The Inflammatory Signals Associated with Psychosis: Impact of Comorbid Drug Abuse
Abstract
1. Introduction
1.1. Pathogenic Factors of Psychosis
1.2. Psychosis, Drug Abuse and Neuroinflammation
2. Methods
3. Results
3.1. Inflammation and Psychosis
3.1.1. Cytokines
- -
- The elevation of the pro-inflammatory cytokine IL-6 is a finding that, with greater consistency between the different studies, could be considered a trait marker in schizophrenia; that is, one that is associated with hereditary and neurodevelopmental factors and, therefore, of susceptibility to the disease, remaining more or less stable during the different phases of it. Other potential trait markers would be elevations of the pro-inflammatory cytokines IL-1β and TNF-α, but there is insufficient evidence of their rise in high- or ultra-high-risk states of psychosis.
- -
- Elevation of the pro-inflammatory cytokines IFN-γ and TGF-β could be considered state markers of schizophrenia, i.e., those that are associated with the disease itself and its symptoms, and may vary depending on the phase of the disease or antipsychotic treatment. Other potential state markers are IL-4 and IL-10, although in this case, only in chronic schizophrenia and not in the first episodes of psychosis.
3.1.2. Chemokines
3.1.3. Endocannabinoids
3.1.4. Eicosanoids
3.1.5. Lysophospholipids
3.1.6. Bacterial Products
3.2. Inflammation and Drug Abuse
3.2.1. Inflammatory Proteins and Drug Abuse
3.2.2. Inflammatory Lipids and Drug Abuse
4. Discussion
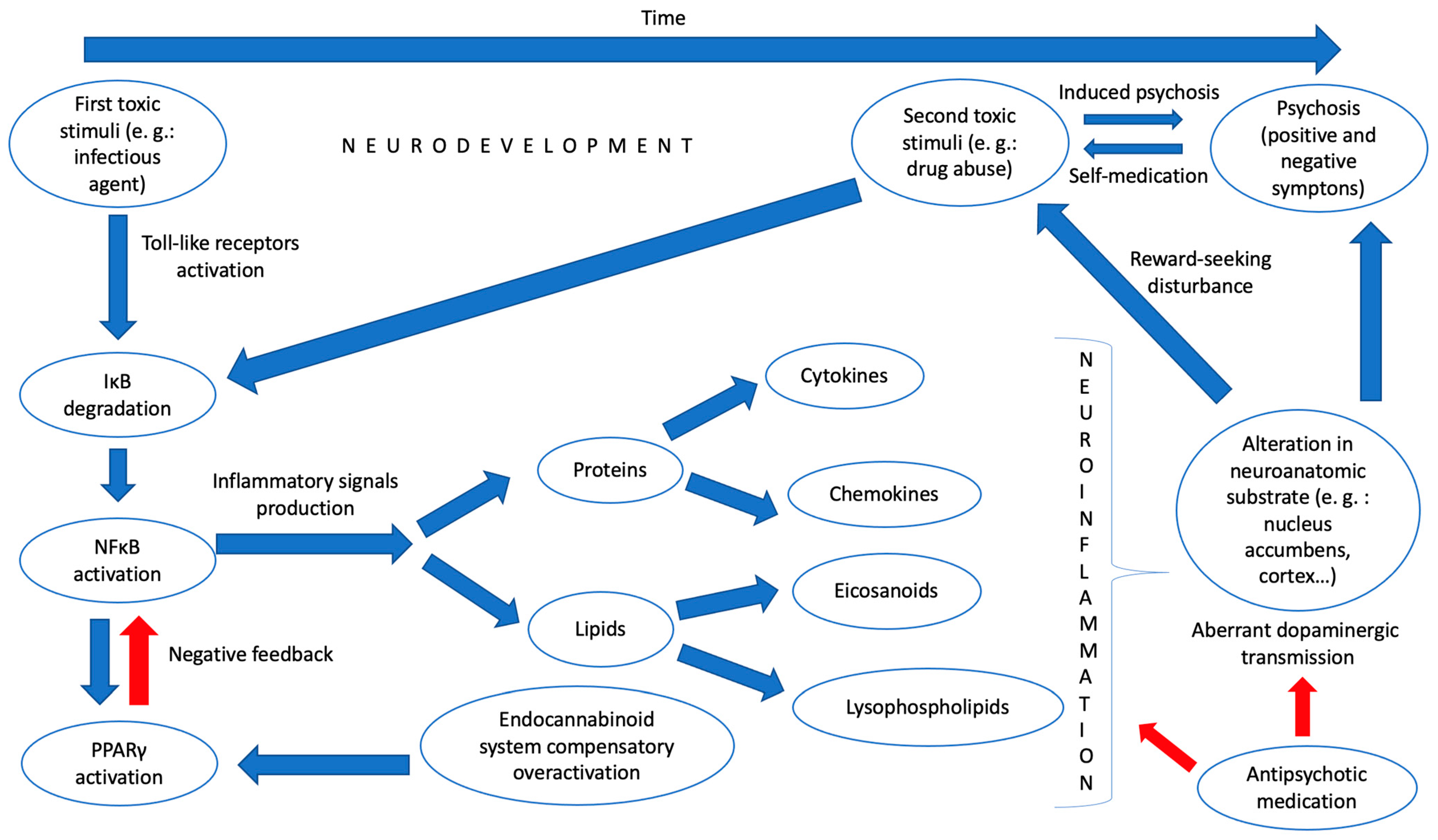
4.1. Drug Abuse and Psychosis: An Inflammatory Convergent Origin?
4.2. Future Perspectives
4.3. Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Arciniegas, D.B. Psychosis. Contin. Minneap. Minn. 2015, 21, 715–736. [Google Scholar] [CrossRef]
- Gaebel, W.; Zielasek, J. Focus on Psychosis. Dialogues Clin. Neurosci. 2015, 17, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Stahl, S.M. Psicosis y Esquizofrenia. In Psicofarmacología Esencial de Stahl; Aula Médica: Madrid, Spain, 2013; pp. 79–128. [Google Scholar]
- Geschwind, D.H.; Flint, J. Genetics and Genomics of Psychiatric Disease HHS Public Access. Science 2015, 349, 1489–1494. [Google Scholar] [CrossRef] [PubMed]
- Stefansson, H.; Rujescu, D.; Cichon, S.; Pietiläinen, O.P.H.; Ingason, A.; Steinberg, S.; Fossdal, R.; Sigurdsson, E.; Sigmundsson, T.; Buizer-Voskamp, J.E.; et al. Large Recurrent Microdeletions Associated with Schizophrenia. Nature 2008, 455, 232–236. [Google Scholar] [CrossRef] [PubMed]
- Burmeister, M.; McInnis, M.G.; Zöllner, S. Heritability Psychiatric Genetics: Progress amid Controversy. Nat. Rev. Genet. 2008, 9, 527–540. [Google Scholar] [CrossRef] [PubMed]
- Sanders, J.; Gill, M. Unravelling the Genome: A Review of Molecular Genetic Research in Schizophrenia. Ir. J. Med. Sci. 2007, 176, 5–9. [Google Scholar] [CrossRef]
- Read, J.; van Os, J.; Morrison, A.P.; Ross, C.A. Childhood Trauma, Psychosis and Schizophrenia: A Literature Review with Theoretical and Clinical Implications. Acta Psychiatr. Scand. 2005, 112, 330–350. [Google Scholar] [CrossRef]
- van Winkel, R.; van Nierop, M.; Myin-Germeys, I.; van Os, J. Childhood Trauma as a Cause of Psychosis: Linking Genes, Psychology, and Biology. Can. J. Psychiatry 2013, 5858, 44–51. [Google Scholar] [CrossRef]
- Gururajan, A.; Manning, E.E.; Klug, M.; van den Buuse, M. Drugs of Abuse and Increased Risk of Psychosis Development. Aust. N. Z. J. Psychiatry 2012, 46, 1120–1135. [Google Scholar] [CrossRef]
- Fiorentini, A.; Volonteri, L.S.; Dragogna, F.; Rovera, C.; Maffini, M.; Mauri, M.C.; Altamura, C.A. Substance-Induced Psychoses: A Critical Review of the Literature. Curr. Drug Abus. Rev. 2011, 4, 228–240. [Google Scholar] [CrossRef]
- Damjanoviü, A.; Pantoviü, M.; Damjanoviü, A.; Dunjiü-Kostiü, B.; Ivkoviü, M.; Milovanoviü, S.; Lackoviü, M.; Dimitrijeviü, I. Cannabis and psychosis revisited. Psychiatr. Danub. 2015, 27, 97–100. [Google Scholar]
- Andrade, C. Cannabis and Neuropsychiatry, 2: The Longitudinal Risk of Psychosis as an Adverse Outcome. J. Clin. Psychiatry 2016, 77, 2252. [Google Scholar] [CrossRef] [PubMed]
- Herrero, M.J.; Domingo-Salvany, A.; Torrens, M.; Brugal, M.T. ITINERE Investigators Psychiatric Comorbidity in Young Cocaine Users: Induced versus Independent Disorders. Addict. Abingdon Engl. 2008, 103, 284–293. [Google Scholar] [CrossRef]
- Mahoney, J.J.; Kalechstein, A.D.; de La Garza, R.; Newton, T.F. Presence and Persistence of Psychotic Symptoms in Cocaine- versus Methamphetamine-Dependent Participants. Am. J. Addict. 2008, 17, 83–98. [Google Scholar] [CrossRef] [PubMed]
- Roncero, C.; Comín, M.; Daigre, C.; Grau-López, L.; Martínez-Luna, N.; Eiroa-Orosa, F.J.; Barral, C.; Torrens, M.; Casas, M. Clinical Differences between Cocaine-Induced Psychotic Disorder and Psychotic Symptoms in Cocaine-Dependent Patients. Psychiatry Res. 2014, 216, 398–403. [Google Scholar] [CrossRef] [PubMed]
- Vergara-Moragues, E.; Mestre-Pintó, J.I.; Araos Gómez, P.; Rodríguez-Fonseca, F.; Torrens, M.; González-Saiz, F. Can Symptoms Help in Differential Diagnosis between Substance-Induced vs. Independent Psychosis in Adults with a Lifetime Diagnosis of Cocaine Use Disorder? Psychiatry Res. 2016, 242, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Green, A.I.; Drake, R.E.; Brunette, M.F.; Noordsy, D.L. Treatment in Psychiatry Schizophrenia and Co-Occurring Substance Use Disorder. Am. J. Psychiatry 2007, 164, 402–408. [Google Scholar] [CrossRef]
- Zweben, J.E.; Cohen, J.B.; Christian, D.; Galloway, G.P.; Salinardi, M.; Parent, D.; Iguchi, M. Methamphetamine Treatment Project Psychiatric Symptoms in Methamphetamine Users. Am. J. Addict. Am. Acad. Psychiatr. Alcohol Addict. 2004, 13, 181–190. [Google Scholar] [CrossRef]
- Archibald, L.; Brunette, M.F.; Wallin, D.J.; Green, A.I. Alcohol Use Disorder and Schizophrenia or Schizoaffective Disorder. Alcohol Res. 2019, 40, e1–e9. [Google Scholar] [CrossRef]
- Quigley, H.; MacCabe, J.H. The Relationship between Nicotine and Psychosis. Adv. Psychopharmacol. 2019, 9, 204512531985996. [Google Scholar] [CrossRef]
- Large, M.; Sharma, S.; Compton, M.T.; Slade, T.; Nielssen, O. Cannabis Use and Earlier Onset of Psychosis: A Systematic Meta-Analysis. Arch. Gen. Psychiatry 2011, 68, 555–561. [Google Scholar] [CrossRef] [PubMed]
- Suvisaari, J.; Mantere, O. Inflammation Theories in Psychotic Disorders: A Critical Review. Infect. Disord. Drug Targets 2013, 13, 59–70. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.S. A Comprehensive Macrophage-T-Lymphocyte Theory of Schizophrenia. Med. Hypotheses 1992, 39, 248–257. [Google Scholar] [CrossRef]
- Smith, R.S.; Maes, M. The Macrophage-T-Lymphocyte Theory of Schizophrenia: Additional Evidence. Med. Hypotheses 1995, 45, 135–141. [Google Scholar] [CrossRef]
- Schwarz, M.J.; Müller, N.; Riedel, M.; Ackenheil, M. The Th2-Hypothesis of Schizophrenia: A Strategy to Identify a Subgroup of Schizophrenia Caused by Immune Mechanisms. Med. Hypotheses 2001, 56, 483–486. [Google Scholar] [CrossRef] [PubMed]
- Monji, A.; Kato, T.; Kanba, S. Cytokines and Schizophrenia: Microglia Hypothesis of Schizophrenia. Psychiatry Clin. Neurosci. 2009, 63, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Lacagnina, M.J.; Rivera, P.D.; Bilbo, S.D. Glial and Neuroimmune Mechanisms as Critical Modulators of Drug Use and Abuse. Neuropsychopharmacology 2017, 42, 156–177. [Google Scholar] [CrossRef] [PubMed]
- Ahearn, O.C.; Watson, M.N.; Rawls, S.M. Chemokines, Cytokines and Substance Use Disorders. Drug Alcohol Depend. 2021, 220. [Google Scholar] [CrossRef]
- García-Bueno, B.; Bioque, M.; Mac-Dowell, K.S.; Barcones, M.F.; Martínez-Cengotitabengoa, M.; Pina-Camacho, L.; Rodríguez-Jiménez, R.; Sáiz, P.A.; Castro, C.; Lafuente, A.; et al. Pro-/Anti-Inflammatory Dysregulation in Patients with First Episode of Psychosis: Toward an Integrative Inflammatory Hypothesis of Schizophrenia. Schizophr. Bull. 2014, 40, 376–387. [Google Scholar] [CrossRef]
- Delaney, S.; Fallon, B.; Alaedini, A.; Yolken, R.; Indart, A.; Feng, T.; Wang, Y.; Javitt, D. Inflammatory Biomarkers in Psychosis and Clinical High Risk Populations. Schizophr. Res. 2019, 206, 440–443. [Google Scholar] [CrossRef]
- Park, S.; Miller, B.J. Meta-Analysis of Cytokine and C-Reactive Protein Levels in High-Risk Psychosis. Schizophr. Res. 2020, 226, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Dawidowski, B.; Górniak, A.; Podwalski, P.; Lebiecka, Z.; Misiak, B.; Samochowiec, J. The Role of Cytokines in the Pathogenesis of Schizophrenia. J. Clin. Med. 2021, 10, 3849. [Google Scholar] [CrossRef] [PubMed]
- Lesh, T.A.; Careaga, M.; Rose, D.R.; McAllister, A.K.; van de Water, J.; Carter, C.S.; Ashwood, P. Cytokine Alterations in First-Episode Schizophrenia and Bipolar Disorder: Relationships to Brain Structure and Symptoms. J. Neuroinflammation 2018, 15, 165. [Google Scholar] [CrossRef] [PubMed]
- Boczek, T.; Mackiewicz, J.; Sobolczyk, M.; Wawrzyniak, J.; Lisek, M.; Ferenc, B.; Guo, F.; Zylinska, L. The Role of g Protein-Coupled Receptors (Gpcrs) and Calcium Signaling in Schizophrenia. Focus on Gpcrs Activated by Neurotransmitters and Chemokines. Cells 2021, 10, 1228. [Google Scholar] [CrossRef]
- Ellman, L.M.; Deicken, R.F.; Vinogradov, S.; Kremen, W.S.; Poole, J.H.; Kern, D.M.; Tsai, W.Y.; Schaefer, C.A.; Brown, A.S. Structural Brain Alterations in Schizophrenia Following Fetal Exposure to the Inflammatory Cytokine Interleukin-8. Schizophr. Res. 2010, 121, 46. [Google Scholar] [CrossRef]
- Brown, A.S. Prenatal Infection as a Risk Factor for Schizophrenia. Schizophr. Bull. 2006, 32, 200. [Google Scholar] [CrossRef]
- Minichino, A.; Senior, M.; Brondino, N.; Zhang, S.H.; Godwlewska, B.R.; Burnet, P.W.J.; Cipriani, A.; Lennox, B.R. Measuring Disturbance of the Endocannabinoid System in Psychosis: A Systematic Review and Meta-Analysis. JAMA Psychiatry 2019, 76, 914. [Google Scholar] [CrossRef]
