The Classification of Suspected Predominant Nociplastic Pain in People with Moderate and Severe Haemophilia: A Secondary Exploratory Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Participants
2.3. The IASP Clinical Criteria and Grading System for Nociplastic Pain Applied to Pain in PwH
- Step 1—A chronic pain duration
- Step 2—A regional/multifocal/widespread pain distribution
- Step 3—The pain cannot entirely be explained by nociceptive mechanisms
- Step 4—The pain cannot entirely be explained by neuropathic mechanisms
- Step 5—Evoked hypersensitivity phenomena
- Step 6–A history of pain hypersensitivity
- Step 7—The presence of comorbidities
2.4. Comparison between Groups
2.5. Statistical Analyses
3. Results
3.1. Participants
3.2. The Classification of Nociplastic Pain
- Step 1—A chronic pain duration
- Step 2—A regional/multifocal/widespread pain distribution
- Step 3—The pain cannot entirely be explained by nociceptive mechanisms
- Step 4—The pain cannot entirely be explained by neuropathic mechanisms
- Step 5—Evoked hypersensitivity phenomena
- Step 6—A history of pain hypersensitivity
- Step 7—The presence of comorbidities
3.3. Comparison between Groups
4. Discussion
4.1. A Clear Definition of Regional/Multifocal/Widespread Pain Is Needed
4.2. Clinical Criteria or a Grading System for Nociceptive Pain Is Needed
4.3. The Evaluation of Evoked Pain Hypersensitivity Needs Clarification
4.4. The Impact of Assessing Comorbidities
4.5. Strengths and Limitations
4.6. Clinical Implications and Implications for Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kempton, C.L.; Recht, M.; Neff, A.; Wang, M.; Buckner, T.W.; Soni, A.; Quon, D.; Witkop, M.; Boggio, L.; Gut, R.Z.; et al. Impact of pain and functional impairment in US adults with haemophilia: Patient-reported outcomes and musculoskeletal evaluation in the pain, functional impairment and quality of life (P-FiQ) study. Haemophilia 2018, 24, 261–270. [Google Scholar] [CrossRef]
- O’Hara, J.; Walsh, S.; Camp, C.; Mazza, G.; Carroll, L.; Hoxer, C.; Wilkinson, L. The impact of severe haemophilia and the presence of target joints on health-related quality-of-life. Health Qual. Life Outcomes 2018, 16, 84. [Google Scholar] [CrossRef]
- Kalnins, W.; Schelle, G.; Jost, K.; Eberl, W.; Tiede, A. Pain therapy in haemophilia in Germany. Patient survey (BESTH study). Hamostaseologie 2015, 35, 167–173. [Google Scholar] [CrossRef]
- Simurda, T.; Drotarova, M.; Skornova, I.; Dobrotova, M.; Brunclikova, M.; Necas, L.; Cibula, Z.; Kubisz, P.; Stasko, J. Perioperative Monitoring with Rotational Thromboelastometry in a Severe Hemophilia A Patient Undergoing Elective Ankle Surgery. In Seminars in Thrombosis and Hemostasis; Thieme Medical Publishers, Inc.: New York, NY, USA, 2023. [Google Scholar]
