Oncostatin M Is Related to Polycystic Ovary Syndrome-Case Control Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Biochemical Analysis
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Guney, G.; Taşkın, M.I.; Sener, N.; Tolu, E.; Dodurga, Y.; Elmas, L.; Cetin, O.; Sarigul, C. The role of ERK-1 and ERK-2 gene polymorphisms in PCOS pathogenesis. Reprod. Biol. Endocrinol. 2022, 20, 95. [Google Scholar] [CrossRef]
- Bednarska, S.; Siejka, A. The pathogenesis and treatment of polycystic ovary syndrome: What’s new? Adv. Clin. Exp. Med. 2017, 26, 359–367. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Zhu, H.; Li, W.; Chen, D.; Xu, Y.; Xu, A.; Ye, D. Targeting adipokines in polycystic ovary syndrome and related metabolic disorders: From experimental insights to clinical studies. Pharmacol. Ther. 2022, 240, 108284. [Google Scholar] [CrossRef] [PubMed]
- Schüler-Toprak, S.; Ortmann, O.; Buechler, C.; Treeck, O. The Complex Roles of Adipokines in Polycystic Ovary Syndrome and Endometriosis. Biomedicines 2022, 10, 2503. [Google Scholar] [CrossRef] [PubMed]
- Clemente-Suárez, V.J.; Redondo-Flórez, L.; Beltrán-Velasco, A.I.; Martín-Rodríguez, A.; Martínez-Guardado, I.; Navarro-Jiménez, E.; Laborde-Cárdenas, C.C.; Tornero-Aguilera, J.F. The Role of Adipokines in Health and Disease. Biomedicines 2023, 11, 1290. [Google Scholar] [CrossRef] [PubMed]
- Stawski, L.; Trojanowska, M. Oncostatin M and its role in fibrosis. Connect. Tissue Res. 2019, 60, 40–49. [Google Scholar] [CrossRef] [PubMed]
- Eddie, S.L.; Childs, A.J.; Jabbour, H.N.; Anderson, R.A. Developmentally regulated IL6-type cytokines signal to germ cells in the human fetal ovary. Mol. Hum. Reprod. 2012, 18, 88–95. [Google Scholar] [CrossRef]
- Nikanfar, S.; Hamdi, K.; Haiaty, S.; Samadi, N.; Shahnazi, V.; Fattahi, A.; Nouri, M. Oncostatin M and its receptor in women with polycystic ovary syndrome and association with assisted reproductive technology outcomes. Reprod. Biol. 2022, 22, 100633. [Google Scholar] [CrossRef]
- Wang, R.; Mol, B.W. The Rotterdam criteria for polycystic ovary syndrome: Evidence-based criteria? Hum. Reprod. 2017, 32, 261–264. [Google Scholar] [CrossRef]
- Rudnicka, E.; Suchta, K.; Grymowicz, M.; Calik-Ksepka, A.; Smolarczyk, K.; Duszewska, A.M.; Smolarczyk, R.; Meczekalski, B. Chronic Low Grade Inflammation in Pathogenesis of PCOS. Int. J. Mol. Sci. 2021, 22, 3789. [Google Scholar] [CrossRef]
