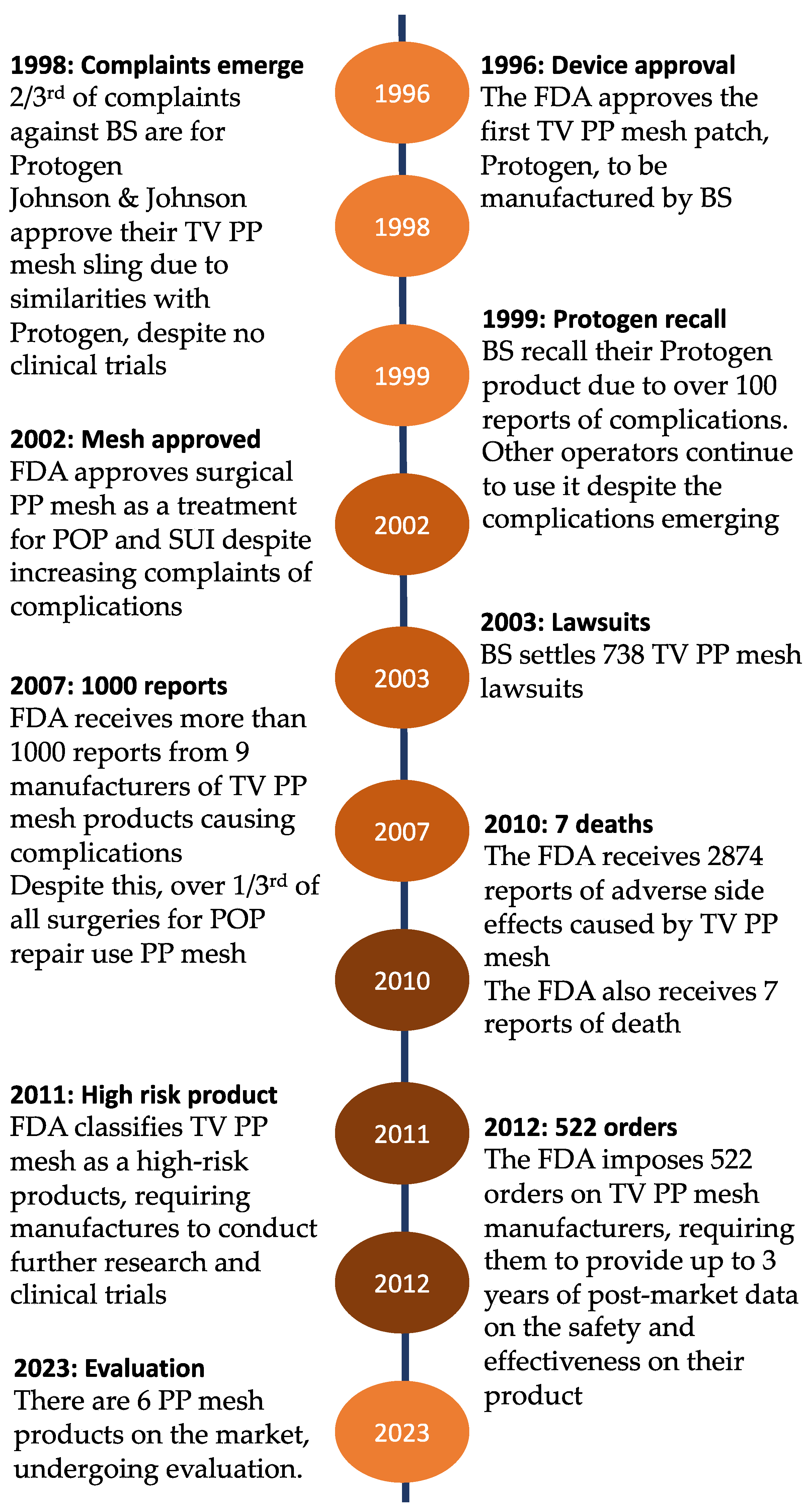
Polypropylene Pelvic Mesh: What Went Wrong and What Will Be of the Future?
Abstract
1. Introduction
2. Pelvic Organ Prolapse
3. Material of the Mesh Implants: Synthetic or Biological?
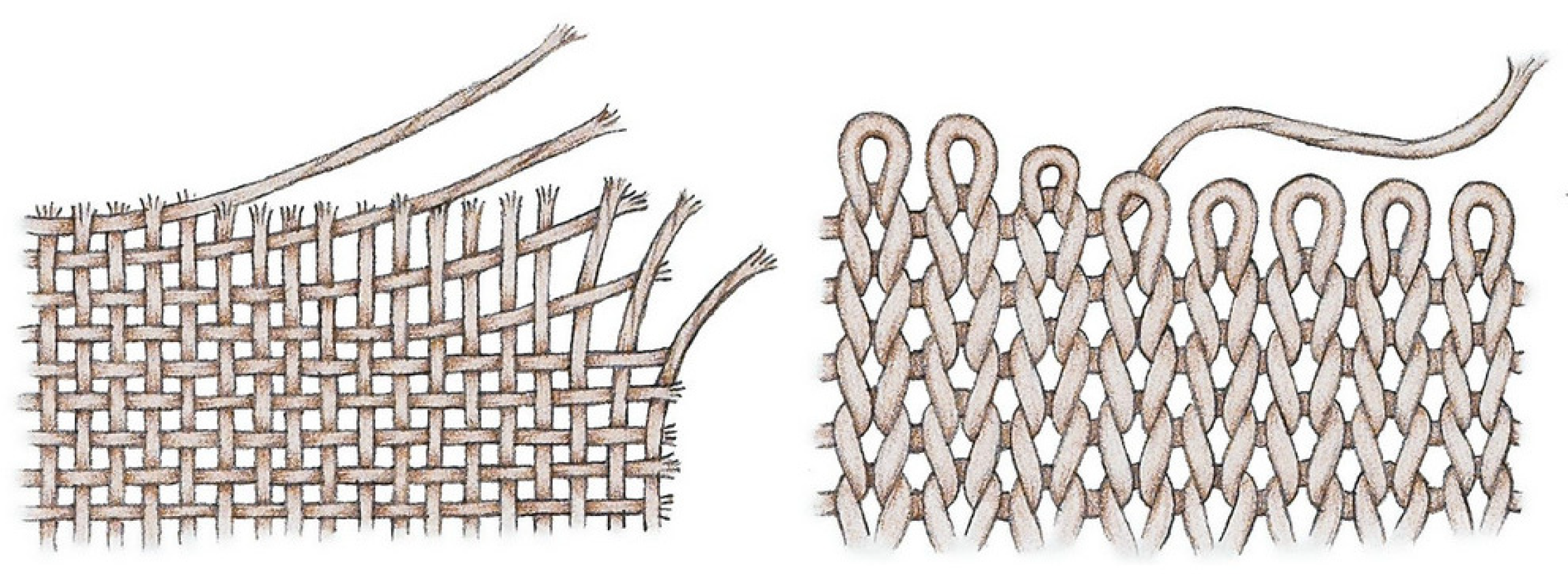
4. Polypropylene and Its Properties Used as Mesh for Treatment of Pelvic Organ Prolapse
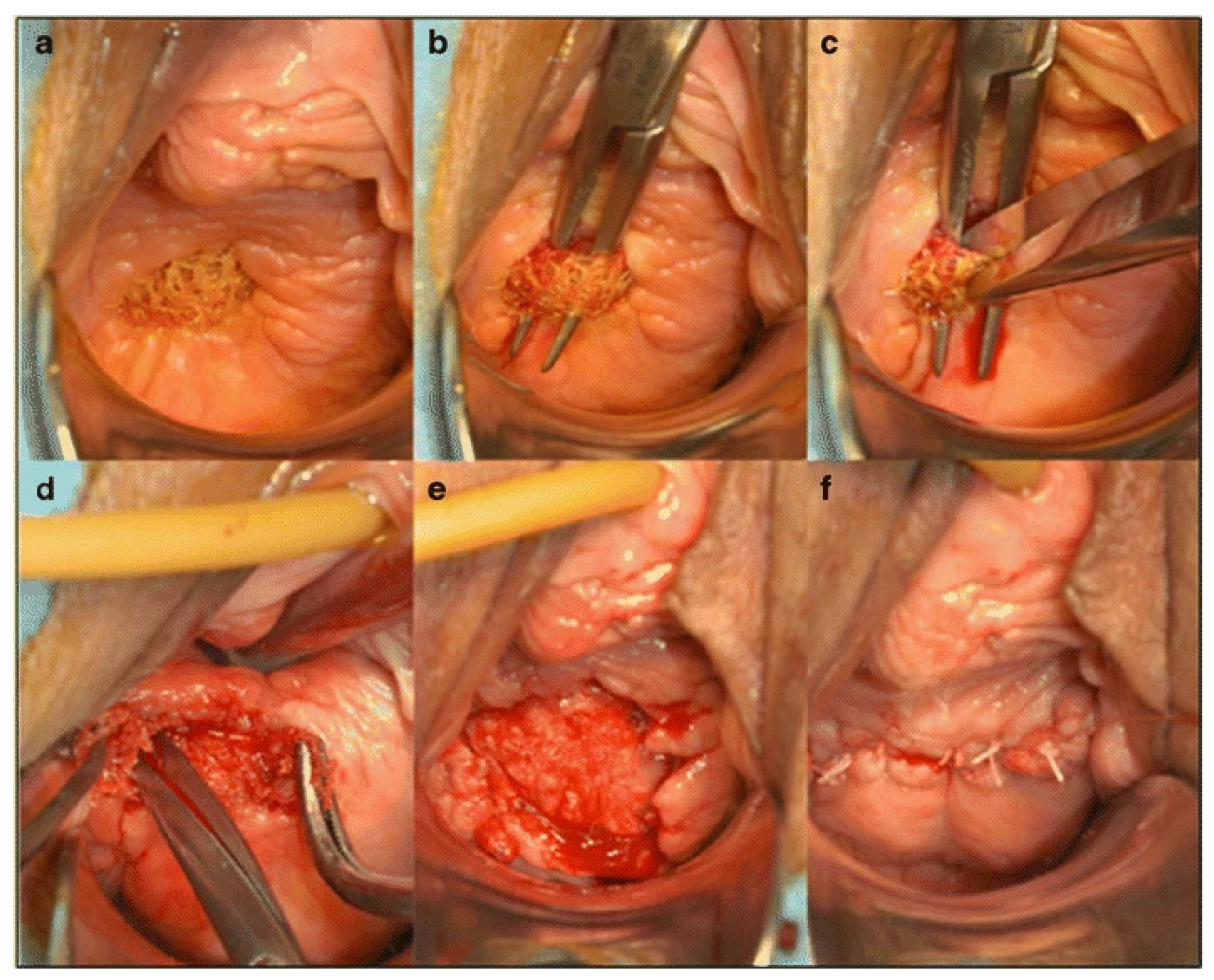
5. Clinical Complications Arising from the Polypropylene Mesh Material
- Chronic infection
- Chronic pain
- Dyspareunia
- Mesh exposure—display of mesh at or near the site of insertion
- Mesh extrusion—where the mesh passes out of a body structure
- Perforation of neighbouring organs secondary to erosion
- Mesh shrinkage
- Recurrence of prolapse with treatment failure and further surgery
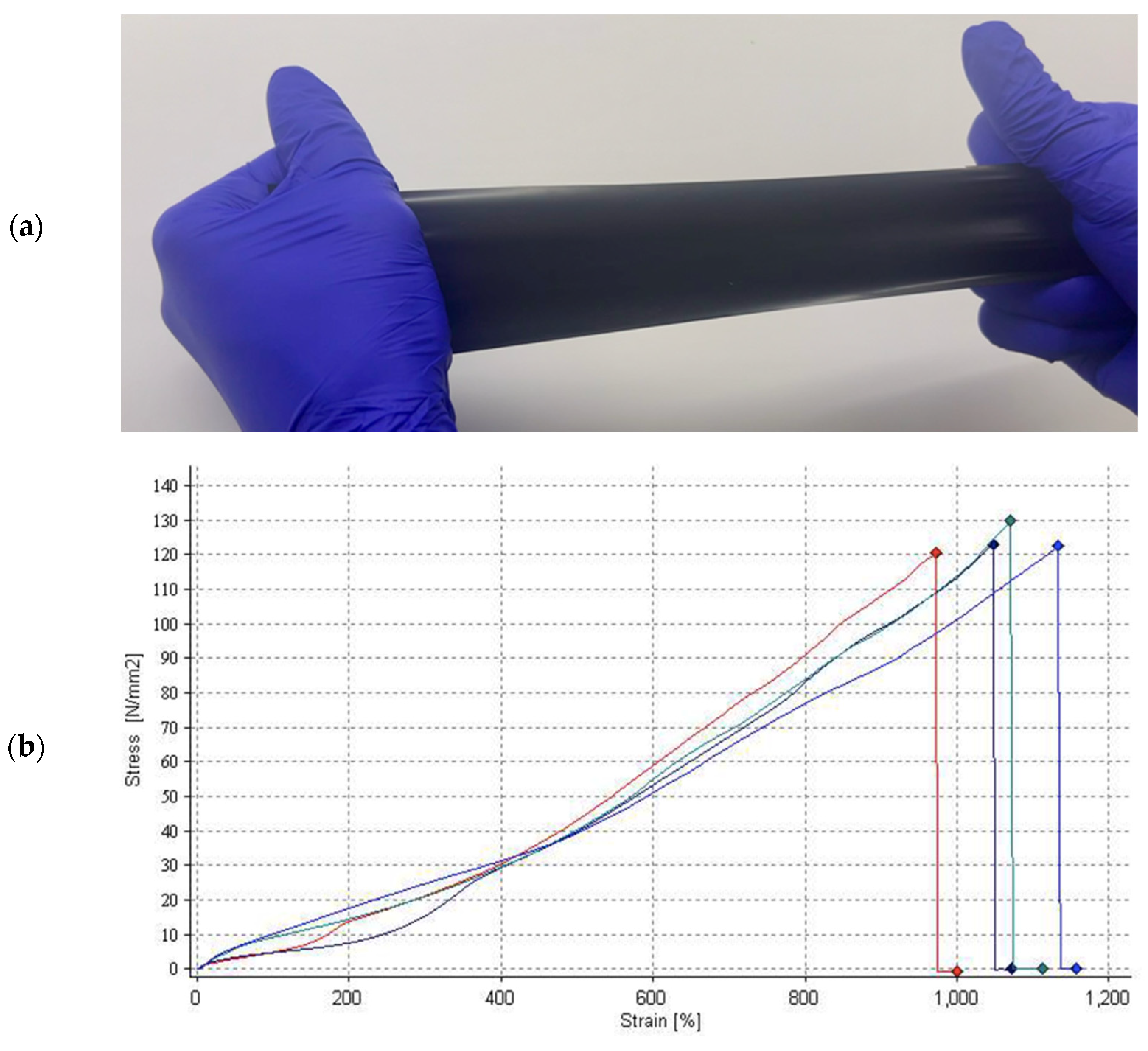
6. Future Direction
- Nontoxic and biocompatible
- Chemically inert
- Lightweight with low density
- Low stiffness
- Large pores and high porosity
- Mechanically strong
- Nondegenerative
- Noncarcinogenic
- Noninflammatory and nonallergenic
- Affordable
- Sterile
- Resistant to mesh shrinkage
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dyer, O. Transvaginal mesh: FDA orders remaining products off US market. BMJ 2019, 365, l1839. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, N.Y.; Edenfield, A.L. Clinical challenges in the management of vaginal prolapse. Int. J. Women’s Health 2014, 6, 83–94. [Google Scholar] [CrossRef] [PubMed]
- Jelovsek, J.E.; Maher, C.; Barber, M.D. Pelvic organ prolapse. Lancet 2007, 369, 1027–1038. [Google Scholar] [CrossRef] [PubMed]
- Barber, M.D. Pelvic organ prolapse. BMJ 2016, 354, i3853. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence. Urinary Incontinence and Pelvic Organ Prolapse in Women: Management; NICE Guide; National Institute for Health and Care Excellence: London, UK, 2019. [Google Scholar]
- House of Commons. Surgical Mesh Implants; House of Commons: London, UK, 2018. [Google Scholar]
- Maher, C. There is still a place for vaginal mesh in urogynaecology: FOR: There Is Still a Place for Vaginal Mesh in Urogynaecology. BJOG Int. J. Obstet. Gynaecol. 2019, 126, 1074. [Google Scholar] [CrossRef]
- Morling, J.; McAllister, D.; Agur, W.; Fischbacher, C.; A Glazener, C.M.; Guerrero, K.; Hopkins, L.; Wood, R. Adverse events after first, single, mesh and non-mesh surgical procedures for stress urinary incontinence and pelvic organ prolapse in Scotland, 1997–2016: A population-based cohort study. Lancet 2016, 389, 629–640. [Google Scholar] [CrossRef]
- Schimpf, M.O.; Abed, H.; Sanses, T.; White, A.B.; Lowenstein, L.; Ward, R.M.; Sung, V.W.; Balk, E.M.; Murphy, M. Graft and Mesh Use in Transvaginal Prolapse Repair: A Systematic Review. Obstet. Gynecol. Surv. 2016, 128, 81–91. [Google Scholar] [CrossRef]
- Cox, A.; Herschorn, S. Evaluation of Current Biologic Meshes in Pelvic Organ Prolapse Repair. Curr. Urol. Rep. 2012, 13, 247–255. [Google Scholar] [CrossRef]
- Campbell, P.; Jha, S.; Cutner, A. Vaginal mesh in prolapse surgery. Obstet. Gynaecol. 2018, 20, 49–56. [Google Scholar] [CrossRef]
- Jeon, M.J.; Bai, S.W. Use of Grafts in Pelvic Reconstructive Surgery. Yonsei Med. J. 2007, 48, 147–156. [Google Scholar] [CrossRef]
- Kalkan, U.; Yoldemir, T.; Ozyurek, E.S.; Daniilidis, A. Native tissue repair versus mesh repair in pelvic organ prolapse surgery. Climacteric 2017, 20, 510–517. [Google Scholar] [CrossRef] [PubMed]
- Birch, C.; Fynes, M.M. The role of synthetic and biological prostheses in reconstructive pelvic floor surgery. Curr. Opin. Obstet. Gynecol. 2002, 14, 527–535. [Google Scholar] [CrossRef] [PubMed]
- Gigliobianco, G.; Regueros, S.R.; Osman, N.I.; Bissoli, J.; Bullock, A.J.; Chapple, C.R.; MacNeil, S. Biomaterials for Pelvic Floor Reconstructive Surgery: How Can We Do Better? BioMed Res. Int. 2015, 2015, 968087. [Google Scholar] [CrossRef] [PubMed]
- Glazener, C.M.; Breeman, S.; Elders, A.; Hemming, C.; Cooper, K.G.; Freeman, R.M.; Smith, A.R.; Reid, F.; Hagen, S.; Montgomery, I.; et al. Mesh, graft, or standard repair for women having primary transvaginal anterior or posterior compartment prolapse surgery: Two parallel-group, multicentre, randomised, controlled trials (PROSPECT). Lancet 2017, 389, 381–392. [Google Scholar] [CrossRef] [PubMed]
