Growth Factor-Primed WJ-MSC Secretome Enhances Fibroblast Expansion In Vitro
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Collection and Cord Processing
2.2. Stimulation and Secretome Collection from WJ-MSC Cultures
2.3. Flow Cytometry Assay
2.4. Multiplex Analysis of WJ-MSC Secretome
2.5. Isolation and Primary Culture of Human Dermal Fibroblasts
2.6. Effect of WJ-MSC Secretome on Cytotoxicity and Proliferation of Human Fibroblasts
2.7. In Vitro Wound-Healing Assay
2.8. Effect of the WJ-MSC Secretome on Procollagen I Production and α-Smooth Muscle Actin Expression in Human Fibroblasts
2.9. Statistical Analysis
3. Results
3.1. Isolation and Characterization of WJ-MSCs
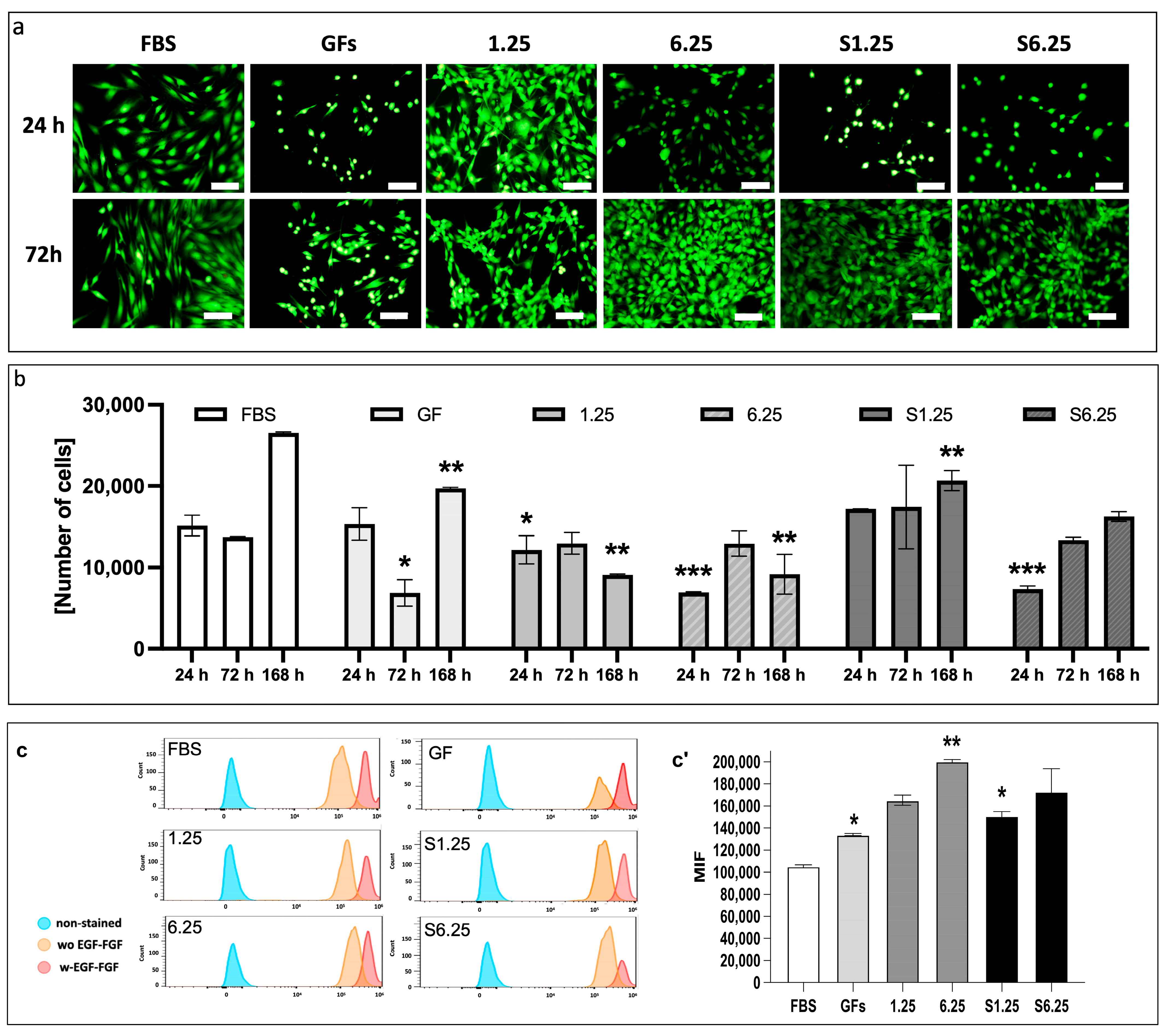
3.2. Secretome Preserves Fibroblast Viability and Enhances Proliferation
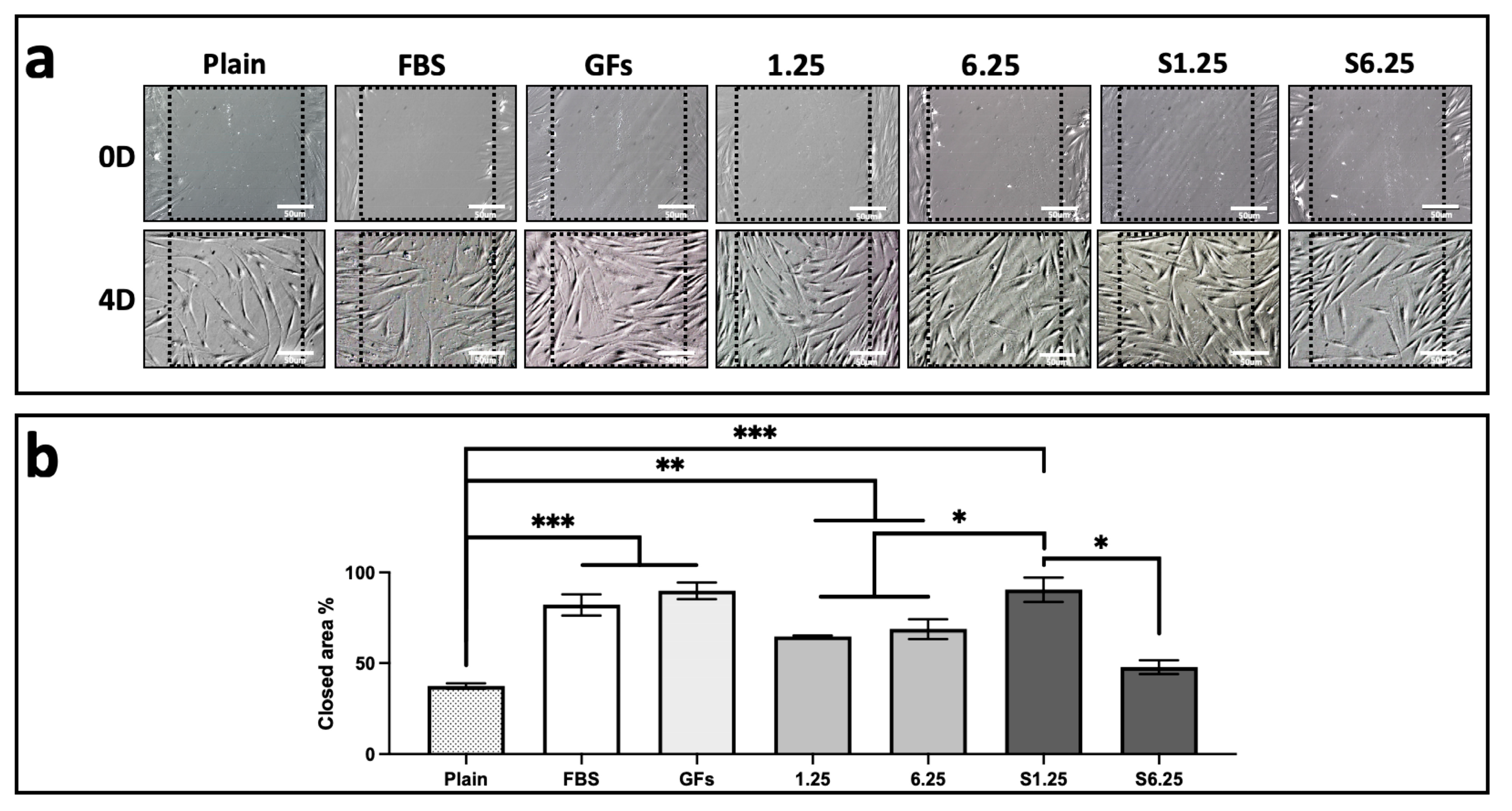
3.3. WJ-MSC Secretome Enhances Fibroblast In Vitro Wound Healing
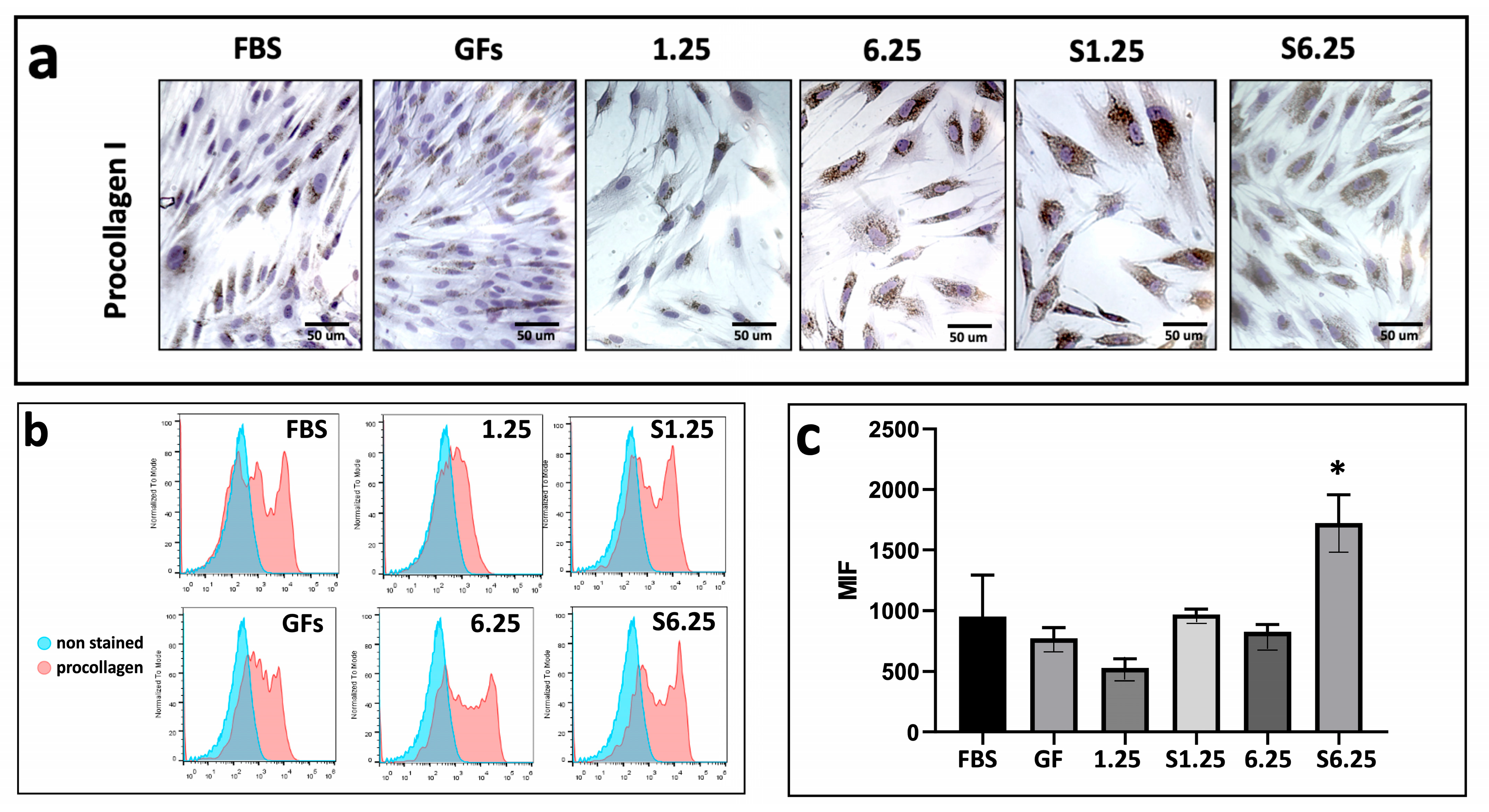
3.4. WJ-MSC Secretome Promotes Type I Procollagen Expression
3.5. Secretome-Mediated Upregulation of Alpha-Actin in Human Fibroblasts
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ANOVA | Analysis of Variance |
| Calcein AM | Calcein acetoxymethyl ester |
| CD105 | Cluster of differentiation 105 |
| CD11b | Cluster of differentiation 11b |
| CD19 | Cluster of differentiation 19 |
| CD34 | Cluster of differentiation 34 |
| CD44 | Cluster of differentiation 44 |
| CD45 | Cluster of differentiation 45 |
| CD73 | Cluster of differentiation 73 |
| CD90 | Cluster of differentiation 90 |
| CFSE | Carboxyfluorescein diacetate succinimidyl ester |
| DMEM | Dulbecco’s Modified Eagle Medium/Nutrient Mixture |
| DMEM-F12 | Dulbecco’s Modified Eagle Medium-Nutrient Mixture F-12 |
| EDTA | Ethylenediaminetetraacetic acid |
| EGF | Epidermal Growth Factor |
| EPO | Erythropoietin |
| FBS | Fetal Bovine Serum |
| FGF | Fibroblast Growth Factor |
| FITC | Fluorescein isothiocyanate |
| G-CSF | Granulocyte Colony-Stimulating Factor |
| GFs | Growth Factors |
| GM-CSF | Granulocyte-Macrophage Colony-Stimulating Factor |
| HBSS | Hanks’ Balanced Salt Solution |
| HGF | Hepatocyte Growth Factor. |
| HLA-ABC | Human Leukocyte Antigen-ABC |
| HLA-DR | Human Leukocyte AntigeN-DR |
| IMH | Immunohistochemistry |
| M-CSF | Macrophage Colony-Stimulating Factor |
| MFI | Mean fluorescence intensity |
| MHC-I | Major Histocompatibility Complex Class I |
