Strain Echocardiography in Acute COVID-19 and Post-COVID Syndrome: More than Just a Snapshot
Abstract
1. Introduction
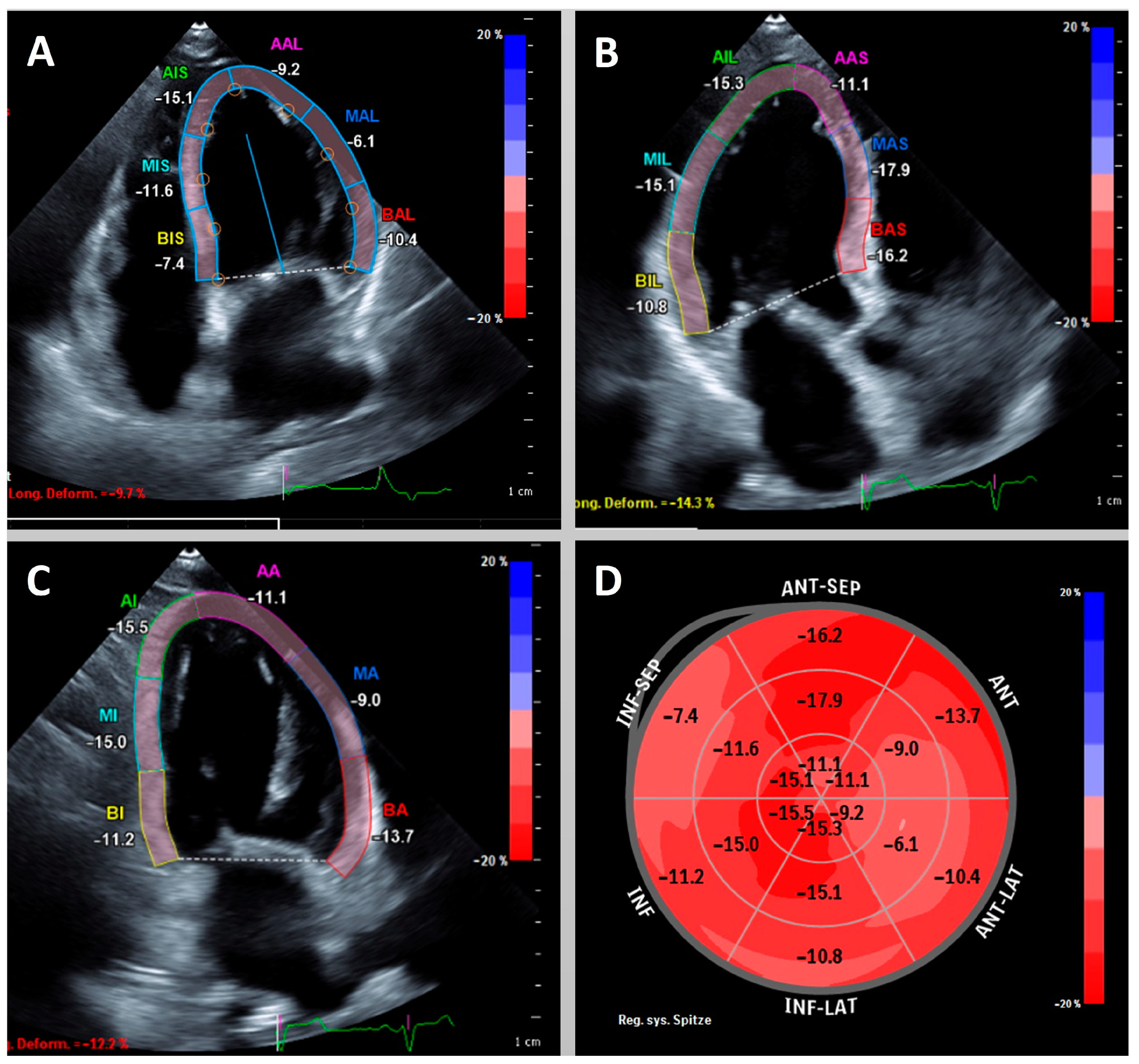
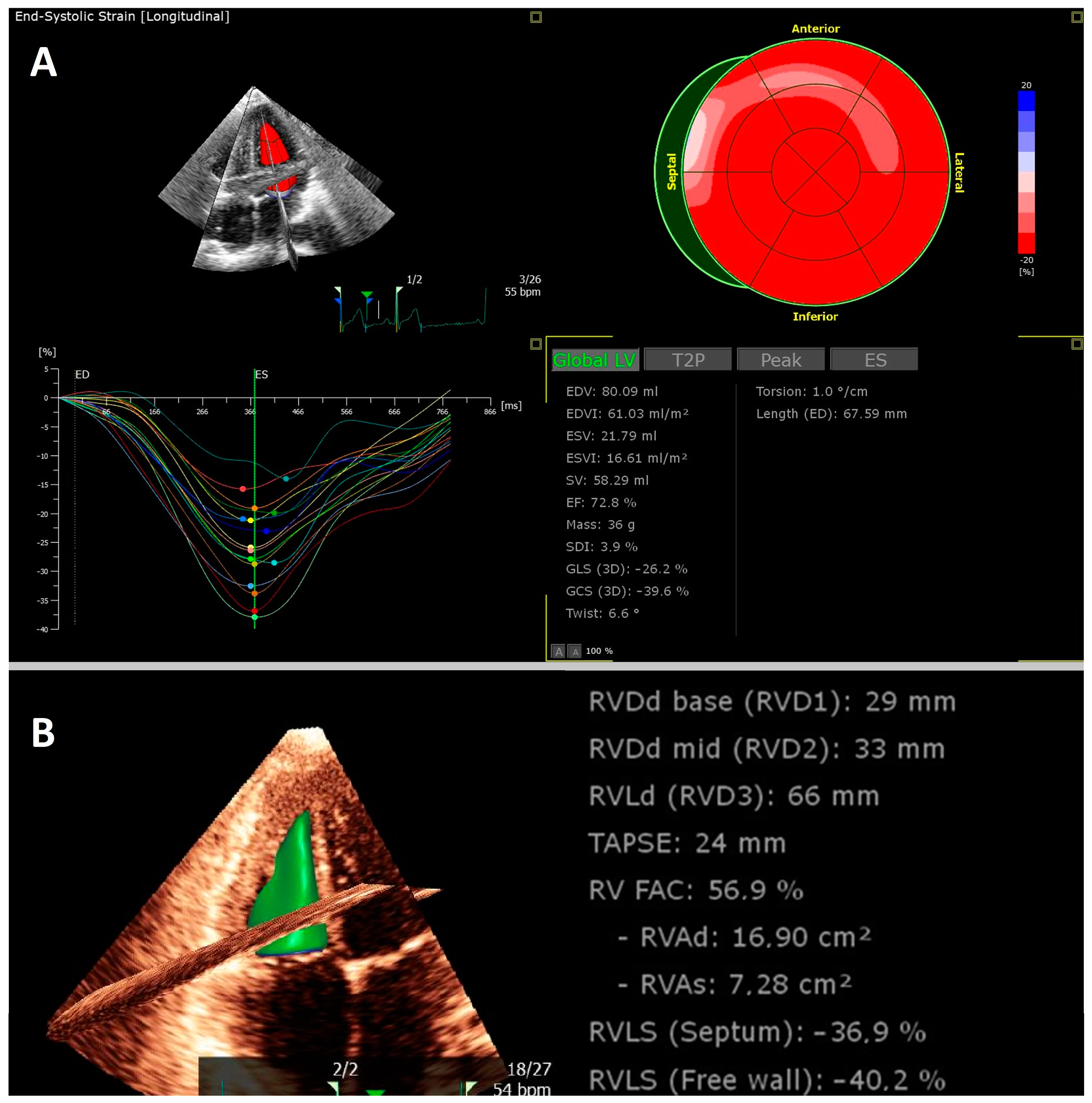
2. Strain in Acute COVID-19
3. Strain in the Diagnostic Work-Up of Post-COVID Syndrome
4. Current Limitations of Knowledge and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Doerner, J.; Bunck, A.C.; Michels, G.; Maintz, D.; Baeßler, B. Incremental value of cardiovascular magnetic resonance feature tracking derived atrial and ventricular strain parameters in a comprehensive approach for the diagnosis of acute myocarditis. Eur. J. Radiol. 2018, 104, 120–128. [Google Scholar] [CrossRef]
- Gavara, J.; Rodriguez-Palomares, J.F.; Valente, F.; Monmeneu, J.V.; Lopez-Lereu, M.P.; Bonanad, C.; Ferreira-Gonzalez, I.; Garcia Del Blanco, B.; Rodriguez-Garcia, J.; Mutuberria, M.; et al. Prognostic Value of Strain by Tissue Tracking Cardiac Magnetic Resonance After ST-Segment Elevation Myocardial Infarction. JACC Cardiovasc. Imaging 2018, 11, 1448–1457. [Google Scholar] [CrossRef] [PubMed]
- Stiermaier, T.; Lange, T.; Chiribiri, A.; Möller, C.; Graf, T.; Villnow, C.; Raaz, U.; Villa, A.; Kowallick, J.T.; Lotz, J.; et al. Left ventricular myocardial deformation in Takotsubo syndrome: A cardiovascular magnetic resonance myocardial feature tracking study. Eur. Radiol. 2018, 28, 5160–5170. [Google Scholar] [CrossRef]
- Oikonomou, E.K.; Kokkinidis, D.G.; Kampaktsis, P.N.; Amir, E.A.; Marwick, T.H.; Gupta, D.; Thavendiranathan, P. Assessment of Prognostic Value of Left Ventricular Global Longitudinal Strain for Early Prediction of Chemotherapy-Induced Cardiotoxicity: A Systematic Review and Meta-analysis. JAMA Cardiol. 2019, 4, 1007–1018. [Google Scholar] [CrossRef] [PubMed]
- Gaibazzi, N.; Bergamaschi, L.; Pizzi, C.; Tuttolomondo, D. Resting global longitudinal strain and stress echocardiography to detect coronary artery disease burden. Eur. Heart J.-Cardiovasc. Imaging 2023, jead046. [Google Scholar] [CrossRef] [PubMed]
- Shi, S.; Qin, M.; Shen, B.; Cai, Y.; Liu, T.; Yang, F.; Gong, W.; Liu, X.; Liang, J.; Zhao, Q.; et al. Association of Cardiac Injury with Mortality in Hospitalized Patients With COVID-19 in Wuhan, China. JAMA Cardiol. 2020, 5, 802–810. [Google Scholar] [CrossRef] [PubMed]
- Halushka, M.K.; Vander Heide, R.S. Myocarditis is rare in COVID-19 autopsies: Cardiovascular findings across 277 postmortem examinations. Cardiovasc. Pathol. 2021, 50, 107300. [Google Scholar] [CrossRef]
- Nishiga, M.; Wang, D.W.; Han, Y.; Lewis, D.B.; Wu, J.C. COVID-19 and cardiovascular disease: From basic mechanisms to clinical perspectives. Nat. Rev. Cardiol. 2020, 17, 543–558. [Google Scholar] [CrossRef]
- Timpau, A.-S.; Miftode, R.-S.; Leca, D.; Timpau, R.; Miftode, I.-L.; Petris, A.O.; Costache, I.I.; Mitu, O.; Nicolae, A.; Oancea, A.; et al. A Real Pandora’s Box in Pandemic Times: A Narrative Review on the Acute Cardiac Injury Due to COVID-19. Life 2022, 12, 1085. [Google Scholar] [CrossRef]
- Yamaoka-Tojo, M. Vascular Endothelial Glycocalyx Damage in COVID-19. Int. J. Mol. Sci. 2020, 21, 9712. [Google Scholar] [CrossRef]
