrosis through Regulating SIRT1 Expression in Hepatic Stellate Cells. Int. J. Med. Sci. 2023, 20, 557–565. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kim, E.Y.; Ner-Gaon, H.; Park, J.; Jeong, M.; Lee, S.; Baek, K.H. Post-transcriptional regulation of MFG-E8 by SENP1-mediated sumoylation contributes to apoptotic cell clearance. Mol. Cell. Biol. 2017, 37, e00527-16. [Google Scholar]
- Ma, A.G.; Yu, L.M.; Zhao, H.; Qin, C.W.; Tian, X.Y.; Wang, Q. PSMD4 regulates the malignancy of esophageal cancer cells by suppressing endoplasmic reticulum stress. J. Exp. Clin. Cancer Res. 2019, 38, 591–597. [Google Scholar] [CrossRef] [PubMed]
- Zhao, C.; Collins, M.N.; Hsiang, T.Y.; Krug, R.M. Interferon-induced ISG15 pathway: An ongoing virus-host battle. Trends Microbiol. 2016, 21, 181–186. [Google Scholar] [CrossRef]
- Hundley, F.V.; Sanvisens Delgado, N.; Marin, H.C.; Carr, K.L.; Tian, R.; Toczyski, D.P. A comprehensive phenotypic CRISPR-Cas9 screen of the ubiquitin pathway uncovers roles of ubiquitin ligases in mitosis. Mol. Cell 2021, 81, 1319–1336.e9. [Google Scholar] [CrossRef]
- Tyagi, A.; Kaushal, K.; Chandrasekaran, A.P.; Sarodaya, N.; Das, S.; Park, C.H.; Hong, S.H.; Kim, K.S.; Ramakrishna, S. CRISPR/Cas9-based genome-wide screening for deubiquitinase subfamily identifies USP1 regulating MAST1-driven cisplatin-resistance in cancer cells. Theranostics 2022, 12, 5949. [Google Scholar] [CrossRef]
- Kaushal, K.; Kim, E.J.; Tyagi, A.; Karapurkar, J.K.; Haq, S.; Jung, H.S.; Kim, K.S.; Ramakrishna, S. Genome-wide screening for deubiquitinase subfamily identifies ubiquitin-specific protease 49 as a novel regulator of odontogenesis. Cell Death Differ. 2022, 29, 1689–1704. [Google Scholar] [CrossRef]
- Inns, J. The Role of E3 Ubiquitin-Protein Ligase DTX3L in the Innate Immune Response. Ph.D. Thesis, Newcastle University, Newcastle upon Tyne, UK, 2023. [Google Scholar]
- Gong, S.; Xiong, H.; Lei, Y.; Huang, S.; Ouyang, Y.; Cao, C.; Wang, Y. Usp9x contributes to the development of sepsis-induced acute kidney injury by promoting inflammation and apoptosis in renal tubular epithelial cells via activation of the TLR4/nf-κb pathway. Ren. Fail. 2024, 46, 2361089. [Google Scholar] [CrossRef]
- Delrue, C.; Speeckaert, M.M. Renal Implications of Dysregulated Protein Homeostasis: Insights into Ubiquitin–Proteasome and Autophagy Systems. Biomolecules 2025, 15, 349. [Google Scholar] [CrossRef] [PubMed]
- Bakinowska, E.; Kiełbowski, K.; Pawlik, A. The Role of MicroRNA in the Pathogenesis of Acute Kidney Injury. Cells 2024, 13, 1559. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Huang, L.; Zhang, Z.; Yang, P.; Chen, Q.; Zeng, X.; Tan, F.; Wang, C.; Ruan, X.; Liao, X. CD36 promotes tubular ferroptosis by regulating the ubiquitination of FSP1 in acute kidney injury. Genes. Dis. 2024, 11, 449–463. [Google Scholar]
- Yan, X.; Ma, Y.; Yang, J.; Chang, X.; Shi, S.; Song, G. The role and advance of ubiquitination and deubiquitination in depression pathogenesis and treatment. Drug Dev. Res. 2024, 85, e70005. [Google Scholar] [CrossRef]
- Ming, W.H.; Wen, L.; Hu, W.J.; Qiao, R.F.; Zhou, Y.; Su, B.W.; Bao, Y.N.; Gao, P.; Luan, Z.L. The crosstalk of Wnt/β-catenin signaling and p53 in acute kidney injury and chronic kidney disease. Kidney Res. Clin. Pract. 2024, 43, 724–738. [Google Scholar] [CrossRef]