- Ceponis, A.; Wong-Sefidan, I.; Glass, C.; Von Drygalski, A. Rapid musculoskeletal ultrasound for painful episodes in adult haemophilia patients. Haemophilia 2013, 19, 790–798. [Google Scholar] [CrossRef]
- Roussel, N. Gaining insight into the complexity of pain in patients with haemophilia: State-of-the-art review on pain processing. Haemophilia 2018, 24, 3–8. [Google Scholar] [CrossRef]
- Cortesi, P.A.; Rocino, A.; Preti, D.; Fragomeno, A.; Cucuzza, F.; Ceresi, N.; Santoro, C.; Ferretti, A.; Fornari, A.; Antonazzo, I.C. Haemophilia management and treatment: An Italian survey on patients’, caregivers’ and clinicians’ point of view. Haemophilia 2022, 28, 254–263. [Google Scholar] [CrossRef]
- Kruger, S.; Boettger, M.K.; Hilberg, T. Somatosensory profile of patients with haemophilia. Haemophilia 2018, 24, 97–103. [Google Scholar] [CrossRef]
- Roussel, N.A.; Chantrain, V.A.; Foubert, A.; Lambert, C.; Hermans, C.; Meeus, M.; Guillaume, S.; Lecouvet, F.; Krüger, S.; Hilberg, T. Gaining more insight into ankle pain in haemophilia: A study exploring pain, structural and functional evaluation of the ankle joint. Haemophilia 2022, 28, 480–490. [Google Scholar] [CrossRef]
- Foubert, A.; Chantrain, V.A.; Meeus, M.; Maes, P.; Haenen, V.; Lobet, S.; Lambert, C.; Hermans, C.; Roussel, N. Psychophysical assessment of pain in adults with moderate and severe haemophilia: A cross-sectional study. Haemophilia 2023, 1–16. [Google Scholar] [CrossRef]
- Finnerup, N.B.; Kuner, R.; Jensen, T.S. Neuropathic pain: From mechanisms to treatment. Physiol. Rev. 2020, 101, 259–301. [Google Scholar] [CrossRef]
- Arant, K.; Katz, J.; Neogi, T. Quantitative sensory testing: Identifying pain characteristics in patients with osteoarthritis. Osteoarthr. Cartil. 2022, 30, 17–31. [Google Scholar] [CrossRef] [PubMed]
- Trouvin, A.-P.; Attal, N.; Perrot, S. Assessing central sensitization with quantitative sensory testing in inflammatory rheumatic diseases: A systematic review. Jt. Bone Spine 2022, 89, 105399. [Google Scholar] [CrossRef] [PubMed]
- den Bandt, H.L.; Paulis, W.D.; Beckwée, D.; Ickmans, K.; Nijs, J.; Voogt, L. Pain Mechanisms in Low Back Pain: A Systematic Review with Meta-analysis of Mechanical Quantitative Sensory Testing Outcomes in People with Nonspecific Low Back Pain. J. Orthop. Sports Phys. Ther. 2019, 49, 698–715. [Google Scholar] [CrossRef] [PubMed]
- Spasov, N.; Dimitrova-Popova, D.; Traikova-Djambazova, N.; Spasova, M.; Bosheva, M. Magnetic Resonance Imaging of Hemophilic Joints: Correlations with the Bleeding Phenotype and Physical Examination. Folia Medica 2020, 62, 762–768. [Google Scholar] [CrossRef]
- Chantrain, V.A.; Guillaume, S.; Foubert, A.; Meeus, M.; Lobet, S.; Lambert, C.; Lecouvet, F.; Hermans, C.; Roussel, N.A. Discordance between joint pain and imagery severity in the ankle joint and contributors of lower limb activity limitations in adults with haemophilia: A cross-sectional study. Haemophilia 2023, 29, 648–657. [Google Scholar] [CrossRef]