- Wang, Y.; Xie, L.; Tian, E.; Li, X.; Wen, Z.; Li, L.; Chen, L.; Zhong, Y.; Ge, R.S. Oncostatin M inhibits differentiation of rat stem Leydig cells in vivo and in vitro. J. Cell. Mol. Med. 2019, 23, 426–438. [Google Scholar] [CrossRef] [PubMed]
- Soares-Jr, J.M.; Hayashida, S.A.Y.; Marcondes, J.A.M.; Maciel, G.A.R.; Barcellos, C.R.G.; Maffazioli, G.N.; Monteiro, K.; Turri, J.A.O.; Azziz, R.; Baracat, E.C. Influence of Phenotypes on the Metabolic Syndrome of Women with Polycystic Ovary Syndrome over a Six-Year Follow-Up in Brazil. Biomedicines 2023, 11, 3262. [Google Scholar] [CrossRef] [PubMed]
- Kelly, C.C.; Lyall, H.; Petrie, J.R.; Gould, G.W.; Connell, J.M.; Sattar, N. Low grade chronic inflammation in women with polycystic ovarian syndrome. J. Clin. Endocrinol. Metab. 2001, 86, 2453–2455. [Google Scholar] [CrossRef] [PubMed]
- Rudnicka, E.; Kunicki, M.; Suchta, K.; Machura, P.; Grymowicz, M.; Smolarczyk, R. Inflammatory Markers in Women with Polycystic Ovary Syndrome. Biomed. Res. Int. 2020, 2020, 4092470. [Google Scholar] [CrossRef] [PubMed]
- Tola, E.N.; Yalcin, S.E.; Dugan, N. The predictive effect of inflammatory markers and lipid accumulation product index on clinical symptoms associated with polycystic ovary syndrome in nonobese adolescents and younger aged women. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 214, 168–172. [Google Scholar] [CrossRef] [PubMed]
- Diamanti-Kandarakis, E.; Paterakis, T.; Alexandraki, K.; Piperi, C.; Aessopos, A.; Katsikis, I.; Katsilambros, N.; Kreatsas, G.; Panidis, D. Indices of low-grade chronic inflammation in polycystic ovary syndrome and the beneficial effect of metformin. Hum. Reprod. 2006, 21, 1426–1431. [Google Scholar] [CrossRef]
- Toulis, K.A.; Goulis, D.G.; Mintziori, G.; Kintiraki, E.; Eukarpidis, E.; Mouratoglou, S.A.; Pavlaki, A.; Stergianos, S.; Poulasouchidou, M.; Tzellos, T.G.; et al. Meta-analysis of cardiovascular disease risk markers in women with polycystic ovary syndrome. Hum. Reprod. Update 2011, 17, 741–760. [Google Scholar] [CrossRef] [PubMed]
- Lantieri, F.; Bachetti, T. OSM/OSMR and Interleukin 6 Family Cytokines in Physiological and Pathological Condition. Int. J. Mol. Sci. 2022, 23, 11096. [Google Scholar] [CrossRef]