- Bizjak, D.A.; John, L.; Matits, L.; Uhl, A.; Schulz, S.V.W.; Schellenberg, J.; Peifer, J.; Bloch, W.; Weiß, M.; Grüner, B.; et al. SARS-CoV-2 Altered Hemorheological and Hematological Parameters during One-Month Observation Period in Critically Ill COVID-19 Patients. Int. J. Mol. Sci. 2022, 23, 15332. [Google Scholar] [CrossRef] [PubMed]
- Vollenberg, R.; Tepasse, P.-R.; Ochs, K.; Floer, M.; Strauss, M.; Rennebaum, F.; Kabar, I.; Rovas, A.; Nowacki, T. Indications of Persistent Glycocalyx Damage in Convalescent COVID-19 Patients: A Prospective Multicenter Study and Hypothesis. Viruses 2021, 13, 2324. [Google Scholar] [CrossRef] [PubMed]
- Shafiee, S.; Cegolon, L.; Khafaei, M.; Gholami, N.; Zhao, S.; Khalesi, N.; Moosavian, H.; Fathi, S.; Izadi, M.; Ghadian, A.; et al. Gastrointestinal cancers, ACE-2/TMPRSS2 expression and susceptibility to COVID-19. Cancer Cell Int. 2021, 21, 431. [Google Scholar] [CrossRef] [PubMed]
- Rahban, M.; Stanek, A.; Hooshmand, A.; Khamineh, Y.; Ahi, S.; Kazim, S.N.; Ahmad, F.; Muronetz, V.; Samy Abousenna, M.; Zolghadri, S.; et al. Infection of Human Cells by SARS-CoV-2 and Molecular Overview of Gastrointestinal, Neurological, and Hepatic Problems in COVID-19 Patients. J. Clin. Med. 2021, 10, 4802. [Google Scholar] [CrossRef] [PubMed]
- Soriano, J.B.; Murthy, S.; Marshall, J.C.; Relan, P.; Diaz, J.V. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect. Dis. 2022, 22, e102–e107. [Google Scholar] [CrossRef]
- Peter, R.S.; Nieters, A.; Kräusslich, H.-G.; Brockmann, S.O.; Göpel, S.; Kindle, G.; Merle, U.; Steinacker, J.M.; Rothenbacher, D.; Kern, W.V. Post-acute sequelae of covid-19 six to 12 months after infection: Population based study. BMJ 2022, 379, e071050. [Google Scholar] [CrossRef]
- Stöbe, S.; Richter, S.; Seige, M.; Stehr, S.; Laufs, U.; Hagendorff, A. Echocardiographic characteristics of patients with SARS-CoV-2 infection. Clin. Res. Cardiol. 2020, 109, 1549–1566. [Google Scholar] [CrossRef]
- Stockenhuber, A.; Vrettos, A.; Androschuck, V.; George, M.; Robertson, C.; Bowers, N.; Clifford, P.; Firoozan, S. A pilot study on right ventricular longitudinal strain as a predictor of outcome in COVID-19 patients with evidence of cardiac involvement. Echocardiography 2021, 38, 222–229. [Google Scholar] [CrossRef]
- Li, Y.; Li, H.; Zhu, S.; Xie, Y.; Wang, B.; He, L.; Zhang, D.; Zhang, Y.; Yuan, H.; Wu, C.; et al. Prognostic Value of Right Ventricular Longitudinal Strain in Patients With COVID-19. JACC Cardiovasc. Imaging 2020, 13, 2287–2299. [Google Scholar] [CrossRef]
- Bleakley, C.; Singh, S.; Garfield, B.; Morosin, M.; Surkova, E.; Mandalia, M.S.; Dias, B.; Androulakis, E.; Price, L.C.; McCabe, C.; et al. Right ventricular dysfunction in critically ill COVID-19 ARDS. Int. J. Cardiol. 2021, 327, 251–258. [Google Scholar] [CrossRef]
- Park, J.; Kim, Y.; Pereira, J.; Hennessey, K.C.; Faridi, K.F.; McNamara, R.L.; Velazquez, E.J.; Hur, D.J.; Sugeng, L.; Agarwal, V. Understanding the role of left and right ventricular strain assessment in patients hospitalized with COVID-19. Am. Heart J. Plus Cardiol. Res. Pract. 2021, 6, 100018. [Google Scholar] [CrossRef]