| MHC-II | Major Histocompatibility Complex Class II |
| MSC | Mesenchymal stem cells |
| ns | not significant |
| P0 | Passage 0 |
| P1 | Passage 1 |
| P2 | Passage 2 |
| PBS | Phosphate-Buffered Saline |
| PDGF-AA | Platelet-Derived Growth Factor AA |
| PDGF-BB | Platelet-Derived Growth Factor BB |
| PE | Phycoerythrin |
| PMA | Phorbol ester 12-myristate 13-acetate |
| RNA | Ribonucleic acid |
| S1.25 | Stimulated secretome concentration 1.25 mg/mL |
| S6.25 | Stimulated secretome concentration 6.25 mg/mL |
| SCF | Stem Cell Factor |
| SD | Standard deviation |
| TGF-α | Transforming Growth Factor-alpha |
| TGF-β | Transforming Growth Factor-beta |
| 1.25 | Unstimulated secretome concentration 1.25 mg/mL |
| 6.25 | Unstimulated secretome concentration 6.25 mg/mL |
| VEGF | Vascular Endothelial Growth Factor |
| W FGF/EGF | With FGF/EGF |
| WJ-MSC | Wharton’s jelly-derived Mesenchymal Stem Cells |
| WO FGF/EGF | Without FGF/EGF |
References
- Kim, D.W.; Staples, M.; Shinozuka, K.; Pantcheva, P.; Kang, S.D.; Borlongan, C.V. Wharton’s jelly-derived mesenchymal stem cells: Phenotypic characterization and optimizing their therapeutic potential for clinical applications. Int. J. Mol. Sci. 2013, 14, 11692–11712. [Google Scholar] [CrossRef]
- Saleh, M.; Fotook Kiaei, S.Z.; Kavianpour, M. Application of Wharton jelly-derived mesenchymal stem cells in patients with pulmonary fibrosis. Stem. Cell Res. Ther. 2022, 13, 71. [Google Scholar] [CrossRef]
- Zakrzewski, W.; Dobrzyński, M.; Szymonowicz, M.; Rybak, Z. Stem cells: Past, present, and future. Stem. Cell Res. Ther. 2019, 10, 68. [Google Scholar] [CrossRef]
- Prasanna, S.J.; Jahnavi, V.S. Wharton’s jelly mesenchymal stem cells as off-the-shelf cellular therapeutics: A closer look into their regenerative and immunomodulatory properties. Open Tissue Eng. Regen. Med. J. 2011, 4, 28–38. [Google Scholar] [CrossRef]
- Dominici, M.; Le Blanc, K.; Mueller, I.; Slaper-Cortenbach, I.; Marini, F.; Krause, D.; Deans, R.; Keating, A.; Prockop, D.j.; Horwitz, E. Minimal criteria for defining multipotent mesenchymal stromal cells. Cytotherapy 2006, 8, 315–317. [Google Scholar] [CrossRef] [PubMed]
- Vizoso, F.J.; Eiro, N.; Cid, S.; Schneider, J.; Perez-Fernandez, R. Mesenchymal stem cell secretome: Toward cell-free therapeutic strategies in regenerative medicine. Int. J. Mol. Sci. 2017, 18, 1852. [Google Scholar] [CrossRef]
