Circulating Biomarkers of Fibrosis Formation in Patients with Arrhythmogenic Cardiomyopathy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Clinical Data Collection
2.3. Measurement of Fibrosis Markers
2.4. Statistics
3. Results
3.1. Patient Characteristics
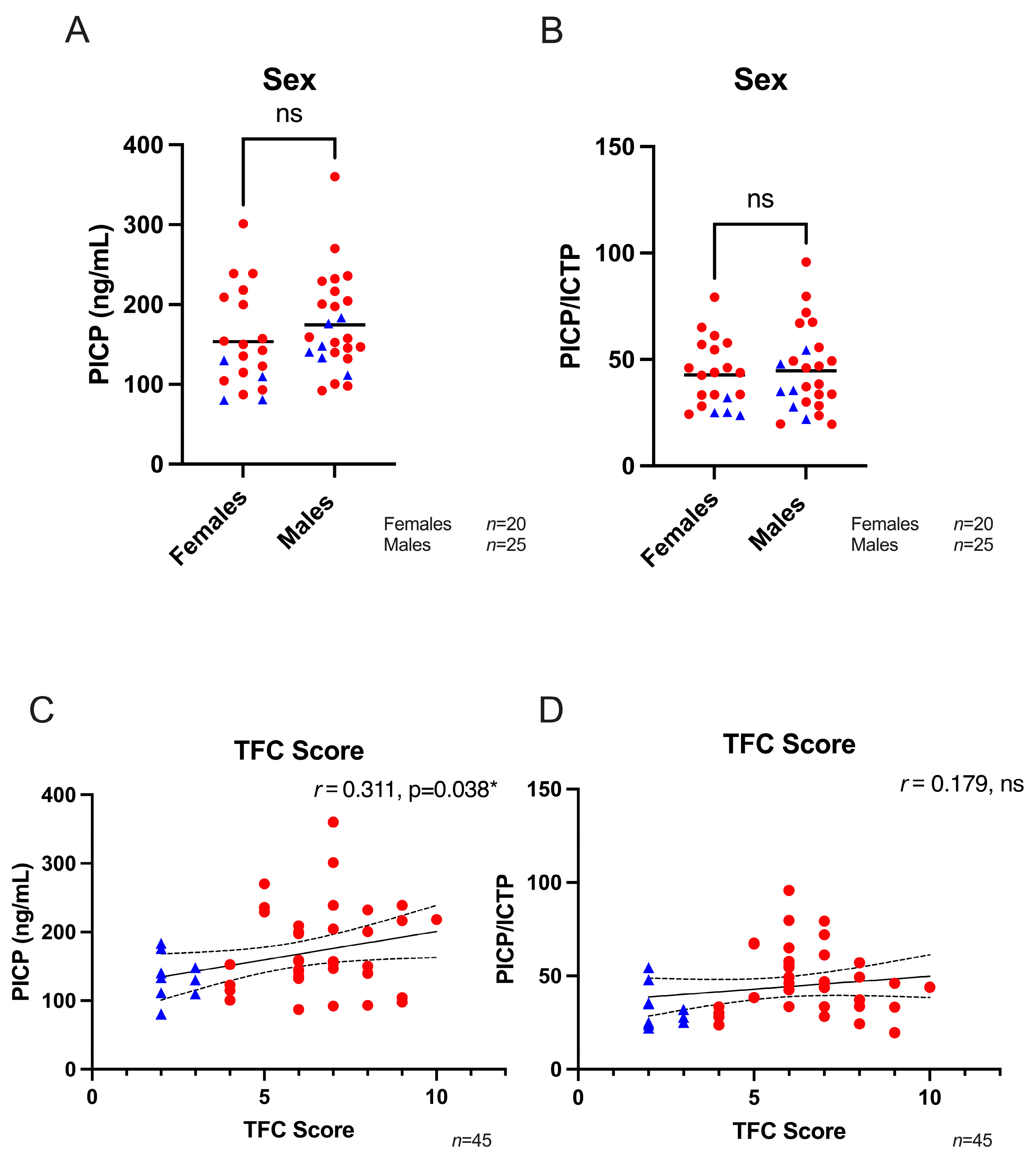
3.2. Fibrosis Biomarkers
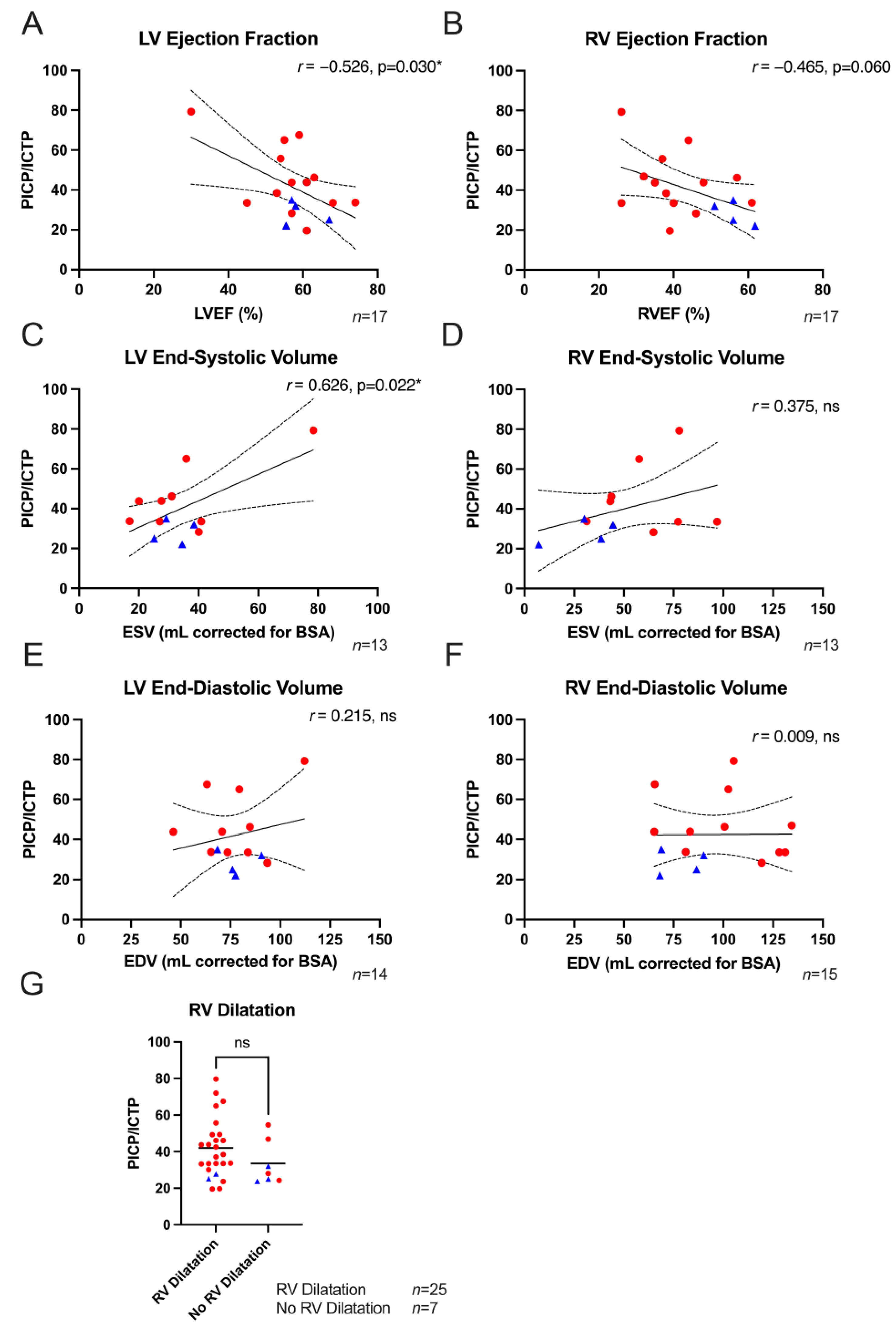
3.3. Structural Parameters and Fibrosis Biomarkers
3.4. Electrical Parameters and Fibrosis Biomarkers
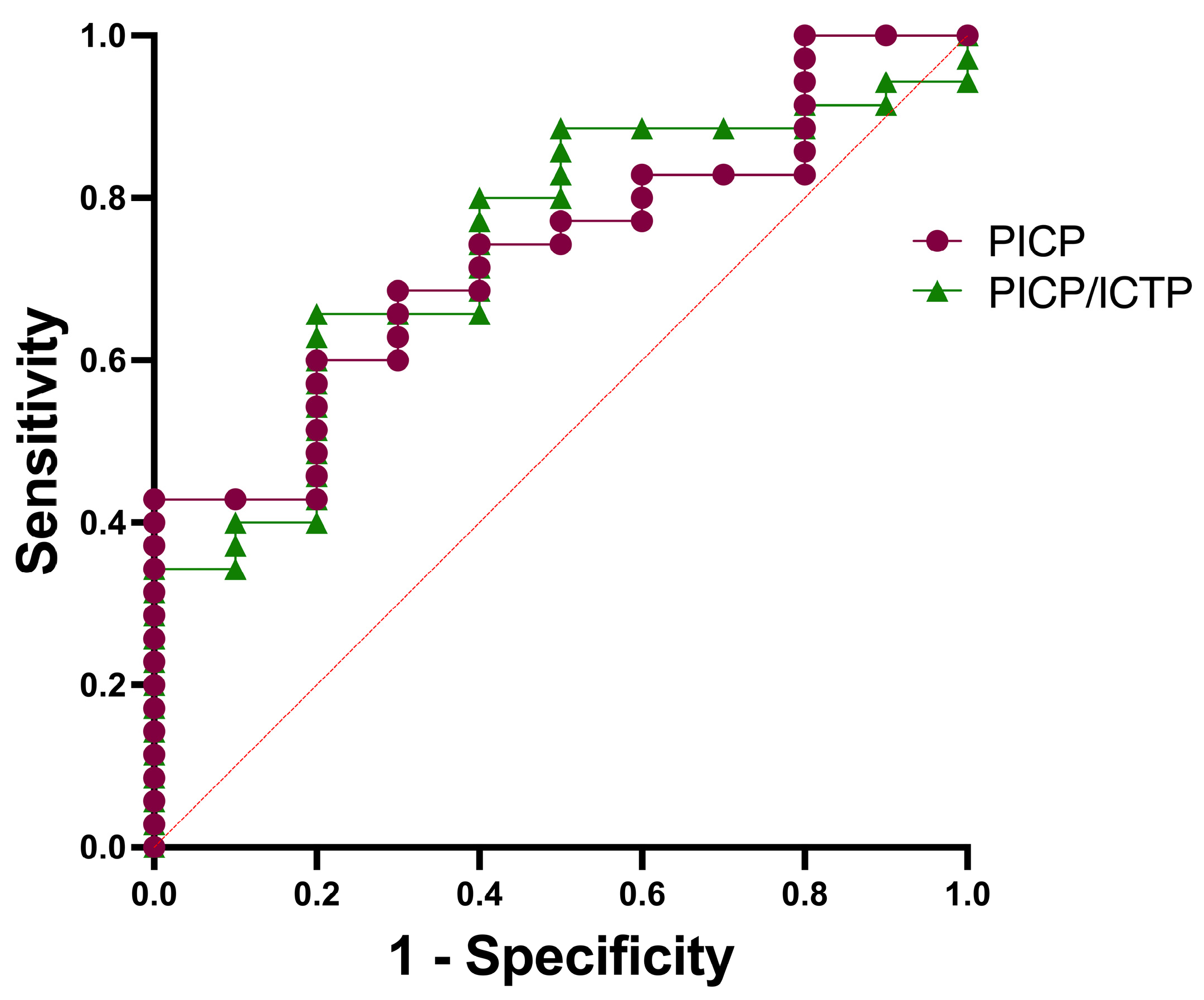
3.5. Diagnostic Value of Fibrosis Biomarkers
4. Discussion
5. Conclusions
6. Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Corrado, D.; Link, M.S.; Calkins, H. Arrhythmogenic right ventricular cardiomyopathy. N. Engl. J. Med. 2017, 376, 61–72. [Google Scholar] [CrossRef] [PubMed]
- Pilichou, K.; Thiene, G.; Bauce, B.; Rigato, I.; Lazzarini, E.; Migliore, F.; Perazzolo Marra, M.; Rizzo, S.; Zorzi, A.; Daliento, L.; et al. Arrhythmogenic cardiomyopathy. Orphanet. J. Rare Dis. 2016, 11, 33. [Google Scholar] [CrossRef] [PubMed]
- van der Voorn, S.M.; Te Riele, A.S.J.M.; Basso, C.; Calkins, H.; Remme, C.A.; van Veen, T.A.B. Arrhythmogenic cardiomyopathy: Pathogenesis, pro-arrhythmic remodelling, and novel approaches for risk stratification and therapy. Cardiovasc. Res. 2020, 116, 1571–1584. [Google Scholar] [CrossRef] [PubMed]
- Haugaa, K.H.; Haland, T.F.; Leren, I.S.; Saberniak, J.; Edvardsen, T. Arrhythmogenic right ventricular cardiomyopathy, clinical manifestations, and diagnosis. Europace 2016, 18, 965–972. [Google Scholar] [CrossRef]
