A Cross-Sectional Study Investigating Lumbar Proprioception Impairments in Individuals with Type 2 Diabetes Mellitus: Correlations with Glycated Hemoglobin Levels
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Participants
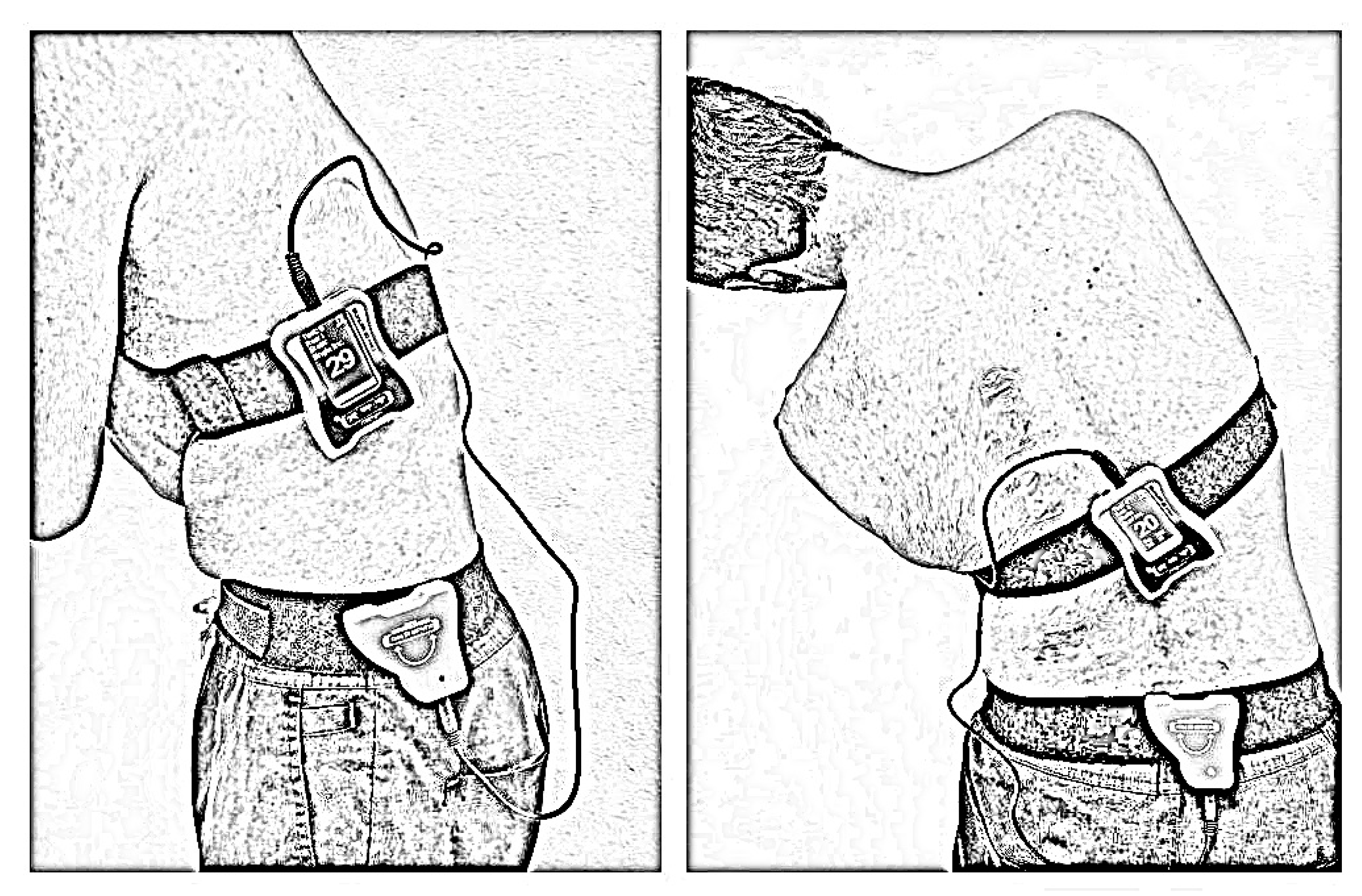
2.3. Lumbar Proprioception Assessment
2.4. Glycated Hemoglobin (HbA1c) Measurement
2.5. Sample Size Calculation
2.6. Data Analysis
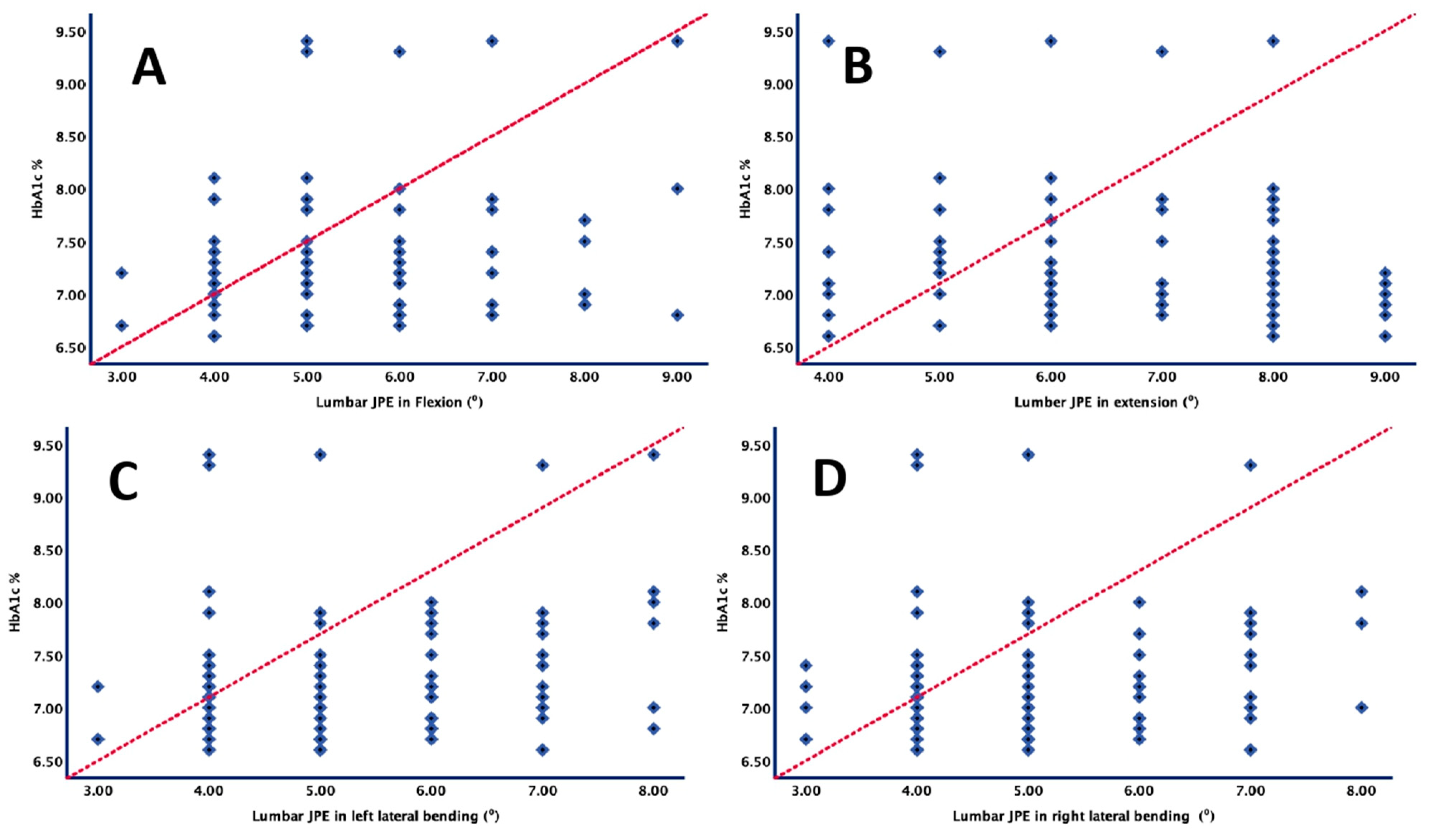
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wang, Y.; Gao, H.; Di, W.; Gu, Z. Endocrinological and metabolic characteristics in patients who are non-obese and have polycystic ovary syndrome and different types of a family history of type 2 diabetes mellitus. J. Int. Med. Res. 2021, 49, 03000605211016672. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.A.B.; Hashim, M.J.; King, J.K.; Govender, R.D.; Mustafa, H.; Al Kaabi, J. Epidemiology of type 2 diabetes–global burden of disease and forecasted trends. J. Epidemiol. Glob. Health 2020, 10, 107. [Google Scholar] [CrossRef] [PubMed]
- Saeedi, P.; Petersohn, I.; Salpea, P.; Malanda, B.; Karuranga, S.; Unwin, N.; Colagiuri, S.; Guariguata, L.; Motala, A.A.; Ogurtsova, K. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas. Diabetes Res. Clin. Pract. 2019, 157, 107843. [Google Scholar] [CrossRef]
- Moradi, Y.; Baradaran, H.R.; Djalalinia, S.; Chinekesh, A.; Khamseh, M.E.; Dastoorpoor, M.; Sioofy-Khojine, A.-B.; Saed, L.; Qorbani, M. Complications of type 2 diabetes in Iranian population: An updated systematic review and meta-analysis. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 2300–2312. [Google Scholar] [CrossRef]
- Abdelhamid, A.; Hooper, L.; Sivakaran, R.; Hayhoe, R.P.; Welch, A. The relationship between omega-3, omega-6 and total polyunsaturated fat and musculoskeletal health and functional status in adults: A systematic review and meta-analysis of RCTs. Calcif. Tissue Int. 2019, 105, 353–372. [Google Scholar] [CrossRef] [PubMed]
- Reddy, R.S.; Alshahrani, M.S.; Tedla, J.S.; Asiri, F.; Nambi, G.; Kakaraparthi, V.N. Cervical Joint Position Sense in Individuals With Type 2 Diabetes and Its Correlations With Glycated Hemoglobin Levels: A Cross-Sectional Study. J. Manip. Physiol. Ther. 2022, 45, 273–281. [Google Scholar] [CrossRef]