- Xie, Y.; Wang, L.; Li, M.; Li, H.; Zhu, S.; Wang, B.; He, L.; Zhang, D.; Zhang, Y.; Yuan, H.; et al. Biventricular Longitudinal Strain Predict Mortality in COVID-19 Patients. Front. Cardiovasc. Med. 2021, 7, 632434. [Google Scholar] [CrossRef] [PubMed]
- Shmueli, H.; Shah, M.; Ebinger, J.E.; Nguyen, L.-C.; Chernomordik, F.; Flint, N.; Botting, P.; Siegel, R.J. Left ventricular global longitudinal strain in identifying subclinical myocardial dysfunction among patients hospitalized with COVID-19. IJC Heart Vasc. 2021, 32, 100719. [Google Scholar] [CrossRef] [PubMed]
- Minhas, A.S.; Gilotra, N.A.; Goerlich, E.; Metkus, T.; Garibaldi, B.T.; Sharma, G.; Bavaro, N.; Phillip, S.; Michos, E.D.; Hays, A.G. Myocardial Work Efficiency, A Novel Measure of Myocardial Dysfunction, Is Reduced in COVID-19 Patients and Associated with In-Hospital Mortality. Front. Cardiovasc. Med. 2021, 8, 461. [Google Scholar] [CrossRef]
- Ghantous, E.; Shetrit, A.; Hochstadt, A.; Banai, A.; Lupu, L.; Levi, E.; Szekely, Y.; Schellekes, N.; Jacoby, T.; Zahler, D.; et al. Cardiologic Manifestations in Omicron-Type Versus Wild-Type COVID-19: A Systematic Echocardiographic Study. JAHA 2023, 12, e027188. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, H.S.; Bui, Q.M.; King, K.; De Maria, A.; Daniels, L.B. Subclinical left ventricular dysfunction in COVID-19. IJC Heart Vasc. 2021, 34, 100770. [Google Scholar] [CrossRef]
- Gonzalez, F.A.; Ângelo-Dias, M.; Martins, C.; Gomes, R.; Bacariza, J.; Fernandes, A.; Borrego, L.M. Left atrial strain is associated with distinct inflammatory and immune profile in patients with COVID-19 pneumonia. Ultrasound J. 2023, 15, 2. [Google Scholar] [CrossRef]
- D’Andrea, A.; Cante, L.; Palermi, S.; Carbone, A.; Ilardi, F.; Sabatella, F.; Crescibene, F.; Di Maio, M.; Giallauria, F.; Messalli, G.; et al. COVID-19 Myocarditis: Prognostic Role of Bedside Speckle-Tracking Echocardiography and Association with Total Scar Burden. Int. J. Environ. Res. Public Health 2022, 19, 5898. [Google Scholar] [CrossRef] [PubMed]
- Lassen, M.C.H.; Skaarup, K.G.; Lind, J.N.; Alhakak, A.S.; Sengeløv, M.; Nielsen, A.B.; Simonsen, J.Ø.; Johansen, N.D.; Davidovski, F.S.; Christensen, J.; et al. Recovery of cardiac function following COVID-19—ECHOVID-19: A prospective longitudinal cohort study. Eur. J. Heart Fail. 2021, 23, 1903–1912. [Google Scholar] [CrossRef]
- Oikonomou, E.; Lampsas, S.; Theofilis, P.; Souvaliotis, N.; Papamikroulis, G.A.; Katsarou, O.; Kalogeras, K.; Pantelidis, P.; Papaioannou, T.G.; Tsatsaragkou, A.; et al. Impaired left ventricular deformation and ventricular-arterial coupling in post-COVID-19: Association with autonomic dysregulation. Heart Vessel. 2023, 38, 381–393. [Google Scholar] [CrossRef] [PubMed]
- Shimoni, O.; Korenfeld, R.; Goland, S.; Meledin, V.; Haberman, D.; George, J.; Shimoni, S. Subclinical Myocardial Dysfunction in Patients Recovered from COVID-19 Disease: Correlation with Exercise Capacity. Biology 2021, 10, 1201. [Google Scholar] [CrossRef] [PubMed]
- Tryfou, E.S.; Kostakou, P.M.; Chasikidis, C.G.; Kostopoulos, V.S.; Serafetinidis, I.I.; Ferdianaki, E.K.; Mihas, C.; Olympios, C.D.; Kouris, N.T. Biventricular myocardial function in Covid-19 recovered patients assessed by speckle tracking echocardiography: A prospective cohort echocardiography study. Int. J. Cardiovasc. Imaging 2021, 38, 995–1003. [Google Scholar] [CrossRef] [PubMed]