- Eijgenraam, T.R.; Boukens, B.J.; Boogerd, C.J.; Schouten, E.M.; van de Kolk, C.W.A.; Stege, N.M.; te Rijdt, W.P.; Hoorntje, E.T.; van der Zwaag, P.A.; van Rooij, E.; et al. Author Correction: The phospholamban p.(Arg14del) pathogenic variant leads to cardiomyopathy with heart failure and is unresponsive to standard heart failure therapy. Sci. Rep. 2020, 10, 16710. [Google Scholar] [CrossRef]
- Posch, M.G.; Perrot, A.; Geier, C.; Boldt, L.-H.; Schmidt, G.; Lehmkuhl, H.B.; Hetzer, R.; Dietz, R.; Gutberlet, M.; Haverkamp, W.; et al. Genetic deletion of arginine 14 in phospholamban causes dilated cardiomyopathy with attenuated electrocardiographic R amplitudes. Heart Rhythm. 2009, 6, 480–486. [Google Scholar] [CrossRef]
- Groeneweg, J.A.; van der Heijden, J.F.; Dooijes, D.; van Veen, T.A.B.; van Tintelen, J.P.; Hauer, R.N. Arrhythmogenic cardiomyopathy: Diagnosis, genetic background, and risk management. Neth. Heart J. 2014, 22, 316–325. [Google Scholar] [CrossRef]
- Li, G.; Fontaine, G.H.; Fan, S.; Yan, Y.; Bode, P.K.; Duru, F.; Frank, R.; Saguner, A.M. Right atrial pathology in arrhythmogenic right ventricular dysplasia. Cardiol. J. 2019, 26, 736–743. [Google Scholar] [CrossRef]
- de Jong, S.; van Veen, T.A.B.; de Bakker, J.M.T.; van Rijen, H.V.M. Monitoring cardiac fibrosis: A technical challenge. Neth. Heart J. 2012, 20, 44–48. [Google Scholar] [CrossRef]
- Te Rijdt, W.P.; Ten Sande, J.N.; Gorter, T.M.; van der Zwaag, P.A.; van Rijsingen, I.A.; Boekholdt, S.M.; van Tintelen, J.P.; van Haelst, P.L.; Planken, R.N.; de Boer, R.A.; et al. Myocardial fibrosis as an early feature in phospholamban p.Arg14del mutation carriers: Phenotypic insights from cardiovascular magnetic resonance imaging. Eur. Heart J. Cardiovasc. Imaging 2019, 20, 92–100. [Google Scholar] [CrossRef]