- Prasajak, P.; Rattananinsruang, P.; Chotinantakul, K.; Dechsukhum, C.; Leeanansaksiri, W. Embryonic stem cells conditioned medium enhances Wharton’s jelly-derived mesenchymal stem cells expansion under hypoxic condition. Cytotechnology 2015, 67, 493–505. [Google Scholar] [CrossRef] [PubMed]
- Musiał-Wysocka, A.; Kot, M.; Sułkowski, M.; Badyra, B.; Majka, M. Molecular and Functional Verification of Wharton’s Jelly Mesenchymal Stem Cells (WJ-MSCs) Pluripotency. Int. J. Mol. Sci. 2019, 20, 1807. [Google Scholar] [CrossRef]
- Asserson, D.B. Allogeneic Mesenchymal Stem Cells After In Vivo Transplantation: A Review. Cell. Reprogram. 2023, 25, 264–276. [Google Scholar] [CrossRef]
- Gomez-Ruiz, V.; Blanco, J.F.; Villarón, E.M.; Fidalgo, H.; López-Parra, M.; Sánchez-Guijo, F. Autologous mesenchymal stem cell transplantation for spinal fusion: 10 years follow-up of a phase I/II clinical trial. Stem Cell Res. Ther. 2023, 14, 78. [Google Scholar] [CrossRef]
- Krupa, P.; Vackova, I.; Ruzicka, J.; Zaviskova, K.; Dubisova, J.; Koci, Z.; Turnovcova, K.; Urdzikova, L.M.; Kubinova, S.; Rehak, S.; et al. The Effect of Human Mesenchymal Stem Cells Derived from Wharton’s Jelly in Spinal Cord Injury Treatment Is Dose-Dependent and Can Be Facilitated by Repeated Application. Int. J. Mol. Sci. 2018, 19, 1503. [Google Scholar] [CrossRef]
- Liang, H.; Suo, H.; Wang, Z.; Feng, W. Progress in the treatment of osteoarthritis with umbilical cord stem cells. Hum. Cell 2020, 33, 470–475. [Google Scholar] [CrossRef]
- Kalaszczynska, I.; Ferdyn, K. Wharton’s jelly derived mesenchymal stem cells: Future of regenerative medicine? Recent findings and clinical significance. BioMed Res. Int. 2015, 2015, 430847. [Google Scholar] [CrossRef]
- Yang, Q.; Pinto, V.M.R.; Duan, W.; Paxton, E.E.; Dessauer, J.H.; Ryan, W.; Lopez, M.J. In vitro characteristics of heterogeneous equine hoof progenitor cell isolates. Front. Bioeng. Biotechnol. 2019, 7, 155. [Google Scholar] [CrossRef]
- Thompson, P.A.; Perera, T.; Marin, D.; Oran, B.; Popat, U.; Qazilbash, M.; Hosing, C.M. Double umbilical cord blood transplant is effective therapy for relapsed or refractory Hodgkin lymphoma. Leuk. Lymphoma 2015, 57, 1607–1615. [Google Scholar] [CrossRef]
- Zhang, Y.; Na, T.; Zhang, K.; Yang, Y.; Xu, H.; Wei, L.; Du, Y. GMP-grade microcarrier and automated closed industrial scale cell production platform for culture of MSCs. J. Tissue Eng. Regen. 2022, 16, 934–944. [Google Scholar] [CrossRef]