- Asiri, F.; Reddy, R.S.; Narapureddy, B.R.; Raizah, A. Comparisons and Associations between Hip-Joint Position Sense and Glycosylated Hemoglobin in Elderly Subjects with Type 2 Diabetes Mellitus—A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 15514. [Google Scholar] [CrossRef]
- Raizah, A.; Reddy, R.S.; Alshahrani, M.S.; Gautam, A.P.; Alkhamis, B.A.; Kakaraparthi, V.N.; Ahmad, I.; Kandakurti, P.K.; ALMohiza, M.A. A Cross-Sectional Study on Mediating Effect of Chronic Pain on the Relationship between Cervical Proprioception and Functional Balance in Elderly Individuals with Chronic Neck Pain: Mediation Analysis Study. J. Clin. Med. 2023, 12, 3140. [Google Scholar] [CrossRef]
- Alahmari, K.; Reddy, R.S.; Silvian, P.; Ahmad, I.; Nagaraj, V.; Mahtab, M. Intra-and inter-rater reliability of neutral head position and target head position tests in patients with and without neck pain. Braz. J. Phys. Ther. 2017, 21, 259–267. [Google Scholar] [CrossRef]
- Alahmari, K.A.; Kakaraparthi, V.N.; Reddy, R.S.; Silvian, P.; Tedla, J.S.; Rengaramanujam, K.; Ahmad, I. Combined effects of strengthening and proprioceptive training on stability, balance, and proprioception among subjects with chronic ankle instability in different age groups: Evaluation of clinical outcome measures. Indian J. Orthop. 2021, 55, 199–208. [Google Scholar] [CrossRef]
- Alahmari, K.A.; Reddy, R.S.; Silvian, P.; Ahmad, I.; Kakarparthi, V.N.; Rengaramanujam, K. Intra and inter-rater reliability for deep neck flexor and neck extensor muscle endurance tests in subjects with and without subclinical neck pain. Phys. Med. Rehabil. Kurortmed. 2019, 58, 310–316. [Google Scholar] [CrossRef]
- Alahmari, K.A.; Reddy, R.S.; Silvian, P.; Ahmad, I.; Nagaraj, V.; Mahtab, M. Influence of chronic neck pain on cervical joint position error (JPE): Comparison between young and elderly subjects. J. Back Musculoskelet. Rehabil. 2017, 30, 1265–1271. [Google Scholar] [CrossRef]
- Alahmari, K.A.; Reddy, R.S.; Silvian, P.S.; Ahmad, I.; Kakaraparthi, V.N.; Alam, M.M. Association of age on cervical joint position error. J. Adv. Res. 2017, 8, 201–207. [Google Scholar] [CrossRef]
- ALMohiza, M.A.; Reddy, R.S.; Asiri, F.; Alshahrani, A.; Tedla, J.S.; Dixit, S.; Gular, K.; Kakaraparthi, V.N. The Mediation Effect of Pain on the Relationship between Kinesiophobia and Lumbar Joint Position Sense in Chronic Low Back Pain Individuals: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2023, 20, 5193. [Google Scholar] [CrossRef]