- Leweke, F.M.; Giuffrida, A.; Koethe, D.; Schreiber, D.; Nolden, B.M.; Kranaster, L.; Neatby, M.A.; Schneider, M.; Gerth, C.W.; Hellmich, M.; et al. Anandamide Levels in Cerebrospinal Fluid of First-Episode Schizophrenic Patients: Impact of Cannabis Use. Schizophr. Res. 2007, 94, 29–36. [Google Scholar] [CrossRef]
- Giuffrida, A.; Leweke, F.M.; Gerth, C.W.; Schreiber, D.; Koethe, D.; Faulhaber, J.; Klosterkötter, J.; Piomelli, D. Cerebrospinal Anandamide Levels Are Elevated in Acute Schizophrenia and Are Inversely Correlated with Psychotic Symptoms. Neuropsychopharmacology 2004, 29, 2108–2114. [Google Scholar] [CrossRef]
- Chase, K.A.; Feiner, B.; Rosen, C.; Gavin, D.P.; Sharma, R.P. Characterization of Peripheral Cannabinoid Receptor Expression and Clinical Correlates in Schizophrenia. Psychiatry Res. 2016, 245, 346–353. [Google Scholar] [CrossRef]
- Smesny, S.; Kunstmann, C.; Kunstmann, S.; Willhardt, I.; Lasch, J.; Yotter, R.A.; Proffitt, T.M.; Kerr, M.; Marculev, C.; Milleit, B.; et al. Phospholipase A2 Activity in First Episode Schizophrenia: Associations with Symptom Severity and Outcome at Week 12. World J. Biol. Psychiatry 2011, 12, 598–607. [Google Scholar] [CrossRef] [PubMed]
- Noponen, M.; Sanfilipo, M.; Samanich, K.; Ryer, H.; Ko, G.; Angrist, B.; Wolkin, A.; Duncan, E.; Rotrosen, J. Elevated PLA2 Activity in Schizophrenics and Other Psychiatric Patients. Biol. Psychiatry 1993, 34, 641–649. [Google Scholar] [CrossRef]
- Gattaz, W.F.; Köllisch, M.; Thuren, T.; Virtanen, J.A.; Kinnunen, P.K.J. Increased Plasma Phospholipase-A2 Activity in Schizophrenic Patients: Reduction after Neuroleptic Therapy. Biol. Psychiatry 1987, 22, 421–426. [Google Scholar] [CrossRef] [PubMed]
- Pereira, C.A.C.; Costa, A.C.; Joaquim, H.P.G.; Talib, L.L.; van de Bilt, M.T.; Loch, A.A.; Gattaz, W.F. COX-2 Pathway Is Upregulated in Ultra-High Risk Individuals for Psychosis. World J. Biol. Psychiatry 2021, 23, 236–241. [Google Scholar] [CrossRef] [PubMed]
- Bowden, N.A.; Weidenhofer, J.; Scott, R.J.; Schall, U.; Todd, J.; Michie, P.T.; Tooney, P.A. Preliminary Investigation of Gene Expression Profiles in Peripheral Blood Lymphocytes in Schizophrenia. Schizophr. Res. 2006, 82, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Omori, W.; Kano, K.; Hattori, K.; Kajitani, N.; Okada-Tsuchioka, M.; Boku, S.; Kunugi, H.; Aoki, J.; Takebayashi, M. Reduced Cerebrospinal Fluid Levels of Lysophosphatidic Acid Docosahexaenoic Acid in Patients With Major Depressive Disorder and Schizophrenia. Int. J. Neuropsychopharmacol. 2021, 24, 948. [Google Scholar] [CrossRef]
- Gotoh, L.; Yamada, M.; Hattori, K.; Sasayama, D.; Noda, T.; Yoshida, S.; Kunugi, H.; Yamada, M. Levels of Lysophosphatidic Acid in Cerebrospinal Fluid and Plasma of Patients with Schizophrenia. Psychiatry Res. 2019, 273, 331–335. [Google Scholar] [CrossRef]
- Madrid-Gambin, F.; Föcking, M.; Sabherwal, S.; Heurich, M.; English, J.A.; O’Gorman, A.; Suvitaival, T.; Ahonen, L.; Cannon, M.; Lewis, G.; et al. Integrated Lipidomics and Proteomics Point to Early Blood-Based Changes in Childhood Preceding Later Development of Psychotic Experiences: Evidence From the Avon Longitudinal Study of Parents and Children. Biol. Psychiatry 2019, 86, 25. [Google Scholar] [CrossRef]
- Maes, M.; Plaimas, K.; Suratanee, A.; Noto, C.; Kanchanatawan, B. First Episode Psychosis and Schizophrenia Are Systemic Neuro-Immune Disorders Triggered by a Biotic Stimulus in Individuals with Reduced Immune Regulation and Neuroprotection. Cells 2021, 10, 2929. [Google Scholar] [CrossRef]
- Maes, M.; Vojdani, A.; Sirivichayakul, S.; Barbosa, D.S.; Kanchanatawan, B. Inflammatory and Oxidative Pathways Are New Drug Targets in Multiple Episode Schizophrenia and Leaky Gut, Klebsiella Pneumoniae, and C1q Immune Complexes Are Additional Drug Targets in First Episode Schizophrenia. Mol. Neurobiol. 2021, 58, 3319–3334. [Google Scholar] [CrossRef]
- Maes, M.; Kanchanatawan, B.; Sirivichayakul, S.; Carvalho, A.F. In Schizophrenia, Increased Plasma IgM/IgA Responses to Gut Commensal Bacteria are Associated with Negative Symptoms, Neurocognitive Impairments, and the Deficit Phenotype. Neurotox. Res. 2019, 35, 684–698. [Google Scholar] [CrossRef]
- Bayazit, H.; Selek, S.; Karababa, I.F.; Cicek, E.; Aksoy, N. Evaluation of Oxidant/Antioxidant Status and Cytokine Levels in Patients with Cannabis Use Disorder. Clin. Psychopharmacol. Neurosci. 2017, 15, 237–242. [Google Scholar] [CrossRef] [PubMed]
- Pacifici, R.; Zuccaro, P.; Farré, M.; Poudevida, S.; Abanades, S.; Pichini, S.; Langohr, K.; Segura, J.; de La Torre, R. Combined Immunomodulating Properties of 3,4-Methylenedioxymethamphetamine (MDMA) and Cannabis in Humans. Addict. Abingdon Engl. 2007, 102, 931–936. [Google Scholar] [CrossRef]
- Fernandez-Egea, E.; Scoriels, L.; Theegala, S.; Giro, M.; Ozanne, S.E.; Burling, K.; Jones, P.B. Cannabis Use is Associated with Increased CCL11 Plasma Levels in Young Healthy Volunteers. Prog. Neuropsychopharmacol. Biol. Psychiatry 2013, 46, 25–28. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, C.B.; de Castro, F.D.O.F.; Dorneles, G.P.; de Sousa Barros, J.B.; Silva, J.M.; Tavares, C.; Carvalho, H.R.; Carlos da Cunha, L.; Nagib, P.; Hoffmann, C.; et al. The Concomitant Use of Cannabis and Cocaine Coexists with Increased LPS Levels and Systemic Inflammation in Male Drug Users. Cytokine 2021, 141, 155472. [Google Scholar] [CrossRef] [PubMed]
- Keen, L.; Turner, A.D. Differential Effects of Self-Reported Lifetime Marijuana Use on Interleukin-1 Alpha and Tumor Necrosis Factor in African American Adults. J. Behav. Med. 2015, 38, 527–534. [Google Scholar] [CrossRef] [PubMed]
- Araos, P.; Pedraz, M.; Serrano, A.; Lucena, M.; Barrios, V.; García-Marchena, N.; Campos-Cloute, R.; Ruiz, J.J.; Romero, P.; Suárez, J.; et al. Plasma Profile of Pro-Inflammatory Cytokines and Chemokines in Cocaine Users under Outpatient Treatment: Influence of Cocaine Symptom Severity and Psychiatric Co-Morbidity. Addict. Biol. 2015, 20, 756–772. [Google Scholar] [CrossRef]
- Moreira, F.P.; Medeiros, J.R.C.; Lhullier, A.C.; de Souza, L.D.M.; Jansen, K.; Portela, L.V.; Lara, D.R.; da Silva, R.A.; Wiener, C.D.; Oses, J.P. Cocaine Abuse and Effects in the Serum Levels of Cytokines IL-6 and IL-10. Drug Alcohol Depend. 2016, 158, 181–185. [Google Scholar] [CrossRef]
- Maza-Quiroga, R.; García-Marchena, N.; Romero-Sanchiz, P.; Barrios, V.; Pedraz, M.; Serrano, A.; Nogueira-Arjona, R.; Ruiz, J.J.; Soria, M.; Campos, R.; et al. Evaluation of Plasma Cytokines in Patients with Cocaine Use Disorders in Abstinence Identifies Transforming Growth Factor Alpha (Tgfα) as a Potential Biomarker of Consumption and Dual Diagnosis. PeerJ 2017, 2017, e3926. [Google Scholar] [CrossRef]
- Halpern, J.H.; Sholar, M.B.; Glowacki, J.; Mello, N.K.; Mendelson, J.H.; Siegel, A.J. Diminished Interleukin-6 Response to Proinflammatory Challenge in Men and Women after Intravenous Cocaine Administration. J. Clin. Endocrinol. Metab. 2003, 88, 1188–1193. [Google Scholar] [CrossRef]
- Pedraz, M.; Araos, P.; García-Marchena, N.; Serrano, A.; Romero-Sanchiz, P.; Suárez, J.; Castilla-Ortega, E.; Mayoral-Cleries, F.; Ruiz, J.J.; Pastor, A.; et al. Sex Differences in Psychiatric Comorbidity and Plasma Biomarkers for Cocaine Addiction in Abstinent Cocaine-Addicted Subjects in Outpatient Settings. Front. Psychiatry 2015, 6, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Levandowski, M.L.; Hess, A.R.B.; Grassi-Oliveira, R.; de Almeida, R.M.M. Plasma Interleukin-6 and Executive Function in Crack Cocaine-Dependent Women. Neurosci. Lett. 2016, 628, 85–90. [Google Scholar] [CrossRef]
- Achur, R.N.; Freeman, W.M.; Vrana, K.E. Circulating Cytokines as Biomarkers of Alcohol Abuse and Alcoholism. J. Neuroimmune Pharm. 2010, 5, 83. [Google Scholar] [CrossRef] [PubMed]
- Moura, H.F.; Hansen, F.; Galland, F.; Silvelo, D.; Rebelatto, F.P.; Ornell, F.; Massuda, R.; Scherer, J.N.; Schuch, F.; Kessler, F.H.; et al. Inflammatory Cytokines and Alcohol Use Disorder: Systematic Review and Meta-Analysis. Braz. J. Psychiatry 2022, 44, 548. [Google Scholar] [CrossRef] [PubMed]
- Crews, F.T.; Bechara, R.; Brown, L.A.; Guidot, D.M.; Mandrekar, P.; Oak, S.; Qin, L.; Szabo, G.; Wheeler, M.; Zou, J. Cytokines and Alcohol. Alcohol Clin. Exp. Res. 2006, 30, 720–730. [Google Scholar] [CrossRef]
- García-Marchena, N.; Maza-Quiroga, R.; Serrano, A.; Barrios, V.; Requena-Ocaña, N.; Suárez, J.; Chowen, J.A.; Argente, J.; Rubio, G.; Torrens, M.; et al. Abstinent Patients with Alcohol Use Disorders Show an Altered Plasma Cytokine Profile: Identification of Both Interleukin 6 and Interleukin 17A as Potential Biomarkers of Consumption and Comorbid Liver and Pancreatic Diseases. J. Psychopharmacol. 2020, 34, 1250–1260. [Google Scholar] [CrossRef]
- Fox, H.C.; Milivojevic, V.; MacDougall, A.; LaVallee, H.; Simpson, C.; Angarita, G.A.; Sinha, R. Stress-Related Suppression of Peripheral Cytokines Predicts Future Relapse in Alcohol-Dependent Individuals with and without Subclinical Depression. Addict. Biol. 2020, 25. [Google Scholar] [CrossRef]
- Clark, K.H.; Wiley, C.A.; Bradberry, C.W. Psychostimulant Abuse and Neuroinflammation: Emerging Evidence of Their Interconnection. Neurotox. Res. 2013, 23, 174–188. [Google Scholar] [CrossRef]
- Loftis, J.M.; Choi, D.; Hoffman, W.; Huckans, M.S. Methamphetamine Causes Persistent Immune Dysregulation: A Cross-Species, Translational Report. Neurotox. Res. 2011, 20, 59. [Google Scholar] [CrossRef]
- Yamamoto, B.K.; Moszczynska, A.; Gudelsky, G.A. Amphetamine Toxicities Classical and Emerging Mechanisms. Ann. N. Y. Acad. Sci. 2010, 1187, 101. [Google Scholar] [CrossRef]
- Yamamoto, B.K.; Raudensky, J. The Role of Oxidative Stress, Metabolic Compromise, and Inflammation in Neuronal Injury Produced by Amphetamine-Related Drugs of Abuse. J. Neuroimmune Pharm. 2008, 3, 203. [Google Scholar] [CrossRef] [PubMed]
- Qiu, F.; Liang, C.L.; Liu, H.; Zeng, Y.Q.; Hou, S.; Huang, S.; Lai, X.; Dai, Z. Impacts of Cigarette Smoking on Immune Responsiveness: Up and down or Upside Down? Oncotarget 2017, 8, 268. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Taneja, V.; Vassallo, R. Cigarette Smoking and Inflammation: Cellular and Molecular Mechanisms. J. Dent. Res. 2012, 91, 142. [Google Scholar] [CrossRef]