- Clavé, A.; Yahi, H.; Hammou, J.-C.; Montanari, S.; Gounon, P.; Clavé, H. Polypropylene as a reinforcement in pelvic surgery is not inert: Comparative analysis of 100 explants. Int. Urogynecol. J. 2010, 21, 261–270. [Google Scholar] [CrossRef]
- De Tayrac, R.; Sentilhes, L. Complications of pelvic organ prolapse surgery and methods of prevention. Int. Urogynecol. J. 2013, 24, 1859–1872. [Google Scholar] [CrossRef] [PubMed]
- Mancuso, E.; Downey, C.; Doxford-Hook, E.; Bryant, M.G.; Culmer, P. The use of polymeric meshes for pelvic organ prolapse: Current concepts, challenges, and future perspectives. J. Biomed. Mater. Res. Part B Appl. Biomater. 2020, 108, 771–789. [Google Scholar] [CrossRef]
- Vijaya, G.; Digesu, G.; Khullar, V. Is There a Role for Synthetic Meshes or Biological Grafts in Vaginal Prolapse Surgery? Women’s Health 2010, 6, 631–633. [Google Scholar] [CrossRef]
- Mangera, A.; Bullock, A.J.; Chapple, C.R.; MacNeil, S. Are biomechanical properties predictive of the success of prostheses used in stress urinary incontinence and pelvic organ prolapse? A systematic review. Neurourol. Urodyn. 2011, 31, 13–21. [Google Scholar] [CrossRef]
- Roman, S.; Mangir, N.; MacNeil, S. Designing new synthetic materials for use in the pelvic floor: What Is the Problem with the Existing Polypropylene Materials? Curr. Opin. Urol. 2019, 29, 407–413. [Google Scholar] [CrossRef]
- Feola, A.; Abramowitch, S.; Jallah, Z.; Stein, S.; Barone, W.; Palcsey, S.; Moalli, P. Deterioration in biomechanical properties of the vagina following implantation of a high-stiffness prolapse mesh. BJOG Int. J. Obstet. Gynaecol. 2013, 120, 224–232. [Google Scholar] [CrossRef] [PubMed]
- Liang, R.; Abramowitch, S.; Knight, K.; Palcsey, S.; Nolfi, A.; Feola, A.; Stein, S.; Moalli, P. Vaginal degeneration following implantation of synthetic mesh with increased stiffness. BJOG Int. J. Obstet. Gynaecol. 2012, 120, 233–243. [Google Scholar] [CrossRef] [PubMed]
- Feola, A.; Barone, W.; Moalli, P.; Abramowitch, S. Characterizing the ex vivo textile and structural properties of synthetic prolapse mesh products. Int. Urogynecol. J. 2013, 24, 559–564. [Google Scholar] [CrossRef] [PubMed]
- Kelly, M.; MacDougall, K.; Olabisi, O.; McGuire, N. In vivo response to polypropylene following implantation in animal models: A review of biocompatibility. Int. Urogynecol. J. 2017, 28, 171–180. [Google Scholar] [CrossRef] [PubMed]
- Veit-Rubin, N.; Tayrac, R.; Cartwright, R.; Franklin-Revill, L.; Warembourg, S.; Dunyach-Remy, C.; Lavigne, J.; Khullar, V. Abnormal vaginal microbiome associated with vaginal mesh complications. Neurourol. Urodyn. 2019, 38, 2255–2263. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Cheng, T. Mesh erosion after hiatal hernia repair: The tip of the iceberg? Hernia 2019, 23, 1243–1252. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence. Transvaginal Mesh Repair of Anterior or Posterior Vaginal Wall Prolapse. Available online: https://www.nice.org.uk/guidance/ipg599/chapter/5-Safety (accessed on 4 September 2019).
- Zambon, J.P.; Badlani, G.H. Vaginal Mesh Exposure Presentation, Evaluation, and Management. Curr. Urol. Rep. 2016, 17, 65. [Google Scholar] [CrossRef]
- Nieminen, K.; Hiltunen, R.; Heiskanen, E.; Takala, T.; Niemi, K.; Merikari, M.; Heinonen, P.K. Symptom resolution and sexual function after anterior vaginal wall repair with or without polypropylene mesh. Int. Urogynecol. J. 2008, 19, 1611–1616. [Google Scholar] [CrossRef]
- Culligan, P.J.; Salamon, C.; Priestley, J.; Shariati, A. Porcine Dermis Compared with Polypropylene Mesh for Laparoscopic Sacrocolpopexy: A Randomized Controlled Trial. Obstet. Gynecol. 2013, 121, 143–151. [Google Scholar] [CrossRef]
- Menefee, S.A.; Dyer, K.Y.; Lukacz, E.S.; Simsiman, A.J.; Luber, K.M.; Nguyen, J.N. Colporrhaphy Compared with Mesh or Graft-Reinforced Vaginal Paravaginal Repair for Anterior Vaginal Wall Prolapse: A Randomized Controlled Trial. Obstet. Gynecol. 2011, 118, 1337–1344. [Google Scholar] [CrossRef]
- Allègre, L.; Callewaert, G.; Alonso, S.; Cornille, A.; Fernandez, H.; Eglin, G.; de Tayrac, R. Long-term outcomes of a randomized controlled trial comparing trans-obturator vaginal mesh with native tissue repair in the treatment of anterior vaginal wall prolapse. Int. Urogynecol. J. 2020, 31, 745–753. [Google Scholar] [CrossRef]