- Alshahrani, M.S.; Reddy, R.S. Relationship between Kinesiophobia and Ankle Joint Position Sense and Postural Control in Individuals with Chronic Ankle Instability—A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 2792. [Google Scholar] [CrossRef]
- Alshahrani, M.S.; Reddy, R.S.; Tedla, J.S.; Asiri, F.; Alshahrani, A. Association between kinesiophobia and knee pain intensity, joint position sense, and functional performance in individuals with bilateral knee osteoarthritis. Healthcare 2022, 10, 120. [Google Scholar] [CrossRef]
- Asiri, F.; Reddy, R.S.; Alshahrani, M.S.; Tedla, J.S.; Dixit, S.; Alshahrani, A.; Gular, K.; Raizah, A. Mediation Effect of Pain on the Relationship between Kinesiophobia and Postural Control: Comparison and Correlations in Individuals with Fibromyalgia Syndrome and Asymptomatic Individuals—A Cross-Sectional Study. Life 2023, 13, 175. [Google Scholar] [CrossRef]
- Asiri, F.; Reddy, R.S.; Tedla, J.S.; ALMohiza, M.A.; Alshahrani, M.S.; Govindappa, S.C.; Sangadala, D.R. Kinesiophobia and its correlations with pain, proprioception, and functional performance among individuals with chronic neck pain. PLoS ONE 2021, 16, e0254262. [Google Scholar] [CrossRef]
- Kandakurti, P.K.; Reddy, R.S.; Kakarparthy, V.N.; Rengaramanujam, K.; Tedla, J.S.; Dixit, S.; Gautam, A.P.; Silvian, P.; Gular, K.; Eapen, C. Comparison and Association of Neck Extensor Muscles’ Endurance and Postural Function in Subjects with and without Chronic Neck Pain–A Cross-Sectional Study. Phys. Med. Rehabil. Kurortmed. 2021, 31, 295–301. [Google Scholar] [CrossRef]
- Raizah, A.; Reddy, R.S.; Alshahrani, M.S.; Tedla, J.S.; Dixit, S.; Gular, K.; Gautam, A.P.; Ahmad, I.; Kandakurti, P.K. Investigating Knee Joint Proprioception and Its Impact on Limits of Stability Using Dynamic Posturography in Individuals with Bilateral Knee Osteoarthritis—A Cross-Sectional Study of Comparisons and Correlations. J. Clin. Med. 2023, 12, 2764. [Google Scholar] [CrossRef]
- Reddy, R.S.; Tedla, J.S.; Alshahrani, M.S.; Asiri, F.; Kakaraparthi, V.N.; Samuel, P.S.; Kandakurti, P.K. Reliability of hip joint position sense tests using a clinically applicable measurement tool in elderly participants with unilateral hip osteoarthritis. Sci. Rep. 2022, 12, 376. [Google Scholar] [CrossRef]