- Kruger, S.; Weitz, C.; Runkel, B.; Hilberg, T. Pain sensitivity in patients with haemophilia following moderate aerobic exercise intervention. Haemophilia 2016, 22, 886–893. [Google Scholar] [CrossRef]
- Fitzcharles, M.-A.; Cohen, S.P.; Clauw, D.J.; Littlejohn, G.; Usui, C.; Häuser, W. Nociplastic pain: Towards an understanding of prevalent pain conditions. Lancet 2021, 397, 2098–2110. [Google Scholar] [CrossRef]
- Kosek, E.; Clauw, D.; Nijs, J.; Baron, R.; Gilron, I.; Harris, R.E.; Mico, J.-A.; Rice, A.S.; Sterling, M. Chronic nociplastic pain affecting the musculoskeletal system: Clinical criteria and grading system. Pain 2021, 162, 2629–2634. [Google Scholar] [CrossRef]
- Finnerup, N.B.; Haroutounian, S.; Kamerman, P.; Baron, R.; Bennett, D.L.; Bouhassira, D.; Cruccu, G.; Freeman, R.; Hansson, P.; Nurmikko, T. Neuropathic pain: An updated grading system for research and clinical practice. Pain 2016, 157, 1599. [Google Scholar] [CrossRef]
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13, S31. [Google Scholar] [CrossRef]
- Chantrain, V.-A.; Foubert, A.; Meeus, M.; Lambert, C.; Lobet, S.; Maes, P.; Durnez, L.; Hermans, C.; Roussel, N.A. Joint status, pain, and quality of life in elderly people with haemophilia: A case-control study. Submitt. Haemoph. 2023. [Google Scholar]
- Yarnitski, D. Neurophysiological examinations in neuropathic pain. Quant. Sens. Test. Handb. Clin. Neurol. 2006, 27, 397–409. [Google Scholar]
- Bech, K.T.; Larsen, C.M.; Sjøgaard, G.; Holtermann, A.; Taylor, J.L.; Søgaard, K. Voluntary activation of the trapezius muscle in cases with neck/shoulder pain compared to healthy controls. J. Electromyogr. Kinesiol. 2017, 36, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Macfarlane, G.J.; Jones, G.; Knekt, P.; Aromaa, A.; McBeth, J.; Mikkelsson, M.; Heliovaara, M. Is the report of widespread body pain associated with long-term increased mortality? Data from the Mini-Finland Health Survey. Rheumatology 2007, 46, 805–807. [Google Scholar] [CrossRef]
- Bailly, F.; Cantagrel, A.; Bertin, P.; Perrot, S.; Thomas, T.; Lansaman, T.; Grange, L.; Wendling, D.; Dovico, C.; Trouvin, A.-P. Part of pain labelled neuropathic in rheumatic disease might be rather nociplastic. RMD Open 2020, 6, e001326. [Google Scholar] [CrossRef]
- Rolke, R.; Baron, R.; Maier, C.a.; Tölle, T.; Treede, R.-D.; Beyer, A.; Binder, A.; Birbaumer, N.; Birklein, F.; Bötefür, I. Quantitative sensory testing in the German Research Network on Neuropathic Pain (DFNS): Standardized protocol and reference values. Pain 2006, 123, 231–243. [Google Scholar] [CrossRef]
- Schmidt, H.; Drusko, A.; Renz, M.; Schloemp, L.; Tost, H.; Tesarz, J.; Schuh-Hofer, S.; Meyer-Lindenberg, A.; Treede, R.-D. Application of the IASP grading system for ‘nociplastic pain’ in chronic pain conditions: A field study. medRxiv 2022. [Google Scholar]