- Walter, C.; Ferreirós, N.; Bishay, P.; Geisslinger, G.; Tegeder, I.; Lötsch, J. Exogenous Delta9-Tetrahydrocannabinol Influences Circulating Endogenous Cannabinoids in Humans. J. Clin. Psychopharmacol. 2013, 33, 699–705. [Google Scholar] [CrossRef] [PubMed]
- Manza, P.; Yuan, K.; Shokri-Kojori, E.; Tomasi, D.; Volkow, N.D. Brain Structural Changes in Cannabis Dependence: Association with MAGL. Mol. Psychiatry 2020, 25, 3256. [Google Scholar] [CrossRef]
- Spindle, T.R.; Kuwabara, H.; Eversole, A.; Nandi, A.; Vandrey, R.; Antoine, D.G.; Umbricht, A.; Guarda, A.S.; Wong, D.F.; Weerts, E.M. Brain Imaging of Cannabinoid Type I (CB 1) Receptors in Women with Cannabis Use Disorder and Male and Female Healthy Controls. Addict. Biol. 2021, 26, e13061. [Google Scholar] [CrossRef]
- Ceccarini, J.; Kuepper, R.; Kemels, D.; van Os, J.; Henquet, C.; van Laere, K. [18F]MK-9470 PET Measurement of Cannabinoid CB1 Receptor Availability in Chronic Cannabis Users. Addict. Biol. 2015, 20, 357–367. [Google Scholar] [CrossRef]
- Hirvonen, J.; Goodwin, R.S.; Li, C.T.; Terry, G.E.; Zoghbi, S.S.; Morse, C.; Pike, V.W.; Volkow, N.D.; Huestis, M.A.; Innis, R.B. Reversible and Regionally Selective Downregulation of Brain Cannabinoid CB1 Receptors in Chronic Daily Cannabis Smokers. Mol. Psychiatry 2012, 17, 642. [Google Scholar] [CrossRef]
- Pavõn, F.J.; Araos, P.; Pastor, A.; Calado, M.; Pedraz, M.; Campos-Cloute, R.; Ruiz, J.J.; Serrano, A.; Blanco, E.; Rivera, P.; et al. Evaluation of Plasma-Free Endocannabinoids and Their Congeners in Abstinent Cocaine Addicts Seeking Outpatient Treatment: Impact of Psychiatric Co-Morbidity. Addict. Biol. 2013, 18, 955–969. [Google Scholar] [CrossRef]
- Voegel, C.D.; Kroll, S.L.; Schmid, M.W.; Kexel, A.-K.; Baumgartner, M.R.; Kraemer, T.; Binz, T.M.; Quednow, B.B. Alterations of Stress-Related Glucocorticoids and Endocannabinoids in Hair of Chronic Cocaine Users. Int. J. Neuropsychopharmacol. 2022, 25, 226. [Google Scholar] [CrossRef]
- Kunos, G. Interactions Between Alcohol and the Endocannabinoid System. Alcohol Clin. Exp. Res. 2020, 44, 790–805. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Marchena, N.; Pavon, F.J.; Pastor, A.; Araos, P.; Pedraz, M.; Romero-Sanchiz, P.; Calado, M.; Suarez, J.; Castilla-Ortega, E.; Orio, L.; et al. Plasma Concentrations of Oleoylethanolamide and Other Acylethanolamides Are Altered in Alcohol-Dependent Patients: Effect of Length of Abstinence. Addict. Biol. 2017, 22, 1366–1377. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Chen, C. Cyclooxygenase-2 in Synaptic Signaling. Curr. Pharm. Des. 2008, 14, 1443. [Google Scholar] [CrossRef] [PubMed]
- Copeland, J.R.; Willoughby, K.A.; Police, R.J.; Ellis, E.F. Repeated Cocaine Administration Reduces Bradykinin-Induced Dilation of Pial Arterioles. Am. J. Physiol. 1996, 271. [Google Scholar] [CrossRef]
- Mastrogiannis, D.S.; O’Brien, W.F. Cocaine Affects Prostaglandin Production in Human Umbilical Cord Cell Cultures. J. Matern. Fetal. Neonatal. Med. 2003, 14, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Anton, R.F.; Randall, C.L. Central Nervous System Prostaglandins and Ethanol. Alcohol. Clin. Exp. Res. 1987, 11, 10–18. [Google Scholar] [CrossRef]
- Murphy, R.C.; Westcott, J.Y. Synthesis of Prostaglandins and Leukotrienes. Effects of Ethanol. Recent Dev. Alcohol. 1985, 3, 101–122. [Google Scholar] [CrossRef]
- García-Marchena, N.; Pizarro, N.; Pavón, F.J.; Martínez-Huélamo, M.; Flores-López, M.; Requena-Ocaña, N.; Araos, P.; Silva-Peña, D.; Suárez, J.; Santín, L.J.; et al. Potential Association of Plasma Lysophosphatidic Acid (LPA) Species with Cognitive Impairment in Abstinent Alcohol Use Disorders Outpatients. Sci. Rep. 2020, 10, 17163. [Google Scholar] [CrossRef]
- Holtmann, H.; Resch, K. Cytokines. Naturwissenschaften 1995, 82, 178–187. [Google Scholar] [CrossRef]
- Liu, C.; Chu, D.; Kalantar-Zadeh, K.; George, J.; Young, H.A.; Liu, G. Cytokines: From Clinical Significance to Quantification. Adv. Sci. 2021, 8, 2004433. [Google Scholar] [CrossRef]
- Purves-Tyson, T.D.; Weber-Stadlbauer, U.; Richetto, J.; Rothmond, D.A.; Labouesse, M.A.; Polesel, M.; Robinson, K.; Shannon Weickert, C.; Meyer, U. Increased Levels of Midbrain Immune-Related Transcripts in Schizophrenia and in Murine Offspring after Maternal Immune Activation. Mol. Psychiatry 2021, 26, 849–863. [Google Scholar] [CrossRef] [PubMed]
- Pedraz-Petrozzi, B.; Elyamany, O.; Rummel, C.; Mulert, C. Effects of Inflammation on the Kynurenine Pathway in Schizophrenia—A Systematic Review. J. Neuroinflammation 2020, 17, 56. [Google Scholar] [CrossRef] [PubMed]
- Momtazmanesh, S.; Zare-Shahabadi, A.; Rezaei, N. Cytokine Alterations in Schizophrenia: An Updated Review. Front. Psychiatry 2019, 10, 1. [Google Scholar] [CrossRef] [PubMed]
- Rosenblat, J.D.; McIntyre, R.S. Bipolar Disorder and Inflammation. Psychiatr. Clin. N. Am. 2016, 39, 125–137. [Google Scholar] [CrossRef]
- Munkholm, K.; Vinberg, M.; Vedel Kessing, L. Cytokines in Bipolar Disorder: A Systematic Review and Meta-Analysis. J. Affect. Disord. 2013, 144, 16–27. [Google Scholar] [CrossRef]
- Miller, M.C.; Mayo, K.H. Chemokines from a Structural Perspective. Int. J. Mol. Sci. 2017, 18, 2088. [Google Scholar] [CrossRef]
- Raman, D.; Sobolik-Delmaire, T.; Richmond, A. Chemokines in Health and Disease. Exp. Cell Res. 2011, 317, 575. [Google Scholar] [CrossRef]
- Rostène, W.; Dansereau, M.A.; Godefroy, D.; van Steenwinckel, J.; Goazigo, A.R.; Mélik-Parsadaniantz, S.; Apartis, E.; Hunot, S.; Beaudet, N.; Sarret, P. Neurochemokines: A Menage a Trois Providing New Insights on the Functions of Chemokines in the Central Nervous System. J. Neurochem. 2011, 118, 680–694. [Google Scholar] [CrossRef]
- Najjar, S.; Pahlajani, S.; de Sanctis, V.; Stern, J.N.H.; Najjar, A.; Chong, D. Neurovascular Unit Dysfunction and Blood–Brain Barrier Hyperpermeability Contribute to Schizophrenia Neurobiology: A Theoretical Integration of Clinical and Experimental Evidence. Front. Psychiatry 2017, 8, 1. [Google Scholar] [CrossRef]
- Miller, B.J.; Buckley, P.; Seabolt, W.; Mellor, A.; Kirkpatrick, B. Meta-Analysis of Cytokine Alterations in Schizophrenia: Clinical Status and Antipsychotic Effects. Biol. Psychiatry 2011, 70, 663–671. [Google Scholar] [CrossRef]
- Goldsmith, D.R.; Rapaport, M.H.; Miller, B.J. A Meta-Analysis of Blood Cytokine Network Alterations in Psychiatric Patients: Comparisons between Schizophrenia, Bipolar Disorder and Depression. Mol. Psychiatry 2016, 21, 1696. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.K.; Miller, B.J. Meta-Analysis of Cerebrospinal Fluid Cytokine and Tryptophan Catabolite Alterations in Psychiatric Patients: Comparisons between Schizophrenia, Bipolar Disorder, and Depression. Schizophr. Bull. 2018, 44, 75. [Google Scholar] [CrossRef] [PubMed]
- Çakici, N.; Sutterland, A.L.; Penninx, B.W.J.H.; Dalm, V.A.; de Haan, L.; van Beveren, N.J.M. Altered Peripheral Blood Compounds in Drug-Naïve First-Episode Patients with Either Schizophrenia or Major Depressive Disorder: A Meta-Analysis. Brain Behav. Immun. 2020, 88, 547–558. [Google Scholar] [CrossRef] [PubMed]
- Frydecka, D.; Krzystek-Korpacka, M.; Lubeiro, A.; Stramecki, F.; Stańczykiewicz, B.; Beszłej, J.A.; Piotrowski, P.; Kotowicz, K.; Szewczuk-Bogusławska, M.; Pawlak-Adamska, E.; et al. Profiling Inflammatory Signatures of Schizophrenia: A Cross-Sectional and Meta-Analysis Study. Brain Behav. Immun. 2018, 71, 28–36. [Google Scholar] [CrossRef]
- Isgren, A.; Sellgren, C.; Ekman, C.J.; Holmén-Larsson, J.; Blennow, K.; Zetterberg, H.; Jakobsson, J.; Landén, M. Markers of Neuroinflammation and Neuronal Injury in Bipolar Disorder: Relation to Prospective Clinical Outcomes. Brain Behav. Immun. 2017, 65, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Johansson, V.; Erhardt, S.; Engberg, G.; Kegel, M.; Bhat, M.; Schwieler, L.; Blennow, K.; Zetterberg, H.; Cannon, T.D.; Wetterberg, L.; et al. Twin Study Shows Association between Monocyte Chemoattractant Protein-1 and Kynurenic Acid in Cerebrospinal Fluid. Eur. Arch. Psychiatry Clin. Neurosci. 2020, 270, 933–938. [Google Scholar] [CrossRef]
- Perry, B.I.; Upthegrove, R.; Kappelmann, N.; Jones, P.B.; Burgess, S.; Khandaker, G.M. Associations of Immunological Proteins/Traits with Schizophrenia, Major Depression and Bipolar Disorder: A Bi-Directional Two-Sample Mendelian Randomization Study. Brain Behav. Immun. 2021, 97, 176–185. [Google Scholar] [CrossRef]
- Sathyanarayanan, G.; Thippeswamy, H.; Mani, R.; Venkataswamy, M.; Kumar, M.; Philip, M.; Chandra, P.S. Cytokine Alterations in First-Onset Postpartum Psychosis-Clues for Underlying Immune Dysregulation. Asian J. Psychiatr. 2019, 42, 74–78. [Google Scholar] [CrossRef]
- di Marzo, V.; Piscitelli, F. The Endocannabinoid System and Its Modulation by Phytocannabinoids. Neurotherapeutics 2015, 12, 692. [Google Scholar] [CrossRef]
- Zou, S.; Kumar, U. Cannabinoid Receptors and the Endocannabinoid System: Signaling and Function in the Central Nervous System. Int. J. Mol. Sci. 2018, 19, 833. [Google Scholar] [CrossRef]
- Sugiura, T.; Kondo, S.; Sukagawa, A.; Nakane, S.; Shinoda, A.; Itoh, K.; Yamashita, A.; Waku, K. 2-Arachidonoylglycerol: A Possible Endogenous Cannabinoid Receptor Ligand in Brain. Biochem. Biophys. Res. Commun. 1995, 215, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Stella, N. Endocannabinoid Signaling in Microglial Cells. Neuropharmacology 2009, 56, 244. [Google Scholar] [CrossRef] [PubMed]
- Kleberg, K.; Hassing, H.A.; Hansen, H.S. Classical Endocannabinoid-like Compounds and Their Regulation by Nutrients. Biofactors 2014, 40, 363–372. [Google Scholar] [CrossRef] [PubMed]
- Alger, B.E. Getting High on the Endocannabinoid System. Cerebrum 2013, 2013, 14. [Google Scholar] [PubMed]
- De Marchi, N.; de Petrocellis, L.; Orlando, P.; Daniele, F.; Fezza, F.; di Marzo, V. di Endocannabinoid Signalling in the Blood of Patients with Schizophrenia. Lipids Health Dis. 2003, 2, 5. [Google Scholar] [CrossRef]