- Altman, D.; Falconer, C. Perioperative Morbidity Using Transvaginal Mesh in Pelvic Organ Prolapse Repair. Obstet. Gynecol. 2007, 109, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Palma, P.; Riccetto, C.; Prudente, A.; Dalphorno, F.; Delroy, C.; Castro, R.; Tcherniakovsky, M.; Salvador, M.; Bartos, P.; Paladini, M.; et al. Monoprosthesis for anterior vaginal prolapse and stress urinary incontinence: Midterm results of an international multicentre prospective study. Int. Urogynecol. J. 2011, 22, 1535–1541. [Google Scholar] [CrossRef] [PubMed]
- Keltie, K.; Elneil, S.; Monga, A.; Patrick, H.; Powell, J.; Campbell, B.; Sims, A.J. Complications following vaginal mesh procedures for stress urinary incontinence: An 8 year study of 92,246 women. Sci. Rep. 2017, 7, 12015. [Google Scholar] [CrossRef]
- Gutman, R.E.; Nosti, P.A.; Sokol, A.I.; Sokol, E.R.; Peterson, J.L.; Wang, H.; Iglesia, C.B. Three-Year Outcomes of Vaginal Mesh for Prolapse: A Randomized Controlled Trial. Obstet. Gynecol. 2013, 122, 770–777. [Google Scholar] [CrossRef] [PubMed]
- Milani, A.L.; Hinoul, P.; Gauld, J.M.; Sikirica, V.; van Drie, D.; Cosson, M. Trocar-guided mesh repair of vaginal prolapse using partially absorbable mesh: 1 year outcomes. Am. J. Obstet. Gynecol. 2011, 204, 74.e1–74.e8. [Google Scholar] [CrossRef] [PubMed]
- Scheiner, D.A.; Betschart, C.; Wiederkehr, S.; Seifert, B.; Fink, D.; Perucchini, D. Twelve months effect on voiding function of retropubic compared with outside-in and inside-out transobturator midurethral slings. Int. Urogynecol. J. 2011, 23, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Rudnicki, M.; Laurikainen, E.; Pogosean, R.; Kinne, I.; Jakobsson, U.; Teleman, P. A 3-year follow-up after anterior colporrhaphy compared with collagen-coated transvaginal mesh for anterior vaginal wall prolapse: A randomised controlled trial. BJOG Int. J. Obstet. Gynaecol. 2016, 123, 136–142. [Google Scholar] [CrossRef]
- Culligan, P.J.; Gurshumov, E.; Lewis, C.; Priestley, J.; Komar, J.; Shah, N.; Salamon, C.G. Subjective and objective results 1 year after robotic sacrocolpopexy using a lightweight Y-mesh. Int. Urogynecol. J. 2014, 25, 731–735. [Google Scholar] [CrossRef]
- Costantini, E.; Mearini, L.; Bini, V.; Zucchi, A.; Mearini, E.; Porena, M. Uterus Preservation in Surgical Correction of Urogenital Prolapse. Eur. Urol. 2005, 48, 642–649. [Google Scholar] [CrossRef]
- Wei, A.-M.; Fan, Y.; Zhang, L.; Shen, Y.-F.; Kou, Q.; Tan, X.-M. Evaluation of Clinical Outcome and Risk Factors for Recurrence after Pelvic Reconstruction of Pelvic Organ Prolapse with Implanted Mesh or Biological Grafts: A Single-Blind Randomized Trial. Gynecol. Obstet. Investig. 2019, 84, 503–511. [Google Scholar] [CrossRef] [PubMed]
- Okulu, E.; Kayıgil, O.; Aldemir, M.; Onen, E. Use of three types of synthetic mesh material in sling surgery: A prospective randomized clinical trial evaluating effectiveness and complications. Scand. J. Urol. 2013, 47, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Alexandridis, V.; Rudnicki, M.; Jakobsson, U.; Teleman, P. Adjustable mini-sling compared with conventional mid-urethral slings in women with urinary incontinence: A 3-year follow-up of a randomized controlled trial. Int. Urogynecol. J. 2019, 30, 1465–1473. [Google Scholar] [CrossRef] [PubMed]
- Skorupska, K.A.; Futyma, K.; Bogusiewicz, M.; Rechberger, E.; Ziętek-Strobl, A.; Miotła, P.; Wróbel, A.; Rechberger, T. Four-arm polypropylene mesh for vaginal vault prolapse-surgical technique and outcomes. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 255, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Matthews, C.A.; Geller, E.J.; Henley, B.R.; Kenton, K.; Myers, E.M.; Dieter, A.A.; Parnell, B.; Lewicky-Gaupp, C.; Mueller, M.G.; Wu, J.M. Permanent Compared with Absorbable Suture for Vaginal Mesh Fixation During Total Hysterectomy and Sacrocolpopexy: A Randomized Controlled Trial. Obstet. Gynecol. 2020, 136, 355–364. [Google Scholar] [CrossRef]
- Senturk, M.B.; Guraslan, H.; Cakmak, Y.; Ekin, M. Bilateral sacrospinous fixation without hysterectomy: 18-month follow-up. J. Turk. Gynecol. Assoc. 2015, 16, 102–106. [Google Scholar] [CrossRef]