- Bourfiss, M.; Prakken, N.H.J.; van der Heijden, J.F.; Kamel, I.; Zimmerman, S.L.; Asselbergs, F.W.; Leiner, T.; Velthuis, B.K.; te Riele, A.S.J.M. Diagnostic Value of Native T1 Mapping in Arrhythmogenic Right Ventricular Cardiomyopathy. JACC Cardiovasc. Imaging 2019, 12, 1580–1582. [Google Scholar] [CrossRef] [PubMed]
- de Jong, S.; van Veen, T.A.B.; van Rijen, H.V.M.; de Bakker, J.M.T. Fibrosis and cardiac arrhythmias. J. Cardiovasc. Pharmacol. 2011, 57, 630–638. [Google Scholar] [CrossRef]
- de Jong, S.; van Veen, T.A.B.; de Bakker, J.M.T.; Vos, M.A.; van Rijen, H.V.M. Biomarkers of myocardial fibrosis. J. Cardiovasc. Pharmacol. 2011, 57, 522–535. [Google Scholar] [CrossRef] [PubMed]
- Sammani, A.; Jansen, M.; Linschoten, M.; Bagheri, A.; de Jonge, N.; Kirkels, H.; van Laake, L.W.; Vink, A.; van Tintelen, J.P.; Dooijes, D.; et al. UNRAVEL: Big data analytics research data platform to improve care of patients with cardiomyopathies using routine electronic health records and standardised biobanking. Neth. Heart J. 2019, 27, 426–434. [Google Scholar] [CrossRef] [PubMed]
- van der Voorn, S.M.; Bourfiss, M.; Te Riele, A.S.J.M.; Taha, K.; Vos, M.A.; de Brouwer, R.; Verstraelen, T.E.; de Boer, R.A.; Remme, C.A.; van Veen, T.A.B. Exploring the Correlation Between Fibrosis Biomarkers and Clinical Disease Severity in PLN p.Arg14del Patients. Front. Cardiovasc. Med. 2021, 8, 802–998. [Google Scholar] [CrossRef]
- Bosman, L.P.; Verstraelen, T.E.; van Lint, F.H.M.; Cox, M.G.P.J.; Groeneweg, J.A.; Mast, T.P.; van der Zwaag, P.A.; Volders, P.G.A.; Evertz, R.; Wong, L.; et al. Netherlands ACM Registry The Netherlands Arrhythmogenic Cardiomyopathy Registry: Design and status update. Neth. Heart J. 2019, 27, 480–486. [Google Scholar] [CrossRef]