- Leweke, F.M.; Piomelli, D.; Pahlisch, F.; Muhl, D.; Gerth, C.W.; Hoyer, C.; Klosterkötter, J.; Hellmich, M.; Koethe, D. Cannabidiol Enhances Anandamide Signaling and Alleviates Psychotic Symptoms of Schizophrenia. Transl. Psychiatry 2012, 2, e94. [Google Scholar] [CrossRef]
- Calde, P.C. Eicosanoids. Essays Biochem. 2020, 64, 423–441. [Google Scholar] [CrossRef]
- Mitchell, J.A.; Kirkby, N.S. Eicosanoids, Prostacyclin and Cyclooxygenase in the Cardiovascular System. Br. J. Pharm. 2019, 176, 1038–1050. [Google Scholar] [CrossRef]
- Wallace, J.L. Eicosanoids in the Gastrointestinal Tract. Br. J. Pharm. 2019, 176, 1000–1008. [Google Scholar] [CrossRef]
- Wang, D.; Dubois, R.N. Eicosanoids and Cancer. Nat. Rev. Cancer 2010, 10, 181–193. [Google Scholar] [CrossRef]
- Biringer, R.G. The Role of Eicosanoids in Alzheimer’s Disease. Int. J. Env. Res. Public Health 2019, 16, 2560. [Google Scholar] [CrossRef]
- Hammock, B.D.; Wang, W.; Gilligan, M.M.; Panigrahy, D. Eicosanoids: The Overlooked Storm in Coronavirus Disease 2019 (COVID-19)? Am. J. Pathol. 2020, 190, 1782–1788. [Google Scholar] [CrossRef] [PubMed]
- Dennis, E.A.; Norris, P.C. Eicosanoid Storm in Infection and Inflammation. Nat. Rev. Immunol. 2015, 15, 511–523. [Google Scholar] [CrossRef] [PubMed]
- Wymann, M.P.; Schneiter, R. Lipid Signalling in Disease. Nat. Rev. Mol. Cell Biol. 2008, 9, 162–176. [Google Scholar] [CrossRef] [PubMed]
- Harizi, H.; Corcuff, J.B.; Gualde, N. Arachidonic-Acid-Derived Eicosanoids: Roles in Biology and Immunopathology. Trends Mol. Med. 2008, 14, 461–469. [Google Scholar] [CrossRef]
- Law, M.H.; Cotton, R.G.H.; Berger, G.E. The Role of Phospholipases A2 in Schizophrenia. Mol. Psychiatry 2006, 11, 547–556. [Google Scholar] [CrossRef]
- Gattaz, W.F. Phospholipase A2 in Schizophrenia. Biol. Psychiatry 1992, 31, 214–216. [Google Scholar] [CrossRef]
- Schmidt, L.; Ceglarek, U.; Kortz, L.; Hoop, M.; Kirkby, K.; Thiery, J.; Himmerich, H. Mechanisms of Involvement of Eicosanoids and Their Precursors in the Pathophysiology and Treatment of Schizophrenia. Med. Chem. 2013, 9, 763–773. [Google Scholar] [CrossRef]
- Ong, W.Y.; Farooqui, T.; Kokotos, G.; Farooqui, A.A. Synthetic and Natural Inhibitors of Phospholipases A2: Their Importance for Understanding and Treatment of Neurological Disorders. ACS Chem. Neurosci. 2015, 6, 814–831. [Google Scholar] [CrossRef]
- Tan, S.T.; Ramesh, T.; Toh, X.R.; Nguyen, L.N. Emerging Roles of Lysophospholipids in Health and Disease. Prog. Lipid Res. 2020, 80, 101068. [Google Scholar] [CrossRef]
- Xu, Y.; Xiao, Y.J.; Baudhuin, L.M.; Schwartz, B.M. The Role and Clinical Applications of Bioactive Lysolipids in Ovarian Cancer. J. Soc. Gynecol. Investig. 2001, 8, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.W.; Chun, J. Lysophospholipids and Their Receptors in the Central Nervous System. Biochim. Biophys. Acta 2013, 1831, 20. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, M.O.; Hunt, J.; Middleton, S.; LeBeau, F.E.N.; Gillies, M.G.; Davies, C.H.; Maycox, P.R.; Whittington, M.A.; Racca, C. Region-Specific Reduction in Entorhinal Gamma Oscillations and Parvalbumin-Immunoreactive Neurons in Animal Models of Psychiatric Illness. J. Neurosci. 2006, 26, 2767. [Google Scholar] [CrossRef] [PubMed]
- Musazzi, L.; di Daniel, E.; Maycox, P.; Racagni, G.; Popoli, M. Abnormalities in α/β-CaMKII and Related Mechanisms Suggest Synaptic Dysfunction in Hippocampus of LPA1 Receptor Knockout Mice. Int. J. Neuropsychopharmacol. 2011, 14, 941–953. [Google Scholar] [CrossRef]
- Roberts, C.; Winter, P.; Shilliam, C.S.; Hughes, Z.A.; Langmead, C.; Maycox, P.R.; Dawson, L.A. Neurochemical Changes in LPA1 Receptor Deficient Mice—A Putative Model of Schizophrenia. Neurochem. Res. 2005, 30, 371–377. [Google Scholar] [CrossRef] [PubMed]
- Harrison, S.M.; Reavill, C.; Brown, G.; Brown, J.T.; Cluderay, J.E.; Crook, B.; Davies, C.H.; Dawson, L.A.; Grau, E.; Heidbreder, C.; et al. LPA1 Receptor-Deficient Mice Have Phenotypic Changes Observed in Psychiatric Disease. Mol. Cell Neurosci. 2003, 24, 1170–1179. [Google Scholar] [CrossRef] [PubMed]
- Ellman, L.M.; Yolken, R.H.; Buka, S.L.; Torrey, E.F.; Cannon, T.D. Cognitive Functioning Prior to the Onset of Psychosis: The Role of Fetal Exposure to Serologically Determined Influenza Infection. Biol. Psychiatry 2009, 65, 1040–1047. [Google Scholar] [CrossRef]
- Sham, P.C.; O’Callaghan, E.; Takei, N.; Murray, G.K.; Hare, E.H.; Murray, R.M. Schizophrenia Following Pre-Natal Exposure to Influenza Epidemics between 1939 and 1960. Br. J. Psychiatry 1992, 160, 461–466. [Google Scholar] [CrossRef]
- O’Callaghan, E.; Gibson, T.; Colohan, H.A.; Walshe, D.; Buckley, P.; Larkin, C.; Waddington, J.L. Season of Birth in Schizophrenia. Evidence for Confinement of an Excess of Winter Births to Patients without a Family History of Mental Disorder. Br. J. Psychiatry 1991, 158, 764–769. [Google Scholar] [CrossRef]
- Barr, C.E.; Mednick, S.A.; Munk-Jorgensen, P. Exposure to Influenza Epidemics during Gestation and Adult Schizophrenia. A 40-Year Study. Arch. Gen. Psychiatry 1990, 47, 869–874. [Google Scholar] [CrossRef]
- Kendell, R.E.; Kemp, I.W. Maternal Influenza in the Etiology of Schizophrenia. Arch. Gen. Psychiatry 1989, 46, 878–882. [Google Scholar] [CrossRef] [PubMed]
- Mednick, S.A.; Machon, R.A.; Huttunen, M.O.; Bonett, D. Adult Schizophrenia Following Prenatal Exposure to an Influenza Epidemic. Arch. Gen. Psychiatry 1988, 45, 189–192. [Google Scholar] [CrossRef] [PubMed]
- Cannon, M.; Cotter, D.; Coffey, V.P.; Sham, P.C.; Takei, N.; Larkin, C.; Murray, R.M.; O’Callaghan, E. Prenatal Exposure to the 1957 Influenza Epidemic and Adult Schizophrenia: A Follow-up Study. Br. J. Psychiatry 1996, 168, 368–371. [Google Scholar] [CrossRef]
- Sorensen, H.J.; Mortensen, E.L.; Reinisch, J.M.; Mednick, S.A. Association Between Prenatal Exposure to Bacterial Infection and Risk of Schizophrenia. Schizophr. Bull. 2009, 35, 631–637. [Google Scholar] [CrossRef]
- Brown, A.S.; Cohen, P.; Greenwald, S.; Susser, E. Nonaffective Psychosis after Prenatal Exposure to Rubella. Am. J. Psychiatry 2000, 157, 438–443. [Google Scholar] [CrossRef] [PubMed]
- Mortensen, P.B.; Nørgaard-Pedersen, B.; Waltoft, B.L.; Sørensen, T.L.; Hougaard, D.; Torrey, E.F.; Yolken, R.H. Toxoplasma Gondii as a Risk Factor for Early-Onset Schizophrenia: Analysis of Filter Paper Blood Samples Obtained at Birth. Biol. Psychiatry 2007, 61, 688–693. [Google Scholar] [CrossRef]
- Brown, A.S.; Derkits, E.J. Prenatal Infection and Schizophrenia: A Review of Epidemiologic and Translational Studies. Am. J. Psychiatry 2013, 167, 261–280. [Google Scholar] [CrossRef]
- Sandhu, K.V.; Sherwin, E.; Schellekens, H.; Stanton, C.; Dinan, T.G.; Cryan, J.F. Feeding the Microbiota-Gut-Brain Axis: Diet, Microbiome, and Neuropsychiatry. Transl. Res. 2017, 179, 223–244. [Google Scholar] [CrossRef]
- Wang, X.; Quinn, P.J. Lipopolysaccharide: Biosynthetic Pathway and Structure Modification. Prog. Lipid Res. 2010, 49, 97–107. [Google Scholar] [CrossRef]
- Barclay, G.R. Endogenous Endotoxin-Core Antibody (EndoCAb) as a Marker of Endotoxin Exposure and a Prognostic Indicator: A Review. Prog. Clin. Biol. Res. 1995, 392, 263–272. [Google Scholar]
- Cai, B.; Wang, M.; Zhu, X.; Xu, J.; Zheng, W.; Zhang, Y.; Zheng, F.; Feng, Z.; Zhu, J. The Fab Fragment of a Humanized Anti-Toll Like Receptor 4 (TLR4) Monoclonal Antibody Reduces the Lipopolysaccharide Response via TLR4 in Mouse Macrophages. Int. J. Mol. Sci 2015, 16, 25502–25515. [Google Scholar] [CrossRef]
- Morcuende, A.; Navarrete, F.; Nieto, E.; Manzanares, J.; Femenía, T. Inflammatory Biomarkers in Addictive Disorders. Biomolecules 2021, 11, 1824. [Google Scholar] [CrossRef]
- Cui, C.; Shurtleff, D.; Harris, R.A. Neuroimmune Mechanisms of Alcohol and Drug Addiction. Int. Rev. Neurobiol. 2014, 118, 1. [Google Scholar] [CrossRef] [PubMed]
- Baldwin, G.C.; Tashkin, D.P.; Buckley, D.M.; Park, A.N.; Dubinett, S.M.; Roth, M.D. Marijuana and Cocaine Impair Alveolar Macrophage Function and Cytokine Production. Am. J. Respir. Crit. Care Med. 1997, 156, 1606–1613. [Google Scholar] [CrossRef] [PubMed]
- Roth, M.D.; Arora, A.; Barsky, S.H.; Kleerup, E.C.; Simmons, M.; Tashkin, D.P. Airway Inflammation in Young Marijuana and Tobacco Smokers. Am. J. Respir. Crit. Care Med. 1998, 157, 928–937. [Google Scholar] [CrossRef] [PubMed]
- Bailey, K.L.; Wyatt, T.A.; Katafiasz, D.M.; Taylor, K.W.; Heires, A.J.; Sisson, J.H.; Romberger, D.J.; Burnham, E.L. Alcohol and Cannabis Use Alter Pulmonary Innate Immunity. Alcohol 2019, 80, 131. [Google Scholar] [CrossRef]
- Klein, T.W.; Lane, B.; Newton, C.A.; Friedman, H. The Cannabinoid System and Cytokine Network. Proc. Soc. Exp. Biol. Med. 2000, 225, 1–8. [Google Scholar] [CrossRef]
- Verhoeckx, K.C.M.; Korthout, H.A.A.J.; van Meeteren-Kreikamp, A.P.; Ehlert, K.A.; Wang, M.; van der Greef, J.; Rodenburg, R.J.T.; Witkamp, R.F. Unheated Cannabis Sativa Extracts and Its Major Compound THC-Acid Have Potential Immuno-Modulating Properties Not Mediated by CB1 and CB2 Receptor Coupled Pathways. Int. Immunopharmacol. 2006, 6, 656–665. [Google Scholar] [CrossRef]
- Klein, T.W. Cannabinoid-Based Drugs as Anti-Inflammatory Therapeutics. Nat. Rev. Immunol. 2005, 5, 400–411. [Google Scholar] [CrossRef]
- Nayak, S.U.; Cicalese, S.; Tallarida, C.; Oliver, C.F.; Rawls, S.M. Chemokine CCR5 and Cocaine Interactions in the Brain: Cocaine Enhances Mesolimbic CCR5 MRNA Levels and Produces Place Preference and Locomotor Activation That Are Reduced by a CCR5 Antagonist. Brain Behav. Immun. 2020, 83, 288. [Google Scholar] [CrossRef]
- Guyon, A.; Skrzydelski, D.; de Giry, I.; Rovère, C.; Conductier, G.; Trocello, J.M.; Daugé, V.; Kitabgi, P.; Rostène, W.; Nahon, J.L.; et al. Long Term Exposure to the Chemokine CCL2 Activates the Nigrostriatal Dopamine System: A Novel Mechanism for the Control of Dopamine Release. Neuroscience 2009, 162, 1072–1080. [Google Scholar] [CrossRef] [PubMed]