- Zhang, L.; Liu, S.; Zhao, Q.; Liu, X.; Zhang, Q.; Liu, M.; Zhao, W. The role of ubiquitination and deubiquitination in the pathogenesis of non-alcoholic fatty liver disease. Front. Immunol. 2025, 16, 1535362. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhao, Q.Q.; Fan, S.J.; Xu, D.Y.; Lin, L.M.; Luo, W.; Ye, B.Z.; Zou, C.P.; Zhu, H.; Zhuang, Z.S.; et al. JOSD2 alleviates acute kidney injury through deubiquitinating SIRT7 and negativity regulating SIRT7-NF-κB inflammatory pathway in renal tubular epithelial cells. Acta Pharmacol. Sin. 2025, 46, 2468–2481. [Google Scholar] [CrossRef]
- Yang, Y.; Wang, P.; Zhou, K.; Zhang, W.; Liu, S.; Ouyang, J.; Bai, M.; Ding, G.; Huang, S.; Jia, Z.; et al. HUWE1-Mediated Degradation of MUTYH Facilitates DNA Damage and Mitochondrial Dysfunction to Promote Acute Kidney Injury. Adv. Sci. 2025, 12, 2412250. [Google Scholar] [CrossRef]
- Hu, C.; Zhang, B.; Zhao, S. METTL3-mediated N6-methyladenosine modification stimulates mitochondrial damage and ferroptosis of kidney tubular epithelial cells following acute kidney injury by modulating the stabilization of MDM2-p53-LMNB1 axis. Eur. J. Med. Chem. 2023, 259, 115677. [Google Scholar] [CrossRef]
- Huang, Z.; Peng, Y.; Ke, G.; Xiao, Y.; Chen, Y. CaMKII may regulate renal tubular epithelial cell apoptosis through YAP/NFAT2 in acute kidney injury mice. Ren. Fail. 2023, 45, 2172961. [Google Scholar] [CrossRef]
- Wang, X.; Li, Q.; Sui, B.; Xu, M.; Pu, Z.; Qiu, T. Schisandrin a from schisandra chinensis attenuates ferroptosis and NLRP3 inflammasome-mediated pyroptosis in diabetic nephropathy through mitochondrial damage by AdipoR1 ubiquitination. Oxidative Med. Cell. Longev. 2022, 2022, 5411462. [Google Scholar] [CrossRef]
- Li, Y.; Ren, D.; Shen, Y.; Zheng, X.; Xu, G. Altered DNA methylation of TRIM13 in diabetic nephropathy suppresses mesangial collagen synthesis by promoting ubiquitination of CHOP. EBioMedicine 2020, 51, 102582. [Google Scholar] [CrossRef]
- He, H.; Wang, L.; Xian, B.; Xia, Y. Regulatory Roles of E3 Ubiquitin Ligases and Deubiquitinases in Bone. Biomolecules 2025, 15, 679. [Google Scholar] [CrossRef]
- Kim, M.S.; Kim, M.S. Deubiquitination of epidermal growth factor receptor by ubiquitin-specific peptidase 54 enhances drug sensitivity to gefitinib in gefitinib-resistant non-small cell lung cancer cells. PLoS ONE 2025, 20, e0320668. [Google Scholar] [CrossRef]
- Shen, J.; Jiang, Y.; Bu, W.; Yu, M.; Huang, R.; Tang, C.; Yang, Z.; Gao, H.; Su, L.; Cheng, D.; et al. Protein Ubiquitination Modification in Pulmonary Fibrosis. Compr. Physiol. 2025, 15, e70013. [Google Scholar] [CrossRef]

| Functional Category | DUB/Enzyme | Target Protein | Regulatory Mechanism | Biological Significance | References |
|---|---|---|---|---|---|
| DNA Damage Response and Protein Stability | USP1 | FANCD2 | Removes monoubiquitin after DNA repair | Allows cell cycle progression and maintains normal cellular functions | [32,33] |
| USP4 | BRCA1 | Deubiquitination-mediated stabilization | Positively regulates BRCA1 stability and genomic integrity maintenance | [34] | |
| OTUB1 | DNA repair proteins | Ubiquitin removal from repair factors | Key regulator in DNA damage repair and cellular protection | [38,39] | |