- Pan, Y.; Wu, W.; Jiang, X.; Liu, Y. Mesenchymal stem cell-derived exosomes in cardiovascular and cerebrovascular diseases: From mechanisms to therapy. Biomed. Pharmacother. 2023, 163, 114817. [Google Scholar] [CrossRef]
- Maguire, G. Stem cell therapy without the cells. Commun. Integr. Biol. 2013, 6, e26631. [Google Scholar] [CrossRef] [PubMed]
- Duan, L.; Li, X.; Xu, X.; Xu, L.; Wang, D.; Ouyang, K.; Liang, Y. Large-scale Preparation of Synovial Fluid Mesenchymal Stem Cell-Derived Exosomes by 3D Bioreactor Culture. J. Vis. Exp. 2022, 26, 185. [Google Scholar] [CrossRef]
- Li, X.; Zhang, D.; Yu, Y.; Wang, L.; Zhao, M. Umbilical cord-derived mesenchymal stem cell secretome promotes skin regeneration and rejuvenation: From mechanism to therapeutics. Cell Prolif. 2024, 57, e13586. [Google Scholar] [CrossRef] [PubMed]
- Trotzier, C.; Bellanger, C.; Abdessadeq, H.; Delannoy, P.; Mojallal, A.; Auxenfans, C. Deciphering influence of donor age on adipose-derived stem cells: In vitro paracrine function and angiogenic potential. Sci. Rep. 2024, 14, 27589. [Google Scholar] [CrossRef]
- Miclau, K.; Hambright, W.S.; Huard, J.; Stoddart, M.J.; Bahney, C.S. Cellular expansion of MSCs: Shifting the regenerative potential. Aging Cell 2023, 22, e13759. [Google Scholar] [CrossRef]
- Turlo, A.J.; E Hammond, D.; Ramsbottom, K.A.; Soul, J.; Gillen, A.; McDonald, K.; Peffers, M.J. Mesenchymal stromal cell secretome is affected by tissue source and donor age. Stem Cells 2023, 41, 1047–1059. [Google Scholar] [CrossRef] [PubMed]
- Ionescu, L.; Byrne, R.N.; van Haaften, T.; Vadivel, A.; Alphonse, R.S.; Rey-Parra, G.J.; Weissmann, G.; Hall, A.; Eaton, F.; Thébaud, B. Stem cell conditioned medium improves acute lung injury in mice: In vivo evidence for stem cell paracrine action. Am. J. Physiol. Lung Cell Mol. Physiol. 2012, 303, 967–977. [Google Scholar] [CrossRef]
- Engler, A.J.; Sen, S.; Sweeney, H.L.; Discher, D.E. Matrix elasticity directs stem cell lineage specification. Cell 2006, 126, 677–689. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, J.R.; Teixeira, G.Q.; Santos, S.G.; Barbosa, M.A.; Almeida-Porada, G.; Gonçalves, R.M. Mesenchymal stromal cell secretome: Influencing therapeutic potential by cellular pre-conditioning. Front. Immunol. 2018, 9, 2837. [Google Scholar] [CrossRef]
- Mohyeldin, A.; Garzón-Muvdi, T.; Quiñones-Hinojosa, A. Oxygen in stem cell biology: A critical component of the stem cell niche. Cell Stem Cell 2010, 7, 150–161. [Google Scholar] [CrossRef]