- Reddy, R.S.; Tedla, J.S.; Dixit, S.; Raizah, A.; Al-Otaibi, M.L.; Gular, K.; Ahmad, I.; Sirajudeen, M.S. Cervical Joint Position Sense and Its Correlations with Postural Stability in Subjects with Fibromyalgia Syndrome. Life 2022, 12, 1817. [Google Scholar] [CrossRef]
- Saeed Alshahrani, M.; Reddy, R.S.; Asiri, F.; Tedla, J.S.; Alshahrani, A.; Kandakurti, P.K.; Kakaraparthi, V.N. Correlation and comparison of quadriceps endurance and knee joint position sense in individuals with and without unilateral knee osteoarthritis. BMC Musculoskelet. Disord. 2022, 23, 23. [Google Scholar] [CrossRef]
- Ferlinc, A.; Fabiani, E.; Velnar, T.; Gradisnik, L. The importance and role of proprioception in the elderly: A short review. Mater. Socio-Medica 2019, 31, 219. [Google Scholar] [CrossRef]
- Henry, M.; Baudry, S. Age-related changes in leg proprioception: Implications for postural control. J. Neurophysiol. 2019, 122, 525–538. [Google Scholar] [CrossRef]
- Maras, O.; Dulgeroglu, D.; Cakci, A. Ankle Proprioception in Patients with Type 2 Diabetes Mellitus. J. Am. Podiatr. Med. Assoc. 2021, 111, 8. [Google Scholar] [CrossRef]
- Luo, S.; Soh, K.G.; Nasiruddin, N.J.; Sun, H.; Du, C.; Soh, K.L. Effect of core training on skill performance among athletes: A systematic review. Front. Physiol. 2022, 13, 915259. [Google Scholar] [CrossRef]
- Cheng, X.; Yang, J.; Hao, Z.; Li, Y.; Fu, R.; Zu, Y.; Ma, J.; Lo, W.L.A.; Yu, Q.; Zhang, G. The effects of proprioceptive weighting changes on posture control in patients with chronic low back pain: A cross-sectional study. Front. Neurol. 2023, 14, 1144900. [Google Scholar] [CrossRef]
- Ghamkhar, L.; Kahlaee, A.H. The effect of trunk muscle fatigue on postural control of upright stance: A systematic review. Gait Posture 2019, 72, 167–174. [Google Scholar] [CrossRef]
- Kanaley, J.A.; Colberg, S.R.; Corcoran, M.H.; Malin, S.K.; Rodriguez, N.R.; Crespo, C.J.; Kirwan, J.P.; Zierath, J.R. Exercise/physical activity in individuals with type 2 diabetes: A consensus statement from the American College of Sports Medicine. Med. Sci. Sports Exerc. 2022, 54, 353–368. [Google Scholar] [CrossRef]
- Ahmad, I.; Noohu, M.M.; Verma, S.; Singla, D.; Hussain, M.E. Effect of sensorimotor training on balance measures and proprioception among middle and older age adults with diabetic peripheral neuropathy. Gait Posture 2019, 74, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Salzman, B. Gait and balance disorders in older adults. Am. Fam. Physician 2010, 82, 61–68. [Google Scholar] [PubMed]