- West, N.R.; Hegazy, A.N.; Owens, B.M.J.; Bullers, S.J.; Linggi, B.; Buonocore, S.; Coccia, M.; Görtz, D.; This, S.; Stockenhuber, K.; et al. Oncostatin M drives intestinal inflammation and predicts response to tumor necrosis factor-neutralizing therapy in patients with inflammatory bowel disease. Nat. Med. 2017, 23, 579–589. [Google Scholar] [CrossRef]
- Jones, S.A.; Jenkins, B.J. Recent insights into targeting the IL-6 cytokine family in inflammatory diseases and cancer. Nat. Rev. Immunol. 2018, 18, 773–789. [Google Scholar] [CrossRef]
- Elks, C.M.; Zhao, P.; Grant, R.W.; Hang, H.; Bailey, J.L.; Burk, D.H.; McNulty, M.A.; Mynatt, R.L.; Stephens, J.M. Loss of Oncostatin M Signaling in Adipocytes Induces Insulin Resistance and Adipose Tissue Inflammation In Vivo. J. Biol. Chem. 2016, 291, 17066–17076. [Google Scholar] [CrossRef] [PubMed]
- Akarsu, M.; Hurşitoğlu, M.; Toprak, Z.; Yoldemir, Ş.A.; Altun, Ö.; Toprak, I.D.; Özcan, M.; Yürüyen, G.; Uğurlukişi, B.; Erdem, M.G.; et al. Relationships among oncostatin M, insulin resistance, and chronic inflammation: A pilot study. Arch. Endocrinol. Metab. 2020, 64, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Liao, B.; Qiao, J.; Pang, Y. Central Regulation of PCOS: Abnormal Neuronal-Reproductive-Metabolic Circuits in PCOS Pathophysiology. Front. Endocrinol. 2021, 12, 667422. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, M.F.; Sisk, E.C.; Rasgon, N.L. Valproate and neuroendocrine changes in relation to women treated for epilepsy and bipolar disorder: A review. Curr. Med. Chem. 2007, 14, 2799–2812. [Google Scholar] [CrossRef] [PubMed]
- Igaz, P.; Salvi, R.; Rey, J.P.; Glauser, M.; Pralong, F.P.; Gaillard, R.C. Effects of cytokines on gonadotropin-releasing hormone (GnRH) gene expression in primary hypothalamic neurons and in GnRH neurons immortalized conditionally. Endocrinology 2006, 147, 1037–1043. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Liu, Q.; Xie, Y.J.; Qu, L.H.; Zhang, M.X.; Mo, Z.C. Dyslipidemia involvement in the development of polycystic ovary syndrome. Taiwan J. Obstet. Gynecol. 2019, 58, 447–453. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Li, J.; Qin, J.J.; Cheng, W.L.; Zhu, X.; Gong, F.H.; She, Z.; Huang, Z.; Xia, H.; Li, H. Oncostatin M receptor β deficiency attenuates atherogenesis by inhibiting JAK2/STAT3 signaling in macrophages. J. Lipid Res. 2017, 58, 895–906. [Google Scholar] [CrossRef]
