COVID-19 on Oral Health: A New Bilateral Connection for the Pandemic
Abstract
:1. Introduction
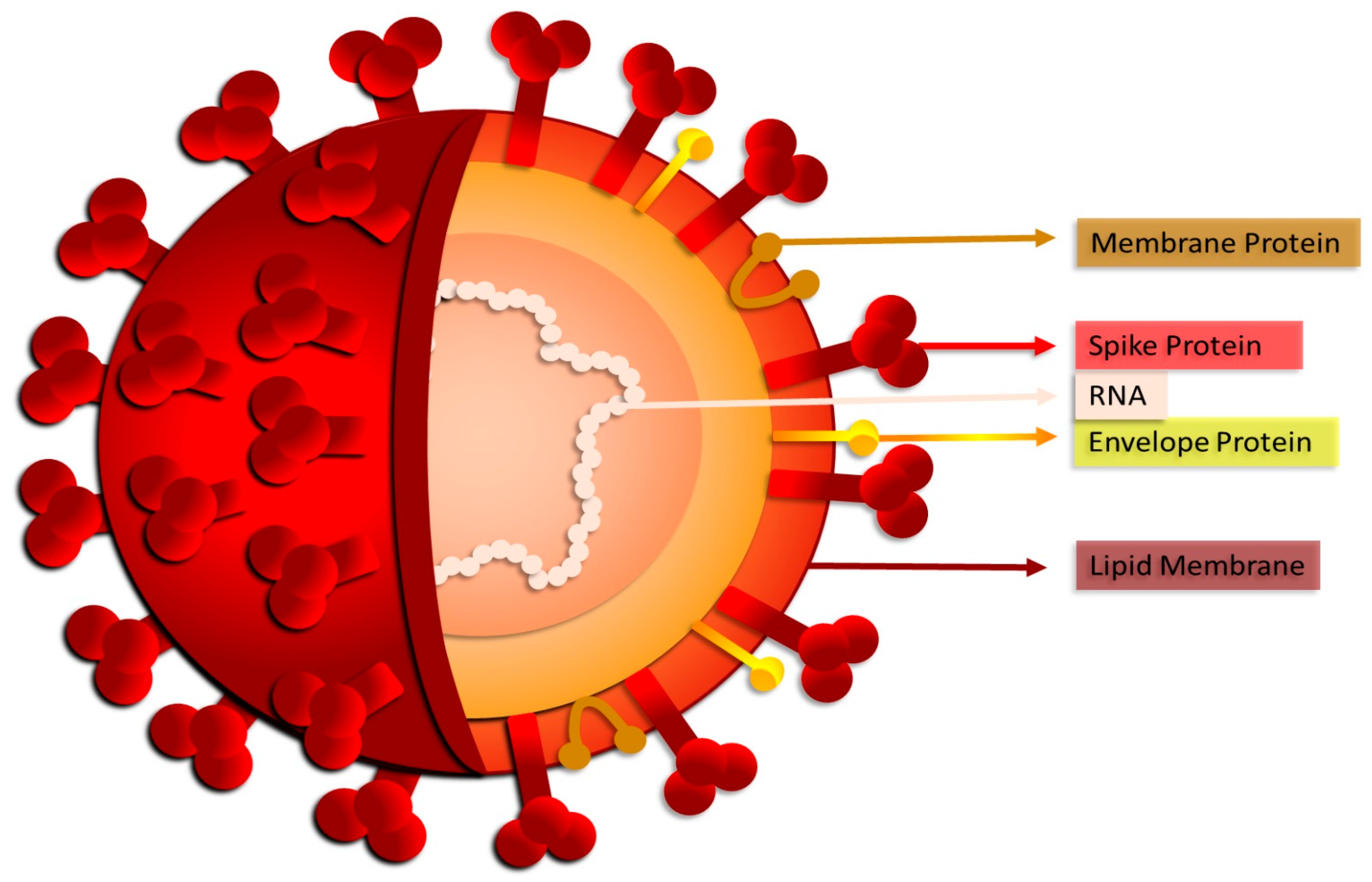
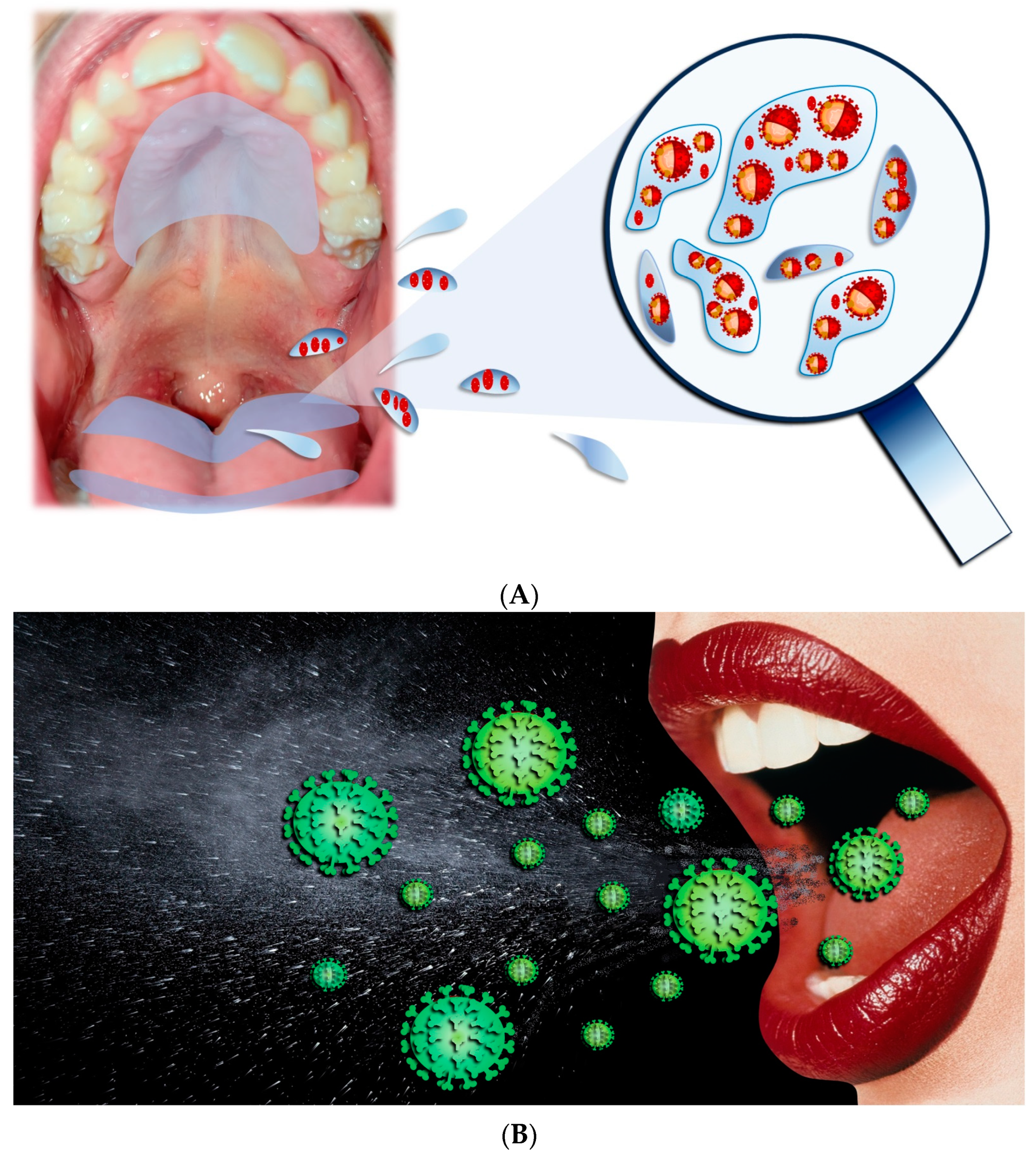
2. SARS-CoV-2 Transmission via the Saliva
3. SARS-CoV-2 and Oral Cavity: A New Entry Route in the Body
3.1. Salivary Glands
- The virus can enter the O.C. through the upper respiratory tract, such as the nose and throat, mainly via respiratory droplets released when an infected person coughs, sneezes, or talks. Viral particles can be inhaled or deposited on the surfaces of the mouth and nose.
- Once in the O.C., the SARS-CoV-2 virus binds to ACE2 receptors present on host cells. This is the entry point of the virus into human cells.
- The virus can penetrate the oral mucosa through adhesion and invasion of the epithelial cells present in this region. This process could be favored by lesions or microlesions in the mucosa, providing an entry route for the virus.
- Once inside the oral mucosa, the virus can be transmitted to the salivary glands via the lymphatic or circulatory system. In saliva, the existence of SARS-CoV-2 has been observed, suggesting that the virus may be transported through the saliva itself or through the bloodstream.
3.2. Tongue
3.3. Oral Mucosa
3.4. Dental Pulp
4. SARS-CoV-2 Infection of O.C. Is Controlled by Different Factors
- -
- Aggravation of periodontitis: Systemic inflammation caused by the COVID-19 infection could affect oral health conditions, including periodontitis. This inflammatory condition of the gums may be exacerbated or worsened due to systemic stress and an altered immune response during the COVID-19 infection.
- -
- Changes in the oral microbiome: some studies have suggested that prolonged use of medical devices such as ventilators or the effect of drugs used to treat COVID-19 could alter the oral microbiome. This could affect the balance of bacteria in your mouth, potentially increasing your risk of developing disease conditions such as periodontitis.