- Hassoon, A.; Bydon, M.; Kerezoudis, P.; Maloney, P.R.; Rinaldo, L.; Yeh, H.-C. Chronic low-back pain in adult with diabetes: NHANES 2009–2010. J. Diabetes Its Complicat. 2017, 31, 38–42. [Google Scholar] [CrossRef]
- Pozzobon, D.; Ferreira, P.H.; Dario, A.B.; Almeida, L.; Vesentini, G.; Harmer, A.R.; Ferreira, M.L. Is there an association between diabetes and neck and back pain? A systematic review with meta-analyses. PLoS ONE 2019, 14, e0212030. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Hng, T.-M. HbA1c: More than just a number. Aust. J. Gen. Pract. 2021, 50, 628–632. [Google Scholar] [CrossRef]
- Lu, Y.; Xing, P.; Cai, X.; Luo, D.; Li, R.; Lloyd, C.; Sartorius, N.; Li, M. Prevalence and risk factors for diabetic peripheral neuropathy in type 2 diabetic patients from 14 countries: Estimates of the INTERPRET-DD study. Front. Public Health 2020, 8, 534372. [Google Scholar] [CrossRef]
- Bhatt, U.; Mehta, M.; Kumar, G.P. Postural Control in Diabetic Peripheral Neuropathy: A Narrative Review. J. Clin. Diagn. Res. 2022, 16, 6–14. [Google Scholar] [CrossRef]
- Chamberlain, J.J.; Rhinehart, A.S.; Shaefer Jr, C.F.; Neuman, A. Diagnosis and management of diabetes: Synopsis of the 2016 American Diabetes Association Standards of Medical Care in Diabetes. Ann. Intern. Med. 2016, 164, 542–552. [Google Scholar] [CrossRef]
- Reddy, R.S.; Alahmari, K.A.; Samuel, P.S.; Tedla, J.S.; Kakaraparthi, V.N.; Rengaramanujam, K. Intra-rater and inter-rater reliability of neutral and target lumbar positioning tests in subjects with and without non-specific lower back pain. J. Back Musculoskelet. Rehabil. 2021, 34, 289–299. [Google Scholar] [CrossRef]
- Moslemi Haghighi, F.; Ghafarinejad, F.; Hemmati, L.; Saadat, Z.; Oorangi, Z.; Torabi, S.; Mohammadzadeh, M.A. Evaluation of ankle joint proprioception and balance in patients with type 2 diabetes and healthy subjects. J. Rehabil. Sci. Res. 2015, 2, 17–19. [Google Scholar]
- Obilor, E.I.; Amadi, E.C. Test for significance of Pearson’s correlation coefficient. Int. J. Innov. Math. Stat. Energy Policies 2018, 6, 11–23. [Google Scholar]
- Hlaing, S.S.; Puntumetakul, R.; Wanpen, S.; Boucaut, R. Balance control in patients with subacute non-specific low back pain, with and without lumbar instability: A cross-sectional study. J. Pain Res. 2020, 13, 795–803. [Google Scholar] [CrossRef]