- Krüger, S.; Hilberg, T. Understanding the pain profile in patients with haemophilia: Impaired descending pain inhibition as measured by conditioned pain modulation. Haemophilia 2020, 26, 236–242. [Google Scholar] [CrossRef]
- Dams, L.; Haenen, V.; Van der Gucht, E.; Devoogdt, N.; Smeets, A.; Bernar, K.; De Vrieze, T.; De Groef, A.; Meeus, M. Absolute and relative reliability of a comprehensive quantitative sensory testing protocol in women treated for breast cancer. Pain Med. 2022, 23, 1162–1175. [Google Scholar] [CrossRef]
- Nijs, J.; Lahousse, A.; Kapreli, E.; Bilika, P.; Saraçoğlu, İ.; Malfliet, A.; Coppieters, I.; De Baets, L.; Leysen, L.; Roose, E. Nociplastic pain criteria or recognition of central sensitization? Pain phenotyping in the past, present and future. J. Clin. Med. 2021, 10, 3203. [Google Scholar] [CrossRef]
- Scerbo, T.; Colasurdo, J.; Dunn, S.; Unger, J.; Nijs, J.; Cook, C. Measurement properties of the central sensitization inventory: A systematic review. Pain Pract. 2018, 18, 544–554. [Google Scholar] [CrossRef] [PubMed]
- Nijs, J.; Lahousse, A.; Fernández-de-Las-Peñas, C.; Madeleine, P.; Fontaine, C.; Nishigami, T.; Desmedt, C.; Vanhoeij, M.; Mostaqim, K.; Cuesta-Vargas, A.I. Towards precision pain medicine for pain after cancer: The Cancer Pain Phenotyping Network multidisciplinary international guidelines for pain phenotyping using nociplastic pain criteria. Br. J. Anaesth. 2023, 130, 611–621. [Google Scholar] [CrossRef] [PubMed]
- Buckner, T.W.; Batt, K.; Quon, D.; Witkop, M.; Recht, M.; Kessler, C.; Baumann, K.; Hernandez, G.; Wang, M.; Cooper, D.L.; et al. Assessments of pain, functional impairment, anxiety, and depression in US adults with hemophilia across patient-reported outcome instruments in the Pain, Functional Impairment, and Quality of Life (P-FiQ) study. Eur. J. Haematol. 2018, 100 (Suppl. S1), 5–13. [Google Scholar] [CrossRef]
- Chantrain, V.-A.; Lambert, C.; De Smet, P.; Lobet, S.; Foubert, A.; Meeus, M.; Hermans, C.; Roussel, N.A. Pain interferes with daily activities, emotions and sleep in adults with severe, moderate and mild haemophilia: A national cross-sectional survey. Haemoph. Off. J. World Fed. Hemoph. 2023, 29, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Pavlova, M.K.; Latreille, V. Sleep disorders. Am. J. Med. 2019, 132, 292–299. [Google Scholar] [CrossRef]
- Wheeler, C.H.; Williams, A.C.D.C.; Morley, S.J. Meta-analysis of the psychometric properties of the Pain Catastrophizing Scale and associations with participant characteristics. Pain 2019, 160, 1946–1953. [Google Scholar] [CrossRef]
- Wu, Y.; Levis, B.; Sun, Y.; He, C.; Krishnan, A.; Neupane, D.; Bhandari, P.M.; Negeri, Z.; Benedetti, A.; Thombs, B.D. Accuracy of the Hospital Anxiety and Depression Scale Depression subscale (HADS-D) to screen for major depression: Systematic review and individual participant data meta-analysis. BMJ 2021, 373, n972. [Google Scholar] [CrossRef]