| Protein Quality Control | BRCA1 (E3 ligase) | PERK, IRE1 | Ubiquitination of UPR sensors | Controls unfolded protein response; dysfunction leads to proteostatic stress | [35] |
| DUBs (general) | UPR components | Counterbalance ubiquitination | Essential for protein homeostasis maintenance in stress conditions | [36] | |
| Signal Transduction | DUBs (general) | ABA signaling factors | Regulation of ubiquitination levels | Modulate hormone signaling strength and cellular responses to environmental stimuli | [37] |
| Cellular Protection | DUBs (general) | Stress response proteins | Enhanced protein stability | Promote cellular survival under various stress conditions | [40,41] |
| Modification Type | Structural Features | Key Enzymes | Regulatory Targets | Role in AKI | References |
|---|---|---|---|---|---|
| SUMOylation | Small, structurally compact | UBC9, PIAS | p53, Bcl-2 | Anti-apoptotic, protein stabilization | [42,43,44] |
| Neddylation | Ubiquitin-like | NAE1, UBC12 | Cullin, CDKs | Initiates cell repair | [21,45,46,47,48] |
| ISGylation | IFN-induced | UBE1L, UBE2L6 | IRF3, STATs | Antiviral, antioxidant | [37,39,49] |
| UFMylation | Novel UBL | UBA5, UFC1 | DDRGK1, ERAD complex | Alleviates ER stress | [50] |
| FATylation | Affects immunity | UBA6, USE1 | β-catenin, TNF-R | Promotes fibrosis and stress response | [51,52] |
| Urmylation | Affects tRNA modification | UBA4, URM1 | Mitochondrial oxidases | Antioxidant protection | [53] |
| Chain Type | Target Protein | E3 Ligase | Functional Outcome | Role in AKI | References |
|---|---|---|---|---|---|
| K63-linked | TRAF6 | TRAF6 (auto) | Signal platform formation | Pro-inflammatory | [67,68] |
| K63-linked | RIP1 | TRAF6, cIAP1/2 | MAPK/NF-κB activation | Pro-inflammatory | [67] |
| K48-linked | IκBα | SCFβ-TrCP | Proteasomal degradation | Pro-inflammatory | [66] |
| K48-linked | NOX4 | Unknown | Protein degradation | Anti-inflammatory | [55] |
| Mixed chains | NEMO | Linear ubiquitin chain assembly complex | Enhanced NF-κB activation | Pro-inflammatory | [65,69] |
| Component | Modification | Function | Outcome in AKI | References |
|---|---|---|---|---|
| PINK1 | Autophosphorylation | Ubiquitin kinase activation | Mitophagy initiation | [86] |
| Parkin | Phospho-ubiquitin binding | E3 ligase activation | Mitochondrial ubiquitination | [87] |
| NDP52 | K63-Ub recognition | Autophagy receptor | Mitophagy execution | [90] |
| OPTN | Linear/K63-Ub binding | Autophagy receptor | Enhanced clearance | [91] |
| URM1 | Protein urmylation | Antioxidant enhancement | Cytoprotection | [59,60,61] |
| DUB | Substrates | Signal Pathway | Effects | References |
|---|---|---|---|---|
| A20 | IκBα, TRAF6, RIP1 | NF-κB | Removes ubiquitin chain from IκBα, preventing degradation; maintains NF-κB in inactive state; removes K63-linked ubiquitin chains; protective mechanism to limit inflammation; A20 overexpression confers protection in AKI | [94,96,97] |
| CYLD | TRAF2, TRAF6, NEMO | NF-κB | Negatively regulates NF-κB activation by removing K63-linked ubiquitin chains; CYLD-deficient mice showed enhanced NF-κB activation and increased inflammatory cytokine production following renal IRI | [98,99] |