- Caiado, L.D.C.; Azevedo, N.C.; Azevedo, R.R.C.; Caiado, B.R. Cardiac involvement in patients recovered from COVID-19 identified using left ventricular longitudinal strain. J. Echocardiogr. 2022, 20, 51–56. [Google Scholar] [CrossRef]
- Petersen, E.L.; Goßling, A.; Adam, G.; Aepfelbacher, M.; Behrendt, C.-A.; Cavus, E.; Cheng, B.; Fischer, N.; Gallinat, J.; Kühn, S.; et al. Multi-organ assessment in mainly non-hospitalized individuals after SARS-CoV-2 infection: The Hamburg City Health Study COVID programme. Eur. Heart J. 2022, 43, 1124–1137. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Zamora, S.; Picco, J.M.; Lepori, A.J.; Galello, M.I.; Saad, A.K.; Ayón, M.; Monga-Aguilar, N.; Shehadeh, I.; Manganiello, C.F.; Izaguirre, C.; et al. Abnormal echocardiographic findings after COVID-19 infection: A multicenter registry. Int. J. Cardiovasc. Imaging 2023, 39, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Young, K.A.; Krishna, H.; Jain, V.; Hamza, I.; Scott, C.G.; Pellikka, P.A.; Villarraga, H.R. Serial Left and Right Ventricular Strain Analysis in Patients Recovered from COVID-19. J. Am. Soc. Echocardiogr. 2022, 35, 1055–1063. [Google Scholar] [CrossRef]
- Baruch, G.; Rothschild, E.; Sadon, S.; Szekely, Y.; Lichter, Y.; Kaplan, A.; Taieb, P.; Banai, A.; Hochstadt, A.; Merdler, I.; et al. Evolution of right and left ventricle routine and speckle-tracking echocardiography in patients recovering from coronavirus disease 2019: A longitudinal study. Eur. Heart J. Cardiovasc. Imaging 2022, 23, 1055–1065. [Google Scholar] [CrossRef]
- Akkaya, F.; Yenerçağ, F.N.T.; Kaya, A.; Şener, Y.Z.; Bağcı, A. Long term effects of mild severity COVID-19 on right ventricular functions. Int. J. Cardiovasc. Imaging 2021, 37, 3451–3457. [Google Scholar] [CrossRef]
- García-Abellán, J.; Fernández, M.; Padilla, S.; García, J.A.; Agulló, V.; Lozano, V.; Ena, N.; García-Sánchez, L.; Gutiérrez, F.; Masiá, M. Immunologic phenotype of patients with long-COVID syndrome of 1-year duration. Front. Immunol. 2022, 13, 920627. [Google Scholar] [CrossRef]
- Ozer, P.K.; Govdeli, E.A.; Baykiz, D.; Karaayvaz, E.B.; Medetalibeyoglu, A.; Catma, Y.; Elitok, A.; Cagatay, A.; Umman, B.; Oncul, A.; et al. Impairment of right ventricular longitudinal strain associated with severity of pneumonia in patients recovered from COVID-19. Int. J. Cardiovasc. Imaging 2021, 37, 2387–2397. [Google Scholar] [CrossRef]
- Mahajan, S.; Kunal, S.; Shah, B.; Garg, S.; Palleda, G.M.; Bansal, A.; Batra, V.; Yusuf, J.; Mukhopadhyay, S.; Kumar, S.; et al. Left ventricular global longitudinal strain in COVID-19 recovered patients. Echocardiography 2021, 38, 1722–1730. [Google Scholar] [CrossRef] [PubMed]
- Sugimoto, T.; Dulgheru, R.; Bernard, A.; Ilardi, F.; Contu, L.; Addetia, K.; Caballero, L.; Akhaladze, N.; Athanassopoulos, G.D.; Barone, D.; et al. Echocardiographic reference ranges for normal left ventricular 2D strain: Results from the EACVI NORRE study. Eur. Heart J. Cardiovasc. Imaging 2017, 18, 833–840. [Google Scholar] [CrossRef]