- Qu, X.; Hu, X.; Zhao, J.; Zhao, Z. The roles of lower-limb joint proprioception in postural control during gait. Appl. Ergon. 2022, 99, 103635. [Google Scholar] [CrossRef]
- Ettinger, L.R.; Boucher, A.; Simonovich, E. Patients with type 2 diabetes demonstrate proprioceptive deficit in the knee. World J. Diabetes 2018, 9, 59. [Google Scholar] [CrossRef] [PubMed]
- Guney, H.; Kaya, D.; Citaker, S.; Kafa, N.; Yosmaoglu, B.; Yetkin, I.; Yuksel, I.; Doral, M.N. Is there any loss of ankle proprioception in diabetic patients without neuropathy? Isokinet. Exerc. Sci. 2013, 21, 317–323. [Google Scholar] [CrossRef]
- Li, L.; Zhang, S.; Dobson, J. The contribution of small and large sensory afferents to postural control in patients with peripheral neuropathy. J. Sport Health Sci. 2019, 8, 218–227. [Google Scholar] [CrossRef]
- Ferris, J.K.; Inglis, J.T.; Madden, K.M.; Boyd, L.A. Brain and body: A review of central nervous system contributions to movement impairments in diabetes. Diabetes 2020, 69, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Zilliox, L.A. Diabetes and peripheral nerve disease. Clin. Geriatr. Med. 2021, 37, 253–267. [Google Scholar] [CrossRef] [PubMed]
- Sung, P.S.; Park, M.S. Delayed response in rectus abdominis muscle following a step perturbation in subjects with and without recurrent low back pain. Eur. Spine J. 2023, 32, 1842–1849. [Google Scholar] [CrossRef] [PubMed]
- Gorji, S.M.; Mohammadi Nia Samakosh, H.; Watt, P.; Henrique Marchetti, P.; Oliveira, R. Pain neuroscience education and motor control exercises versus core stability exercises on pain, disability, and balance in women with chronic low back pain. Int. J. Environ. Res. Public Health 2022, 19, 2694. [Google Scholar] [CrossRef]
- Hlaing, S.S.; Puntumetakul, R.; Khine, E.E.; Boucaut, R. Effects of core stabilization exercise and strengthening exercise on proprioception, balance, muscle thickness and pain related outcomes in patients with subacute nonspecific low back pain: A randomized controlled trial. BMC Musculoskelet. Disord. 2021, 22, 998. [Google Scholar] [CrossRef]
- Sakai, Y.; Watanabe, T.; Wakao, N.; Matsui, H.; Osada, N.; Sugiura, T.; Morita, Y.; Kawai, K.; Ito, T.; Yamazaki, K. Proprioception and Geriatric Low Back Pain. Spine Surg. Relat. Res. 2022, 6, 422–432. [Google Scholar] [CrossRef]