- Trecki, J.; Unterwald, E.M. Modulation of Cocaine-Induced Activity by Intracerebral Administration of CXCL12. Neuroscience 2009, 161, 13. [Google Scholar] [CrossRef] [PubMed]
- Trocello, J.M.; Rostene, W.; Melik-Parsadaniantz, S.; Godefroy, D.; Roze, E.; Kitabgi, P.; Kuziel, W.A.; Chalon, S.; Caboche, J.; Apartis, E. Implication of CCR2 Chemokine Receptor in Cocaine-Induced Sensitization. J. Mol. Neurosci. 2011, 44, 147–151. [Google Scholar] [CrossRef] [PubMed]
- Crews, F.T.; Zou, J.; Qin, L. Induction of Innate Immune Genes in Brain Create the Neurobiology of Addiction. Brain Behav. Immun. 2011, 25 (Suppl. 1), S4–S12. [Google Scholar] [CrossRef]
- Adams, C.; Conigrave, J.H.; Lewohl, J.; Haber, P.; Morley, K.C. Alcohol Use Disorder and Circulating Cytokines: A Systematic Review and Meta-Analysis. Brain Behav. Immun. 2020, 89, 501–512. [Google Scholar] [CrossRef]
- Hofford, R.S.; Russo, S.J.; Kiraly, D.D. Neuroimmune Mechanisms of Psychostimulant and Opioid Use Disorders. Eur. J. Neurosci. 2019, 50, 2562. [Google Scholar] [CrossRef]
- Hillard, C.J. Lipids and Drugs of Abuse. Life Sci. 2005, 77, 1531–1542. [Google Scholar] [CrossRef]
- Navarrete, F.; García-Gutiérrez, M.S.; Gasparyan, A.; Navarro, D.; López-Picón, F.; Morcuende, Á.; Femenía, T.; Manzanares, J. Biomarkers of the Endocannabinoid System in Substance Use Disorders. Biomolecules 2022, 12, 396. [Google Scholar] [CrossRef]
- Akaneya, Y. The Remarkable Mechanism of Prostaglandin E2 on Synaptic Plasticity. Gene Regul. Syst. Biol. 2007, 1, 83. [Google Scholar]
- Yamamoto, T.; Anggadiredja, K.; Hiranita, T. New Perspectives in the Studies on Endocannabinoid and Cannabis: A Role for the Endocannabinoid-Arachidonic Acid Pathway in Drug Reward and Long-Lasting Relapse to Drug Taking. J. Pharm. Sci. 2004, 96, 382–388. [Google Scholar] [CrossRef]
- Famitafreshi, H.; Karimian, M. Prostaglandins as the Agents That Modulate the Course of Brain Disorders. Degener. Neurol. Neuromuscul. Dis. 2020, 10, 1. [Google Scholar] [CrossRef] [PubMed]
- Orio, L.; Pavón, F.J.; Blanco, E.; Serrano, A.; Araos, P.; Pedraz, M.; Rivera, P.; Calado, M.; Suárez, J.; Rodríguez De Fonseca, F. Lipid Transmitter Signaling as a New Target for Treatment of Cocaine Addiction: New Roles for Acylethanolamides and Lysophosphatidic Acid. Curr. Pharm. Des 2013, 19, 7036–7049. [Google Scholar] [CrossRef] [PubMed]
- Trang, T.; Sutak, M.; Quirion, R.; Jhamandas, K. The Role of Spinal Neuropeptides and Prostaglandins in Opioid Physical Dependence. Br. J. Pharm. 2002, 136, 37. [Google Scholar] [CrossRef] [PubMed]
- Mohn, A.R.; Yao, W.D.; Caron, M.G. Genetic and Genomic Approaches to Reward and Addiction. Neuropharmacology 2004, 47 (Suppl. 1), 101–110. [Google Scholar] [CrossRef]
- Volkow, N.D.; Michaelides, M.; Baler, R. The Neuroscience of Drug Reward and Addiction. Physiol. Rev. 2019, 99, 2115. [Google Scholar] [CrossRef]
- Pribiag, H.; Stellwagen, D. TNF-α Downregulates Inhibitory Neurotransmission through Protein Phosphatase 1-Dependent Trafficking of GABAA Receptors. J. Neurosci. 2013, 33, 15879. [Google Scholar] [CrossRef]
- Pribiag, H.; Stellwagen, D. Neuroimmune Regulation of Homeostatic Synaptic Plasticity. Neuropharmacology 2014, 78, 13–22. [Google Scholar] [CrossRef]
- Stellwagen, D.; Malenka, R.C. Synaptic Scaling Mediated by Glial TNF-Alpha. Nature 2006, 440, 1054–1059. [Google Scholar] [CrossRef]
- Avital, A.; Goshen, I.; Kamsler, A.; Segal, M.; Iverfeldt, K.; Richter-Levin, G.; Yirmiya, R. Impaired Interleukin-1 Signaling is Associated with Deficits in Hippocampal Memory Processes and Neural Plasticity. Hippocampus 2003, 13, 826–834. [Google Scholar] [CrossRef]
- Mori, F.; Nisticò, R.; Mandolesi, G.; Piccinin, S.; Mango, D.; Kusayanagi, H.; Berretta, N.; Bergami, A.; Gentile, A.; Musella, A.; et al. Interleukin-1β Promotes Long-Term Potentiation in Patients with Multiple Sclerosis. Neuromolecular. Med. 2014, 16, 38–51. [Google Scholar] [CrossRef]
- Heinisch, S.; Kirby, L.G. SDF-1alpha/CXCL12 Enhances GABA and Glutamate Synaptic Activity at Serotonin Neurons in the Rat Dorsal Raphe Nucleus. Neuropharmacology 2010, 58, 501–514. [Google Scholar] [CrossRef] [PubMed]
- Rostène, W.; Kitabgi, P.; Parsadaniantz, S.M. Chemokines: A New Class of Neuromodulator? Nat. Rev. Neurosci. 2007, 8, 895–904. [Google Scholar] [CrossRef] [PubMed]
- Guyon, A.; Nahon, J.L. Multiple Actions of the Chemokine Stromal Cell-Derived Factor-1alpha on Neuronal Activity. J. Mol. Endocrinol. 2007, 38, 365–376. [Google Scholar] [CrossRef] [PubMed]
- Paolicelli, R.C.; Bolasco, G.; Pagani, F.; Maggi, L.; Scianni, M.; Panzanelli, P.; Giustetto, M.; Ferreira, T.A.; Guiducci, E.; Dumas, L.; et al. Synaptic Pruning by Microglia is Necessary for Normal Brain Development. Science 2011, 333, 1456–1458. [Google Scholar] [CrossRef] [PubMed]
- Schafer, D.P.; Lehrman, E.K.; Kautzman, A.G.; Koyama, R.; Mardinly, A.R.; Yamasaki, R.; Ransohoff, R.M.; Greenberg, M.E.; Barres, B.A.; Stevens, B. Microglia Sculpt Postnatal Neural Circuits in an Activity and Complement-Dependent Manner. Neuron 2012, 74, 691. [Google Scholar] [CrossRef]
- Pruessner, M.; Cullen, A.E.; Aas, M.; Walker, E.F. The Neural Diathesis-Stress Model of Schizophrenia Revisited: An Update on Recent Findings Considering Illness Stage and Neurobiological and Methodological Complexities. Neurosci. Biobehav. Rev. 2017, 73, 191–218. [Google Scholar] [CrossRef] [PubMed]
- Vargas, T.; Conley, R.E.; Mittal, V.A. Chronic Stress, Structural Exposures and Neurobiological Mechanisms: A Stimulation, Discrepancy and Deprivation Model of Psychosis. Int. Rev. Neurobiol. 2020, 152, 41. [Google Scholar] [CrossRef] [PubMed]
- Nusslock, R.; Miller, G.E. Early-Life Adversity and Physical and Emotional Health across the Lifespan: A Neuro-Immune Network Hypothesis. Biol. Psychiatry 2016, 80, 23. [Google Scholar] [CrossRef]
- Millan, M.J.; Andrieux, A.; Bartzokis, G.; Cadenhead, K.; Dazzan, P.; Fusar-Poli, P.; Gallinat, J.; Giedd, J.; Grayson, D.R.; Heinrichs, M.; et al. Altering the Course of Schizophrenia: Progress and Perspectives. Nat. Rev. Drug Discov. 2016, 15, 485–515. [Google Scholar] [CrossRef]
- Sheehan, M.F. Dual Diagnosis. Psychiatr. Q. 1993, 64, 107–134. [Google Scholar] [CrossRef]
- Mueser, K.T.; Drake, R.E.; Wallach, M.A. Dual Diagnosis: A Review of Etiological Theories. Addict. Behav. 1998, 23, 717–734. [Google Scholar] [CrossRef] [PubMed]
- Nennig, S.E.; Schank, J.R. The Role of NFkB in Drug Addiction: Beyond Inflammation. Alcohol 2017, 52, 172. [Google Scholar] [CrossRef] [PubMed]
- Gerondakis, S.; Fulford, T.S.; Messina, N.L.; Grumont, R.J. NF-KB Control of T Cell Development. Nat. Immunol. 2014, 15, 15–25. [Google Scholar] [CrossRef] [PubMed]
- Hayden, M.S.; Ghosh, S. Signaling to NF-KappaB. Genes Dev. 2004, 18, 2195–2224. [Google Scholar] [CrossRef] [PubMed]
- Oeckinghaus, A.; Ghosh, S. The NF-KB Family of Transcription Factors and Its Regulation. Cold Spring Harb. Perspect. Biol. 2009, 1, 15. [Google Scholar] [CrossRef]
- García-Bueno, B.; Caso, J.R.; Leza, J.C. Stress as a Neuroinflammatory Condition in Brain: Damaging and Protective Mechanisms. Neurosci. Biobehav. Rev. 2008, 32, 1136–1151. [Google Scholar] [CrossRef]
- Ang, E.; Chen, J.; Zagouras, P.; Magna, H.; Holland, J.; Schaeffer, E.; Nestler, E.J. Induction of Nuclear Factor-KappaB in Nucleus Accumbens by Chronic Cocaine Administration. J. Neurochem. 2001, 79, 221–224. [Google Scholar] [CrossRef]
- Russo, S.J.; Wilkinson, M.B.; Mazei-Robison, M.S.; Dietz, D.M.; Maze, I.; Krishnan, V.; Renthal, W.; Graham, A.; Birnbaum, S.G.; Green, T.A.; et al. Nuclear Factor KB Signaling Regulates Neuronal Morphology and Cocaine Reward. J. Neurosci. 2009, 29, 3529. [Google Scholar] [CrossRef]
- Zhang, X.; Cui, Y.; Jing, J.; Cui, Y.; Xin, W.; Liu, X. Involvement of P38/NF-KB Signaling Pathway in the Nucleus Accumbens in the Rewarding Effects of Morphine in Rats. Behav. Brain Res. 2011, 218, 184–189. [Google Scholar] [CrossRef]
- Crews, F.; Nixon, K.; Kim, D.; Joseph, J.; Shukitt-Hale, B.; Qin, L.; Zou, J. BHT Blocks NF-KappaB Activation and Ethanol-Induced Brain Damage. Alcohol. Clin. Exp. Res. 2006, 30, 1938–1949. [Google Scholar] [CrossRef]
- Qin, L.; He, J.; Hanes, R.N.; Pluzarev, O.; Hong, J.S.; Crews, F.T. Increased Systemic and Brain Cytokine Production and Neuroinflammation by Endotoxin Following Ethanol Treatment. J. Neuroinflammation 2008, 5, 10. [Google Scholar] [CrossRef] [PubMed]
- Zou, J.; Crews, F. Induction of Innate Immune Gene Expression Cascades in Brain Slice Cultures by Ethanol: Key Role of NF-KB and Proinflammatory Cytokines. Alcohol. Clin. Exp. Res. 2010, 34, 777–789. [Google Scholar] [CrossRef]
- García-Bueno, B.; Madrigal, J.L.M.; Lizasoain, I.; Moro, M.A.; Lorenzo, P.; Leza, J.C. Peroxisome Proliferator-Activated Receptor Gamma Activation Decreases Neuroinflammation in Brain after Stress in Rats. Biol. Psychiatry 2005, 57, 885–894. [Google Scholar] [CrossRef] [PubMed]
- Brunetti, L.; Carrieri, A.; Piemontese, L.; Tortorella, P.; Loiodice, F.; Laghezza, A. Beyond the Canonical Endocannabinoid System. A Screening of PPAR Ligands as FAAH Inhibitors. Int J. Mol. Sci. 2020, 21, 7026. [Google Scholar] [CrossRef]
- Jablensky, A. The Diagnostic Concept of Schizophrenia: Its History, Evolution, and Future Prospects. Dialogues Clin. Neurosci. 2010, 12, 271–287. [Google Scholar] [CrossRef]
- Gottesman, I.I.; Gould, T.D. The Endophenotype Concept in Psychiatry: Etymology and Strategic Intentions. Am. J. Psychiatry 2003, 160, 636–645. [Google Scholar] [CrossRef] [PubMed]
- Hosak, L.; Hakeem, K.; Raad, M.; Studnicka, J. Is Microvascular Abnormality a New Endophenotype in Schizophrenia? Psychiatr. Danub. 2015, 27, 225–229. [Google Scholar] [PubMed]
- Smesny, S.; Klemm, S.; Stockebrand, M.; Grunwald, S.; Gerhard, U.J.; Rosburg, T.; Sauer, H.; Blanz, B. Endophenotype Properties of Niacin Sensitivity as Marker of Impaired Prostaglandin Signalling in Schizophrenia. Prostaglandins Leukot Essent Fat. Acids 2007, 77, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Tsuang, M.T.; Stone, W.S.; Faraone, S.V. Toward Reformulating the Diagnosis of Schizophrenia. Am. J. Psychiatry 2000, 157, 1041–1050. [Google Scholar] [CrossRef]