- Luchian, M.-L.; Motoc, A.; Lochy, S.; Magne, J.; Belsack, D.; de Mey, J.; Roosens, B.; van den Bussche, K.; Boeckstaens, S.; Chameleva, H.; et al. Subclinical Myocardial Dysfunction in Patients with Persistent Dyspnea One Year after COVID-19. Diagnostics 2021, 12, 57. [Google Scholar] [CrossRef] [PubMed]
- Baum, P.; Do, L.; Deterding, L.; Lier, J.; Kunis, I.; Saur, D.; Classen, J.; Wirtz, H.; Laufs, U. Cardiac function in relation to functional status and fatigue in patients with post-COVID syndrome. Sci. Rep. 2022, 12, 19575. [Google Scholar] [CrossRef]
- ZeinElabdeen, S.G.; Sherif, A.; Kandil, N.T.; Altabib, A.M.O.; Abdelrashid, M.A. Left atrial longitudinal strain analysis in long COVID-19 syndrome. Int. J. Cardiovasc. Imaging 2023, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Kalogeropoulos, A.P.; Georgiopoulou, V.V.; Butler, J. From risk factors to structural heart disease: The role of inflammation. Heart Fail. Clin. 2012, 8, 113–123. [Google Scholar] [CrossRef]
- Schellenberg, J.; Ahathaller, M.; Matits, L.; Kirsten, J.; Kersten, J.; Steinacker, J. Left ventricular global longitudinal strain as a parameter of mild myocardial dysfunction in athletes after COVID-19. Preprint. medRxiv 2023. [Google Scholar] [CrossRef]
- Kersten, J.; Hoyo, L.; Wolf, A.; Hüll, E.; Nunn, S.; Tadic, M.; Scharnbeck, D.; Rottbauer, W.; Buckert, D. Cardiopulmonary Exercise Testing Distinguishes between Post-COVID-19 as a Dysfunctional Syndrome and Organ Pathologies. Int. J. Environ. Res. Public Health 2022, 19, 11421. [Google Scholar] [CrossRef]
- Gluckman, T.J.; Bhave, N.M.; Allen, L.A.; Chung, E.H.; Spatz, E.S.; Ammirati, E.; Baggish, A.L.; Bozkurt, B.; Cornwell, W.K.; Harmon, K.G.; et al. 2022 ACC Expert Consensus Decision Pathway on Cardiovascular Sequelae of COVID-19 in Adults: Myocarditis and Other Myocardial Involvement, Post-Acute Sequelae of SARS-CoV-2 Infection, and Return to Play: A Report of the American College of Cardiology Solution Set Oversight Committee. J. Am. Coll. Cardiol. 2022, 79, 1717–1756. [Google Scholar] [CrossRef]
- Gherbesi, E.; Bergamaschi, L.; Cusmano, I.; Tien, T.T.; Paolisso, P.; Foà, A.; Pizzi, C.; Barosi, A. The usefulness of speckle tracking echocardiography in identifying subclinical myocardial dysfunction in young adults recovered from mild COVID-19. Echocardiography 2022, 39, 1190–1197. [Google Scholar] [CrossRef]
- Italia, L.; Ingallina, G.; Napolano, A.; Boccellino, A.; Belli, M.; Cannata, F.; Rolando, M.; Ancona, F.; Melillo, F.; Stella, S.; et al. Subclinical myocardial dysfunction in patients recovered from COVID-19. Echocardiography 2021, 38, 1778–1786. [Google Scholar] [CrossRef] [PubMed]
- Petersen, S.E.; Friedrich, M.G.; Leiner, T.; Elias, M.D.; Ferreira, V.M.; Fenski, M.; Flamm, S.D.; Fogel, M.; Garg, R.; Halushka, M.K.; et al. Cardiovascular Magnetic Resonance for Patients With COVID-19. JACC Cardiovasc. Imaging 2021, 15, 685–699. [Google Scholar] [CrossRef]
- Kotecha, T.; Knight, D.S.; Razvi, Y.; Kumar, K.; Vimalesvaran, K.; Thornton, G.; Patel, R.; Chacko, L.; Brown, J.T.; Coyle, C.; et al. Patterns of myocardial injury in recovered troponin-positive COVID-19 patients assessed by cardiovascular magnetic resonance. Eur. Heart J. 2021, 42, 1866–1878. [Google Scholar] [CrossRef]