- Giri, H.S.; Borkar, P. Effects of sensory stimulation on balance and postural control in diabetic neuropathy: Systematic review. Int. J. Res. Med. Sci. 2021, 9, 2090. [Google Scholar] [CrossRef]
- Winter, L.; Huang, Q.; Sertic, J.V.; Konczak, J. The Effectiveness of Proprioceptive Training for Improving Motor Performance and Motor Dysfunction: A Systematic Review. Front. Rehabil. Sci. 2022, 3, 830166. [Google Scholar] [CrossRef]
- Liu, Y.; Yang, Y.; Liu, H.; Wu, W.; Wu, X.; Wang, T. A systematic review and meta-analysis of fall incidence and risk factors in elderly patients after total joint arthroplasty. Medicine 2020, 99, e23664. [Google Scholar] [CrossRef] [PubMed]
- Roman de Mettelinge, T.; Desimpelaere, P.; Cambier, D. Cervical mobility and cervical proprioception in relation to fall risk among older adults: A prospective cohort study. Eur. Geriatr. Med. 2023, 14, 447–453. [Google Scholar] [CrossRef] [PubMed]
- Derby, H.; Chander, H.; Kodithuwakku Arachchige, S.N.; Turner, A.J.; Knight, A.C.; Burch, R.; Freeman, C.; Wade, C.; Garner, J.C. Occupational Footwear Design Influences Biomechanics and Physiology of Human Postural Control and Fall Risk. Appl. Sci. 2022, 13, 116. [Google Scholar] [CrossRef]
- Ghorbani, F.; Kamyab, M.; Azadinia, F.; Ahmadi, A. The Reliability and Concurrent Validity of Digital Inclinometer, Smartphone Applications, and the Cervical Range of Motion Device for Measuring the Cervical Range of Motion. Iran. Rehabil. J. 2020, 18, 405–418. [Google Scholar] [CrossRef]
- Ahmed, I.; Bandpei, M.A.M.; Gilani, S.A.; Ahmad, A.; Zaidi, F. Reliability of dual inclinometer for lumbar range of motion using two different Landmarking techniques. JPMA. J. Pak. Med. Assoc. 2022, 72, 1994–1997. [Google Scholar] [CrossRef]
- Rondanelli, M.; Perna, S.; Astrone, P.; Grugnetti, A.; Solerte, S.B.; Guido, D. Twenty-four-week effects of liraglutide on body composition, adherence to appetite, and lipid profile in overweight and obese patients with type 2 diabetes mellitus. Patient Prefer. Adherence 2016, 10, 407–413. [Google Scholar] [PubMed]
| Variables | Diabetes Group (n = 85) | HealthyGroup (n = 85) | p-Value |
|---|---|---|---|
| Age in years | 62.13 ± 4.82 | 61.42 ± 3.98 | 0.159 |
| Gender ratio (n) M: F | 46:39 | 45:40 | 0.186 |
| Body mass index (kg/m2) | 24.12 ± 3.26 | 23.33 ± 2.13 | 0.135 |
| Duration of diabetes in years | 7.63 ± 1.98 | - | - |
| Glycosylated hemoglobin | 7.46 ± 0.63 | - | - |