5. O.C. Pathologies Triggered by COVID-19
6. Therapeutic Potential of O.C. against SARS-CoV-2
7. The Role of O.C. in the Diagnosis of COVID-19
8. Clinical Implications
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACEg2 | (Angiotensin Converting Enzyme Type 2) |
| COVID-19 | (Corona Virus Disease, 2019) |
| Iga, IgG, IgM | (Immunoglobulins A, G, and M) |
| Il1β | (Interleukin 1 beta) |
| mRNA | (messanger RiboNucleic Acid) |
| Nrp-1 | (Neuropilin-1) |
| OC | (Oral Cavity) |
| Pck+ | (Pan-Cytokeratin Positive) |
| Pge2 | (Prostaglandin E2) |
| PGLPS | (Porphyromonas Gingivalis-Derived Lipopolysaccharide) |
| Rps System | (Recombinant Poliovirus Sabin-1) |
| SARS-CoV-2 | (Severe Acute Respiratory Syndrome Coronavirus 2) |
| TMPRSS2 | (Transmembrane Serine Protease 2) |
| Tnfα | (Tumor necrosis factor) |
References
- Rusu, L.C.; Ardelean, L.C.; Tigmeanu, C.V.; Matichescu, A.; Sauciur, I.; Bratu, E.A. COVID-19 and Its Repercussions on Oral Health: A Review. Medicina 2021, 57, 1189. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8619825/ (accessed on 21 November 2023). [CrossRef] [PubMed]
- Maggialetti, N.; Piemonte, S.; Sperti, E.; Inchingolo, F.; Greco, S.; Lucarelli, N.M.; De Chirico, P.; Lofino, S.; Coppola, F.; Catacchio, C.; et al. Iatrogenic Barotrauma in COVID-19-Positive Patients: Is It Related to the Pneumonia Severity? Prevalence and Trends of This Complication Over Time. Biomedicines 2022, 10, 2493. [Google Scholar] [CrossRef] [PubMed]
- Villarroel-Dorrego, M.; Chacón, L.; Rosas, R.; Barrios, V.; Pernía, Y.; Vélez, H. [Translated article] Oral Findings in Patients With COVID-19. Actas Dermo-Sifiliográficas 2022, 113, T183–T186. [Google Scholar] [CrossRef]
- Kusiak, A.; Cichońska, D.; Tubaja, M.; Skorek, A.; Jereczek-Fossa, B.A.; Corrao, G.; Marvaso, G.; Alterio, D. COVID-19 Manifestation in the Oral Cavity—A Narrative Literature Review. Acta Otorhinolaryngol. Ital. 2021, 41, 395–400. [Google Scholar] [CrossRef]
- Brandini, D.A.; Takamiya, A.S.; Thakkar, P.; Schaller, S.; Rahat, R.; Naqvi, A.R. COVID-19 and Oral Diseases: Crosstalk, Synergy or Association? Rev. Med. Virol. 2021, 31, e2226. [Google Scholar] [CrossRef]
- Tsuchiya, H. Characterization and Pathogenic Speculation of Xerostomia Associated with COVID-19: A Narrative Review. Dent. J. 2021, 9, 130. [Google Scholar] [CrossRef]
- Dolci, C.; Cenzato, N.; Maspero, C.; Giannini, L.; Khijmatgar, S.; Dipalma, G.; Tartaglia, G.M.; Inchingolo, F. Skull Biomechanics and Simplified Cephalometric Lines for the Estimation of Muscular Lines of Action. J. Pers. Med. 2023, 13, 1569. [Google Scholar] [CrossRef]
- Lee, W.S.; Yousefi, M.; Yan, B.; Yong, C.L.; Ooi, Y.S. Know Your Enemy and Know Yourself—The Case of SARS-CoV-2 Host Factors. Curr. Opin. Virol. 2021, 50, 159–170. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8379091/ (accessed on 21 November 2023). [CrossRef]
- Barthe, M.; Hertereau, L.; Lamghari, N.; Osman-Ponchet, H.; Braud, V.M. Receptors and Cofactors That Contribute to SARS-CoV-2 Entry: Can Skin Be an Alternative Route of Entry? Int. J. Mol. Sci. 2023, 24, 6253. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10094153/ (accessed on 21 November 2023). [CrossRef]
- Scarano, A.; Inchingolo, F.; Lorusso, F. Facial Skin Temperature and Discomfort When Wearing Protective Face Masks: Thermal Infrared Imaging Evaluation and Hands Moving the Mask. Int. J. Environ. Res. Public Health 2020, 17, 4624. [Google Scholar] [CrossRef]
- Bohn, M.K.; Hall, A.; Sepiashvili, L.; Jung, B.; Steele, S.; Adeli, K. Pathophysiology of COVID-19: Mechanisms Underlying Disease Severity and Progression. Physiology 2020, 35, 288. [Google Scholar] [CrossRef]
- Huang, Y.; Yang, C.; Xu, X.; Xu, W.; Liu, S. Structural and Functional Properties of SARS-CoV-2 Spike Protein: Potential Antivirus Drug Development for COVID-19. Acta Pharmacol. Sin. 2020, 41, 1141–1149. [Google Scholar] [CrossRef] [PubMed]
- Jackson, C.B.; Farzan, M.; Chen, B.; Choe, H. Mechanisms of SARS-CoV-2 Entry into Cells. Nat. Rev. Mol. Cell Biol. 2022, 23, 3–20. Available online: https://www.nature.com/articles/s41580-021-00418-x (accessed on 17 November 2023). [CrossRef] [PubMed]
- Mayi, B.S.; Leibowitz, J.A.; Woods, A.T.; Ammon, K.A.; Liu, A.E.; Raja, A. The Role of Neuropilin-1 in COVID-19. PLoS Pathog. 2021, 17, e1009153. Available online: https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1009153 (accessed on 8 November 2023). [CrossRef] [PubMed]
- Singh, M.; Bansal, V.; Feschotte, C. A Single-Cell RNA Expression Map of Human Coronavirus Entry Factors. Cell Rep. 2020, 32, 108175. [Google Scholar] [CrossRef] [PubMed]
- Balzanelli, M.G.; Distratis, P.; Lazzaro, R.; Dipalma, G.; Inchingolo, F.; Del Prete, R.; Hung Pham, V.; Aityan, S.K.; Nguyen, K.C.; Isacco Gargiulo, C. The Long COVID-19 Syndrome the Spike Protein and Stem Cells, the Underrated Role of Retrotransposons, a Working Hypothesis. Preprints 2023, 2023081130. Available online: https://www.preprints.org/manuscript/202308.1130/v1 (accessed on 14 November 2023).
- Demi, L.; Mento, F.; Di Sabatino, A.; Fiengo, A.; Sabatini, U.; Macioce, V.N.; Robol, M.; Tursi, F.; Sofia, C.; Di Cienzo, C.; et al. Lung Ultrasound in COVID-19 and Post-COVID-19 Patients, an Evidence-Based Approach. J. Ultrasound Med. 2022, 41, 2203–2215. [Google Scholar] [CrossRef]
- Khan, U.; Afrakhteh, S.; Mento, F.; Fatima, N.; De Rosa, L.; Custode, L.L.; Azam, Z.; Torri, E.; Soldati, G.; Tursi, F.; et al. Benchmark Methodological Approach for the Application of Artificial Intelligence to Lung Ultrasound Data from COVID-19 Patients: From Frame to Prognostic-Level. Ultrasonics 2023, 132, 106994. [Google Scholar] [CrossRef]
- Ghosh, S.; Dhobley, A.; Avula, K.K.; Joseph, S.; Gavali, N.; Sinha, S. Role of Saliva as a Non-Invasive Diagnostic Method for Detection of COVID-19. Cureus 2022, 14, e27471. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9421123/ (accessed on 26 November 2023). [CrossRef]
- Daniell, H.; Nair, S.K.; Esmaeili, N.; Wakade, G.; Shahid, N.; Ganesan, P.K.; Islam, M.R.; Shepley-McTaggart, A.; Feng, S.; Gary, E.N.; et al. Debulking SARS-CoV-2 in Saliva Using Angiotensin Converting Enzyme 2 in Chewing Gum to Decrease Oral Virus Transmission and Infection. Mol. Ther. 2022, 30, 1966. [Google Scholar] [CrossRef]
- Sungnak, W.; Huang, N.; Bécavin, C.; Berg, M.; Queen, R.; Litvinukova, M.; Talavera-López, C.; Maatz, H.; Reichart, D.; Sampaziotis, F.; et al. SARS-CoV-2 Entry Factors Are Highly Expressed in Nasal Epithelial Cells Together with Innate Immune Genes. Nat. Med. 2020, 26, 681–687. [Google Scholar] [CrossRef] [PubMed]
- Le, T.H.; Balzanelli, M.G.; Le, T.V.; le Quoc, T.; Thuy, D.D.; Distratis, P.; Lazzaro, R.; Prete, R.D.; Triggiano, F.; Gargiulo, C.I.; et al. A Different Perspective on SARS-CoV-2 Pandemic: Data, Outcomes and Demographic Analysis of a Study Conducted at General Hospital Ninh Thuan Province in Vietnam in 2022. Preprint 2023. [Google Scholar] [CrossRef]
- Balzanelli, M.G.; Distratis, P.; Lazzaro, R.; D’Ettorre, E.; Nico, A.; Inchingolo, F.; Dipalma, G.; Tomassone, D.; Serlenga, E.M.; Dalagni, G.; et al. New Translational Trends in Personalized Medicine: Autologous Peripheral Blood Stem Cells and Plasma for COVID-19 Patient. J. Pers. Med. 2022, 12, 85. [Google Scholar] [CrossRef] [PubMed]
- Vaz, S.N.; de Santana, D.S.; Netto, E.M.; Pedroso, C.; Wang, W.-K.; Santos, F.D.A.; Brites, C. Saliva Is a Reliable, Non-Invasive Specimen for SARS-CoV-2 Detection. Braz. J. Infect. Dis. 2020, 24, 422–427. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Inchingolo, F.; Lorusso, F. Environmental Disinfection of a Dental Clinic during the COVID-19 Pandemic: A Narrative Insight. BioMed Res. Int. 2020, 2020, 8896812. [Google Scholar] [CrossRef] [PubMed]
- Lo Giudice, R. The Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) in Dentistry. Management of Biological Risk in Dental Practice. Int. J. Environ. Res. Public Health 2020, 17, 3067. [Google Scholar] [CrossRef] [PubMed]
- Huang, N.; Pérez, P.; Kato, T.; Mikami, Y.; Okuda, K.; Gilmore, R.C.; Conde, C.D.; Gasmi, B.; Stein, S.; Beach, M.; et al. SARS-CoV-2 Infection of the Oral Cavity and Saliva. Nat. Med. 2021, 27, 892–903. [Google Scholar] [CrossRef] [PubMed]