- Haunhorst, S.; Bloch, W.; Wagner, H.; Ellert, C.; Krüger, K.; Vilser, D.C.; Finke, K.; Reuken, P.; Pletz, M.W.; Stallmach, A.; et al. Long COVID: A narrative review of the clinical aftermaths of COVID-19 with a focus on the putative pathophysiology and aspects of physical activity. Oxf. Open Immunol. 2022, 3, iqac006. [Google Scholar] [CrossRef] [PubMed]
- Charfeddine, S.; Ibn Hadj Amor, H.; Jdidi, J.; Torjmen, S.; Kraiem, S.; Hammami, R.; Bahloul, A.; Kallel, N.; Moussa, N.; Touil, I.; et al. Long COVID 19 Syndrome: Is It Related to Microcirculation and Endothelial Dysfunction? Insights From TUN-EndCOV Study. Front. Cardiovasc. Med. 2021, 8, 745758. [Google Scholar] [CrossRef] [PubMed]
- Osiaevi, I.; Schulze, A.; Evers, G.; Harmening, K.; Vink, H.; Kümpers, P.; Mohr, M.; Rovas, A. Persistent capillary rarefication in long COVID syndrome. Angiogenesis 2023, 26, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Amzulescu, M.S.; de Craene, M.; Langet, H.; Pasquet, A.; Vancraeynest, D.; Pouleur, A.C.; Vanoverschelde, J.L.; Gerber, B.L. Myocardial strain imaging: Review of general principles, validation, and sources of discrepancies. Eur. Heart J. Cardiovasc. Imaging 2019, 20, 605–619. [Google Scholar] [CrossRef] [PubMed]
- Nicolosi, G.L. The strain and strain rate imaging paradox in echocardiography: Overabundant literature in the last two decades but still uncertain clinical utility in an individual case. Arch. Med. Sci. Atheroscler. Dis. 2020, 5, e297–e305. [Google Scholar] [CrossRef]
| Reference | Number of Patients | Subject | Main Finding |
|---|---|---|---|
| Stöbe S. et al. (August 2020) [17] | 19 | LV GLS, GCS, GRS Free wall RV LS | There are patterns of myocardial injury in hospitalised patients that differ from other cardiomyopathies, including viral myocarditis. |
| Li Y. et al. (November 2020) [19] | 120 | Free wall RV LS | Evaluating consecutive hospitalized patients, RV GLS was the best predictor of outcome and can help to identify patients at higher risk, with a cut-off of −23%. |
| Stockenhuber A. et al. (December 2020) [18] | 30 | Free wall RV LS | In hospitalised patients with elevated levels of troponin I, worsening free wall RV LS was associated with mortality. |
| Xie Y. et al. (January 2021) [22] | 132 | Four-chamber LV GLS Free wall RV LS | LV GLS (four chamber) and free wall RV LS were independent predictors of mortality and were useful tools in follow-up during convalescence of hospitalized patients. |
| Minhas A. et al. (June 2021) [24] | 136 | LV GLS MWE | In hospitalised patients, STE parameters were impaired in a significant proportion of patients. Worse values were associated with mortality and inflammatory biomarkers. |
| Shmueli H. et al. (January 2021) [23] | 40 | LV GLS | LV GLS was reduced in a high proportion of hospitalised patients. Impairment in LV GLS was correlated with elevated levels of troponin T and inflammatory biomarkers. |
| Bhatia H. et al. (March 2021) [26] | 67 | LV GLS | Despite normal LVEF, LV GLS was impaired in 91% of hospitalised patients, with improvement in those patients who survived to discharge. |