- Buckner, T.W.; Sidonio Jr, R.; Guelcher, C.; Kessler, C.M.; Witkop, M.; Clark, D.; Owens, W.; Fridman, M.; Iyer, N.N.; Cooper, D.L. Reliability and validity of patient-reported outcome instruments in US adults with hemophilia B and caregivers in the B-HERO-S study. Eur. J. Haematol. 2018, 101, 781–790. [Google Scholar] [CrossRef]
- Freynhagen, R.; Parada, H.A.; Calderon-Ospina, C.A.; Chen, J.; Rakhmawati Emril, D.; Fernández-Villacorta, F.J.; Franco, H.; Ho, K.-Y.; Lara-Solares, A.; Li, C.C.-F. Current understanding of the mixed pain concept: A brief narrative review. Curr. Med. Res. Opin. 2019, 35, 1011–1018. [Google Scholar] [CrossRef]
- Rolke, R.; Magerl, W.; Campbell, K.A.; Schalber, C.; Caspari, S.; Birklein, F.; Treede, R.-D. Quantitative sensory testing: A comprehensive protocol for clinical trials. Eur. J. Pain 2006, 10, 77–88. [Google Scholar] [CrossRef]
- Treede, R.-D.; Hoheisel, U.; Wang, D.; Magerl, W. Central sensitization: Clinical utility of a physiological concept for the International Statistical Classification of Diseases and Related Health Problems and for nociplastic pain. Pain 2022, 163, S99–S107. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.-T.; Liu, Z.; Liu, Y.-L.; Zhao, J.-J.; Liu, D.-W.; Tian, Q.-B. Obesity as a risk factor for low Back pain. Clin. Spine Surg. 2018, 31, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Nijs, J.; Mairesse, O.; Neu, D.; Leysen, L.; Danneels, L.; Cagnie, B.; Meeus, M.; Moens, M.; Ickmans, K.; Goubert, D. Sleep disturbances in chronic pain: Neurobiology, assessment, and treatment in physical therapist practice. Phys. Ther. 2018, 98, 325–335. [Google Scholar] [CrossRef] [PubMed]
- Helminen, E.-E.; Arokoski, J.P.; Selander, T.A.; Sinikallio, S.H. Multiple psychological factors predict pain and disability among community-dwelling knee osteoarthritis patients: A five-year prospective study. Clin. Rehabil. 2020, 34, 404–415. [Google Scholar] [CrossRef]
- Santoro, C.; Di Minno, M.N.D.; Corcione, A.; Di Minno, G.; Martinelli, M.; Mancuso, M.E.; Acone, B.; Molinari, A.C.; Passeri, E.V.; Rocino, A. Improving assessment and management of pain in hemophilia: An Italian Delphi consensus statement. Blood Rev. 2021, 51, 100885. [Google Scholar] [CrossRef] [PubMed]
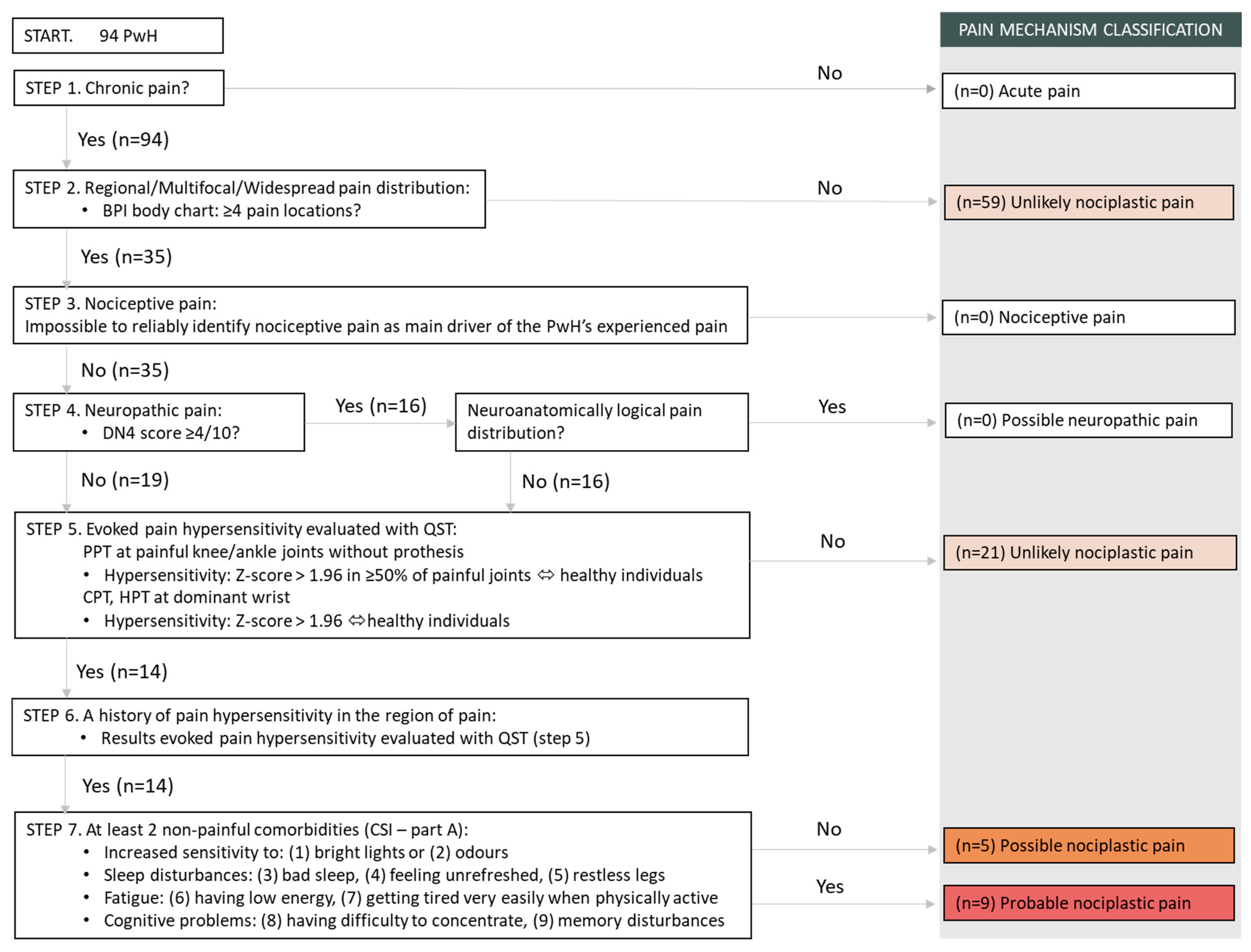
| STEP 1. | The pain is chronic: PwH with chronic pain will fulfil this step. |
| STEP 2. | The pain has a regional/multifocal/widespread distribution: ≥4 painful body sites on the BPI-Body chart. |
| STEP 3. | The pain cannot entirely be explained by nociceptive mechanisms: All PwH will fulfil this step, since it is impossible to reliably identify nociceptive pain as the main driver of the PwH’s experienced pain. |