- Wu, M.; Ruan, J.; Zhong, B. Progress in human epidermal growth factor research. Sheng Wu Gong Cheng Xue Bao Chin. J. Biotechnol. 2020, 36, 2813–2823. [Google Scholar] [CrossRef]
- Andrae, J.; Gallini, R.; Betsholtz, C. Role of platelet-derived growth factors in physiology and medicine. Genes Dev. 2008, 22, 1276–1312. [Google Scholar] [CrossRef]
- Sotiropoulou, P.A.; Perez, S.A.; Salagianni, M.; Baxevanis, C.N.; Papamichail, M. Characterization of the optimal culture conditions for clinical scale production of human mesenchymal stem cells. Stem Cells 2006, 24, 462–471. [Google Scholar] [CrossRef]
- Tsutsumi, S.; Shimazu, A.; Miyazaki, K.; Pan, H.; Koike, C.; Yoshida, E. Retention of multilineage differentiation potential of mesenchymal cells during proliferation in response to FGF. Biochem. Biogr. Common Res. 2001, 288, 413–419. [Google Scholar] [CrossRef]
- Castell-Rodríguez, A.E.; Herrera-Enríquez, M.A.; Piñón-Zárate, G.; Jarquín-Yáñez, K.; Chaires-Rosas, C.P.; Arellano-Olivares, R.M. Method for Preparing a Supplement from Mesenchymal Cell Cultures of Wharton’s Jelly and Uses of Same. Patent No. 380950, 9 March 2021. [Google Scholar]
- Park, S.B.; Yu, K.R.; Jung, J.W.; Lee, S.R.; Roh, K.H.; Seo, M.S.; Park, J.R.; Kang, S.K.; Lee, Y.S.; Kang, K.S. bFGF enhances the IGFs-mediated pluripotent and differentiation potentials in multipotent stem cells. Growth Factors 2009, 27, 425–437. [Google Scholar] [CrossRef]
- González-González, A.; García-Sánchez, D.; Dotta, M.; Rodríguez-Rey, J.C.; Pérez-Campo, F.M. Mesenchymal stem cells secretome: The cornerstone of cell-free regenerative medicine. World J. Stem Cells 2020, 12, 1529–1552. [Google Scholar] [CrossRef] [PubMed]
- Buyl, K.; Vanhaecke, T.; Desmae, T.; Lagneaux, L.; Rogiers, V.; Najar, M.; De Kock, J. Evaluation of a new standardized enzymatic isolation protocol for human umbilical cord-derived stem cells. Toxicol. Vitr. 2015, 29, 1254–1262. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Lin, H.; Yu, Y.; Lu, Y.; He, B.; Liu, M.; Zhuang, L.; Xu, Y.; Li, W. In Situ Rapid-Formation Sprayable Hydrogels for Challenging Tissue Injury Management. Adv. Mater. 2024, 36, e2400310. [Google Scholar] [CrossRef]