| Bleakley C. et al. (March 2021) [20] | 90 | Free wall RV LS | In patients in need of membrane oxygenation, free wall RV LS was not associated with cardiac biomarkers and could not show any additional benefit to other measurements of RV function. |
| Park J. (May 2021) [21] | 48 | LV GLS Free wall RV LS | In hospitalised patients, an LV GLS of greater than –13.8% was associated with a 5.15-fold increased risk of death. Free wall RV LS was not associated with that outcome. |
| D’Andrea A. et al. (May 2022) [28] | 55 with signs for myocarditis in CMR | LV GLS | LV GLS in acute illness was associated with total scar burden in CMR and functional recovery at follow-up. Patients were initially hospitalized. |
| Ghantous E. et al. (January 2023) [25] | 148 omicron propensity matched to wild type (alpha) | LV GLS RV GLS Free wall RV LS | All strain values were similar in patients with omicron variants and the wild type. Other hemodynamic and right ventricular parameters were worse in wild type patients. Patients included were in need of hospitalization. |
| Gonzalez F. et al. (January 2023) [27] | 30 | LA strain | In ICU patients, LA strain was more sensitive in detecting diastolic dysfunction than classical markers. It revealed protracted inflammatory states. |
| Reference | Number of Patients | Time after Infection | Subject | Main Finding |
|---|---|---|---|---|
| Ozer P. et al. (April 2021) [40] | 79 | 133 ± 35 days | RV GLS Free wall RV LS | Impairment, especially in free wall RV LS, was correlated to disease severity, age, male sex, steroid treatment and presence of pneumonia in a chest CT scan. |
| Akkaya F. et al. (June 2021) [38] | 105 | 3 months | RV GLS Free wall RV LS | In mild COVID-19, RV longitudinal strain was impaired and inversely correlated to inflammatory biomarkers and D-dimers. |
| Caiado L. et al. (July 2021) [33] | 100 | 130 ± 70 days | LV GLS Segmental LS | LVEF and LV GLS were normal in post-COVID patients and comparable to healthy controls. |
| Mahajan S. et al. (September 2021) [41] | 134 | 36 ± 5 days | LV GLS | Impaired LV GLS occurred in 29.9% of patients, with a significant correlation to initial disease severity. |
| Italia L. et al. (September 2021) [43] | 123 | 85 days (IQR 70, 103) | LV GLS Free wall RV LS | The patients were divided into a group with and a group without troponin T elevation at follow-up as a marker of myocardial injury; LV GLS but not free wall RV LS was significant lower in the group with elevated troponin T. |
| Baruch G. et al. (September 2021) [37] | 80 | 88 ± 33 days | Four-chamber LV GLS RV GLS | LV GLS was impaired in 33% of hospitalised patients, and RV GLS was impaired in 23%; significant improvement was observed in RV GLS but not in LV GLS (8% vs. 25% persistent deterioration, respectively). |
| Lassen M. et al. (October 2021) [29] | 91 | 77 days (IQR 72, 92) | LV GLS RV GLS | During acute COVID-19, LV GLS and RV GLS were impaired compared to healthy controls. This impairment was fully reversible at follow-up in RV GLS but not in LV GLS. |
| Shimoni O. et al. (November 2021) [31] | 184 | 57 days (IQR 27, 100) | LV GLS RV GLS Free wall RV LS | Strain values were reduced compared to those in controls but were not related to initial disease severity. Patients with an LV GLS of −20% or better had improved exercise capacities. |