- Saeidnia, S.; Manayi, A.; Abdollahi, M. From in vitro Experiments to in vivo and Clinical Studies; Pros and Cons. Curr. Drug Discov. Technol. 2015, 12, 218–224. [Google Scholar] [CrossRef]
- Bizoń, A.; Franik, G.; Niepsuj, J.; Czwojdzińska, M.; Leśniewski, M.; Nowak, A.; Szynkaruk-Matusiak, M.; Madej, P.; Piwowar, A. The Associations between Sex Hormones and Lipid Profiles in Serum of Women with Different Phenotypes of Polycystic Ovary Syndrome. J. Clin. Med. 2021, 10, 3941. [Google Scholar] [CrossRef]
- Spałkowska, M.; Mrozińska, S.; Gałuszka-Bednarczyk, A.; Gosztyła, K.; Przywara, A.; Guzik, J.; Janeczko, M.; Milewicz, T.; Wojas-Pelc, A. The PCOS Patients differ in Lipid Profile According to their Phenotypes. Exp. Clin. Endocrinol. Diabetes 2018, 126, 437–444. [Google Scholar] [CrossRef]
- Myers, M.; Britt, K.L.; Wreford, N.G.; Ebling, F.J.; Kerr, J.B. Methods for quantifying follicular numbers within the mouse ovary. Reproduction 2004, 127, 569–580. [Google Scholar] [CrossRef]
- Anagnostis, P.; Tarlatzis, B.C.; Kauffman, R.P. Polycystic ovarian syndrome (PCOS): Long-term metabolic consequences. Metabolism 2018, 86, 33–43. [Google Scholar] [CrossRef]
- Tian, L.; Li, X.; Wang, Y.; Chen, Q.; Li, X.; Ge, R.S.; Li, X. Oncostatin M stimulates immature Leydig cell proliferation but inhibits its maturation and function in rats through JAK1/STAT3 signaling and induction of oxidative stress in vitro. Andrology 2022, 10, 354–366. [Google Scholar] [CrossRef]
- de Medeiros, S.F.; Winck Yamamoto de Medeiros, A.L.; Souto de Medeiros, M.A.; da Silva Carvalho, A.B.; Yamamoto, M.W.; M. Soares, J.; Baracat, E.C. Anthropometric, Metabolic, and Endocrine Parameters as Predictors of Estimated Average Glucose and Other Biomarkers of Dysglycemia in Women with Different Phenotypes of Polycystic Ovary Syndrome. Horm. Metab. Res. 2024, 111–176, online ahead of print. [Google Scholar] [CrossRef]
| Variables | PCOS (n = 32) | Control (n = 32) | p-Value |
|---|---|---|---|
| Age (years) | 26.00 ± 4.67 | 25.00 ± 5.18 | 0.54 |
| BMI (kg/m2) | 24.95 ± 4.84 | 23.88 ± 2.82 | 0.63 |
| Fasting glucose (mg/dL) | 91.16 ± 6.02 | 84.19 ± 6.08 | <0.001 *** |
| HOMA-IR | 3.25 ± 1.95 | 1.42 ± 0.99 | <0.001 *** |