- Napolitano, F.; Giudice, V.; D’Esposito, V.; Prevete, N.; Scala, P.; de Paulis, A.; Selleri, C.; Formisano, P.; Rossi, F.W.; Montuori, N. Cell-free regenerative medicine: Identifying the best source of mesenchymal stem cells for skin therapy in Systemic Sclerosis. Front. Cell. Dev. Biol. 2025, 13, 1518412. [Google Scholar] [CrossRef]
- Riekstina, U.; Muceniece, R.; Cakstina, I.; Muiznieks, I.; Ancans, J. Characterization of human skin-derived mesenchymal stem cell proliferation rate in different growth conditions. Cytotechnology 2008, 58, 153–162. [Google Scholar] [CrossRef]
- Marino, L.; Castaldi, M.A.; Fulgione, C.; Castaldi, S.G.; Manzo, P.; Giudice, V.; Picone, F.; Campitiello, M.R.; Polichetti, M.; Guida, M.; et al. Reduced proliferative potential with conserved stem/stromal phenotype of human umbilical cord mesenchymal stem cells in placental syndromes: A prospective cohort study. Clin. Exp. Obstet. Gynecol. 2023, 50, 196. [Google Scholar] [CrossRef]
- Salehinejad, P.; Alitheen, N.B.; Mandegary, A.; Nematollahi-Mahani, S.N.; Janzamin, E. Effect of EGF and bFGF on the expansion properties of human umbilical cord mesenchymal cells. Vitr. Cell Dev. Biol. Anim. 2013, 49, 515–523. [Google Scholar] [CrossRef]
- Nie, W.B.; Zhang, D.; Wang, L.S. Growth Factor Gene-Modified Mesenchymal Stem Cells in Tissue Regeneration. Drug Des. Devel. Ther. 2020, 14, 1241–1256. [Google Scholar] [CrossRef] [PubMed]
- Bogatcheva, N.V.; Coleman, M.E. Conditioned medium of mesenchymal stromal cells: A new class of therapeutics. Biochem. Biokhimiia 2019, 84, 1375–1389. [Google Scholar] [CrossRef]
- Pawitan, J.A. Prospect of stem cell conditioned medium in regenerative medicine. BioMed Res. Int. 2014, 2014, 965849. [Google Scholar] [CrossRef]
- Yamada, M.; Tatsumi, R.; Yamanouchi, K.; Hosoyama, T.; Shiratsuchi, S.; Sato, A.; Mizunoya, W.; Ikeuchi, Y.; Furuse, M.; Allen, R.E. High concentrations of HGF inhibit skeletal muscle satellite cell proliferation in vitro by inducing expression of myostatin: A possible mechanism for reestablishing satellite cell quiescence In Vivo. Am. J. Physiol. Cell Physiol. 2010, 298, 465–476. [Google Scholar] [CrossRef]
- Ding, J.; Wang, J.; Cai, X.; Yin, T.; Zhang, Y.; Yang, C.; Yang, J. Granulocyte colony-stimulating factor in reproductive-related disease: Function, regulation and therapeutic effect. Biomed. Pharmacother. 2022, 150, 112903. [Google Scholar] [CrossRef]