| STEP 4. | The pain cannot entirely be explained by neuropathic mechanisms: PwH without possible neuropathic pain will fulfil this step. (Possible neuropathic pain: a DN4 score of ≥4/10 and a neuroanatomically plausible pain distribution). |
| STEP 5. | Evoked hypersensitivity phenomena: PwH presenting evoked hypersensitivity evaluated with QST will fulfil this step: - Pressure Pain Threshold at painful knee/ankle joints without prothesis: Hypersensitivity: Z-score > 1.96 in ≥50 of painful joints ⇔ healthy individuals - Cold & Heat Pain Threshold at dominant wrist: Hypersensitivity: Z-score > 1.96 ⇔ healthy individuals |
| Possible nociplastic pain: PwH who fulfil all 5 steps. Unlikely nociplastic pain: PwH who fulfil none or some of the steps. | |
| STEP 6. | A history of pain hypersensitivity: When QST results are present they can be used to determine whether PwH have a history of pain hypersensitivity. PwH who present pain hypersensitivity in step 5 will automatically fulfil step 6. |
| STEP 7. | The presence of comorbidities: PwH will fulfil step 7 if they achieve at least a score of 3 (often present) for ≥2 comorbidities on the CSI part A: - Increased sensitivity to: (1) bright lights or (2) odours - Sleep disturbances: (3) bad sleep, (4) feeling unrefreshed, (5) restless legs - Fatigue: (6) having low energy, (7) getting tired very easily when physically active - Cognitive problems: (8) having difficulty to concentrate, (9) memory disturbances |
| Probable nociplastic pain: PwH who fulfil all 7 steps. | |
| PwH (n = 94) | Healthy Individuals (n = 41) | p-Value a | |||
|---|---|---|---|---|---|
| Mean ± SD (Range) | n (%) | Mean ± SD (Range) | n (%) | ||
| Age (years) | 41.7 ± 16.9 (18–81) | - | 38.8 ± 17.2 (18–79) | - | 0.372 |
| Weight (kg) | 80.8 ± 16.1 (48.7–128) | - | 77.5 ± 10.9 (60–104) | - | 0.177 |
| Height (m) | 1.77 ± 0.06 (1.60–1.88) | - | 1.80 ± 0.07 (1.64–1.93) | - | 0.005 |
| BMI (kg/m2) | 26.0 ± 4.9 (16.9–40.9) | - | 24.1 ± 3.3 (18.6–31.1) | - | 0.008 |
| Type of haemophilia—severity | - | ||||
| A—severe | - | 62 (66.0%) | - | - | |
| A—moderate | 12 (12.8%) | ||||
| B—severe | 11 (11.7%) | ||||
| B—moderate | - | 9 (9.6%) | - | - | |
| Treatment regimen | - | ||||
| On-demand | - | 11 (11.7%) | - | - | |
| Prophylaxis | - | 83 (88.3%) | - | - | |
| Self-reported use of pain medication | 24 (25.5%) | 0 (0%) | <0.001 b | ||
| Non-opioid analgesics | - | 14 (14.9%) | - | - | |
| Non-opioid + weak opioid analgesics | - | 1 (1.1%) | - | - | |
| Non-opioid analgesics + recombinant factor | - | 9 (9.6%) | - | - | |
| Positive HIV | - | 6 (6.4%) | - | - | - |
| Hepatitis C | - | ||||
| Negative | - | 44 (46.8%) | - | - | |
| Succesfully treated for HCV (negative viral load) | - | 50 (53.2%) | - | - | |
| QST | Healthy Individuals (n = 41) | PwH (n = 35) | ||||
|---|---|---|---|---|---|---|