- Martos, R.; Baugh, J.; Ledwidge, M.; O’Loughlin, C.; Conlon, C.; Patle, A.; Donnelly, S.C.; McDonald, K. Diastolic heart failure: Evidence of increased myocardial collagen turnover linked to diastolic dysfunction. Circulation 2007, 115, 888–895. [Google Scholar] [CrossRef]
- Querejeta, R.; López, B.; González, A.; Sánchez, E.; Larman, M.; Martínez Ubago, J.L.; Díez, J. Increased collagen type I synthesis in patients with heart failure of hypertensive origin: Relation to myocardial fibrosis. Circulation 2004, 110, 1263–1268. [Google Scholar] [CrossRef]
- Rojek, A.; Cielecka-Prynda, M.; Przewlocka-Kosmala, M.; Laczmanski, L.; Mysiak, A.; Kosmala, W. Impact of the PPARGC1A Gly482Ser polymorphism on left ventricular structural and functional abnormalities in patients with hypertension. J. Hum. Hypertens. 2014, 28, 557–563. [Google Scholar] [CrossRef]
- Roongsritong, C.; Bradley, J.; Sutthiwan, P.; Simoni, J.; Arif, A.; Meyerrose, G. Elevated carboxy-terminal peptide of procollagen type I in elderly patients with diastolic dysfunction. Am. J. Med. Sci. 2006, 331, 131–133. [Google Scholar] [CrossRef]
- Barasch, E.; Gottdiener, J.S.; Aurigemma, G.; Kitzman, D.W.; Han, J.; Kop, W.J.; Tracy, R.P. Association between elevated fibrosis markers and heart failure in the elderly: The cardiovascular health study. Circ. Heart Fail. 2009, 2, 303–310. [Google Scholar] [CrossRef]
- Schwartzkopff, B.; Fassbach, M.; Pelzer, B.; Brehm, M.; Strauer, B.E. Elevated serum markers of collagen degradation in patients with mild to moderate dilated cardiomyopathy. Eur. J. Heart Fail. 2002, 4, 439–444. [Google Scholar] [CrossRef]