- Demi, L.; Wolfram, F.; Klersy, C.; De Silvestri, A.; Ferretti, V.V.; Muller, M.; Miller, D.; Feletti, F.; Wełnicki, M.; Buda, N.; et al. New International Guidelines and Consensus on the Use of Lung Ultrasound. J. Ultrasound Med. 2023, 42, 309–344. [Google Scholar] [CrossRef]
- Cazzolla, A.P.; Lovero, R.; Spirito, F.; Di Cosola, M.; Santacroce, L.; Muzio, E.L.; Ciavarella, D.; Dioguardi, M.; Crincoli, V.; Pepe, M.; et al. Evaluation of Qualitative and Quantitative Taste Alterations in COVID-19. Biomol. Biomed. 2023, 23, 344. Available online: https://pubmed.ncbi.nlm.nih.gov/35801415/ (accessed on 26 November 2023). [CrossRef]
- Dioguardi, M.; Cazzolla, A.P.; Arena, C.; Sovereto, D.; Caloro, G.A.; Dioguardi, A.; Crincoli, V.; Laino, L.; Troiano, G.; Lo Muzio, L. Innate Immunity in Children and the Role of ACE2 Expression in SARS-CoV-2 Infection. Pediatr. Rep. 2021, 13, 363–382. [Google Scholar] [CrossRef]
- Cazzolla, A.P.; Lovero, R.; Lo Muzio, L.; Testa, N.F.; Schirinzi, A.; Palmieri, G.; Pozzessere, P.; Procacci, V.; Di Comite, M.; Ciavarella, D.; et al. Taste and Smell Disorders in COVID-19 Patients: Role of Interleukin-6. ACS Chem. Neurosci. 2020, 11, 2774–2781. [Google Scholar] [CrossRef] [PubMed]
- Dawes, C. Estimates, from Salivary Analyses, of the Turnover Time of the Oral Mucosal Epithelium in Humans and the Number of Bacteria in an Edentulous Mouth. Arch. Oral Biol. 2003, 48, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Pham, V.H.; Pham, H.T.; Balzanelli, M.G.; Distratis, P.; Lazzaro, R.; Nguyen, Q.V.; Tran, V.Q.; Tran, D.K.; Phan, L.D.; Pham, S.M.; et al. Multiplex RT Real-Time PCR Based on Target Failure to Detect and Identify Different Variants of SARS-CoV-2: A Feasible Method That Can Be Applied in Clinical Laboratories. Diagnostics 2023, 13, 1364. [Google Scholar] [CrossRef] [PubMed]
- Silva, J.; Lucas, C.; Sundaram, M.; Israelow, B.; Wong, P.; Klein, J.; Tokuyama, M.; Lu, P.; Venkataraman, A.; Liu, F.; et al. Saliva Viral Load Is a Dynamic Unifying Correlate of COVID-19 Severity and Mortality. MedRxiv Prepr. Serv. Health Sci. 2021. [Google Scholar] [CrossRef]
- Bustamante-Marin, X.M.; Ostrowski, L.E. Cilia and Mucociliary Clearance. Cold Spring Harb. Perspect. Biol. 2017, 9, a028241. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5378048/ (accessed on 20 December 2023). [CrossRef] [PubMed]
- Xiang, Z.; Koo, H.; Chen, Q.; Zhou, X.; Liu, Y.; Simon-Soro, A. Potential Implications of SARS-CoV-2 Oral Infection in the Host Microbiota. J. Oral Microbiol. 2021, 13, 1853451. [Google Scholar] [CrossRef] [PubMed]
- Mohapatra, R.K.; Dhama, K.; Mishra, S.; Sarangi, A.K.; Kandi, V.; Tiwari, R.; Pintilie, L. The Microbiota-Related Coinfections in COVID-19 Patients: A Real Challenge. Beni-Suef Univ. J. Basic Appl. Sci. 2021, 10, 47. [Google Scholar] [CrossRef]
- Harcourt, J.; Tamin, A.; Lu, X.; Kamili, S.; Sakthivel, S.K.; Murray, J.; Queen, K.; Tao, Y.; Paden, C.R.; Zhang, J.; et al. Severe Acute Respiratory Syndrome Coronavirus 2 from Patient with Coronavirus Disease, United States. Emerg. Infect. Dis. 2020, 26, 1266–1273. [Google Scholar] [CrossRef]
- Marchesan, J.T.; Warner, B.M.; Byrd, K.M. The “Oral” History of COVID-19: Primary Infection, Salivary Transmission, and Post-acute Implications. J. Periodontol. 2021, 92, 1357–1367. [Google Scholar] [CrossRef]
- Drozdzik, A.; Drozdzik, M. Oral Pathology in COVID-19 and SARS-CoV-2 Infection-Molecular Aspects. Int. J. Mol. Sci. 2022, 23, 1431. [Google Scholar] [CrossRef]
- Tang, S.; Mao, Y.; Jones, R.M.; Tan, Q.; Ji, J.S.; Li, N.; Shen, J.; Lv, Y.; Pan, L.; Ding, P.; et al. Aerosol Transmission of SARS-CoV-2? Evidence, Prevention and Control. Environ. Int. 2020, 144, 106039. [Google Scholar] [CrossRef] [PubMed]
- Balzanelli, M.G.; Distratis, P.; Lazzaro, R.; Pham, V.H.; Tran, T.C.; Dipalma, G.; Bianco, A.; Serlenga, E.M.; Aityan, S.K.; Pierangeli, V.; et al. Analysis of Gene Single Nucleotide Polymorphisms in COVID-19 Disease Highlighting the Susceptibility and the Severity towards the Infection. Diagn. Basel 2022, 12, 2824. [Google Scholar] [CrossRef] [PubMed]
- De Maria, L.; Sponselli, S.; Caputi, A.; Stefanizzi, P.; Pipoli, A.; Giannelli, G.; Delvecchio, G.; Tafuri, S.; Inchingolo, F.; Migliore, G.; et al. SARS-CoV-2 Breakthrough Infections in Health Care Workers: An Italian Retrospective Cohort Study on Characteristics, Clinical Course and Outcomes. J. Clin. Med. 2023, 12, 628. [Google Scholar] [CrossRef]
- Zhu, J.; Guo, J.; Xu, Y.; Chen, X. Viral Dynamics of SARS-CoV-2 in Saliva from Infected Patients. J. Infect. 2020, 81, e48–e50. [Google Scholar] [CrossRef] [PubMed]
- Puhach, O.; Meyer, B.; Eckerle, I. SARS-CoV-2 Viral Load and Shedding Kinetics. Nat. Rev. Microbiol. 2023, 21, 147–161. [Google Scholar] [CrossRef] [PubMed]
- Drozdzik, A. COVID-19 and SARS-CoV-2 Infection in Periodontology: A Narrative Review. J. Periodontal Res. 2022, 57, 933–941. [Google Scholar] [CrossRef]
- Badran, Z.; Gaudin, A.; Struillou, X.; Amador, G.; Soueidan, A. Periodontal Pockets: A Potential Reservoir for SARS-CoV-2? Med. Hypotheses 2020, 143, 109907. [Google Scholar] [CrossRef]
- Botros, N.; Iyer, P.; Ojcius, D.M. Is There an Association between Oral Health and Severity of COVID-19 Complications? Biomed. J. 2020, 43, 325–327. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Gargiulo, C.I.; Malcangi, G.; Ciocia, A.M.; Patano, A.; Azzollini, D.; Piras, F.; Barile, G.; Settanni, V.; Mancini, A.; et al. Diagnosis of SARS-CoV-2 during the Pandemic by Multiplex RT-rPCR hCoV Test: Future Perspectives. Pathogens 2022, 11, 1378. [Google Scholar] [CrossRef]
- Fernandes Matuck, B.; Dolhnikoff, M.; Maia, G.V.A.; Isaac Sendyk, D.; Zarpellon, A.; Costa Gomes, S.; Duarte-Neto, A.N.; Rebello Pinho, J.R.; Gomes-Gouvêa, M.S.; Sousa, S.C.O.M.; et al. Periodontal Tissues Are Targets for SARS-CoV-2: A Post-Mortem Study. J. Oral Microbiol. 2020, 13, 1848135. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Malcangi, G.; Ceci, S.; Patano, A.; Corriero, A.; Azzollini, D.; Marinelli, G.; Coloccia, G.; Piras, F.; Barile, G.; et al. Antispike Immunoglobulin-G (IgG) Titer Response of SARS-CoV-2 mRNA-Vaccine (BNT162b2): A Monitoring Study on Healthcare Workers. Biomedicines 2022, 10, 2402. [Google Scholar] [CrossRef]
- Altaie, A.M.; Hamdy, R.; Venkatachalam, T.; Hamoudi, R.; Soliman, S.S.M. Estimating the Viral Loads of SARS-CoV-2 in the Oral Cavity When Complicated with Periapical Lesions. BMC Oral Health 2021, 21, 567. [Google Scholar] [CrossRef] [PubMed]
- Amante, L.F.L.S.; Afonso, J.T.M.; Skrupskelyte, G. Dentistry and the COVID-19 Outbreak. Int. Dent. J. 2021, 71, 358–368. [Google Scholar] [CrossRef] [PubMed]
- Izzetti, R.; Nisi, M.; Gabriele, M.; Graziani, F. COVID-19 Transmission in Dental Practice: Brief Review of Preventive Measures in Italy. J. Dent. Res. 2020, 99, 1030–1038. Available online: https://journals.sagepub.com/doi/full/10.1177/0022034520920580 (accessed on 15 November 2023). [CrossRef] [PubMed]
- Atukorallaya, D.S.; Ratnayake, R.K. Oral Mucosa, Saliva, and COVID-19 Infection in Oral Health Care. Front. Med. 2021, 8, 656926. [Google Scholar] [CrossRef] [PubMed]
- Di Spirito, F.; Amato, A.; Di Palo, M.P.; Contaldo, M.; D’Ambrosio, F.; Lo Giudice, R.; Amato, M. Oral Lesions Following Anti-SARS-CoV-2 Vaccination: A Systematic Review. Int. J. Environ. Res. Public. Health 2022, 19, 10228. [Google Scholar] [CrossRef] [PubMed]
- Coke, C.J.; Davison, B.; Fields, N.; Fletcher, J.; Rollings, J.; Roberson, L.; Challagundla, K.B.; Sampath, C.; Cade, J.; Farmer-Dixon, C.; et al. SARS-CoV-2 Infection and Oral Health: Therapeutic Opportunities and Challenges. J. Clin. Med. 2021, 10, 156. [Google Scholar] [CrossRef]
- Sawa, Y.; Ibaragi, S.; Okui, T.; Yamashita, J.; Ikebe, T.; Harada, H. Expression of SARS-CoV-2 Entry Factors in Human Oral Tissue. J. Anat. 2021, 238, 1341–1354. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Malcangi, G.; Ceci, S.; Patano, A.; Corriero, A.; Vimercati, L.; Azzollini, D.; Marinelli, G.; Coloccia, G.; Piras, F.; et al. Effectiveness of SARS-CoV-2 Vaccines for Short- and Long-Term Immunity: A General Overview for the Pandemic Contrast. Int. J. Mol. Sci. 2022, 23, 8485. [Google Scholar] [CrossRef]