- Cadenbach-Blome, T.; Grebe, M.; Mengel, M.; Pauli, F.; Greser, A.; Fünfgeld, C. Significant Improvement in Quality of Life, Positive Effect on Sexuality, Lasting Reconstructive Result and Low Rate of Complications Following Cystocele Correction Using a Lightweight, Large-Pore, Titanised Polypropylene Mesh: Final Results of a National. Geburtshilfe Frauenheilkd. 2019, 79, 959–968. [Google Scholar] [CrossRef]
- Illiano, E.; Ditonno, P.; Giannitsas, K.; de Rienzo, G.; Bini, V.; Costantini, E. Robot-assisted vs. Laparoscopic Sacrocolpopexy for High-stage Pelvic Organ Prolapse: A Prospective, Randomized, Single-center Study. Urology 2019, 134, 116–123. [Google Scholar] [CrossRef]
- Marcus-Braun, N.; von Theobald, P. Mesh removal following transvaginal mesh placement: A case series of 104 operations. Int. Urogynecol. J. 2010, 21, 423–430. [Google Scholar] [CrossRef]
- Hympanova, L.; da Cunha, M.G.M.C.M.; Rynkevic, R.; Wach, R.A.; Olejnik, A.K.; Dankers, P.Y.; Arts, B.; Mes, T.; Bosman, A.W.; Albersen, M.; et al. Experimental reconstruction of an abdominal wall defect with electrospun polycaprolactone-ureidopyrimidinone mesh conserves compliance yet may have insufficient strength. J. Mech. Behav. Biomed. Mater. 2018, 88, 431–441. [Google Scholar] [CrossRef]
- Eisenakh, I.A.; Bondarev, O.I.; Mozes, V.G.; Lapii, G.A.; Lushnikova, E.L. Features of in Vitro Degradation and Physical Properties of a Biopolymer and in Vivo Tissue Reactions in Comparison with Polypropylene. Bull. Exp. Biol. Med. 2020, 170, 88–92. [Google Scholar] [CrossRef] [PubMed]
- Hympanova, L.; da Cunha, M.G.M.C.M.; Rynkevic, R.; Zündel, M.; Gallego, M.R.; Vange, J.; Callewaert, G.; Urbankova, I.; Van der Aa, F.; Mazza, E.; et al. Physiologic musculofascial compliance following reinforcement with electrospun polycaprolactone-ureidopyrimidinone mesh in a rat model. J. Mech. Behav. Biomed. Mater. 2017, 74, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Fu, S.; Zhou, S.; Chen, G.; Zhu, C.; Li, N.; Ma, Y. Preparation and biocompatibility evaluation of polypropylene mesh coated with electrospinning membrane for pelvic defects repair. J. Mech. Behav. Biomed. Mater. 2018, 81, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, S.; Darzi, S.; Rosamilia, A.; Kadam, V.; Truong, Y.; Werkmeister, J.A.; Gargett, C.E. Blended Nanostructured Degradable Mesh with Endometrial Mesenchymal Stem Cells Promotes Tissue Integration and Anti-Inflammatory Response in Vivo for Pelvic Floor Application. Biomacromolecules 2019, 20, 454–468. [Google Scholar] [CrossRef]
- Paul, K.; Darzi, S.; McPhee, G.; Del Borgo, M.P.; Werkmeister, J.A.; Gargett, C.E.; Mukherjee, S. 3D bioprinted endometrial stem cells on melt electrospun poly ε-caprolactone mesh for pelvic floor application promote anti-inflammatory responses in mice. Acta Biomater. 2019, 97, 162–176. [Google Scholar] [CrossRef] [PubMed]
- Hansen, S.G.; Taskin, M.B.; Chen, M.; Wogensen, L.; Nygaard, J.V.; Axelsen, S.M. Electrospun nanofiber mesh with fibroblast growth factor and stem cells for pelvic floor repair. J. Biomed. Mater. Res. Part B Appl. Biomater. 2020, 108, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Glindtvad, C.; Chen, M.; Nygaard, J.V.; Wogensen, L.; Forman, A.; Danielsen, C.C.; Taskin, M.B.; Andersson, K.-E.; Axelsen, S.M. Electrospun biodegradable microfibers induce new collagen formation in a rat abdominal wall defect model: A possible treatment for pelvic floor repair? J. Biomed. Mater. Res. Part B Appl. Biomater. 2018, 106, 680–688. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Dong, S.; Zhang, P.; Liu, X.; Wang, X. Preparation of a polylactic acid knitting mesh for pelvic floor repair and in vivo evaluation. J. Mech. Behav. Biomed. Mater. 2017, 74, 204–213. [Google Scholar] [CrossRef]
- Emmerson, S.; Mukherjee, S.; Melendez-Munoz, J.; Cousins, F.; Edwards, S.; Karjalainen, P.; Ng, M.; Tan, K.; Darzi, S.; Bhakoo, K.; et al. Composite mesh design for delivery of autologous mesenchymal stem cells influences mesh integration, exposure and biocompatibility in an ovine model of pelvic organ prolapse. Biomaterials 2019, 225, 119495. [Google Scholar] [CrossRef]