- Lombardi, R.; Betocchi, S.; Losi, M.A.; Tocchetti, C.G.; Aversa, M.; Miranda, M.; D’Alessandro, G.; Cacace, A.; Ciampi, Q.; Chiariello, M. Myocardial collagen turnover in hypertrophic cardiomyopathy. Circulation 2003, 108, 1455–1460. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Qiao, S.; Song, Y.; Liu, Y.; Tang, Y.; Deng, L.; Yuan, J.; Hu, F.; Yang, W. Procollagen type I carboxy-terminal propeptide (PICP) and MMP-2 are potential biomarkers of myocardial fibrosis in patients with hypertrophic cardiomyopathy. Cardiovasc. Pathol. 2019, 43, 107150. [Google Scholar] [CrossRef] [PubMed]
- López, B.; Querejeta, R.; González, A.; Sánchez, E.; Larman, M.; Díez, J. Effects of loop diuretics on myocardial fibrosis and collagen type I turnover in chronic heart failure. J. Am. Coll. Cardiol. 2004, 43, 2028–2035. [Google Scholar] [CrossRef] [PubMed]
- Raafs, A.G.; Verdonschot, J.A.J.; Henkens, M.T.H.M.; Adriaans, B.P.; Wang, P.; Derks, K.; Abdul Hamid, M.A.; Knackstedt, C.; van Empel, V.P.M.; Díez, J.; et al. The combination of carboxy-terminal propeptide of procollagen type I blood levels and late gadolinium enhancement at cardiac magnetic resonance provides additional prognostic information in idiopathic dilated cardiomyopathy—A multilevel assessment of myocardial fibrosis in dilated cardiomyopathy. Eur. J. Heart Fail. 2021, 23, 933–944. [Google Scholar] [CrossRef]
- González, A.; López, B.; Querejeta, R.; Zubillaga, E.; Echeverría, T.; Díez, J. Filling pressures and collagen metabolism in hypertensive patients with heart failure and normal ejection fraction. Hypertension 2010, 55, 1418–1424. [Google Scholar] [CrossRef] [PubMed]

| All ACM (n = 45) | Preclinical Variant Carriers (n = 10) | Affected Patients (n = 35) | Adjusted p-Value | |
|---|---|---|---|---|
| Demographics | ||||