- Torrens, M.; Mestre-Pintó, J.I.; Montanari, L.; Vicente, J.; Domingo-Salvany, A. Dual Diagnosis: An European Perspective. Adicciones 2017, 29, 3–5. [Google Scholar] [CrossRef]
- Alsuhaibani, R.; Smith, D.C.; Lowrie, R.; Aljhani, S.; Paudyal, V. Scope, Quality and Inclusivity of International Clinical Guidelines on Mental Health and Substance Abuse in Relation to Dual Diagnosis, Social and Community Outcomes: A Systematic Review. BMC Psychiatry 2021, 21, 209. [Google Scholar] [CrossRef] [PubMed]
- Szerman, M.N. Patología Dual: Integrando La Salud Mental. Rev. Int. Investig. Adicciones 2017, 3, 1–2. [Google Scholar] [CrossRef]
- Keshavan, M.S.; Kaneko, Y. Secondary Psychoses: An Update. World Psychiatry 2013, 12, 4–15. [Google Scholar] [CrossRef] [PubMed]
- Starzer, M.S.K.; Nordentoft, M.; Hjorthøj, C. Rates and Predictors of Conversion to Schizophrenia or Bipolar Disorder Following Substance-Induced Psychosis. Am. J. Psychiatry 2018, 175, 343–350. [Google Scholar] [CrossRef] [PubMed]
- Correll, C.U.; Howes, O.D. Treatment-Resistant Schizophrenia: Definition, Predictors, and Therapy Options. J. Clin. Psychiatry 2021, 7, 82. [Google Scholar] [CrossRef]
- Silva, M.A.; Restrepo, D. Functional Recovery in Schizophrenia. Rev. Colomb. Psiquiatr. Engl. Ed. 2019, 48, 252–260. [Google Scholar] [CrossRef]
- Seppälä, A.; Pylvänäinen, J.; Lehtiniemi, H.; Hirvonen, N.; Corripio, I.; Koponen, H.; Seppälä, J.; Ahmed, A.; Isohanni, M.; Miettunen, J.; et al. Predictors of Response to Pharmacological Treatments in Treatment-Resistant Schizophrenia—A Systematic Review and Meta-Analysis. Schizophr. Res. 2021, 236, 123–134. [Google Scholar] [CrossRef]
- Levchenko, A.; Nurgaliev, T.; Kanapin, A.; Samsonova, A.; Gainetdinov, R.R. Current Challenges and Possible Future Developments in Personalized Psychiatry with an Emphasis on Psychotic Disorders. Heliyon 2020, 6, e03990. [Google Scholar] [CrossRef]
- Çakici, N.; van Beveren, N.J.M.; Judge-Hundal, G.; Koola, M.M.; Sommer, I.E.C. An Update on the Efficacy of Anti-Inflammatory Agents for Patients with Schizophrenia: A Meta-Analysis. Psychol. Med. 2019, 49, 2307–2319. [Google Scholar] [CrossRef]
- Catalan, A.; Salazar de Pablo, G.; Vaquerizo Serrano, J.; Mosillo, P.; Baldwin, H.; Fernández-Rivas, A.; Moreno, C.; Arango, C.; Correll, C.U.; Bonoldi, I.; et al. Annual Research Review: Prevention of Psychosis in Adolescents–Systematic Review and Meta-Analysis of Advances in Detection, Prognosis and Intervention. J. Child Psychol. Psychiatry 2021, 62, 657–673. [Google Scholar] [CrossRef]
- Agostoni, C.; Nobile, M.; Ciappolino, V.; Delvecchio, G.; Tesei, A.; Turolo, S.; Crippa, A.; Mazzocchi, A.; Altamura, C.A.; Brambilla, P. The Role of Omega-3 Fatty Acids in Developmental Psychopathology: A Systematic Review on Early Psychosis, Autism, and ADHD. Int. J. Mol. Sci. 2017, 18, 2608. [Google Scholar] [CrossRef]
- Murray, R.M.; David, A.S.; Ajnakina, O. Prevention of Psychosis: Moving on from the at-Risk Mental State to Universal Primary Prevention. Psychol. Med. 2021, 51, 223. [Google Scholar] [CrossRef] [PubMed]
- Mcgrath, J. Universal Interventions for the Primary Prevention of Schizophrenia. Aust. N. Z. J. Psychiatry 2000, 34, S58–S64. [Google Scholar] [CrossRef] [PubMed]
- Warner, R. The Prevention of Schizophrenia: What Interventions Are Safe and Effective? Schizophr. Bull. 2001, 27, 551–562. [Google Scholar] [CrossRef]
- Brown, A.S.; McGrath, J.J. The Prevention of Schizophrenia. Schizophr. Bull. 2011, 37, 257. [Google Scholar] [CrossRef] [PubMed]
- Sommer, I.E.; Bearden, C.E.; van Dellen, E.; Breetvelt, E.J.; Duijff, S.N.; Maijer, K.; van Amelsvoort, T.; de Haan, L.; Gur, R.E.; Arango, C.; et al. Early Interventions in Risk Groups for Schizophrenia: What Are We Waiting For? NPJ Schizophr. 2016, 2, 16003. [Google Scholar] [CrossRef]
- di Forti, M.; Quattrone, D.; Freeman, T.P.; Tripoli, G.; Gayer-Anderson, C.; Quigley, H.; Rodriguez, V.; Jongsma, H.E.; Ferraro, L.; la Cascia, C.; et al. The Contribution of Cannabis Use to Variation in the Incidence of Psychotic Disorder across Europe (EU-GEI): A Multicentre Case-Control Study. Lancet Psychiatry 2019, 6, 427. [Google Scholar] [CrossRef] [PubMed]
- Collins, J.A.; Fauser, B.C.J.M. Balancing the Strengths of Systematic and Narrative Reviews. Hum. Reprod. Update 2005, 11, 103–104. [Google Scholar] [CrossRef] [PubMed]
- Köhler-Forsberg, O.; Müller, N.; Lennox, B.R. Editorial: The Role of Inflammation in the Etiology and Treatment of Schizophrenia. Front. Psychiatry 2020, 11, 603296. [Google Scholar] [CrossRef]
- Caviedes, A.; Lafourcade, C.; Soto, C.; Wyneken, U. BDNF/NF-KB Signaling in the Neurobiology of Depression. Curr. Pharm. Des. 2017, 23, 3154–3163. [Google Scholar] [CrossRef]
- Anttila, V.; Bulik-Sullivan, B.; Finucane, H.K.; Walters, R.K.; Bras, J.; Duncan, L.; Escott-Price, V.; Falcone, G.J.; Gormley, P.; Malik, R.; et al. Analysis of Shared Heritability in Common Disorders of the Brain. Science 2018, 360, 8757. [Google Scholar] [CrossRef]
| Study | Type | Population | Aim |
|---|---|---|---|
| García-Bueno et al. [30] | Observational original research | 117 patients (mean age 23.91 ± 5.83 years; 69.2% male) during the first year after their first episode of psychosis (FEP) according to the DSM-IV criteria and 106 matched controls | To contrast the hypothesis that the physiological balance between interrelated pro-inflammatory/anti-inflammatory pathways may be disrupted in FEP |
| Delaney et al. [31] | Observational original research | 47 children, adolescents and young adults with psychosis (mean age 24.30 ± 5.91; 63.83% male), 17 individuals at clinical high risk for psychosis (mean age 22.76 ± 3.68; 64.71% male) and 33 unaffected comparison-matched controls | To compare the levels of vitamin D, C-reactive protein (CRP), antibodies to lipopolysaccharide (LPS) and IL-6 between the groups |
| Park et al. [32] | Systematic review | 8 studies of subjects at high-risk for psychosis (mean age range from 16.1 to 26.2; 31–100% male) versus matched controls (n range for cases from 14 to 76, and for controls from 39 to 115); 4 studies of high-risk converters versus non-converters (n range for converters from 14 to 56, and for non-converters from 60 to 129; mean age range from 16.1 to 21.9; 31–69% male) | To perform a meta-analysis of cytokine and C-reactive protein levels in high-risk psychosis |
| Dawidowski et al. [33] | Review | N/A | To present the most valuable evidence on cytokine dysregulation in schizophrenia, the links between cytokine levels and psychopathological presentation, as well as their alterations in response to antipsychotics |
| Lesh et al. [34] | Observational original research | 69 first-episode schizophrenia-spectrum patients (mean age 19.9 ± 3.5; 88% male), 16 first-episode bipolar patients with psychotic features (mean age 21.4 ± 3.4 years; 75% male) and 53 healthy matched controls | To investigate differences in cytokine levels in plasma between individuals with first-episode schizophrenia, first-episode bipolar disorder with psychotic features, and healthy controls |
| Boczek et al. [35] | Review | N/A | To provide a summary of GPCR (G protein-coupled receptor)-acting neurotransmitters and chemokines and their role in schizophrenia |
| Ellman et al. [36] | Observational original research | 17 cases diagnosed with schizophrenia (mean age 39.96 ± 1.78 years; 70.59% male) and 8 healthy matched controls | To determine the association between fetal exposure to IL-8 and structural brain changes among schizophrenia cases and controls |
| Brown et al. [37] | Review | N/A | To discuss the contribution of exposure to infection to the etiology of schizophrenia |
| Michino et al. [38] | Systematic review | 18 studies in subjects with schizophrenia-related illnesses (44.3–75% male) versus healthy matched controls (n range for cases from 10 to 162, and for controls from 11 to 94). | To conduct a systematic review and meta-analysis of the blood and cerebrospinal fluid (CSF) measures of the endocannabinoid system (ECS) in psychotic disorders |
| Leweke et al. [39] | Observational original research | 25 first-episode, antipsychotic-naïve schizophrenics with low frequency cannabis use (mean age 28.4 ± 8.8 years; 64% male); 19 first-episode, antipsychotic-naïve schizophrenics with high frequency of cannabis use (mean age 30.3; 84.21% male); and 81 healthy matched controls | To examine how cannabis use alters levels of anandamide in cerebrospinal fluid (CSF) in schizophrenic patients |
| Giuffrida et al. [40] | Observational original research | 47 antipsychotic-naïve first-episode paranoid schizophrenics (mean age 28.9 ± 9 years; 53.6% male), 13 dementia patients (mean age 77.8 ± 7.8 years; 46.2% male), 22 affective disorder patients (mean age 44.7 ± 15.8 years; 46.2% male), 71 schizophrenics patients treated with antipsychotics (mean age 29.1 ± 10.1 years; 80.3% male), and 84 volunteers with no family history of psychiatric disturbances (mean age 27.9 ± 2.8 years; 53.6% male) | To examine the role of endocannabinoid signaling in psychotic states by measuring levels of the endocannabinoid anandamide in cerebrospinal fluid (CSF) of acute paranoid-type schizophrenic patients |
| Chase et al. [41] | Observational original research | 35 participants with schizophrenia (mean age 36.14 ± 11.64 years; 51.43% male) and 35 healthy matched controls | To measure mRNA levels of cannabinoid receptors (CBRs) in human peripheral blood mononuclear cells (PBMCs) |
| Smesny et al. [42] | Observational original research | 48 patients with first episode of schizophrenia (mean age 19.41 ± 2.94 years; 72.92% male) and 22 healthy matched controls | To investigate if intracellular phospholipases A2 (inPLA2) activity is associated with symptoms severity and treatment response in first-episode schizophrenia (FES) |