- Hympánová, L.; Rynkevic, R.; Román, S.; da Cunha, M.G.M.; Mazza, E.; Zündel, M.; Urbánková, I.; Gallego, M.R.; Vange, J.; Callewaert, G.; et al. Assessment of Electrospun and Ultra-lightweight Polypropylene Meshes in the Sheep Model for Vaginal Surgery. Eur. Urol. Focus 2020, 6, 190–198. [Google Scholar] [CrossRef]
- da Cunha, M.G.M.M.; Arts, B.; Hympanova, L.; Rynkevic, R.; Mackova, K.; Bosman, A.W.; Dankers, P.Y.; Deprest, J. Functional supramolecular bioactivated electrospun mesh improves tissue ingrowth in experimental abdominal wall reconstruction in rats. Acta Biomater. 2020, 106, 82–91. [Google Scholar] [CrossRef] [PubMed]
- Bickhaus, J.A.; Fraser, M.O.; Weidner, A.C.; Jayes, F.L.; Amundsen, C.L.; Gall, K.; Miller, A.T.; Marini, F.C.; Robboy, S.J.; Siddiqui, N.Y. Polycarbonate Urethane Mesh: A New Material for Pelvic Reconstruction. Urogynecology 2021, 27, e469–e475. [Google Scholar] [CrossRef] [PubMed]
- Iva, U.; Nikhil, S.; Geertje, C.; Alice, T.; Rynkevic, R.; Lucie, H.; Andrew, F.; Jan, D. In vivo documentation of shape and position changes of MRI-visible mesh placed in rectovaginal septum. J. Mech. Behav. Biomed. Mater. 2017, 75, 379–389. [Google Scholar] [CrossRef] [PubMed]
- Jansen, A.K.; Ludwig, S.; Malter, W.; Sauerwald, A.; Hachenberg, J.; Pahmeyer, C.; Wegmann, K.; Rudroff, C.; Karapanos, L.; Radosa, J.; et al. Tacks vs. sutures: A biomechanical analysis of sacral bony fixation methods for laparoscopic apical fixations in the porcine model. Arch. Gynecol. Obstet. 2022, 305, 631–639. [Google Scholar] [CrossRef]
- Knight, K.M.; King, G.E.; Palcsey, S.L.; Artsen, A.M.; Abramowitch, S.D.; Moalli, P.A. A soft elastomer alternative to polypropylene for pelvic organ prolapse repair: A preliminary study. Int. Urogynecol. J. 2021, 33, 327–335. [Google Scholar] [CrossRef]
- Seifalian, A.M.; Hancock, S. Composite Material and Its Method of Production. Patent GB GB1811090, 22 August 2018. [Google Scholar]
- Nezakati, T.; Seifalian, A.; Tan, A.; Seifalian, A.M. Conductive Polymers: Opportunities and Challenges in Biomedical Applications. Chem. Rev. 2018, 118, 6766–6843. [Google Scholar] [CrossRef]
- Nezakati, T. Development of a Graphene-POSS-Nanocomposite Conductive Material for Biomedical Application. Ph.D. Thesis, University College London, London, UK, 2016. [Google Scholar]
- Ovcharenko, E.A.; Seifalian, A.; Rezvova, M.A.; Klyshnikov, K.Y.; Glushkova, T.V.; Akenteva, T.N.; Antonova, L.V.; Velikanova, E.A.; Chernonosova, V.S.; Shevelev, G.Y.; et al. A New Nanocomposite Copolymer Based on Functionalised Graphene Oxide for Development of Heart Valves. Sci. Rep. 2020, 10, 5271. [Google Scholar] [CrossRef]
- Aleemardani, M.; Bagher, Z.; Farhadi, M.; Chahsetareh, H.; Najafi, R.; Eftekhari, B.; Seifalian, A.M. Can Tissue Engineering Bring Hope to the Development of Human Tympanic Membrane? Tissue Eng. Part B Rev. 2020, 27, 572–589. [Google Scholar] [CrossRef]

| Type | Sub-Type | Material | Advantages | Disadvantages |
|---|---|---|---|---|
| Biologic | Autologous | Rectus sheath |
|
|
| Fascia lata | ||||
| Allografts | Cadaveric fascia lata |
|
| |
| Cadaveric human dermis | ||||
| Xenografts | Porcine dermis | |||
| Porcine small intestinal submucosa | ||||
| Bovine pericardium | ||||
| Synthetic | Polypropylene | Heavyweight polypropylene |
|
|
| Lightweight polypropylene | ||||
| Polyethylene terephthalate | Polyester mesh known as Mersilene® |
|
| |
| Expanded—Polytetrafluoroethylene | Soft tissue patch Gore-Tex® |
|
|
| Mechanical Properties | Chemical Properties |
|---|---|
| Low density (0.9 g/cm3) Lighter than water Floats | Great chemical resistance Resistant to most organic solvents at room temperature |
| Tough Acts with elasticity over a range of deflection to prevent deformation | Highly resistant to dilute or concentrated acids, alcohols, and bases |
| Flexible Semi-crystalline nature gives it a high flexural strength | Highly impermeable to water |
| High resistance to fatigue Able to retain shape after a large degree of torsion and bending | High electrical resistance |
| High tensile strength Around 4800 psi Able to withstand heavy loads despite being lightweight | Thermoplastic Becomes liquid at the melting point Can be melted, cooled, and reheated again without degradation |
| High impact tolerance | |
| Hard consistency Semi-rigid structure makes it more likely to bend and flex with impact |