| Age (years) | 50.11 15.53 | 51 17.41 | 49.86 15.22 | >0.999 |
| Female | 20/45 (44) | 4/10 (40) | 16/35 (46) | >0.999 |
| Proband Status | 31/43 (72) | 3/10 (30) | 28/33 (85) | 0.011 * |
| TFC Score | 4 (4–7) | 2 (2–2.75) | 7 (6–8) | <0.003 ** |
| Genetic variant | ||||
| PKP2 | 26/48 (54) | 5/10 (50) | 21/38 (55) | >0.999 |
| DSP | 6/48 (13) | 1/10 (1) | 5/38 (13) | >0.999 |
| JUP | 2/48 (4) | 2/10 (20) | 0/38 (0) | >0.999 |
| DSG2 | 4/48 (8) | 0/10 (0) | 4/38 (11) | >0.999 |
| DSC2 | 2/48 (4) | 0/10 (0) | 2/38 (5) | >0.999 |
| No Variant Detected | 8/48 (17) | 2/10 (20) | 6/38 (16) | >0.999 |
| Medication | ||||
| Betablockers | 17/39 (44) | 2/7 (29) | 15/32 (47) | >0.999 |
| Antiarrhythmics | 19/38 (50) | 2/6 (33) | 17/32 (53) | >0.999 |
| ACE-inhibitors | 5/38 (13) | 0/6 (0) | 5/32 (16) | >0.999 |
| Diuretics | 6/38 (16) | 0/6 (0) | 6/32 (19) | >0.999 |
| Imaging/CMR | ||||
| LGE RV | 7/17 (41) | 0/4 (0) | 7/13 (54) | >0.999 |
| RVEF (%) | 44.23 11.54 | 56.21 4.43 | 40.96 10.55 | 0.351 |
| RV EDVi (mL/m2) | 95.35 24.36 | 78.42 11.52 | 101.50 25.19 | >0.999 |
| RV ESVi (mL/m2) | 50.50 23.92 | 30.12 16.40 | 59.56 21.39 | 0.899 |
| LGE LV | 6/16 (38) | 2/3 (67) | 4/13 (31) | >0.999 |
| LVEF (%) | 57.44 9.44 | 59.37 5.19 | 56.69 10.73 | >0.999 |
| LV EDVi (mL/m2) | 77.55 15.70 | 78.18 9.23 | 77.30 18.10 | >0.999 |
| LV ESVi (mL/m2) | 34.25 15.21 | 31.83 5.85 | 35.33 18.16 | >0.999 |
| Echocardiogram | ||||
| RV Dilatation | 25/32 (78) | 2/5 (40) | 23/27 (85) | 0.662 |
| ECG parameters | ||||
| QRS duration (ms) | 99.54 16.53 | 100 11.1 | 99.45 17.53 | >0.999 |
| T Wave Inversion | 34/37 (92) | 5/6 (83) | 29/31 (94) | >0.999 |
| TAD 55 ms | 7/34 (21) | 0/5 (0) | 7/29 (24) | >0.999 |