- Zhu, F.; Zhong, Y.; Ji, H.; Ge, R.; Guo, L.; Song, H.; Wu, H.; Jiao, P.; Li, S.; Wang, C.; et al. ACE2 and TMPRSS2 in Human Saliva Can Adsorb to the Oral Mucosal Epithelium. J. Anat. 2022, 240, 398–409. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Ceci, S.; Limongelli, L.; Corriero, A.; Curatoli, L.; Azzollini, D.; Mezzapesa, P.P.; Marinelli, G.; Malcangi, G.; Coloccia, G.; et al. Cavernous Sinus Involvement and Near Miss Mediastinitis Following Mandibular Tooth Infection Treated during the COVID-19 Pandemic: Clinical Diagnosis and Treatment. Case Rep. Dent. 2022, 2022, 8650099. [Google Scholar] [CrossRef] [PubMed]
- Matuck, B.F.; Dolhnikoff, M.; Duarte-Neto, A.N.; Maia, G.; Gomes, S.C.; Sendyk, D.I.; Zarpellon, A.; De Andrade, N.P.; Monteiro, R.A.; Pinho, J.R.R.; et al. Salivary Glands Are a Target for SARS-CoV-2: A Source for Saliva Contamination. J. Pathol. 2021, 254, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, J.; Senpuku, H.; Ogawa, M.; Yasuhara, R.; Ohnuma, S.; Takamatsu, K.; Watanabe, T.; Mabuchi, Y.; Nakamura, S.; Ishida, S.; et al. Human Induced Pluripotent Stem Cell-Derived Salivary Gland Organoids Model SARS-CoV-2 Infection and Replication. Nat. Cell Biol. 2022, 24, 1595–1605. [Google Scholar] [CrossRef] [PubMed]
- Anahtar, M.; Chan, L.W.; Ko, H.; Rao, A.; Soleimany, A.P.; Khatri, P.; Bhatia, S.N. Host Protease Activity Classifies Pneumonia Etiology. Proc. Natl. Acad. Sci. USA 2022, 119, e2121778119. [Google Scholar] [CrossRef] [PubMed]
- Maggialetti, N.; Villanova, I.; Castrì, A.; Greco, C.N.; Inchingolo, F.; Virgilio, D.; Moschetta, M.; Sardaro, A.; Stabile Ianora, A.A.; Scardapane, A. COVID-19 in Italy: Comparison of CT Findings from Time Zero to the Delta Variant. Microorganisms 2022, 10, 796. [Google Scholar] [CrossRef] [PubMed]
- Parigiani, M.A.; Ketscher, A.; Timme, S.; Bronsert, P.; Schlimpert, M.; Kammerer, B.; Jacquel, A.; Chaintreuil, P.; Reinheckel, T. Conditional Gene Targeting Reveals Cell Type-Specific Roles of the Lysosomal Protease Cathepsin L in Mammary Tumor Progression. Cancers 2020, 12, 2004. [Google Scholar] [CrossRef]
- Sudhan, D.R.; Siemann, D.W. Cathepsin L Targeting in Cancer Treatment. Pharmacol. Ther. 2015, 155, 105–116. [Google Scholar] [CrossRef]
- Pascolo, L.; Zupin, L.; Melato, M.; Tricarico, P.; Crovella, S. TMPRSS2 and ACE2 Coexpression in SARS-CoV-2 Salivary Glands Infection. J. Dent. Res. 2020, 99, 002203452093358. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Malcangi, G.; Inchingolo, A.M.; Piras, F.; Settanni, V.; Garofoli, G.; Palmieri, G.; Ceci, S.; Patano, A.; De Leonardis, N.; et al. Benefits and Implications of Resveratrol Supplementation on Microbiota Modulations: A Systematic Review of the Literature. Int. J. Mol. Sci. 2022, 23, 4027. [Google Scholar] [CrossRef]
- GTEx Consortium. The GTEx Consortium Atlas of Genetic Regulatory Effects across Human Tissues. Science 2020, 369, 1318–1330. [Google Scholar] [CrossRef]
- Li, N.; Ye, Y.; Wu, Y.; Li, L.; Hu, J.; Luo, D.; Li, Y.; Yang, J.; Gao, Y.; Hai, W.; et al. Alterations in Histology of the Aging Salivary Gland and Correlation with the Glandular Inflammatory Microenvironment. iScience 2023, 26, 106571. [Google Scholar] [CrossRef] [PubMed]
- Shang, Y.F.; Shen, Y.Y.; Zhang, M.C.; Lv, M.C.; Wang, T.Y.; Chen, X.Q.; Lin, J. Progress in Salivary Glands: Endocrine Glands with Immune Functions. Front. Endocrinol. 2023, 14, 88. [Google Scholar] [CrossRef] [PubMed]
- Pedrosa, M.d.S.; Sipert, C.R.; Nogueira, F.N. Salivary Glands, Saliva and Oral Findings in COVID-19 Infection. Pesqui. Bras. Odontopediatria Clínica Integr. 2020, 20, e0104. [Google Scholar] [CrossRef]
- Santacroce, L.; Charitos, I.A.; Ballini, A.; Inchingolo, F.; Luperto, P.; De Nitto, E.; Topi, S. The Human Respiratory System and Its Microbiome at a Glimpse. Biology 2020, 9, 318. [Google Scholar] [CrossRef] [PubMed]
- Schurink, B.; Roos, E.; Radonic, T.; Barbe, E.; Bouman, C.S.C.; de Boer, H.H.; de Bree, G.J.; Bulle, E.B.; Aronica, E.M.; Florquin, S.; et al. Viral Presence and Immunopathology in Patients with Lethal COVID-19: A Prospective Autopsy Cohort Study. Lancet Microbe 2020, 1, e290–e299. [Google Scholar] [CrossRef]
- Malcangi, G.; Inchingolo, A.D.; Inchingolo, A.M.; Piras, F.; Settanni, V.; Garofoli, G.; Palmieri, G.; Ceci, S.; Patano, A.; Mancini, A.; et al. COVID-19 Infection in Children and Infants: Current Status on Therapies and Vaccines. Child. Basel Switz. 2022, 9, 249. [Google Scholar] [CrossRef]
- Balzanelli, M.G.; Distratis, P.; Dipalma, G.; Vimercati, L.; Catucci, O.; Amatulli, F.; Cefalo, A.; Lazzaro, R.; Palazzo, D.; Aityan, S.K.; et al. Immunity Profiling of COVID-19 Infection, Dynamic Variations of Lymphocyte Subsets, a Comparative Analysis on Four Different Groups. Microorganisms 2021, 9, 2036. [Google Scholar] [CrossRef]
- Harikrishnan, P. Gustatory Dysfunction as an Early Symptom in COVID-19 Screening. J. Craniofac. Surg. 2020. [Google Scholar] [CrossRef]
- Gupta, A.; Bhanushali, S.; Sanap, A.; Shekatkar, M.; Kharat, A.; Raut, C.; Bhonde, R.; Shouche, Y.; Kheur, S.; Sharma, A. Oral Dysbiosis and Its Linkage with SARS-CoV-2 Infection. Microbiol. Res. 2022, 261, 127055. [Google Scholar] [CrossRef]
- Lin, W.; Gao, F.; Wang, X.; Qin, N.; Chen, X.; Tam, K.Y.; Zhang, C.; Zhang, M.; Sha, O. The Oral Manifestations and Related Mechanisms of COVID-19 Caused by SARS-CoV-2 Infection. Front. Cell. Neurosci. 2023, 16, 1006977. [Google Scholar] [CrossRef]
- Tamiya, J.; Sakaguchi, W.; Nakagawa, K.; Yamamoto, T.; Saruta, J.; Kubota, N.; Kawata, A.; Hasegawa, I.; Hamada, N.; Tsukinoki, K. Detection of SARS-CoV-2 and Its Related Factors on the Mucosal Epithelium of the Tongue. Acta Histochem. Cytochem. 2023, 56, 29–37. Available online: https://www.jstage.jst.go.jp/article/ahc/56/2/56_22-00089/_html/-char/ja (accessed on 20 November 2023). [CrossRef] [PubMed]
- Sakaguchi, W.; Kubota, N.; Shimizu, T.; Saruta, J.; Fuchida, S.; Kawata, A.; Yamamoto, Y.; Sugimoto, M.; Yakeishi, M.; Tsukinoki, K. Existence of SARS-CoV-2 Entry Molecules in the Oral Cavity. Int. J. Mol. Sci. 2020, 21, 6000. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Zhong, L.; Deng, J.; Peng, J.; Dan, H.; Zeng, X.; Li, T.; Chen, Q. High Expression of ACE2 Receptor of 2019-nCoV on the Epithelial Cells of Oral Mucosa. Int. J. Oral Sci. 2020, 12, 8. [Google Scholar] [CrossRef] [PubMed]
- Marouf, N.; Cai, W.; Said, K.N.; Daas, H.; Diab, H.; Chinta, V.R.; Hssain, A.A.; Nicolau, B.; Sanz, M.; Tamimi, F. Association between Periodontitis and Severity of COVID-19 Infection: A Case-Control Study. J. Clin. Periodontol. 2021, 48, 483–491. [Google Scholar] [CrossRef] [PubMed]
- Orozco, M.F.S.; Niño-Martínez, N.; Martínez-Castañón, G.-A.; Marín, N.P.; Valencia, C.S.; Velázquez, F.A.D.; Munguía, P.d.C.S.; Santana, M.A.C. Presence of SARS-CoV-2 and Its Entry Factors in Oral Tissues and Cells: A Systematic Review. Medicina 2021, 57, 523. [Google Scholar] [CrossRef] [PubMed]
- Balzanelli, M.G.; Distratis, P.; Lazzaro, R.; Cefalo, A.; Catucci, O.; Aityan, S.K.; Dipalma, G.; Vimercati, L.; Inchingolo, A.D.; Maggiore, M.E.; et al. The Vitamin D, IL-6 and the eGFR Markers a Possible Way to Elucidate the Lung–Heart–Kidney Cross-Talk in COVID-19 Disease: A Foregone Conclusion. Microorganisms 2021, 9, 1903. [Google Scholar] [CrossRef] [PubMed]
- Marques, B.B.F.; Guimarães, T.C.; Fischer, R.G.; Tinoco, J.M.M.; Pires, F.R.; Lima Junior, J.D.C.; Stevens, R.H.; Tinoco, E.M.B. Morphological Alterations in Tongue Epithelial Cells Infected by SARS-CoV-2: A Case–Control Study. Oral Dis. 2022, 28, 2417–2422. Available online: https://onlinelibrary.wiley.com/doi/10.1111/odi.13988 (accessed on 20 November 2023). [CrossRef]
- Cui, J.-Y.; Ting, L.; Cao, Y.-X.; Sun, D.-X.; Bing, L.; Wu, X.-P. Morphology Changes of Maxillary Molar Distalization by Clear Aligner Therapy. Int. J. Morphol. 2022, 40, 920–926. [Google Scholar] [CrossRef]
- ACE2 and Spike Protein Cell Lines for SARS-CoV-2 Investigation|GenScript. Available online: https://www.genscript.com/ace2-stable-cell-lines.html?src=google&utm_source=google&utm_medium=cpc&utm_campaign=PRD-SC.-ACE2_Stable_Cell_Line-TCPA&gad_source=1&gclid=EAIaIQobChMItoyc3ZPSggMV0JKDBx0mpAUaEAAYASAAEgKlv_D_BwE (accessed on 20 November 2023).