| USP13 | MCL-1 | USP13-MCL-1 | Regulates MCL-1 ubiquitination to maintain its stability and participate in mitochondrial function modulation; downregulating USP13 expression in AKI leads to increased MCL-1 degradation and exacerbated mitochondrial dysfunction; USP13 inhibition further impairs mitochondrial protection and aggravates AKI pathogenesis | [100] |
| USP18 | ISG15-conjugated proteins, NCOA4 | ISG15/ISGylation, Ferroptosis | Removes ISG15 from ISGylated proteins (de-ISGylation); regulates ISG15-mediated protein stability; USP18-mediated deISGylation of NCOA4 promotes ferroptosis, potential therapeutic target in AKI | [55,75,76] |
| USP7 | p53, MDM2, FOXO4 | p53-MDM2, Oxidative stress | Stabilizes p53 by removing K48-linked ubiquitin chains; promotes cell survival under oxidative stress; dual role in regulating both p53 and MDM2 stability; critical for DNA damage response in AKI | [79,80,101] |
| USP22 | Histones H2A/H2B, SIRT1 | Epigenetic regulation, SIRT1 | Removes ubiquitin from histones; regulates chromatin structure and gene expression; stabilizes SIRT1, promoting anti-inflammatory responses; protects against cisplatin-induced AKI | [102,103,104] |
| USP14 | Proteasome substrates | Proteasome regulation | Regulates proteasome activity by removing ubiquitin chains; controls protein degradation rate; dysregulation leads to accumulation of damaged proteins and cellular stress in AKI | [101,105] |
| Subquinocin (inhibitor) | CYLD, USP family DUBs | NF-κB | Inhibits CYLD and USP family DUBs, promotes NF-κB activation | [95] |
| Target | Modification Type | Drug/Inhibitor | Status | Mechanism of Action | Clinical/Animal Model Studies | References |
|---|---|---|---|---|---|---|
| NAE1 | Neddylation | MLN4924 (Pevonedistat) | Clinical Phase II | Inhibits CRL activation, reduces repair burden | Proven renal protection | [56,57,101,117,118,119,120] |
| A20 | DUB | No available drugs | Potential target | Inhibits NF-κB overactivation | Improves inflammation in mouse AKI models | [108] |
| UBA5 | UFMylation | None | To be developed | Involved in ER-phagy | Known to protect ER function | [111,112] |
| USP14 | DUB | IU1 | Experimental validation | Enhances protein clearance capacity | Trend toward reduced nephrotoxicity | [108] |
| SUMO E2 (Ubc9) | SUMOylation | TAK-981 | Preclinical | Immunomodulator | Under evaluation | [113,114,115,116] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, Y.; Tao, S.; Liu, L.; Zhang, L. The Role of Ubiquitination and Deubiquitination in the Pathogenesis of Acute Kidney Injury: Progress in Research. Biomedicines 2025, 13, 2873. https://doi.org/10.3390/biomedicines13122873
Zhou Y, Tao S, Liu L, Zhang L. The Role of Ubiquitination and Deubiquitination in the Pathogenesis of Acute Kidney Injury: Progress in Research. Biomedicines. 2025; 13(12):2873. https://doi.org/10.3390/biomedicines13122873
Chicago/Turabian StyleZhou, Yu, Shuchun Tao, Lei Liu, and Lei Zhang. 2025. "The Role of Ubiquitination and Deubiquitination in the Pathogenesis of Acute Kidney Injury: Progress in Research" Biomedicines 13, no. 12: 2873. https://doi.org/10.3390/biomedicines13122873
APA StyleZhou, Y., Tao, S., Liu, L., & Zhang, L. (2025). The Role of Ubiquitination and Deubiquitination in the Pathogenesis of Acute Kidney Injury: Progress in Research. Biomedicines, 13(12), 2873. https://doi.org/10.3390/biomedicines13122873