| BBB | 5/37 (14) | 1/6 (17) | 4/31 (13) | >0.999 |
| All ACM (n = 45) | Preclinical Variant Carriers (n = 10) | Affected Patients (n = 35) | p-Value | |
|---|---|---|---|---|
| PICP (ng/mL) | 165.18 61.43 | 129.47 35.11 | 175.38 63.84 | 0.036 * |
| ICTP (ng/mL) | 4.02 1.46 | 4.02 0.71 | 4.02 1.62 | 0.991 |
| PICP/ICTP | 43.84 17.91 | 32.89 10.79 | 46.97 18.40 | 0.027 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van der Voorn, S.M.; Bourfiss, M.; Muller, S.A.; Çimen, T.; Saguner, A.M.; Duru, F.; te Riele, A.S.J.M.; Remme, C.A.; van Veen, T.A.B. Circulating Biomarkers of Fibrosis Formation in Patients with Arrhythmogenic Cardiomyopathy. Biomedicines 2023, 11, 813. https://doi.org/10.3390/biomedicines11030813
van der Voorn SM, Bourfiss M, Muller SA, Çimen T, Saguner AM, Duru F, te Riele ASJM, Remme CA, van Veen TAB. Circulating Biomarkers of Fibrosis Formation in Patients with Arrhythmogenic Cardiomyopathy. Biomedicines. 2023; 11(3):813. https://doi.org/10.3390/biomedicines11030813
Chicago/Turabian Stylevan der Voorn, Stephanie M., Mimount Bourfiss, Steven A. Muller, Tolga Çimen, Ardan M. Saguner, Firat Duru, Anneline S. J. M. te Riele, Carol Ann Remme, and Toon A. B. van Veen. 2023. "Circulating Biomarkers of Fibrosis Formation in Patients with Arrhythmogenic Cardiomyopathy" Biomedicines 11, no. 3: 813. https://doi.org/10.3390/biomedicines11030813
APA Stylevan der Voorn, S. M., Bourfiss, M., Muller, S. A., Çimen, T., Saguner, A. M., Duru, F., te Riele, A. S. J. M., Remme, C. A., & van Veen, T. A. B. (2023). Circulating Biomarkers of Fibrosis Formation in Patients with Arrhythmogenic Cardiomyopathy. Biomedicines, 11(3), 813. https://doi.org/10.3390/biomedicines11030813