| Total cholesterol (mg/dL) | 193 ± 32.5 | 150 ± 24.7 | <0.001 *** |
| LDL cholesterol (mg/dL) | 115.56 ± 28.21 | 74.75 ± 22.12 | <0.001 *** |
| Non-HDL cholesterol (mg/dL) | 139.28 ± 35.11 | 95.78 ± 25.28 | <0.001 *** |
| HDL (mg/dL) | 53.88 ± 3.93 | 55.00 ± 7.59 | 0.51 |
| LH/FSH ratio | 1.73 ± 0.31 | 0.61 ± 0.20 | <0.001 *** |
| Total testosterone (μg/L) | 0.64± 0.21 | 0.40± 0.11 | <0.001 *** |
| WBC | 7859 ± 2299 | 7159 ± 1719 | 0.21 |
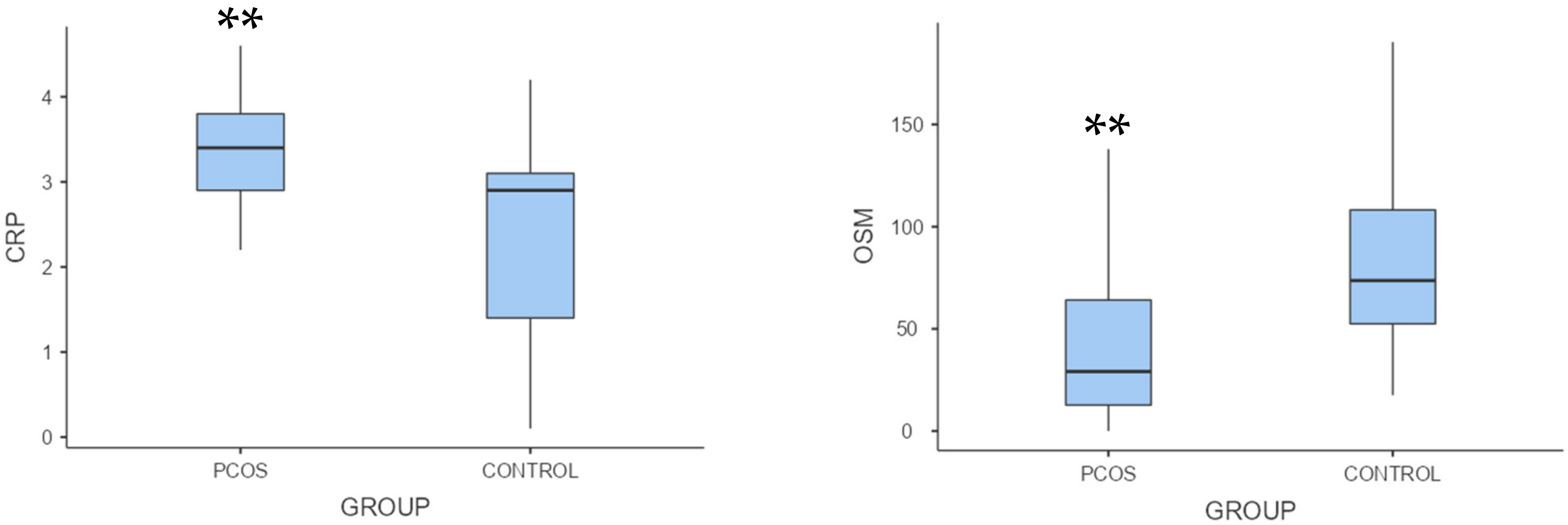
| C-reactive protein (mg/dL) | 4.37 ± 3.01 | 3.08 ± 4.14 | 0.001 ** |
| Oncostatin M (pg/mL) | 79.70 ± 107.23 | 166.11 ± 196.04 | 0.002 ** |
| Variables | PCOS Group Correlation Coefficient (ρ) | p-Value | Control Group Correlation Coefficient (ρ) | p-Value |
|---|---|---|---|---|
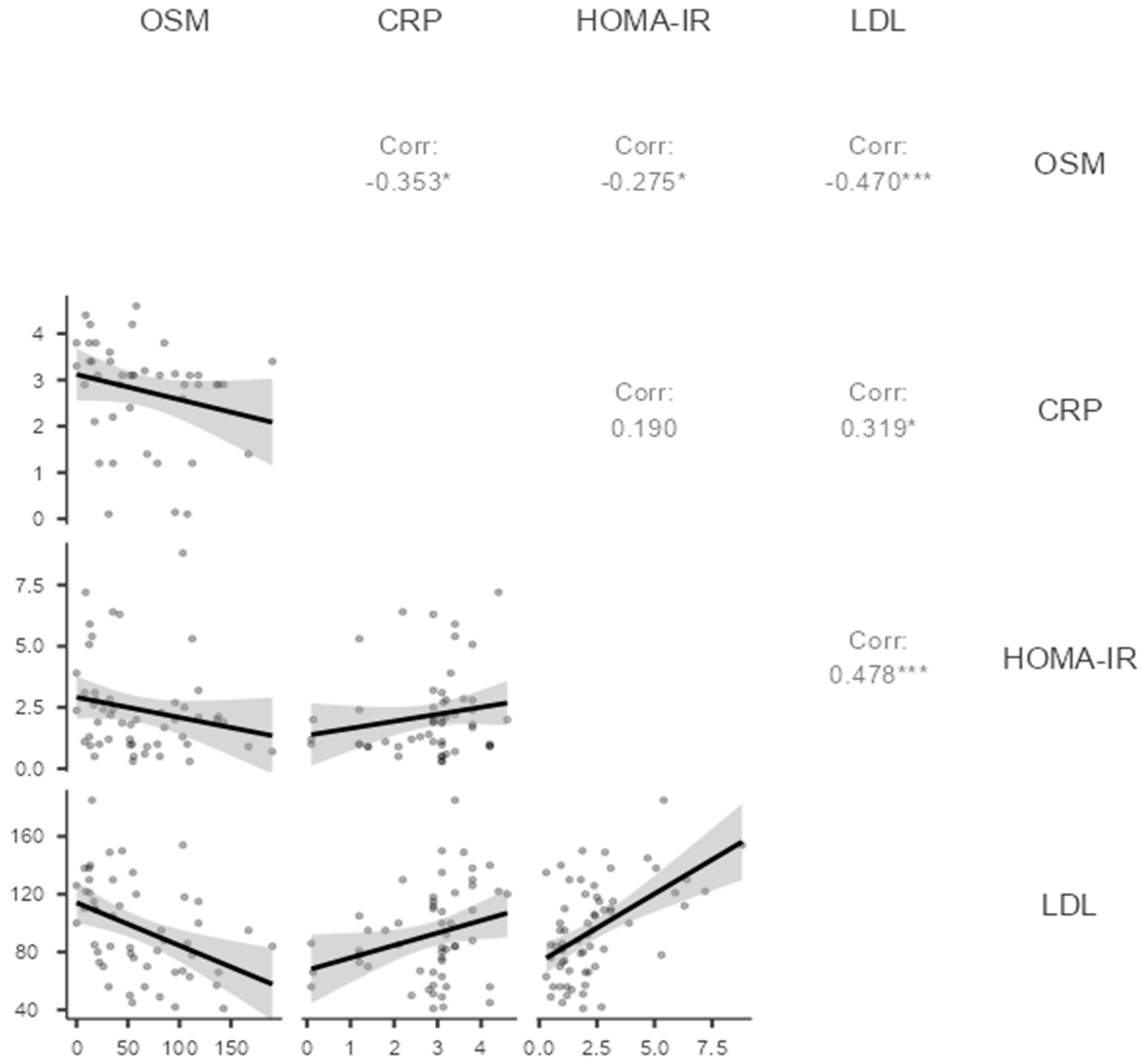
| Fasting glucose | −0.329 | 0.017 * | −0.230 | 0.213 |
| HOMA-IR | −0.275 | 0.048 * | −0.130 | 0.486 |
| Total cholesterol | −0.386 | 0.005 ** | −0.130 | 0.470 |
| LDL cholesterol | −0.470 | <0.001 *** | −0.250 | 0.161 |
| Non-HDL cholesterol | −0.440 | 0.001 | −0.270 | 0.132 |
| LH/FSH ratio | −0.316 | 0.023 | −0.180 | 0.321 |
| Total Testosterone | 0.220 | 0.118 | 0.120 | 0.508 |
| C-reactive protein | −0.353 | 0.019 | −0.140 | 0.433 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Camili, F.E.; Akis, M.; Adali, E.; Hismiogullari, A.A.; Taskin, M.I.; Guney, G.; Afsar, S. Oncostatin M Is Related to Polycystic Ovary Syndrome-Case Control Study. Biomedicines 2024, 12, 355. https://doi.org/10.3390/biomedicines12020355
Camili FE, Akis M, Adali E, Hismiogullari AA, Taskin MI, Guney G, Afsar S. Oncostatin M Is Related to Polycystic Ovary Syndrome-Case Control Study. Biomedicines. 2024; 12(2):355. https://doi.org/10.3390/biomedicines12020355
Chicago/Turabian StyleCamili, Figen Efe, Merve Akis, Ertan Adali, Adnan Adil Hismiogullari, Mine Islimye Taskin, Gurhan Guney, and Selim Afsar. 2024. "Oncostatin M Is Related to Polycystic Ovary Syndrome-Case Control Study" Biomedicines 12, no. 2: 355. https://doi.org/10.3390/biomedicines12020355
APA StyleCamili, F. E., Akis, M., Adali, E., Hismiogullari, A. A., Taskin, M. I., Guney, G., & Afsar, S. (2024). Oncostatin M Is Related to Polycystic Ovary Syndrome-Case Control Study. Biomedicines, 12(2), 355. https://doi.org/10.3390/biomedicines12020355