| n | Mean ± SD | n | Mean ± SD | n(%) Z-Score > 1.96 | n(%) Z-Score PPT > 1.96 in ≥50% of Painful Joints or Z-Score CPT/HPT > 1.96 | |
| CPT wrist (°C) | 41 | 6.67 ± 7.98 | 33 a | 10.19 ± 9.77 | 7 (20%) | 14 (40%) |
| HPT wrist (°C) | 41 | 46.36 ± 2.60 | 33 a | 45.90 ± 3.22 | 3 (9%) | |
| PPT knee left (N) | 41 | 67.04 ± 20.18 | 14 b | 36.72 ± 16.72 | 6 (17%) | |
| PPT knee right (N) | 41 | 68.64 ± 22.37 | 10 b | 43.73 ± 16.25 | 1 (3%) | |
| PPT ankle left (N) | 41 | 68.94 ± 19.84 | 22 b | 41.25 ± 17.14 | 7 (20%) | |
| PPT ankle right (N) | 41 | 68.87 ± 22.59 | 24 b | 43.42 ± 19.77 | 3 (9%) | |
| PwH with “Unlikely” Nociplastic Pain (n = 80) | PwH with “Possible” Nociplastic Pain (n = 14) | Healthy Individuals (n = 41) | ANOVA p-Value | p-Value * Pairwise Comparison Subgroups (ANOVA) | ANCOVA p-Value | p-Value * Pairwise Comparison Subgroups (ANCOVA) | |
|---|---|---|---|---|---|---|---|
| Mean ± SD (Range) or n (%) | Mean ± SD (Range) or n (%) | Mean ± SD (Range) or n (%) | |||||
| Age (years) | 40.3 ± 15.9 (18–74) | 49.5 ± 21 (19–81) | 38.8 ± 17.2 (18–79) | 0.117 | - | - | - |
| Weight (kg) | 80.6 ± 15.1 (48.7–128) | 82 ± 21.6 (50–117) | 77.5 ± 10.9 (60–104) | 0.480 | - | 0.526 | - |
| Height (m) | 1.77 ± 0.06 (1.62–1.88) | 1.73 ± 0.08 (1.60–1.87) | 1.80 ± 0.07 (1.64–1.93) | 0.004 | 0.005 (Possible vs. Healthy) | 0.013 | - |
| BMI (kg/m2) | 25.8 ± 4.6 (16.9–40.9) | 27.3 ± 6.7 (18.6–37.9) | 24.1 ± 3.3 (18.6–31.1) | 0.038 | - | 0.069 | - |
| Type of haemophilia—severity | 0.102 a | - | - | - | |||
| A—severe | 53 (66%) | 9 (64%) | - | ||||
| A—moderate | 12 (15%) | - | - | ||||
| B—severe | 7 (9%) | 4 (29%) | - | ||||
| B—moderate | 8 (10%) | 1 (7%) | - | ||||
| Treatment regimen | 0.412 a | - | - | - | |||
| On-demand | 11 (14%) | - | - | ||||
| Prophylaxis | 56 (70%) | 11 (79%) | - | ||||
| Emicizumab | 13 (16%) | 3 (21%) | - | ||||
| Gene therapy | - | - | |||||
| Self-reported use of pain medication | 20 (25%) | 4 (28%) | 0 (0%) | <0.001 a | - | - | - |
| Non-opioid analgesics | 12 (15%) | 2 (14%) | - | ||||
| Non-opioid + weak opioid analgesics | 1 (1%) | - | - | ||||
| Non-opioid + strong opioid analgesics | - | - | - | ||||
| Non-opioid analgesics + recombinant factor | 7 (9%) | 2 (14%) | - | ||||
| HADS | |||||||
| Anxiety (max. 21) | 6.0 ± 3.8 (0–18) | 6.3 ± 3.0 (1–10) | 3.6 ± 2.7 (0–12) | <0.001 | <0.001 (Unlikely vs. Healthy) | <0.001 | <0.001 (Unlikely vs. Healthy) |
| 0.016 (Possible vs. Healthy) | |||||||
| Depression (max. 21) | 4.3 ± 3.5 (0–15) | 5.7 ± 2.6 (0–9) | 2.2 ± 1.9 (0–7) | <0.001 | <0.001 (Unlikely vs. Healthy) | <0.001 | <0.001 (Unlikely vs. Healthy) |
| <0.001 (Possible vs. Healthy) | <0.001 (Possible vs. Healthy) | ||||||
| PCS | |||||||
| Total (max. 52) | 14.2 ± 11.1 (0–47) | 20.3 ± 12.6 (0–37) | 7.2 ± 7.1 (0–23) | <0.001 | 0.002 (Unlikely vs. Healthy) | <0.001 | 0.002 (Unlikely vs. Healthy) |
| <0.001 (Possible vs. Healthy) | <0.001 (Possible vs. Healthy) | ||||||