- Zhong, M.; Lin, B.; Pathak, J.L.; Gao, H.; Young, A.J.; Wang, X.; Liu, C.; Wu, K.; Liu, M.; Chen, J.-M.; et al. ACE2 and Furin Expressions in Oral Epithelial Cells Possibly Facilitate COVID-19 Infection via Respiratory and Fecal-Oral Routes. Front. Med. 2020, 7, 580796. [Google Scholar] [CrossRef]
- Tsuchiya, H. The Oral Cavity Potentially Serving as a Reservoir for SARS-CoV-2 but Not Necessarily Facilitating the Spread of COVID-19 in Dental Practice. Eur. J. Dent. 2023, 17, 310–318. [Google Scholar] [CrossRef]
- Zipeto, D.; Palmeira, J.D.F.; Argañaraz, G.A.; Argañaraz, E.R. ACE2/ADAM17/TMPRSS2 Interplay May Be the Main Risk Factor for COVID-19. Front. Immunol. 2020, 11, 576745. [Google Scholar] [CrossRef] [PubMed]
- Bosshart, H.; Humphrey, J.; Deignan, E.; Davidson, J.; Drazba, J.; Yuan, L.; Oorschot, V.; Peters, P.J.; Bonifacino, J.S. The Cytoplasmic Domain Mediates Localization of Furin to the Trans- Golgi Network En Route to the Endosomal/Lysosomal System. J. Cell Biol. 1994, 126, 1157–1172. [Google Scholar] [CrossRef] [PubMed]
- Braun, E.; Sauter, D. Furin-mediated Protein Processing in Infectious Diseases and Cancer. Clin. Transl. Immunol. 2019, 8, e1073. [Google Scholar] [CrossRef] [PubMed]
- Shang, J.; Ye, G.; Shi, K.; Wan, Y.; Luo, C.; Aihara, H.; Geng, Q.; Auerbach, A.; Li, F. Structural Basis of Receptor Recognition by SARS-CoV-2. Nature 2020, 581, 221–224. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, M.; Kleine-Weber, H.; Pöhlmann, S. A Multibasic Cleavage Site in the Spike Protein of SARS-CoV-2 Is Essential for Infection of Human Lung Cells. Mol. Cell 2020, 78, 779–784.e5. [Google Scholar] [CrossRef] [PubMed]
- Shang, J.; Wan, Y.; Luo, C.; Ye, G.; Geng, Q.; Auerbach, A.; Li, F. Cell Entry Mechanisms of SARS-CoV-2. Proc. Natl. Acad. Sci. USA 2020, 117, 11727–11734. [Google Scholar] [CrossRef]
- De Oliveira, G.L.V.; Oliveira, C.N.S.; Pinzan, C.F.; de Salis, L.V.V.; Cardoso, C.R.d.B. Microbiota Modulation of the Gut-Lung Axis in COVID-19. Front. Immunol. 2021, 12, 214. [Google Scholar] [CrossRef]
- Ballini, A.; Signorini, L.; Inchingolo, A.M.; Saini, R.; Gnoni, A.; Scacco, S.; Cantore, S.; Dipalma, G.; Inchingolo, F.; Santacroce, L. Probiotics May Improve Serum Folate Availability in Pregnant Women: A Pilot Study. Open Access Maced. J. Med. Sci. 2020, 8, 1124–1130. [Google Scholar] [CrossRef]
- Okui, T.; Matsuda, Y.; Karino, M.; Hideshima, K.; Kanno, T. Oral Mucosa Could Be an Infectious Target of SARS-CoV-2. Healthc. Basel Switz. 2021, 9, 1068. [Google Scholar] [CrossRef]
- Niknam, Z.; Jafari, A.; Golchin, A.; Danesh Pouya, F.; Nemati, M.; Rezaei-Tavirani, M.; Rasmi, Y. Potential Therapeutic Options for COVID-19: An Update on Current Evidence. Eur. J. Med. Res. 2022, 27, 6. [Google Scholar] [CrossRef]
- Bellocchio, L.; Bordea, I.R.; Ballini, A.; Lorusso, F.; Hazballa, D.; Isacco, C.G.; Malcangi, G.; Inchingolo, A.D.; Dipalma, G.; Inchingolo, F.; et al. Environmental Issues and Neurological Manifestations Associated with COVID-19 Pandemic: New Aspects of the Disease? Int. J. Environ. Res. Public Health 2020, 17, 8049. Available online: https://pubmed.ncbi.nlm.nih.gov/33139595/ (accessed on 15 November 2023). [CrossRef] [PubMed]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Krüger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.-H.; Nitsche, A.; et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020, 181, 271–280.e8. [Google Scholar] [CrossRef] [PubMed]
- Balzanelli, M.G.; Distratis, P.; Dipalma, G.; Vimercati, L.; Inchingolo, A.D.; Lazzaro, R.; Aityan, S.K.; Maggiore, M.E.; Mancini, A.; Laforgia, R.; et al. SARS-CoV-2 Virus Infection May Interfere CD34+ Hematopoietic Stem Cells and Megakaryocyte-Erythroid Progenitors Differentiation Contributing to Platelet Defection towards Insurgence of Thrombocytopenia and Thrombophilia. Microorganisms 2021, 9, 1632. [Google Scholar] [CrossRef] [PubMed]
- Patano, A.; Cirulli, N.; Beretta, M.; Plantamura, P.; Inchingolo, A.D.; Inchingolo, A.M.; Bordea, I.R.; Malcangi, G.; Marinelli, G.; Scarano, A.; et al. Education Technology in Orthodontics and Paediatric Dentistry during the COVID-19 Pandemic: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 6056. [Google Scholar] [CrossRef] [PubMed]
- Vieira Braga, F.A.; Kar, G.; Berg, M.; Carpaij, O.A.; Polanski, K.; Simon, L.M.; Brouwer, S.; Gomes, T.; Hesse, L.; Jiang, J.; et al. A Cellular Census of Human Lungs Identifies Novel Cell States in Health and in Asthma. Nat. Med. 2019, 25, 1153–1163. [Google Scholar] [CrossRef] [PubMed]
- Smillie, C.S.; Biton, M.; Ordovas-Montanes, J.; Sullivan, K.M.; Burgin, G.; Graham, D.B.; Herbst, R.H.; Rogel, N.; Slyper, M.; Waldman, J.; et al. Intra- and Inter-Cellular Rewiring of the Human Colon during Ulcerative Colitis. Cell 2019, 178, 714–730.e22. [Google Scholar] [CrossRef] [PubMed]
- Mather, M.W.; Jardine, L.; Talks, B.; Gardner, L.; Haniffa, M. Complexity of Immune Responses in COVID-19. Semin. Immunol. 2021, 55, 101545. [Google Scholar] [CrossRef]
- Sarode, S.C.; Sarode, G.S. Saliva Sample and SARS-CoV-2 Detection: More Complexities than Clarity. J. Oral Biol. Craniofacial Res. 2021, 11, 500–501. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Dipalma, G.; Inchingolo, A.M.; Malcangi, G.; Santacroce, L.; D’Oria, M.T.; Isacco, C.G.; Bordea, I.R.; Candrea, S.; Scarano, A.; et al. The 15-Months Clinical Experience of SARS-CoV-2: A Literature Review of Therapies and Adjuvants. Antioxidants 2021, 10, 881. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Inchingolo, A.M.; Bordea, I.R.; Malcangi, G.; Xhajanka, E.; Scarano, A.; Lorusso, F.; Farronato, M.; Tartaglia, G.M.; Isacco, C.G.; et al. SARS-CoV-2 Disease through Viral Genomic and Receptor Implications: An Overview of Diagnostic and Immunology Breakthroughs. Microorganisms 2021, 9, 793. [Google Scholar] [CrossRef]
- Alsulami, M.; Kattan, W.; Alsamadani, L.; Alahmari, G.; Al Juhani, W.; Almabadi, M. An Outlook on Dental Practices to Avoid the Oral Transmission of COVID-19. Microorganisms 2023, 11, 146. [Google Scholar] [CrossRef] [PubMed]
- Knyazev, E.; Nersisyan, S.; Tonevitsky, A. Endocytosis and Transcytosis of SARS-CoV-2 Across the Intestinal Epithelium and Other Tissue Barriers. Front. Immunol. 2021, 12, 636966. [Google Scholar] [CrossRef] [PubMed]
- Galicia, J.C.; Guzzi, P.H.; Giorgi, F.M.; Khan, A.A. Predicting the Response of the Dental Pulp to SARS-CoV2 Infection: A Transcriptome-Wide Effect Cross-Analysis. Genes Immun. 2020, 21, 360–363. [Google Scholar] [CrossRef] [PubMed]
- Karnik, M.; Beeraka, N.M.; Uthaiah, C.A.; Nataraj, S.M.; Bettadapura, A.D.S.; Aliev, G.; Madhunapantula, S.V. A Review on SARS-CoV-2-Induced Neuroinflammation, Neurodevelopmental Complications, and Recent Updates on the Vaccine Development. Mol. Neurobiol. 2021, 58, 4535–4563. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Inchingolo, F.; Rapone, B.; Festa, F.; Tari, S.R.; Lorusso, F. Protective Face Masks: Effect on the Oxygenation and Heart Rate Status of Oral Surgeons during Surgery. Int. J. Environ. Res. Public Health 2021, 18, 2363. [Google Scholar] [CrossRef] [PubMed]
- Peng, J.; Sun, J.; Zhao, J.; Deng, X.; Guo, F.; Chen, L. Age and Gender Differences in ACE2 and TMPRSS2 Expressions in Oral Epithelial Cells. J. Transl. Med. 2021, 19, 358. [Google Scholar] [CrossRef] [PubMed]
- Balzanelli, M.G.; Distratis, P.; Catucci, O.; Cefalo, A.; Lazzaro, R.; Inchingolo, F.; Tomassone, D.; Aityan, S.K.; Ballini, A.; Nguyen, K.C.D.; et al. Mesenchymal Stem Cells: The Secret Children’s Weapons against the SARS-CoV-2 Lethal Infection. Appl. Sci. 2021, 11, 1696. [Google Scholar] [CrossRef]
- Barker, H.; Parkkila, S. Bioinformatic Characterization of Angiotensin-Converting Enzyme 2, the Entry Receptor for SARS-CoV-2. PLoS ONE 2020, 15, e0240647. [Google Scholar] [CrossRef]
- Sena, K.; Furue, K.; Setoguchi, F.; Noguchi, K. Altered Expression of SARS-CoV-2 Entry and Processing Genes by Porphyromonas Gingivalis-Derived Lipopolysaccharide, Inflammatory Cytokines and Prostaglandin E2 in Human Gingival Fibroblasts. Arch. Oral Biol. 2021, 129, 105201. [Google Scholar] [CrossRef]
- Kheur, S.; Kheur, M.; Gupta, A.A.; Raj, A.T. Is the Gingival Sulcus a Potential Niche for SARS-Corona Virus-2? Med. Hypotheses 2020, 143, 109892. [Google Scholar] [CrossRef]
- Gao, M.; Yang, L.; Chen, X.; Deng, Y.; Yang, S.; Xu, H.; Chen, Z.; Gao, X. A Study on Infectivity of Asymptomatic SARS-CoV-2 Carriers. Respir. Med. 2020, 169, 106026. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.-R.; Deng, D.-T.; Wu, N.; Yang, B.; Li, H.-J.; Pan, X.-B. Persistent Viral RNA Positivity during the Recovery Period of a Patient with SARS-CoV-2 Infection. J. Med. Virol. 2020, 92, 1681–1683. [Google Scholar] [CrossRef] [PubMed]
- Aldosari, L.I.N.; Hassan, S.A.B.; Alshahrani, A.A.; Alshadidi, A.A.F.; Ronsivalle, V.; Marrapodi, M.M.; Cicciù, M.; Minervini, G. Prevalence of Temporomandibular Disorders among Psychoactive Substances Abusers: A Systematic Review and Meta-analysis. J. Oral Rehabil. 2023, 50, 894–901. Available online: https://onlinelibrary.wiley.com/doi/full/10.1111/joor.13513?casa_token=41E-zPMqtc4AAAAA%3AE8WQlBlTwR4z-JAjRjag52Hh5swxt53Kx0EciKArZkVRNL9Bs-Tg1LW5xvS4nJG1U2zWlpWXTKxuwqs (accessed on 26 November 2023). [CrossRef]