| Material | Pt Demographic | Country | Study Method | FU | Complications | Outcome | Year, Ref |
|---|---|---|---|---|---|---|---|
| A low-weight PP mesh | 202 with POP | Finland | A prospective RCT comparing low-weight PP mesh for anterior vaginal wall prolapse vs. traditional anterior colporrhaphy. | 24 | ME was seen in 8% of Pts. The dyspareunia score was lower in the mesh group. | Overall symptom rates did not differ in mesh and nonmesh groups. Recurrence rates were 11% in mesh group vs. 41% in nonmesh group. | 2003 [31] |
| Pelivisoft—natural organic mesh made of porcine dermis vs. Pelvitex—PP mesh | 120 with POP | US | An RCT to compare the relative differences between the materials Pelivisoft vs. Pelvitex, as an adjunct to sacral colpopexy surgery. | 12 | One Pt in the Pelvisoft group experienced ME. Two Pts in the porcine group, compared to three Pts in the synthetic mesh group, experienced dyspareunia. | Anatomic cure rates for the Pelvisoft and Pelvitex groups were 81% and 86%, respectively. “Clinical cure” rates for the Pelvisoft and Pelvitex groups were 84% and 90%, respectively. | 2005 [32] |
| Polyform—PP mesh developed by Boston Scientific | 100 with POP | US | A prospective single-blind RCT, to evaluate anterior colporrhaphy vs. cystocele repair using PP mesh or porcine dermis. | 24 | ME in 14% of Pts in the mesh group. Composite failure was 4% in the mesh group, 12% in porcine and 13% in colporrhaphy group. | Pts in PP mesh group had a significantly lower anatomic failure rate (18%) than the porcine (46%) and colporrhaphy groups (58%). | 2005 [33] |
| Ugytex—low-weight and highly porous PP monofilament mesh | 194 with POP | France | A multicentre study to evaluate and compare the prosthesis Ugytex via the transobturator approach vs. anterior colporrhaphy for the surgical treatment of anterior vaginal wall prolapse. | 84 | ME in 13% of Pts during FU. Reintervention for prolapse took place in 9% of Pts. | Similar functional outcomes were seen for both mesh and native tissue repair. Use of mesh did not reduce repeat surgery rates but did reduce anatomical recurrence. | 2005 [34] |
| PROLIFT® system—macroporous PP TVM using a transobturator or transgluteal approach | 260 with POP | Sweden | A prospective multicentre open labelled single cohort study to describe perioperative complications after TVM surgery for POP. | 6 | Serious complications were seen in 4% of Pts. Plus, an extra 15% of Pts experienced minor complications. | Perioperative serious complications are uncommon in the majority of cases after TVM procedure. | 2006 [35] |
| NAZCA TC™ POP repair system—macroporous PP mesh | 104 with POP | Brazil | An RCT to compare colporrhaphy vs. NAZCA TC™ (Promedon HQ, General Manuel Savio L3 M3, Parque Industrial Ferreyra, X5123XAD, Córdoba, Argentina) for the surgical treatment of greater anterior vaginal wall prolapse. | 12 | ME was seen in 5.7% of Pts who underwent surgery with PP mesh adjunct. | Monoprosthesis with combined pre-pubic and trans-obturator arms had high success rates for anterior vaginal POP repair and simultaneous SUI treatment. | 2007 [36] |
| Tension-free vaginal tape PP mesh and transobturator tape PP mesh and suprapubic sling PP mesh | 92,246 with SUI | UK | A retrospective cohort study using hospital episode statistics data measuring complications following tension-free vaginal tape, transobturator tape and suprapubic sling procedures for SUI. | 96 | Peri-procedural and 30-day complication rates were 2.4% and 1.7%, respectively; 6% were readmitted at least once within 5 years. | Study shows that estimated of 9.8% of women experience complications either peri-procedural, within 30 days or within five years of surgery. | 2007 [37] |
| Synthetic monofilament PP mesh | 65 with POP | USA | A double-blind RCT testing the hypothesis that the addition of a standardised technique of inter-positional synthetic PP mesh placement improves the one-year outcome of vaginal reconstructive surgery for POP vs. traditional vaginal reconstructive surgery. | 36 | The study was prematurely halted once a ME complication rate of 16% had been met. | There was no difference in three-year cure rates when comparing Pts undergoing traditional vaginal prolapse surgery without mesh vs. those undergoing vaginal colpopexy repair with mesh. | 2007 [38] |