| Noponen et al. [43] | Observational original research | 39 schizophrenics patients (mean age 44.8 ± 10.9 years; 100% male), 26 psychiatric non-schizophrenics patients (mean age 47.2 ± 12.6 years; 100% male) and 26 non-psychiatric and healthy volunteers (mean age 38.3 ± 11 years; 53.85% male) | To measure serum phospholipase A2 (PLA2) activity in all participants |
| Gattaz et al. [44] | Observational original research | 20 paranoid schizophrenic patients (mean age 32 ± 12 years; 45% male), 6 non-schizophrenic psychiatric patients (mean age 37 ± 11 years; 0% male), and 21 non-psychiatric and healthy volunteers (mean age 31 ± 7 years; 47.62% male) | To investigate the activity of phospholipase A2 in the plasma of schizophrenic patients and healthy controls, as well as in a small group of non-schizophrenic psychiatric patients |
| Pereira et al. [45] | Observational original research | 67 ultra-high-risk (UHR) for psychosis individuals (mean age 23.5 ± 3.4 years; 41.79% male) and 55 healthy matched controls | To investigate whether the study of the inflammatory COX-2 pathway through the quantification of the eicosanoid levels can be a useful approach for the characterization of ultra-high-risk (UHR) for psychosis individuals |
| Bowden et al. [46] | Observational original research | 14 individuals with schizophrenia (mean age 35.86 years; 78.57% male) and 14 non-psychiatric matched controls | To generate gene expression profiles from peripheral blood lymphocytes from participants |
| Omori et al. [47] | Observational original research | 27 patients with schizophrenia (mean age 40.1 ± 10.0 years; 51.9% male), 26 patients with major depressive disorder (mean age 40.4 ± 8.3 years; 50% male) and 27 healthy matched controls | To investigate the levels of lysophospholipid species, including LPA and related metabolic enzymes, in cerebrospinal fluid (CSF) of patients with major depressive disorder and schizophrenia |
| Gotoh et al. [48] | Observational original research | Study 1 (cerebrospinal fluid levels): 49 patients with schizophrenia (mean age 39.7 ± 10.5 years; 48.98% male) and 49 healthy matched controls; Study 2 (plasma levels): 42 patients with schizophrenia (mean age 40.7 ± 8.9 years; 54.76% male) and 44 healthy matched controls | To measure lysophosphatidic acid (LPA) levels by enzyme-linked immunosorbent assay in cerebrospinal fluid (CSF) (study 1) and plasma (study 2) samples |
| Madrid-Gambín et al. [49] | Observational original research | 48 patients with psychotic experiences at 18 years of age but who did not have psychotic disorder (45.83% male) and 67 controls (58.2% male) of the same birth cohort | To identify early biomarkers of psychotic experiences in plasma samples of the participants when they were 12 years old |
| Maes et al. [50] | Secondary data analysis | Subjects with first episode of psychosis and schizophrenia | To delineate a) the characteristics of the protein–protein interaction (PPI) network of antipsychotic-naïve first-episode psychosis (AN-FEP) and its transition to schizophrenia; and b) the biological functions, pathways and molecular patterns which are over-represented in FEP/schizophrenia |
| Maes et al. [51] | Observational original research | 21 subjects with first episode of schizophrenia (mean age 38.4 ± 12 years; 47.62% male), 58 subjects with multiple-episode schizophrenia (mean age 41.9 ± 10.7 years; 59.6% male), and 40 healthy matched controls | To delineate (a) the differences in several pathological and neuroimmune pathways between stable-phase, first- (FES) and multiple (MES)-episode schizophrenia and (b) the pathways that determine the behavioral–cognitive–physical–psychosocial (BCPS) deterioration in FES/MES |
| Maes et al. [52] | Observational original research | 80 schizophrenia patients and 38 healthy controls (overall mean age 39.95 years; 55.93% male) | To measure plasma IgA/IgM responses to five Gram-negative bacteria in association with IgM responses to malondialdehyde (MDA) and azelaic acid in participants |
| Study | Type | Population | Aim |
|---|---|---|---|
| Bayazit et al. [53] | Observational original research | 34 patients with cannabis use disorder (mean age of 26 ± 9 years; 100% male) and 34 healthy matched controls | To evaluate oxidant and antioxidant status and cytokine levels in individuals with cannabis use disorder |
| Pacifi et al. [54] | Observational original research | 37 polydrug consumers of 3,4-methylenedioxymethamphetamine (MDMA) and cannabis (mean age 23.6 ± 3.5 years; 51.4% male) compared to 23 cannabis users only (mean age 22 ± 1.9 years; 34.8% male) and 34 non-consumers (mean age 22 ± 2.6 years; 26.5% male) | To investigate cell-mediated immune function and the occurrence of mild infectious diseases in participants |
| Fernandez-Egea et al. [55] | Observational original research | 18 current cannabis users (mean age 22.3 ± 5.1 years; 66% male), 33 past cannabis users (mean age 23.6 ± 4.3 years; 66% male) and 36 subjects who never used cannabis (mean age 24.3 ± 4.7 years; 68% male) | To explore the possibility that cannabis use influenced CCL11 chemokine plasma levels |
| Ribeiro et al. [56] | Observational original research | 21 cannabis users (mean age 28.6 ± 8.54 years; 100% male), 12 cocaine users (mean age 37.8 ± 4.87 years; 100% male), 27 cannabis-plus-cocaine users (mean age 32.3 ± 7.91 years; 100% male) and 21 non-drug users (mean age 33.42 ± 9.73 years; 100% male) | To investigate the effects of illicit drugs on circulating lipopolysaccharide (LPS), systemic inflammation and oxidative stress markers in drug users |
| Keen et al. [57] | Observational original research | 77 lifetime non-drug users (32% male), 46 lifetime marijuana only users (67% male) and 45 lifetime marijuana and other drug users (60% male); overall median age = 47 years | To explore potential differential effects of lifetime marijuana use on interleukin-1 alpha (IL-1α) and tumor necrosis factor (TNF) in a community-based sample |
| Araos et al. [58] | Observational original research | 82 abstinent cocaine users who sought outpatient cocaine treatment (mean age 36.9 ± 7.8 years; 18.3% male) and 65 healthy matched controls | To examine the plasma pro-inflammatory cytokine and chemokine profile in participants |
| Moreira et al. [59] | Observational original research | 12 cocaine users (mean age 24.92 ± 4.80 years; 75% male) and 24 healthy matched controls | To investigate serum levels of pro and anti-inflammatory cytokines, IL-6 and IL-10, respectively, in cocaine users from a young population-based sample |
| Maza-Quiroga et al. [60] | Observational original research | 79 patients diagnosed with cocaine use disorder (CUD) in abstinence (34.87 ± 7.18 years) and 81 healthy matched controls | To test the hypothesis that patients with CUD in abstinence might have altered circulating levels of signaling proteins related to systemic inflammation |
| Halpern et al. [61] | Experimental original research | 30 healthy participants with a history of cocaine use (16 females (mean age 25.8 ± 1.0 years)) and 14 males (mean age 27.8 ± 1.5 years)) | To measure neuroendocrine and immunological responses to IV injection of 0.4 mg/kg cocaine or saline placebo |
| Pedraz et al. [62] | Observational original research | 55 abstinent cocaine-addicted subjects diagnosed with lifetime cocaine use disorders (40 men (mean age 37.1 ± 6.7 years) and 15 women (mean age 42.8 ± 6.2 years)) and 73 healthy matched controls | To evaluate the sex differences in psychiatric comorbidity and the concentrations of plasma mediators that have been reported to be affected by cocaine |
| Levandowski et al. [63] | Observational original research | 42 crack cocaine-dependent women (mean age 31.22 ± 7.83 years) and 52 healthy matched controls | To investigate the association between plasma interleukin 6 (IL-6) levels and executive function (EF) in crack cocaine-dependent women |
| Anchur et al. [64] | Review | N/A | To discuss cytokine biomarker candidates for alcohol abuse and alcoholism |
| Moura et al. [65] | Systematic review | 23 studies of subjects with alcohol use disorder (56–100% male) and healthy matched controls (n range for cases from 9 to 42, and for controls from 6 to 46) | To assess differences in blood inflammatory cytokines between people with alcohol use disorder (AUD) and healthy controls (HC) |
| Crews et al. [66] | Review | Alcohol users | To discuss the contribution of cytokines in alcohol use and alcoholic pathologies |
| García-Marchena et al. [67] | Observational original research | 85 abstinent subjects with alcohol use disorders (mean age 47.16 ± 7.27 years; 68.24% male) and 55 healthy matched controls | To explore possible associations in circulating plasma cytokine concentrations in abstinent patients diagnosed with alcohol use disorders |
| Fox et al. [68] | Experimental original research | 33 alcohol-dependent individuals (12 with low depressive symptoms (mean age 38.7 ± 2.6 years; 86% male) and 21 with high depressive symptoms (mean age 39.1 ± 2.4 years; 84% male)) and 37 social drinkers (21 with low depressive symptoms (mean age 31.9 ± 2.2 years; 62% male) and 16 with high depressive symptoms (mean age 35.7 ± 2.4 years; 38% male)) | To examine cytokine responses to stress in alcohol-dependent individuals and social drinkers, both with and without subclinical depression |
| Clark et al. [69] | Review | N/A | To review evidence that psychostimulants of abuse (cocaine, methamphetamine, ecstasy) are associated with activation of the innate immune response |
| Loftis et al. [70] | Observational original research (+preclinical experimental model) | 20 adults in remission from methamphetamine (MA) dependence (mean age 33.3 ± 1.84 years; 70% male) and 20 healthy matched controls (+preclinical model) Preclinical model: 32 male C57BL/6J mice that were administered MA (1 mg/kg) or saline subcutaneously for 7 consecutive days | To test the hypothesis that immune factors, such as cytokines, chemokines and cellular adhesion molecules, contribute to MA-induced immune dysfunction, neuronal injury and persistent cognitive impairments |