- Forte, G.; Minieri, M.; Cossa, P.; Antenucci, D.; Sala, M.; Gnocchi, V.; Fiaccavento, R.; Carotenuto, F.; De Vito, P.; Baldini, P.M. Hepatocyte Growth Factor Effects on Mesenchymal Stem Cells: Proliferation, Migration, and Differentiation. Stem Cells 2006, 24, 23–33. [Google Scholar] [CrossRef] [PubMed]
- Meng, H.F.; Jin, J.; Wang, H.; Wang, L.S.; Wu, C.T. Recent advances in the therapeutic efficacy of hepatocyte growth factor gene-modified mesenchymal stem cells in multiple disease settings. J. Cell Mol. Med. 2022, 26, 4745–4755. [Google Scholar] [CrossRef]
- Qin, P.; Kurpakus, M.A. The role of laminin-5 in TGFα/EGF-mediated corneal epithelial cell motility. Exp. Eye Res. 1998, 66, 569–579. [Google Scholar] [CrossRef] [PubMed]
- Praveen, K.L.; Kandoi, S.; Misra, R.; Vijayalakshmi, S.; Rajagopal, K.; Verma, R.S. The mesenchymal stem cell secretome: A new paradigm towards cell-free therapeutic mode in regenerative medicine. Cytokine Growth Factor Rev. 2019, 46, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Stolfi, C.; Troncone, E.; Marafini, I.; Monteleone, G. Role of TGF-Beta and Smad7 in Gut Inflammation, Fibrosis and Cancer. Biomolecules 2020, 11, 17. [Google Scholar] [CrossRef]
- Monika, P.; Chandraprabha, M.N.; Murthy, K.N.C.; Rangarajan, A.; Waiker, P.V.; Sathish, M. Human primary chronic wound derived fibroblasts demonstrate differential pattern in expression of fibroblast specific markers, cell cycle arrest and reduced proliferation. Exp. Mol. Pathol. 2022, 127, 104803. [Google Scholar] [CrossRef]
- Tutuianu, R.; Rosca, A.M.; Iacomi, D.M.; Simionescu, M.; Titorencu, I. Human Mesenchymal Stromal Cell-Derived Exosomes Promote In Vitro Wound Healing by Modulating the Biological Properties of Skin Keratinocytes and Fibroblasts and Stimulating Angiogenesis. Int. J. Mol. Sci. 2021, 22, 6239. [Google Scholar] [CrossRef]
- Schuster, R.; Younesi, F.; Ezzo, M.; Hinz, B. The Role of Myofibroblasts in Physiological and Pathological Tissue Repair. Cold Spring Harb. Perspect. Biol. 2022, 15, a041231. [Google Scholar] [CrossRef]
- Aw, Y.B.; Chen, S.; Yeo, A.; Dangerfield, J.A.; Mok, P. Development and functional testing of a novel in vitro delayed scratch closure assay. Histochem. Cell Biol. 2024, 162, 245–255. [Google Scholar] [CrossRef] [PubMed]
- Chin, J.S.; Tan, M.L.L.; Lim, P.L.K.; Sharma, B.; Yeo, A.; Aw, Y.B.; Ng, Y.Z.; Bonnard, C.; Becker, D.L.; Mok, P. Secretome from prolonged high-density human Wharton’s jelly stem cell culture accelerates wound healing in both in vitro and in vivo models. Int. Wound J. 2025, 22, e70033, Erratum in Int. Wound J. 2025, 22, e70706. [Google Scholar] [CrossRef]