| GYNECARE PROLIFT + M * Pelvic Floor Repair System—a new lightweight PP mesh | 127 with POP | Belgium | A prospective multicentre study to evaluate the clinical performance of the GYNECARE PROLIFT + M * Pelvic Floor Repair System for the repair of vaginal POP. | 12 | ME rate was 10.2% and rate of de novo dyspareunia was 2%. | 86% of Pts indicated their prolapse situation to be “much better” following surgery. | 2008 [39] |
| Midurethral tension-free vaginal tape—macroporous PP mesh | 160 with SUI | Switzerland | A prospective RCT comparing retropubic transvaginal tape (TVT) with the transobturator tape (outside-in TOT or inside-out TVT-O) sling operation in the treatment of female SUI or stress dominated mixed urinary incontinence. | 12 | Five ME complications identified. 2% TVT, 17% TOT, and 0% TVT-O Pts reported de novo sexual dysfunction, considered significant enough to halt the study. | There was no difference for Q-max between TVT, TOT and TVT-O. Female sexual dysfunction and ME may be higher with a transobturator tape. | 2008 [40] |
| Avaulta—collagen-coated prolene mesh | 138 with POP | Norway, Sweden, Finland and Denmark | An RCT comparing conventional anterior colporrhaphy vs. surgery with Avaulta. | 36 | ME occurred in 13% of Pts at one-year FU, this number did not change by three-year FU. | The objective outcome was superior in the mesh group, but the use of mesh had no impact on the subjective outcome. | 2008 [41] |
| Alyte©—monofilament type 1 PP lightweight Y-mesh | 150 with POP | USA | A prospective study looking at the outcome of Pts who underwent a robotic approach to sacral colpopexy using a PP mesh. | 12 | Nil noted. | Robotic sacrocolpopexy using Alyte© offers excellent subjective and objective results, the clinical cure rate was 95%, and the objective anatomic cure rate was 84%. | 2009 [42] |
| Rectangular PP mesh vs. one posterior rectangular and one anterior PP Y-mesh | 72 with POP | Italy | A prospective RCT to evaluate the outcomes of hysterocolposacropexy with one posterior rectangular and one anterior PP Y-mesh vs. colposacropexy with two rectangular meshes. | 51 | Recurrent low-grade cystoceles developed in 2.6% and 14.7% of Pts and low-grade rectoceles in 15.8% and 8.8% of Pts in the colposacropexy and hysterocolposacropexy groups, respectively. | Whether the uterus was preserved or not, Pts had similar results in terms of prolapse resolution, urodynamic outcomes, improvements in voiding and sexual dysfunctions. | 2010 [43] |
| PP mesh vs. biological graft | 232 with POP | China | A single-blind randomised controlled prospective study evaluating the efficacy, quality of life and complication rates of PP mesh vs. biological graft. | 12 | Adverse events occurred with significantly different frequencies over 1 year. | Similar recurrence rates for PP mesh vs. biological grafts, at short-term FU. Eating soy products often and vaginal intercourse after surgery reduced recurrence. | 2010 [44] |
| Vypromesh® vs. Ultrapromesh® vs. Prolene light mesh® | 144 with SUI | Turkey | A prospective RCT evaluating the effectiveness and complications of three types of synthetic mesh materials in sling surgery. | 48 | 4% of Vypromesh®, 2% of Ultrapro® and 4% of Prolene light mesh® Pts experienced ME, respectively. | Ultrapro® mesh can be used in sling surgery owing to its higher success rates, and lower rates of ME and de novo urgency rates, as shown in clinical studies. | 2011 [45] |
| Ajust® sling vs. standard mid-urethral slings | 419 with SUI | Denmark, Norway and Sweden | An RCT (without blinding) investigating the Ajust® system vs. the current standard mid-urethral sling. | 36 | There were no major complications in either group. Minor complications of urinary tract infections were noted in both groups. | Ajust® appears equally as safe and effective as the standard mid-urethral sling with regards to long-term FU of Pt-reported outcomes. | 2012 [46] |
| Four-arm PP TVM | 160 with POP | Poland | An interventional clinical trial to study the safety and efficacy of performing modified anterior TVM surgery using a four-arm PP mesh adjunct for the treatment of advanced urogenital prolapse after hysterectomy. | 24 | Intraoperative bladder injury in 4% of Pts. 3% complained of de novo SUI. Vaginal vault prolapse recurred in 6% of cases. ME seen in 1% of Pts at six months. | Four-arm PP TVM is safe and effective and provides an alternative treatment option for vaginal vault prolapse, especially in Pts with contraindications to laparotomy and laparoscopy. | 2014 [47] |