| Luchian M. et al. (December 2021) [51] | 66 | 1 year | LV GLS MWE | Patients with dyspnoea one year after COVID-19 had lower LV GLS and MWE. |
| Tryfou E. et al. (December 2021) [32] | 100 | 33 ± 9 days | LV GLS Free wall RV LS | LV GLS was significantly impaired in all recovered COVID-19 patients, while free wall RV LS was significantly impaired only in formerly hospitalised patients. |
| Young K. et al. (June 2022) [36] | 259 | 55 days (IQR 37, 92) | LV GLS RV GLS Free wall RV LS | On average, there were no clinically significant differences in STE pre- and post-COVID. Rare reductions were more common in patients with post-COVID symptoms. |
| Gherbesi E. et al. (September 2022) [50] | 40 | At least 3 months | LV GLS RV GLS Free wall RV LS | In young athletes with an asymptomatic or oligosymptomatic course of COVID-19, there was a reduction in LV GLS (but not RV GLS) compared to controls. |
| Garcia-Zamora S. et al. (August 2022) [35] | 595 | 2 months (IQR 1, 3) | LV GLS Free wall RV LS | This registry study included all patients with STE following COVID-19. Overall, LV GLS and RV LS were normal, with abnormal values in 5.7% and 3.1% of patients, respectively. |
| Oikonomou E. et al. (September 2022) [30] | 34 | 1 and 6 months after hospital discharge | LV GLS | One month after hospital discharge, LV GLS was impaired compared to healthy controls. After 6 months, LV GLS improved without reaching the level of the controls. |
| Baum P. et al. (November 2022) [44] | 237 | N/A | LV GLS | LV GLS was impaired in the subgroup of patients with worse fatigue and in patients with elevated troponin T. In most patients, LV GLS was normal. |
| ZeinElabdeen S. et al. (February 2023) [45] | 63 | 4 to 12 weeks | LA strain | LA strain was impaired in symptomatic post-COVID patients. LA reservoir strain and LA stiffness were independent predictors of dyspnoea and exercise intolerance. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kersten, J.; Schellenberg, J.; Jerg, A.; Kirsten, J.; Persch, H.; Liu, Y.; Steinacker, J.M. Strain Echocardiography in Acute COVID-19 and Post-COVID Syndrome: More than Just a Snapshot. Biomedicines 2023, 11, 1236. https://doi.org/10.3390/biomedicines11041236
Kersten J, Schellenberg J, Jerg A, Kirsten J, Persch H, Liu Y, Steinacker JM. Strain Echocardiography in Acute COVID-19 and Post-COVID Syndrome: More than Just a Snapshot. Biomedicines. 2023; 11(4):1236. https://doi.org/10.3390/biomedicines11041236
Chicago/Turabian StyleKersten, Johannes, Jana Schellenberg, Achim Jerg, Johannes Kirsten, Hasema Persch, Yuefei Liu, and Jürgen M. Steinacker. 2023. "Strain Echocardiography in Acute COVID-19 and Post-COVID Syndrome: More than Just a Snapshot" Biomedicines 11, no. 4: 1236. https://doi.org/10.3390/biomedicines11041236
APA StyleKersten, J., Schellenberg, J., Jerg, A., Kirsten, J., Persch, H., Liu, Y., & Steinacker, J. M. (2023). Strain Echocardiography in Acute COVID-19 and Post-COVID Syndrome: More than Just a Snapshot. Biomedicines, 11(4), 1236. https://doi.org/10.3390/biomedicines11041236