| Yamamoto et al. [71] | Review | N/A | To discuss long-term decreases in markers of biogenic amine neurotransmission in methamphetamine and MDMA users |
| Yamamoto et al. [72] | Review | N/A | To highlight experimental evidence that methamphetamine and MDMA increase oxidative stress, produce mitochondrial dysfunction and increase inflammation, all of which converge and culminate in long-term toxicity to dopaminergic and serotonergic neurons |
| Qiu et al. [73] | Review | N/A | To review the influence of smoking on major components of both innate and adaptive immune cells, and summarize cellular and molecular mechanisms underlying effects of cigarette smoking on the immune system |
| Lee et al. [74] | Review | N/A | To discuss specific mechanisms by which cigarette smoking affects host immunity |
| Walter et al. [75] | Experimental original research (+preclinical experimental model) | 15 healthy young men (mean age, 28.1 ± 3.1 years) and 15 women (mean age, 26.6 ± 2.4 years); preclinical model: 20 female Lewis rats (10 rats per treatment group) that were administered 3 mg/kg of the CB1/CB2-agonist WIN 55,212-2 dissolved in 1:1 dimethyl sulfoxide/phosphate buffer | To investigate effects in circulating concentrations of endocannabinoids after administration of a single oral dose of 20 mg delta9-tetrahydrocannabinol (THC) to 30 healthy volunteers and comparison with placebo |
| Manza et al. [76] | Observational original research | 89 individuals with cannabis dependence (mean age 28.6 ± 3.5 years; 71.9% male) and 89 healthy matched controls | To lend insight into biological processes that might link chronic cannabis use to brain structural abnormalities |
| Spindle et al. [77] | Experimental original research | 10 females with cannabis use disorder (mean age 23.2 ± 2.7 years), 10 female healthy controls (mean age 25.5 ± 5 years) and 7 male non-cannabis consumers (mean age 29.6 ± 6.9 years) | To explore the relation between acute cannabis effects and mood/craving/withdrawal and CB1 receptor availability |
| Ceccarini et al. [78] | Observational original research | 10 chronic cannabis users (mean age 26.0 ± 4.1 years; 80% male) and 10 healthy matched controls | To test that chronic cannabis use may alter specific regional CB1 receptor expression |
| Hirvonen et al. [79] | Observational original research | 30 male cannabis smokers (mean age 28 ± 8 years) and 28 healthy matched controls | To demonstrate downregulation of brain cannabinoid CB1 (cannabinoid receptor type 1) receptors after chronic exposure to cannabis in humans |
| Pavon et al. [80] | Observational original research | 88 abstinent cocaine addicts (mean age 36.9 ± 8.4 years; 88.6% male) and 46 matched healthy control | To evaluate circulating endocannabinoid-related lipids as biomarkers of cocaine use disorder |
| Voegel et al. [81] | Observational original research | 73 chronic cocaine users (mean age 31.3 ± 9.5 years; 67.12% male) and 67 healthy matched controls | To investigate alterations of hypothalamic–pituitary–adrenal (HPA) axis and endocannabinoid (eCB) system markers in individuals with chronic cocaine use disorder |
| Kunos et al. [82] | Review | N/A | To show evidence accumulated over the last two decades to indicate that both the addictive neural effects of ethanol and its organ toxic effects in the liver and elsewhere are mediated, to a large extent, by endocannabinoid signaling |
| García-Marchena et al. [83] | Observational original research | 79 abstinent alcohol-dependent subjects (49.13 ± 9.6 years; 65.8% male) and 79 healthy matched controls | To characterize the plasma acylethanolamides in alcohol dependence |
| Yang et al. [84] | Review | N/A | To discuss the role of cyclooxygenase-2 (COX-2) in synaptic signaling |
| Copeland et al. [85] | Experimental preclinical study | Preclinical model: 51 young, male rabbits that were randomly selected to receive subcutaneous injections of either cocaine or saline solution | To study cocaine-induced alterations in cerebrovascular function and metabolism |
| Mastrogiannis et al. [86] | Experimental in vitro model | Endothelial cells were isolated from human umbilical veins derived from uncomplicated pregnancies with a negative history of drug abuse | To investigate the possible effects of cocaine on prostacyclin and prostaglandin (PG) E2 production from endothelial cells derived from human umbilical cord |
| Anton et al. [87] | Review | N/A | To review the nature and role of prostaglandins in the central nervous system, and what is known about the effect of ethanol on prostaglandin production in brain |
| Murphy et al. [88] | Review | N/A | To discuss effects of ethanol in synthesis of prostaglandins and leukotrienes |
| García-Marchena et al. [89] | Observational original research | 55 abstinent alcohol use disorder (AUD) patients (mean age 47.7 ± 7.7 years; 81.8% male) and 34 healthy matched controls | To investigate whether the relevant species of LPA were associated with clinical features of alcohol addiction |
| Type of Biomarker | Main Findings | References |
|---|---|---|
| Cytokines | ↑ Pro-inflammatory cytokines ↓ Anti-inflammatory cytokines ↑ IL-6 as a trait marker of schizophrenia (lower level of evidence for IL-1ß and TNF-α) ↑ IFN-γ and TGF-β as state markers of schizophrenia (lower level of evidence for IL-4 and IL-10) Overlap between altered cytokine profiles in schizophrenia and bipolar disorder | [30,31,32,33,34] |
| Chemokines | Correlation between ↑ pro-inflammatory chemokines (e.g., CCL2, CCL4, CCL11, CCL17, CCL22, and CCL24) and schizophrenic symptoms Relationship between exposure to IL-8/CXCL8 and impaired neurodevelopment MCP-1 (CCL2) as a trait marker of schizophrenia | [33,35,36,37] |
| Endocannabinoids | ↑ Anandamide in CSF and blood ↑ Expression CB1R in peripheral immune cells Negative correlation between positive and negative symptoms and anandamide levels in CSF Positive correlation between positive and negative symptoms of CB1R and CB2R in mononuclear cells | [38,39,40,41] |
| Eicosanoids | ↑ Baseline PLA2 activity in FEP and drug-free schizophrenic patients Positive correlation between PLA2 activity and severity of schizophrenic symptoms ↑ PGE2 and TxB2 in patients with criteria for ultra-high risk of psychosis | [42,43,44,45] |
| Lysophospholipids | Downward regulation of the LPA1R gene ↓ LPA 22:6 in CSF Negative correlation between plasma levels of LPA and score on the PANSS scale ↑ Lysophosphatidylcholines years before the onset of the disease | [46,47,48,49] |
| Bacterial products | Positive correlation between ↑ anti-LPS antibody and IL-6 Overexpression of genes in patients with first episode of psychosis involved in the response to LPS ↑ Increased IgA/IgM responses to LPS in FEP and deficit schizophrenia and association between them and general cognitive impairment | [31,50,51,52] |
| Type of Biomarker | Main Findings | References | |
|---|---|---|---|
| Inflammatory proteins | Cannabis | ↑ IL-1ß, IL-8, TGF-ß, CCL11 ↓ IL-2 Conflicts results for IL-6, TNFα | [53,54,55,56,57] |
| Cocaine | ↓ TNF-α, TGF-α, IL-1β, CXCL12, CCL2, CCL3 and CX3CL1 in substance-dependent humans during periods of withdrawal (but some of them elevated during acute cocaine exposure in mice) ↓ TGF-α as a potential biomarker of dual diagnosis Positive correlation between plasma levels of IL-1β, CXCL12 and CX3CL1, and criteria of abuse and dependence ↓ IL-10 in active users ↓ IL-17 in abstinence users Conflicts results for IL-6 | [58,59,60,61,62,63] | |
| Alcohol | Dysregulation of TNFα, IL-1α, IL-1ß, IL-6, IL-8, IL-12 and MCP-1 ↑IL-1ß, IL-6 and TNFα in abstinent users ↓IL- 4, IL-17A and IFN- γ in abstinent users Transition from Th1 to Th2 cytokines Correlation in changes in IL-6 and IL-17A with liver and pancreatic diseases Stress-related suppression of peripheral cytokines may predict future relapse in alcohol-dependent individuals | [64,65,66,67,68] | |
| MA | ↑ TNF α, IL-1ß, IL-6 and CCL2 | [69,70,71,72] | |
| Tobacco | Dysregulation in production of pro/anti-inflammatory cytokines | [73,74] | |
| Inflammatory lipids | Cannabis | Altered levels of anandamide, 2-AG, PEA and OEA ↓ Density CB1R in brain | [75,76,77,78,79] |
| Cocaine | ↑ NAEs in abstinent cocaine addicts ↓ 2-AG in abstinent cocaine addicts ↓ Hair concentrations of OEA and PEA in DCU compared with RCU and controls Altered plasma levels of PGI2, PDE2 and TXA2 | [80,81,84,85,86] | |
| Alcohol | ↑ Anandamide, 2-AG and NAEs Alterations in the production of prostaglandins, thromboxane and leukotrienes ↓ Total LPA | [82,83,87,88,89] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herrera-Imbroda, J.; Flores-López, M.; Ruiz-Sastre, P.; Gómez-Sánchez-Lafuente, C.; Bordallo-Aragón, A.; Rodríguez de Fonseca, F.; Mayoral-Cleríes, F. The Inflammatory Signals Associated with Psychosis: Impact of Comorbid Drug Abuse. Biomedicines 2023, 11, 454. https://doi.org/10.3390/biomedicines11020454
Herrera-Imbroda J, Flores-López M, Ruiz-Sastre P, Gómez-Sánchez-Lafuente C, Bordallo-Aragón A, Rodríguez de Fonseca F, Mayoral-Cleríes F. The Inflammatory Signals Associated with Psychosis: Impact of Comorbid Drug Abuse. Biomedicines. 2023; 11(2):454. https://doi.org/10.3390/biomedicines11020454
Chicago/Turabian StyleHerrera-Imbroda, Jesús, María Flores-López, Paloma Ruiz-Sastre, Carlos Gómez-Sánchez-Lafuente, Antonio Bordallo-Aragón, Fernando Rodríguez de Fonseca, and Fermín Mayoral-Cleríes. 2023. "The Inflammatory Signals Associated with Psychosis: Impact of Comorbid Drug Abuse" Biomedicines 11, no. 2: 454. https://doi.org/10.3390/biomedicines11020454
APA StyleHerrera-Imbroda, J., Flores-López, M., Ruiz-Sastre, P., Gómez-Sánchez-Lafuente, C., Bordallo-Aragón, A., Rodríguez de Fonseca, F., & Mayoral-Cleríes, F. (2023). The Inflammatory Signals Associated with Psychosis: Impact of Comorbid Drug Abuse. Biomedicines, 11(2), 454. https://doi.org/10.3390/biomedicines11020454