- Zhao, M.; Xie, Y.; Gao, W.; Li, C.; Ye, Q.; Li, Y. Diabetes Mellitus Promotes Susceptibility to Periodontitis—Novel Insight into the Molecular Mechanisms. Front. Endocrinol. 2023, 14, 1192625. [Google Scholar] [CrossRef] [PubMed]
- Gorbunkova, A.; Pagni, G.; Brizhak, A.; Farronato, G.; Rasperini, G. Impact of Orthodontic Treatment on Periodontal Tissues: A Narrative Review of Multidisciplinary Literature. Int. J. Dent. 2016, 2016, 4723589. [Google Scholar] [CrossRef]
- Li, G.; He, X.; Zhang, L.; Ran, Q.; Wang, J.; Xiong, A.; Wu, D.; Chen, F.; Sun, J.; Chang, C. Assessing ACE2 Expression Patterns in Lung Tissues in the Pathogenesis of COVID-19. J. Autoimmun. 2020, 112, 102463. [Google Scholar] [CrossRef]
- Gkogkou, E.; Barnasas, G.; Vougas, K.; Trougakos, I.P. Expression Profiling Meta-Analysis of ACE2 and TMPRSS2, the Putative Anti-Inflammatory Receptor and Priming Protease of SARS-CoV-2 in Human Cells, and Identification of Putative Modulators. Redox Biol. 2020, 36, 101615. [Google Scholar] [CrossRef]
- Charitos, I.A.; Del Prete, R.; Inchingolo, F.; Mosca, A.; Carretta, D.; Ballini, A.; Santacroce, L. What We Have Learned for the Future about COVID-19 and Healthcare Management of It? Acta Bio-Medica Atenei Parm. 2020, 91, e2020126. [Google Scholar] [CrossRef]
- Rashedi, J.; Poor, B.M.; Asgharzadeh, V.; Pourostadi, M.; Kafil, H.S.; Vegari, A.; Tayebi-khosroshahi, H.; Asgharzadeh, M. Risk Factors for COVID-19. Le Infez. Med. 2020, 4, 469–474. [Google Scholar]
- Tosif, S.; Neeland, M.R.; Sutton, P.; Licciardi, P.V.; Sarkar, S.; Selva, K.J.; Do, L.A.H.; Donato, C.; Quan Toh, Z.; Higgins, R.; et al. Immune Responses to SARS-CoV-2 in Three Children of Parents with Symptomatic COVID-19. Nat. Commun. 2020, 11, 5703. [Google Scholar] [CrossRef]
- Garziano, M.; Utyro, O.; Strizzi, S.; Vanetti, C.; Saulle, I.; Conforti, C.; Cicilano, F.; Ardizzone, F.; Cappelletti, G.; Clerici, M.; et al. Saliva and Plasma Neutralizing Activity Induced by the Administration of a Third Bnt162b2 Vaccine Dose. Int. J. Mol. Sci. 2022, 23, 14341. [Google Scholar] [CrossRef] [PubMed]
- Tyagi, R.; Basu, S.; Dhar, A.; Gupta, S.; Gupta, S.L.; Jaiswal, R.K. Role of Immunoglobulin A in COVID-19 and Influenza Infections. Vaccines 2023, 11, 1647. [Google Scholar] [CrossRef] [PubMed]
- Sterlin, D.; Mathian, A.; Miyara, M.; Mohr, A.; Anna, F.; Claër, L.; Quentric, P.; Fadlallah, J.; Devilliers, H.; Ghillani, P.; et al. IgA Dominates the Early Neutralizing Antibody Response to SARS-CoV-2. Sci. Transl. Med. 2021, 13, eabd2223. [Google Scholar] [CrossRef] [PubMed]
- D’Apuzzo, F.; Rotolo, R.P.; Nucci, L.; Simeon, V.; Minervini, G.; Grassia, V. Protective Masks during the SARS-CoV-2 Pandemic: Any Relationship with Temporomandibular Disorders and Orofacial Pain? J. Oral Rehabil. 2023, 50, 767–774. [Google Scholar] [CrossRef] [PubMed]
- Pellegrino, F.; Mazzone, E.; Stabile, A.; Beauval, J.B.; Marra, G.; Campi, R.; Afferi, L.; Zhuang, J.; Sorce, G.; Rosiello, G.; et al. Impact of the Time Elapsed between Prostate Biopsy and Surgery on the Accuracy of Nomograms Predicting Lymph Node Invasion in Patients with Clinically Localized Prostate Cancer. Urol. Oncol. 2023, 41, 387.e17–387.e25. [Google Scholar] [CrossRef] [PubMed]
- Bian, J.; Li, Z. Angiotensin-Converting Enzyme 2 (ACE2): SARS-CoV-2 Receptor and RAS Modulator. Acta Pharm. Sin. B 2021, 11, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Theda, C.; Hwang, S.H.; Czajko, A.; Loke, Y.J.; Leong, P.; Craig, J.M. Quantitation of the Cellular Content of Saliva and Buccal Swab Samples. Sci. Rep. 2018, 8, 6944. [Google Scholar] [CrossRef]
- Baima, G.; Marruganti, C.; Sanz, M.; Aimetti, M.; Romandini, M. Periodontitis and COVID-19: Biological Mechanisms and Meta-Analyses of Epidemiological Evidence. J. Dent. Res. 2022, 101, 1430–1440. Available online: https://journals.sagepub.com/doi/10.1177/00220345221104725?icid=int.sj-full-text.citing-articles.37 (accessed on 26 November 2023). [CrossRef]
- Almeida-da-Silva, C.L.C.; Matshik Dakafay, H.; Liu, K.; Ojcius, D.M. Cigarette Smoke Stimulates SARS-CoV-2 Internalization by Activating AhR and Increasing ACE2 Expression in Human Gingival Epithelial Cells. Int. J. Mol. Sci. 2021, 22, 7669. [Google Scholar] [CrossRef]
- Zecchino, S. Impact of COVID-19 Pandemic on in-Hospital Outcomes for Patients with Acute Coronary Syndrome: A Propensity-Weighted, Multicentre Study. Eur. Heart J. Suppl. J. Eur. Soc. Cardiol. 2021, 23, suab135-014. [Google Scholar] [CrossRef]
- Licordari, R.; Sticchi, A.; Mancuso, F.; Caracciolo, A.; Muscoli, S.; Iacovelli, F.; Ruggiero, R.; Scoccia, A.; Cammalleri, V.; Pavani, M.; et al. The Incidence and Impact of In-Hospital Bleeding in Patients with Acute Coronary Syndrome during the COVID-19 Pandemic. J. Clin. Med. 2022, 11, 2926. [Google Scholar] [CrossRef] [PubMed]
- Capurso, G.; Archibugi, L.; Vanella, G.; Testoni, S.G.G.; Petrone, M.C.; Fanti, L.; Greco, S.; Cavenati, S.; Gaffuri, N.; Lella, F.; et al. Infection Control Practices and Outcomes of Endoscopy Units in the Lombardy Region of Italy: A Survey From the Italian Society of Digestive Endoscopy During COVID-19 Spread. J. Clin. Gastroenterol. 2021, 55, e87–e91. [Google Scholar] [CrossRef] [PubMed]
- Salehi, Z.; Motlagh Ghoochani, B.F.N.; Hasani Nourian, Y.; Jamalkandi, S.A.; Ghanei, M. The Controversial Effect of Smoking and Nicotine in SARS-CoV-2 Infection. Allergy Asthma Clin. Immunol. 2023, 19, 49. Available online: https://aacijournal.biomedcentral.com/articles/10.1186/s13223-023-00797-0 (accessed on 26 November 2023). [CrossRef] [PubMed]
- Simons, D.; Shahab, L.; Brown, J.; Perski, O. The Association of Smoking Status with SARS-CoV-2 Infection, Hospitalisation and Mortality from COVID-19: A Living Rapid Evidence Review with Bayesian Meta-Analyses (Version 8)—Article (Preprint v9). Qeios 2020. Available online: https://www.qeios.com/read/UJR2AW.9 (accessed on 26 November 2023).
- Diamond, G.; Figgins, E.L.; Robinson, T.; Senitko, M.; Abraham, G.E.; Williams, H.B.; Sloan, M.; Owings, A.; Laird, H.; Pride, Y.; et al. Examination of Gene Expression in Saliva Samples from COVID-19 Patients to Study the Host Defense Response against SARS-CoV-2 in the Oral Cavity. Mol. Oral Microbiol. 2021, 36, 157–158. [Google Scholar] [CrossRef] [PubMed]
- Perri, F.; Crispo, A.; Ionna, F.; Muto, P.; Caponigro, F.; Longo, F.; Montagnese, C.; Franco, P.; Pavone, E.; Aversa, C.; et al. Patients Affected by Squamous Cell Carcinoma of the Head and Neck: A Population Particularly Prone to Developing Severe Forms of COVID-19. Exp. Ther. Med. 2021, 22, 1298. [Google Scholar] [CrossRef] [PubMed]
- Kumar, H.; Nishat, R.; Desai, A. A Review on Oral Manifestations of COVID-19 Disease. J. Fam. Med. Prim. Care 2022, 11, 5879–5886. [Google Scholar] [CrossRef]
- Iyer, P.; Chino, T.; Ojcius, D.M. Infection of the Oral Cavity with SARS-CoV-2 Variants: Scope of Salivary Diagnostics. Front. Oral Health 2022, 3, 1001790. [Google Scholar] [CrossRef]
- Karlsson, A.C.; Humbert, M.; Buggert, M. The Known Unknowns of T Cell Immunity to COVID-19. Sci. Immunol. 2020, 5, eabe8063. [Google Scholar] [CrossRef]
- Balzanelli, M.G.; Distratis, P.; Aityan, S.K.; Amatulli, F.; Catucci, O.; Cefalo, A.; De Michele, A.; Dipalma, G.; Inchingolo, F.; Lazzaro, R.; et al. An Alternative “Trojan Horse” Hypothesis for COVID-19: Immune Deficiency of IL-10 and SARS-CoV-2 Biology. Endocr. Metab. Immune Disord. Drug Targets 2022, 22, 1–5. [Google Scholar] [CrossRef]
- Jasmer, K.J.; Gilman, K.E.; Muñoz Forti, K.; Weisman, G.A.; Limesand, K.H. Radiation-Induced Salivary Gland Dysfunction: Mechanisms, Therapeutics and Future Directions. J. Clin. Med. 2020, 9, 4095. Available online: https://www.mdpi.com/2077-0383/9/12/4095 (accessed on 26 November 2023). [CrossRef] [PubMed]
- Sreenivasalu, P.K.P.; Dora, C.P.; Swami, R.; Jasthi, V.C.; Shiroorkar, P.N.; Nagaraja, S.; Asdaq, S.M.B.; Anwer, M.K. Nanomaterials in Dentistry: Current Applications and Future Scope. Nanomaterials 2022, 12, 1676. [Google Scholar] [CrossRef] [PubMed]
- Saccomanno, S.; Quinzi, V.; Albani, A.; D’Andrea, N.; Marzo, G.; Macchiarelli, G. Utility of Teleorthodontics in Orthodontic Emergencies during the COVID-19 Pandemic: A Systematic Review. Healthcare 2022, 10, 1108. [Google Scholar] [CrossRef] [PubMed]
- Hannum, M.E.; Koch, R.J.; Ramirez, V.A.; Marks, S.S.; Toskala, A.K.; Herriman, R.D.; Lin, C.; Joseph, P.V.; Reed, D.R. Taste Loss as a Distinct Symptom of COVID-19: A Systematic Review and Meta-Analysis. Chem. Senses 2022, 47, bjac001. [Google Scholar] [CrossRef]
- Karmous, I.; Sayed Khan, A.; Sahnoun, I.; Ben Othman, R.; Ben Jemaa, H.; Mahjoub, F.; Gamoudi, A.; Douik El Gharbi, L.; Mestiri, T.; Khan, N.A.; et al. Loss of Sour Taste Is the Striking Feature among Four Basic Taste Qualities in Tunisian COVID-19 Patients. J. Clin. Med. 2023, 12, 597. [Google Scholar] [CrossRef] [PubMed]