| PCS Rumination (max. 16) | 4.9 ± 4.4 (0–16) | 7.2 ± 4.5 (0–13) | 3.4 ± 3.7 (0–14) | 0.012 | 0.012 (Possible vs. Healthy) | 0.013 | 0.013 (Possible vs. Healthy) |
| PCS Magnification (max. 12) | 3.0 ± 2.4 (0–10) | 4.6 ± 3.3 (0–9) | 1.3 ± 1.6 (0–6) | <0.001 | <0.001 (Unlikely vs. Healthy) | <0.001 | <0.001 (Unlikely vs. Healthy) |
| <0.001 (Possible vs. Healthy) | <0.001 (Possible vs. Healthy) | ||||||
| PCS Helplessness (max. 24) | 6.3 ± 5.4 (0–23) | 8.4 ± 6.4 (0–21) | 2.5 ± 2.6 (0–10) | <0.001 | <0.001 (Unlikely vs. Healthy) | <0.001 | <0.001 (Unlikely vs. Healthy) |
| <0.001 (Possible vs. Healthy) | <0.001 (Possible vs. Healthy) | ||||||
| FABQ | |||||||
| Physical activity (max. 24) | 13.8 ± 6.2 (0–24) | 16.1 ± 6.4 (7–24) | 9.2 ± 7.5 (0–24) | <0.001 | 0.001 (Unlikely vs. Healthy) | <0.001 | 0.001 (Unlikely vs. Healthy) |
| 0.003 (Possible vs. Healthy) | 0.006 (Possible vs. Healthy) | ||||||
| EQ-5D-5L | |||||||
| EQ-HUI (max. 1) | 0.7 ± 0.2 (0–1) | 0.6 ± 0.2 (0.2–0.9) | 1.0 ± 0.1 (0.7–1) | <0.001 | <0.001 (Unlikely vs. Healthy) | <0.001 | <0.001 (Unlikely vs. Healthy) |
| <0.001 (Possible vs. Healthy) | <0.001 (Possible vs. Healthy) | ||||||
| EQ-VAS (max. 100) | 70.4 ± 15.3 (27–80) | 69.0 ± 19.8 (30–100) | 84.9 ± 8.5 (67–100) | <0.001 | <0.001 (Unlikely vs. Healthy) | <0.001 | <0.001 (Unlikely vs. Healthy) |
| 0.001 (Possible vs. Healthy) | <0.001 (Possible vs. Healthy) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Foubert, A.; Roussel, N.A.; Chantrain, V.-A.; Maes, P.; Durnez, L.; Lobet, S.; Lambert, C.; Hermans, C.; Meeus, M. The Classification of Suspected Predominant Nociplastic Pain in People with Moderate and Severe Haemophilia: A Secondary Exploratory Study. Biomedicines 2023, 11, 2479. https://doi.org/10.3390/biomedicines11092479
Foubert A, Roussel NA, Chantrain V-A, Maes P, Durnez L, Lobet S, Lambert C, Hermans C, Meeus M. The Classification of Suspected Predominant Nociplastic Pain in People with Moderate and Severe Haemophilia: A Secondary Exploratory Study. Biomedicines. 2023; 11(9):2479. https://doi.org/10.3390/biomedicines11092479
Chicago/Turabian StyleFoubert, Anthe, Nathalie Anne Roussel, Valérie-Anne Chantrain, Philip Maes, Lies Durnez, Sébastien Lobet, Catherine Lambert, Cédric Hermans, and Mira Meeus. 2023. "The Classification of Suspected Predominant Nociplastic Pain in People with Moderate and Severe Haemophilia: A Secondary Exploratory Study" Biomedicines 11, no. 9: 2479. https://doi.org/10.3390/biomedicines11092479
APA StyleFoubert, A., Roussel, N. A., Chantrain, V.-A., Maes, P., Durnez, L., Lobet, S., Lambert, C., Hermans, C., & Meeus, M. (2023). The Classification of Suspected Predominant Nociplastic Pain in People with Moderate and Severe Haemophilia: A Secondary Exploratory Study. Biomedicines, 11(9), 2479. https://doi.org/10.3390/biomedicines11092479