| Upsylon™ (Boston Scientific, 300 Boston Scientific Way, Marlborough, MA 01752-1234, USA) —light-weight PP mesh using permanent sutures vs. delayed absorbable sutures for attachment | 198 with POP | US | An RCT to compare mesh and suture exposure rates in women undergoing robotic total hysterectomy and sacrocolpopexy with mesh adjunct with attachment using permanent sutures vs. delayed absorbable sutures. | 12 | Mesh/suture exposure rate of 5.1% in surgery with permanent sutures vs. 7% in surgery with delayed absorbable sutures. 3% of women experienced a serious adverse event. | Suture type used (permanent or delayed absorbable) for vaginal graft attachment did not significantly exposure rates. | 2015 [48] |
| Bilateral abdominal sacral hysteropexy with Prolen®—PP mesh | 22 with POP | Turkey | A single-blind RCT investigating anatomic and sexual outcomes of bilateral sacral hysteropexy with Prolen®. | 18 | Too few Pts to evaluate complications. | This technique appears to provide an adequate clinical resolution, and it has potential to be the primary surgical option for women with POP. | 2015 [49] |
| TiLOOP® PRO A-titanised PP mesh (alloplastic mesh) | 54 with POP | Germany | A multicentre nonrandomised observational clinical investigation to determine usability and collect post-market information on the TiLOOP® PRO A anterior pelvic floor reconstruction meshes, and to determine its effect on quality of life. | 12 | No adverse events related to the investigational device. | Positive outcomes achieved in the reconstruction of the anatomical position of the pelvic floor organs. Pts benefit from anatomical stability as well as improved quality of life, with justifiable risks. | 2016 [50] |
| Ethicon J&J Prolene mesh | 15 with POP | Turkey | An observational study assessing cases of Pts with POP undergoing laparoscopic lateral suspension with mesh and anatomic success measured using transperineal ultrasonography. | 12 | OS | OS | 2016 * |
| Synthetic PP mesh vs. synthetic sutures | 358 with POP | Canada | An interventional randomised controlled multicentre trial to compare experimental bilateral sacrospinous vaginal vault fixation with synthetic mesh arms vs. standard sacrospinous ligament suspension with synthetic sutures. | 24 | OS | OS | 2016 * |
| Two rectangular PP meshes using four absorbable sutures with a nonabsorbable 0.0 PP suture | 100 with POP | Italy | A perspective randomised trial comparing laparoscopic sacrocolpopexy (LASC) vs. robotic-assisted colposacropexy (RASC) for POP repair, both using PP mesh adjunct. In cases of uterus preservation, the anterior mesh was Y-shaped. | 24 | ME rate of 4% in the RASC and 6% in LASC group, all asymptomatic and managed expectantly. | RASC provides outcomes as good as those of LASC with 100% anatomic correction of the apical compartment. RASC was somewhat more efficient and associated with fewer cases of persistent prolapse. | 2018 [51] |
| Ethicon J&J PP mesh | 52 with POP | Egypt | An RCT comparing lateral suspension vs. sacropexy for the treatment of apical POP. | 18 | OS | OS | 2019 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seifalian, A.; Basma, Z.; Digesu, A.; Khullar, V. Polypropylene Pelvic Mesh: What Went Wrong and What Will Be of the Future? Biomedicines 2023, 11, 741. https://doi.org/10.3390/biomedicines11030741
Seifalian A, Basma Z, Digesu A, Khullar V. Polypropylene Pelvic Mesh: What Went Wrong and What Will Be of the Future? Biomedicines. 2023; 11(3):741. https://doi.org/10.3390/biomedicines11030741
Chicago/Turabian StyleSeifalian, Amelia, Zeinab Basma, Alex Digesu, and Vikram Khullar. 2023. "Polypropylene Pelvic Mesh: What Went Wrong and What Will Be of the Future?" Biomedicines 11, no. 3: 741. https://doi.org/10.3390/biomedicines11030741
APA StyleSeifalian, A., Basma, Z., Digesu, A., & Khullar, V. (2023). Polypropylene Pelvic Mesh: What Went Wrong and What Will Be of the Future? Biomedicines, 11(3), 741. https://doi.org/10.3390/biomedicines11030741