- Doyle, M.E.; Appleton, A.; Liu, Q.-R.; Yao, Q.; Mazucanti, C.H.; Egan, J.M. Human Type II Taste Cells Express Angiotensin-Converting Enzyme 2 and Are Infected by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). Am. J. Pathol. 2021, 191, 1511–1519. [Google Scholar] [CrossRef] [PubMed]
- Riestra-Ayora, J.; Yanes-Diaz, J.; Esteban-Sanchez, J.; Vaduva, C.; Molina-Quiros, C.; Larran-Jimenez, A.; Martin-Sanz, E. Long-Term Follow-up of Olfactory and Gustatory Dysfunction in COVID-19: 6 Months Case-Control Study of Health Workers. Eur. Arch. Oto-Rhino-Laryngol. 2021, 278, 4831–4837. [Google Scholar] [CrossRef]
- Kumar, S.; Thambiraja, T.S.; Karuppanan, K.; Subramaniam, G. Omicron and Delta Variant of SARS-CoV-2: A Comparative Computational Study of Spike Protein. J. Med. Virol. 2022, 94, 1641–1649. [Google Scholar] [CrossRef]
- Zhao, H.; Lu, L.; Peng, Z.; Chen, L.-L.; Meng, X.; Zhang, C.; Ip, J.D.; Chan, W.-M.; Chu, A.W.-H.; Chan, K.-H.; et al. SARS-CoV-2 Omicron Variant Shows Less Efficient Replication and Fusion Activity When Compared with Delta Variant in TMPRSS2-Expressed Cells. Emerg. Microbes Infect. 2022, 11, 277–283. [Google Scholar] [CrossRef]
- Shuai, H.; Chan, J.F.-W.; Hu, B.; Chai, Y.; Yuen, T.T.-T.; Yin, F.; Huang, X.; Yoon, C.; Hu, J.-C.; Liu, H.; et al. Attenuated Replication and Pathogenicity of SARS-CoV-2 B.1.1.529 Omicron. Nature 2022, 603, 693–699. [Google Scholar] [CrossRef]
- Wang, T.-E.; Chao, T.-L.; Tsai, H.-T.; Lin, P.-H.; Tsai, Y.-L.; Chang, S.-Y. Differentiation of Cytopathic Effects (CPE) Induced by Influenza Virus Infection Using Deep Convolutional Neural Networks (CNN). PLoS Comput. Biol. 2020, 16, e1007883. [Google Scholar] [CrossRef] [PubMed]
- Santacroce, L.; Inchingolo, F.; Topi, S.; Del Prete, R.; Di Cosola, M.; Charitos, I.A.; Montagnani, M. Potential Beneficial Role of Probiotics on the Outcome of COVID-19 Patients: An Evolving Perspective. Diabetes Metab. Syndr. 2021, 15, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Scannapieco, F.A. Role of Oral Bacteria in Respiratory Infection. J. Periodontol. 1999, 70, 793–802. [Google Scholar] [CrossRef]
- Lee, E.; Lee, S.-W. Prevalence of Periodontitis and Its Association with Reduced Pulmonary Function: Results from the Korean National Health and Nutrition Examination Survey. Medicina 2019, 55, 581. [Google Scholar] [CrossRef] [PubMed]
- Paju, S.; Scannapieco, F.A. Oral Biofilms, Periodontitis, and Pulmonary Infections. Oral Dis. 2007, 13, 508–512. Available online: https://onlinelibrary.wiley.com/doi/10.1111/j.1601-0825.2007.01410a.x (accessed on 20 November 2023). [CrossRef] [PubMed]
- Bordea, I.R.; Xhajanka, E.; Candrea, S.; Bran, S.; Onișor, F.; Inchingolo, A.D.; Malcangi, G.; Pham, V.H.; Inchingolo, A.M.; Scarano, A.; et al. Coronavirus (SARS-CoV-2) Pandemic: Future Challenges for Dental Practitioners. Microorganisms 2020, 8, 1704. [Google Scholar] [CrossRef] [PubMed]
- Lin, E.-C.; Chiang, Y.-C.; Lin, H.-Y.; Tseng, S.-Y.; Hsieh, Y.-T.; Shieh, J.-A.; Huang, Y.-H.; Tsai, H.-T.; Feng, S.-W.; Peng, T.-Y.; et al. Unraveling the Link between Periodontitis and Coronavirus Disease 2019: Exploring Pathogenic Pathways and Clinical Implications. Biomedicines 2023, 11, 2789. [Google Scholar] [CrossRef] [PubMed]
- Øilo, M.; Bakken, V. Biofilm and Dental Biomaterials. Materials 2015, 8, 2887–2900. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5455733/ (accessed on 21 November 2023). [CrossRef]
- Smargiassi, A.; Soldati, G.; Borghetti, A.; Scoppettuolo, G.; Tamburrini, E.; Testa, A.C.; Moro, F.; Natale, L.; Larici, A.R.; Buonsenso, D.; et al. Lung Ultrasonography for Early Management of Patients with Respiratory Symptoms during COVID-19 Pandemic. J. Ultrasound 2020, 23, 449–456. [Google Scholar] [CrossRef]
- Warabi, Y.; Tobisawa, S.; Kawazoe, T.; Murayama, A.; Norioka, R.; Morishima, R.; Inoue, T.; Shimizu, T.; Takahashi, K. Effects of Oral Care on Prolonged Viral Shedding in Coronavirus Disease 2019 (COVID-19). Spec. Care Dentist. 2020, 40, 470–474. [Google Scholar] [CrossRef]
- Chumpitaz-Cerrate, V.; Chávez-Rimache, L.; Ruiz-Ramirez, E.; Franco-Quino, C.; Erazo-Paredes, C. Evaluation of Current Evidence on the Use of Oral Antiseptics Against SARS-CoV-2: A Narrative Review. J. Int. Soc. Prev. Community Dent. 2022, 12, 488. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9753926/ (accessed on 21 November 2023). [CrossRef] [PubMed]
- Mateos-Moreno, M.V.; Mira, A.; Ausina-Márquez, V.; Ferrer, M.D. Oral Antiseptics against Coronavirus: In-Vitro and Clinical Evidence. J. Hosp. Infect. 2021, 113, 30–43. [Google Scholar] [CrossRef] [PubMed]
- Pfab, F.; Buelow-Johansen, B.; Alber, D.; Kriner, M.; Kornmann, O.; Stuermer, M. Reduction of SARS-CoV-2 Viral Load in Exhaled Air by Antiseptic Chewing Gum: A Pilot Trial. Infection 2023, 51, 881–885. [Google Scholar] [CrossRef] [PubMed]
- Tateyama-Makino, R.; Abe-Yutori, M.; Iwamoto, T.; Tsutsumi, K.; Tsuji, M.; Morishita, S.; Kurita, K.; Yamamoto, Y.; Nishinaga, E.; Tsukinoki, K. The Inhibitory Effects of Toothpaste and Mouthwash Ingredients on the Interaction between the SARS-CoV-2 Spike Protein and ACE2, and the Protease Activity of TMPRSS2 in Vitro. PLoS ONE 2021, 16, e0257705. [Google Scholar] [CrossRef]
- Ting, M.; Suzuki, J.B. The In Vitro Virucidal Effects of Mouthwashes on SARS-CoV-2. Int. J. Transl. Med. 2022, 2, 387–397. [Google Scholar] [CrossRef]
- Bertelli, M.; Kiani, A.K.; Paolacci, S.; Manara, E.; Kurti, D.; Dhuli, K.; Bushati, V.; Miertus, J.; Pangallo, D.; Baglivo, M.; et al. Hydroxytyrosol: A Natural Compound with Promising Pharmacological Activities. J. Biotechnol. 2020, 309, 29–33. [Google Scholar] [CrossRef] [PubMed]
- Sticchi, A.; Costa, F.; Muscoli, S.; Zilio, F.; Buono, A.; Ruggiero, R.; Scoccia, A.; Caracciolo, A.; Licordari, R.; Cammalleri, V.; et al. Symptoms-to-Emergency-Call Timing Delay in Acute Coronary Syndrome before and during COVID-19: Independent Predictors and Their Impact on Mortality. Minerva Cardiol. Angiol. 2023, 71, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Ashraf, M.U.; Kim, Y.; Kumar, S.; Seo, D.; Ashraf, M.; Bae, Y.-S. COVID-19 Vaccines (Revisited) and Oral-Mucosal Vector System as a Potential Vaccine Platform. Vaccines 2021, 9, 171. [Google Scholar] [CrossRef]
- Zhang, L.; Yao, L.; Guo, Y.; Li, X.; Ma, L.; Sun, R.; Han, X.; Liu, J.; Huang, J. Oral SARS-CoV-2 Spike Protein Recombinant Yeast Candidate Prompts Specific Antibody and Gut Microbiota Reconstruction in Mice. Front. Microbiol. 2022, 13, 792532. [Google Scholar] [CrossRef]
- Ra, H.; Jw, C. The Open-Air Treatment of Pandemic Influenza. Am. J. Public Health 2009, 99 (Suppl. S2), S236–S242. [Google Scholar] [CrossRef]
- Roberts, J.D.; Tehrani, S.O. Environments, Behaviors, and Inequalities: Reflecting on the Impacts of the Influenza and Coronavirus Pandemics in the United States. Int. J. Environ. Res. Public Health 2020, 17, 4484. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7345270/ (accessed on 21 November 2023). [CrossRef] [PubMed]
- Brahim Belhaouari, D.; Baudoin, J.P.; Lagier, J.C.; Monnet-Corti, V.; La Scola, B.; Antezack, A. Microscopic Observations of SARS-CoV-2 Like Particles in Different Oral Samples. Eur. J. Oral Sci. 2022, 130, e12903. Available online: https://onlinelibrary.wiley.com/doi/full/10.1111/eos.12903 (accessed on 21 November 2023). [CrossRef] [PubMed]
- Sapkota, D.; Søland, T.M.; Galtung, H.K.; Sand, L.P.; Giannecchini, S.; To, K.K.W.; Mendes-Correa, M.C.; Giglio, D.; Hasséus, B.; Braz-Silva, P.H. COVID-19 Salivary Signature: Diagnostic and Research Opportunities. J. Clin. Pathol. 2021, 74, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Guimarães, T.C.; Marques, B.B.F.; Tinoco, J.M.M.; Porto, L.C.M.S.; Tinoco, E.M.B.; Fischer, R.G. SARS-CoV-2 Detection in Saliva and Nasopharyngeal Swabs Using RT-PCR Was Similar. Braz. Dent. J. 2022, 33, 68–72. Available online: https://pubmed.ncbi.nlm.nih.gov/35508038/ (accessed on 21 November 2023). [CrossRef] [PubMed]
- Gertler, M.; Krause, E.; van Loon, W.; Krug, N.; Kausch, F.; Rohardt, C.; Rössig, H.; Michel, J.; Nitsche, A.; Mall, M.A.; et al. Self-Collected Oral, Nasal and Saliva Samples Yield Sensitivity Comparable to Professionally Collected Oro-Nasopharyngeal Swabs in SARS-CoV-2 Diagnosis among Symptomatic Outpatients. Int. J. Infect. Dis. 2021, 110, 261–266. Available online: https://pubmed.ncbi.nlm.nih.gov/34302962/ (accessed on 21 November 2023). [CrossRef] [PubMed]
- Lee, R.A.; Herigon, J.C.; Benedetti, A.; Pollock, N.R.; Denkinger, C.M. Performance of Saliva, Oropharyngeal Swabs, and Nasal Swabs for SARS-CoV-2 Molecular Detection: A Systematic Review and Meta-Analysis. J. Clin. Microbiol. 2021, 59, e02881-20. Available online: https://pubmed.ncbi.nlm.nih.gov/33504593/ (accessed on 21 November 2023). [CrossRef] [PubMed]