| Variables | T2DM Group (n = 85) | Healthy Group (n = 85) | 95% CI of the Difference | Cohen’s d | SEM | MDC | p-Value | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Lumber JRE in flexion (⁰) | 4.83 ± 1.23 | 1.98 ± 0.99 | 0.96 | 3.01 | 1.36 | 0.13 | 0.39 | <0.001 |
| Lumbar JRE in extension (⁰) | 5.33 ± 1.41 | 2.22 ± 1.13 | 1.21 | 3.92 | 1.74 | 0.16 | 0.44 | <0.001 |
| Lumbar JRE in lateral bending left (⁰) | 4.56 ± 1.78 | 2.34 ± 1.11 | 1.23 | 3.01 | 1.66 | 0.16 | 0.39 | <0.001 |
| Lumbar JRE in lateral bending right (⁰) | 4.23 ± 1.64 | 2.22 ± 1.08 | 1.76 | 2.94 | 1.93 | 0.19 | 0.37 | <0.001 |
| Lumbar JRE in Flexion (⁰) | Lumbar JRE in Extension (⁰) | Lumbar JRE in Left Lateral Bending (⁰) | Lumbar JRE in Right Lateral Bending (⁰) | ||
|---|---|---|---|---|---|
| HbA1c % | r | 0.49 | 0.51 | 0.45 | 0.48 |
| p | <0.001 | <0.001 | <0.001 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
ALMohiza, M.A.; Reddy, R.S.; Alkhamis, B.A.; Alghamdi, N.H.; Alshahrani, A.; Ponneru, B.R.; Mukherjee, D. A Cross-Sectional Study Investigating Lumbar Proprioception Impairments in Individuals with Type 2 Diabetes Mellitus: Correlations with Glycated Hemoglobin Levels. Biomedicines 2023, 11, 2068. https://doi.org/10.3390/biomedicines11072068
ALMohiza MA, Reddy RS, Alkhamis BA, Alghamdi NH, Alshahrani A, Ponneru BR, Mukherjee D. A Cross-Sectional Study Investigating Lumbar Proprioception Impairments in Individuals with Type 2 Diabetes Mellitus: Correlations with Glycated Hemoglobin Levels. Biomedicines. 2023; 11(7):2068. https://doi.org/10.3390/biomedicines11072068
Chicago/Turabian StyleALMohiza, Mohammad A., Ravi Shankar Reddy, Batool Abdulelah Alkhamis, Nabeel Hamdan Alghamdi, Adel Alshahrani, Bhaskar Reddy Ponneru, and Debjani Mukherjee. 2023. "A Cross-Sectional Study Investigating Lumbar Proprioception Impairments in Individuals with Type 2 Diabetes Mellitus: Correlations with Glycated Hemoglobin Levels" Biomedicines 11, no. 7: 2068. https://doi.org/10.3390/biomedicines11072068
APA StyleALMohiza, M. A., Reddy, R. S., Alkhamis, B. A., Alghamdi, N. H., Alshahrani, A., Ponneru, B. R., & Mukherjee, D. (2023). A Cross-Sectional Study Investigating Lumbar Proprioception Impairments in Individuals with Type 2 Diabetes Mellitus: Correlations with Glycated Hemoglobin Levels. Biomedicines, 11(7), 2068. https://doi.org/10.3390/biomedicines11072068