- Arno, A.I.; Amini-Nik, S.; Blit, P.H.; Al-Shehab, M.; Belo, C.; Herer, E.; Tien, C.H.; Jeschke, M.G. Human Wharton’s jelly mesenchymal stem cells promote skin wound healing through paracrine signaling. Stem Cell Res. Ther. 2014, 5, 28. [Google Scholar] [CrossRef]
- Sun, J.; Zhang, Y.; Song, X.; Zhu, J.; Zhu, Q. The Healing Effects of Conditioned Medium Derived from Mesenchymal Stem Cells on Radiation-Induced Skin Wounds in Rats. Cell Transplant. 2019, 28, 105–115. [Google Scholar] [CrossRef] [PubMed]
- Miceli, V.; Bulati, M.; Iannolo, G.; Zito, G.; Gallo, A.; Conaldi, P.G. Therapeutic Properties of Mesenchymal Stromal/Stem Cells: The Need of Cell Priming for Cell-Free Therapies in Regenerative Medicine. Int. J. Mol. Sci. 2021, 22, 763. [Google Scholar] [CrossRef] [PubMed]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jarquín-Yáñez, K.; Aguilar-Sandoval, D.M.; Piñón-Zárate, G.; Herrera-Enríquez, M.A.; Avila-Campos, I.D.; Hernandez-Tellez, B.; Dominguez-Diaz, D.M.; Blancas-Luciano, B.E.; Castell-Rodríguez, A.E. Growth Factor-Primed WJ-MSC Secretome Enhances Fibroblast Expansion In Vitro. Biomedicines 2025, 13, 2863. https://doi.org/10.3390/biomedicines13122863
Jarquín-Yáñez K, Aguilar-Sandoval DM, Piñón-Zárate G, Herrera-Enríquez MA, Avila-Campos ID, Hernandez-Tellez B, Dominguez-Diaz DM, Blancas-Luciano BE, Castell-Rodríguez AE. Growth Factor-Primed WJ-MSC Secretome Enhances Fibroblast Expansion In Vitro. Biomedicines. 2025; 13(12):2863. https://doi.org/10.3390/biomedicines13122863
Chicago/Turabian StyleJarquín-Yáñez, Katia, Diana Michel Aguilar-Sandoval, Gabriela Piñón-Zárate, Miguel Angel Herrera-Enríquez, Ivan Daniel Avila-Campos, Beatriz Hernandez-Tellez, Dayana Mayte Dominguez-Diaz, Blanca Esther Blancas-Luciano, and Andrés Eliú Castell-Rodríguez. 2025. "Growth Factor-Primed WJ-MSC Secretome Enhances Fibroblast Expansion In Vitro" Biomedicines 13, no. 12: 2863. https://doi.org/10.3390/biomedicines13122863
APA StyleJarquín-Yáñez, K., Aguilar-Sandoval, D. M., Piñón-Zárate, G., Herrera-Enríquez, M. A., Avila-Campos, I. D., Hernandez-Tellez, B., Dominguez-Diaz, D. M., Blancas-Luciano, B. E., & Castell-Rodríguez, A. E. (2025). Growth Factor-Primed WJ-MSC Secretome Enhances Fibroblast Expansion In Vitro. Biomedicines, 13(12), 2863. https://doi.org/10.3390/biomedicines13122863