- Rao, M.; Rashid, F.A.; Sabri, F.S.; Jamil, N.N.; Seradja, V.; Abdullah, N.A.; Ahmad, H.; Aren, S.L.; Ali, S.A.S.; Ghazali, M.; et al. COVID-19 Screening Test by Using Random Oropharyngeal Saliva. J. Med. Virol. 2021, 93, 2461–2466. Available online: https://pubmed.ncbi.nlm.nih.gov/33393672/ (accessed on 21 November 2023). [CrossRef]
- Audigé, A.; Böni, J.; Schreiber, P.W.; Scheier, T.; Buonomano, R.; Rudiger, A.; Braun, D.L.; Eich, G.; Keller, D.I.; Hasse, B.; et al. Reduced Relative Sensitivity of the Elecsys SARS-CoV-2 Antigen Assay in Saliva Compared to Nasopharyngeal Swabs. Microorganisms 2021, 9, 1700. [Google Scholar] [CrossRef]
- Dipalma, G.; Inchingolo, A.D.; Inchingolo, F.; Charitos, I.A.; Di Cosola, M.; Cazzolla, A.P. Focus on the Cariogenic Process: Microbial and Biochemical Interactions with Teeth and Oral Environment. J. Biol. Regul. Homeost. Agents 2021, 35, 429–440. [Google Scholar] [CrossRef]
- Huber, M.; Schreiber, P.W.; Scheier, T.; Audigé, A.; Buonomano, R.; Rudiger, A.; Braun, D.L.; Eich, G.; Keller, D.I.; Hasse, B.; et al. High Efficacy of Saliva in Detecting SARS-CoV-2 by RT-PCR in Adults and Children. Microorganisms 2021, 9, 642. Available online: https://www.mdpi.com/2076-2607/9/3/642 (accessed on 20 November 2023). [CrossRef]
- Basak, S.; Kayet, P.; Ghosh, M.; Chatterjee, J.; Dutta, S. Emergence of Genomic Diversity in the Spike Protein of the “Omicron” Variant. Viruses 2023, 15, 2132. [Google Scholar] [CrossRef] [PubMed]
- Wu, F.; Zhao, S.; Yu, B.; Chen, Y.-M.; Wang, W.; Song, Z.-G.; Hu, Y.; Tao, Z.-W.; Tian, J.-H.; Pei, Y.-Y.; et al. A New Coronavirus Associated with Human Respiratory Disease in China. Nature 2020, 579, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Vogels, C.B.F.; Watkins, A.E.; Harden, C.A.; Brackney, D.E.; Shafer, J.; Wang, J.; Caraballo, C.; Kalinich, C.C.; Ott, I.M.; Fauver, J.R.; et al. SalivaDirect: A Simplified and Flexible Platform to Enhance SARS-CoV-2 Testing Capacity. Med. N. Y. N 2021, 2, 263. [Google Scholar] [CrossRef] [PubMed]
- Melo Costa, M.; Benoit, N.; Dormoi, J.; Amalvict, R.; Gomez, N.; Tissot-Dupont, H.; Million, M.; Pradines, B.; Granjeaud, S.; Almeras, L. Salivette, a Relevant Saliva Sampling Device for SARS-CoV-2 Detection. J. Oral Microbiol. 2021, 13, 1920226. [Google Scholar] [CrossRef] [PubMed]
- Costa, M.M.; Benoit, N.; Dormoi, J.; Amalvict, R.; Gomez, N.; Tissot-Dupont, H.; Million, M.; Pradines, B.; Granjeaud, S.; Almeras, L. Saliva, a Relevant Alternative Sample for SARS-CoV-2 Detection. medRxiv 2020. [Google Scholar] [CrossRef]
- Vâţă, A.; Anita, A.; Manciuc, C.D.; Savuta, G.; Luca, C.M.; Roșu, F.M.; Mihai, I.F.; Anita, D. Clinical Significance of Early IgA Anti-SARS-CoV-2 Antibody Detection in Patients from a Romanian Referral COVID-19 Hospital. Exp. Ther. Med. 2022, 23, 391. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9019744/ (accessed on 21 November 2023). [CrossRef] [PubMed]
- Isho, B.; Abe, K.T.; Zuo, M.; Jamal, A.J.; Rathod, B.; Wang, J.H.; Li, Z.; Chao, G.; Rojas, O.L.; Bang, Y.M.; et al. Persistence of Serum and Saliva Antibody Responses to SARS-CoV-2 Spike Antigens in COVID-19 Patients. Sci. Immunol. 2020, 5, eabe5511. [Google Scholar] [CrossRef] [PubMed]
- Yu, E.D.; Narowski, T.M.; Wang, E.; Garrigan, E.; Mateus, J.; Frazier, A.; Weiskopf, D.; Grifoni, A.; Premkumar, L.; Da Silva Antunes, R.; et al. Immunological Memory to Common Cold Coronaviruses Assessed Longitudinally over a Three-Year Period Pre-COVID19 Pandemic. Cell Host Microbe 2022, 30, 1269–1278.e4. [Google Scholar] [CrossRef]
- Dobaño, C.; Alonso, S.; Fernández de Sevilla, M.; Vidal, M.; Jiménez, A.; Pons Tomas, G.; Jairoce, C.; Melé Casas, M.; Rubio, R.; Hernández García, M.; et al. Antibody Conversion Rates to SARS-CoV-2 in Saliva from Children Attending Summer Schools in Barcelona, Spain. BMC Med. 2021, 19, 309. [Google Scholar] [CrossRef]
- Gentile, F.; Bocci, T.; Coppola, S.; Pozzi, T.; Modafferi, L.; Priori, A.; Chiumello, D. Putative Role of the Lung–Brain Axis in the Pathogenesis of COVID-19-Associated Respiratory Failure: A Systematic Review. Biomedicines 2022, 10, 729. [Google Scholar] [CrossRef]
- Ubhale, R.; Dahake, S.; Madhu, P.P.; Chhabra, K.G.; Reche, A.; Bankar, A.; Kriplani, S.; Adwani, B. Salivary Biomarkers in COVID-19 Patients. J. Fam. Med. Prim. Care 2022, 11, 6778–6782. [Google Scholar] [CrossRef]
- To, K.K.-W.; Tsang, O.T.-Y.; Yip, C.C.-Y.; Chan, K.-H.; Wu, T.-C.; Chan, J.M.-C.; Leung, W.-S.; Chik, T.S.-H.; Choi, C.Y.-C.; Kandamby, D.H.; et al. Consistent Detection of 2019 Novel Coronavirus in Saliva. Clin. Infect. Dis. 2020, 71, 841–843. [Google Scholar] [CrossRef] [PubMed]
- Malcangi, G.; Patano, A.; Guglielmo, M.; Sardano, R.; Palmieri, G.; Di Pede, C.; de Ruvo, E.; Inchingolo, A.D.; Mancini, A.; Inchingolo, F.; et al. Precision Medicine in Oral Health and Diseases: A Systematic Review. J. Pers. Med. 2023, 13, 725. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.D.; Inchingolo, A.M.; Malcangi, G.; Avantario, P.; Azzollini, D.; Buongiorno, S.; Viapiano, F.; Campanelli, M.; Ciocia, A.M.; De Leonardis, N.; et al. Effects of Resveratrol, Curcumin and Quercetin Supplementation on Bone Metabolism—A Systematic Review. Nutrients 2022, 14, 3519. [Google Scholar] [CrossRef] [PubMed]
- Paulose, A.K.; Huang, C.C.; Chen, P.H.; Tripathi, A.; Chen, P.H.; Huang, Y.S.; Wang, Y.L. A Rapid Detection of COVID-19 Viral RNA in Human Saliva Using Electrical Double Layer-Gated Field-Effect Transistor-Based Biosensors. Adv. Mater. Technol. 2022, 7, 2100842. Available online: https://pubmed.ncbi.nlm.nih.gov/34901383/ (accessed on 26 November 2023). [CrossRef] [PubMed]
- Han, P.; Ivanovski, S. Saliva—Friend and Foe in the COVID-19 Outbreak. Diagnostics 2020, 10, 290. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.D.; Malcangi, G.; Semjonova, A.; Inchingolo, A.M.; Patano, A.; Coloccia, G.; Ceci, S.; Marinelli, G.; Di Pede, C.; Ciocia, A.M.; et al. Oralbiotica/Oralbiotics: The Impact of Oral Microbiota on Dental Health and Demineralization: A Systematic Review of the Literature. Children 2022, 9, 1014. [Google Scholar] [CrossRef] [PubMed]
- Azevedo, L.R.; De Lima, A.A.S.; Machado, M.Â.N.; Grégio, A.M.T.; De Almeida, P.D.V. Saliva Composition and Functions: A Comprehensive Review. J. Contemp. Dent. Pract. 2008, 9, 72–80. [Google Scholar] [CrossRef]
- Fini, M.B. Oral Saliva and COVID-19. Oral Oncol. 2020, 108, 104821. Available online: https://pubmed.ncbi.nlm.nih.gov/32474389/ (accessed on 26 November 2023). [CrossRef]
- King, J.; Kosinski-Collins, M.; Sunderberg, E. Coronavirus Structure, Vaccine and Therapy Development. Available online: https://www.biophysics.org/blog/coronavirus-structure-vaccine-and-therapy-development (accessed on 26 November 2023).
- Caixeta, D.C.; Oliveira, S.W.; Cardoso-Sousa, L.; Cunha, T.M.; Goulart, L.R.; Martins, M.M.; Marin, L.M.; Jardim, A.C.G.; Siqueira, W.L.; Sabino-Silva, R. One-Year Update on Salivary Diagnostic of COVID-19. Front. Public Health 2021, 9, 589564. [Google Scholar] [CrossRef]
- Rafeeq, R.A.; Saleem, A.E.; Nahidh, M.; Kadhum, A.S.; Al-Huwaizi, A.F.; Marrapodi, M.M.; Cicciù, M.; Minervini, G. Clinical Management and Infection Control Protocols during the COVID-19 Pandemic: An Online Survey. Technol. Health Care 2023, 31, 1579–1592. Available online: https://pubmed.ncbi.nlm.nih.gov/37092198/ (accessed on 26 November 2023). [CrossRef] [PubMed]
- Sagredo-Olivares, K.; Morales-Gómez, C.; Aitken-Saavedra, J. Evaluation of Saliva as a Complementary Technique to the Diagnosis of COVID-19: A Systematic Review. Med. Oral Patol. Oral Cir. Bucal 2021, 26, e526–e532. [Google Scholar] [CrossRef] [PubMed]
- Nasiri, K.; Dimitrova, A. Comparing Saliva and Nasopharyngeal Swab Specimens in the Detection of COVID-19: A Systematic Review and Meta-Analysis. J. Dent. Sci. 2021, 16, 799–805. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bellocchio, L.; Dipalma, G.; Inchingolo, A.M.; Inchingolo, A.D.; Ferrante, L.; Del Vecchio, G.; Malcangi, G.; Palermo, A.; Qendro, A.; Inchingolo, F. COVID-19 on Oral Health: A New Bilateral Connection for the Pandemic. Biomedicines 2024, 12, 60. https://doi.org/10.3390/biomedicines12010060
Bellocchio L, Dipalma G, Inchingolo AM, Inchingolo AD, Ferrante L, Del Vecchio G, Malcangi G, Palermo A, Qendro A, Inchingolo F. COVID-19 on Oral Health: A New Bilateral Connection for the Pandemic. Biomedicines. 2024; 12(1):60. https://doi.org/10.3390/biomedicines12010060
Chicago/Turabian StyleBellocchio, Luigi, Gianna Dipalma, Angelo Michele Inchingolo, Alessio Danilo Inchingolo, Laura Ferrante, Gaetano Del Vecchio, Giuseppina Malcangi, Andrea Palermo, Andis Qendro, and Francesco Inchingolo. 2024. "COVID-19 on Oral Health: A New Bilateral Connection for the Pandemic" Biomedicines 12, no. 1: 60. https://doi.org/10.3390/biomedicines12010060
APA StyleBellocchio, L., Dipalma, G., Inchingolo, A. M., Inchingolo, A. D., Ferrante, L., Del Vecchio, G., Malcangi, G., Palermo, A., Qendro, A., & Inchingolo, F. (2024). COVID-19 on Oral Health: A New Bilateral Connection for the Pandemic. Biomedicines, 12(1), 60. https://doi.org/10.3390/biomedicines12010060











