The Regulation of Endothelin-1 in Pregnancies Complicated by Gestational Diabetes: Uncovering the Vascular Effects of Insulin
Abstract
1. Introduction
2. Materials and Methods
2.1. Tissue Collection
2.2. Enzyme-Linked Immunosorbent Assay (ELISA)
2.3. Assessment of Vascular Reactivity
2.4. ET-1 Induced Omental Artery Constriction in Omental Arteries from Healthy Pregnancies and Those Complicated by GDM
2.5. Effect of ET-1 Receptor Antagonists on ET-1 Induced Omental Artery Constriction
2.6. Effect of Insulin Treatment on ET-1 Induced Constriction
2.7. Human Umbilical Vein Endothelial Cell (HUVEC) Isolation and Culture
2.8. In Vitro Treatment with Insulin and ET-1 Receptor Antagonists
2.9. MTS Cell Viability Assay
2.10. Quantitative Real-Time Polymerase Chain Reaction (qPCR)
2.11. Collection and Culture of Placental Explants
2.12. Effect of Conditioned Placental Explant Media on ET-1 Induced Constriction
2.13. Statistical Analysis
3. Results
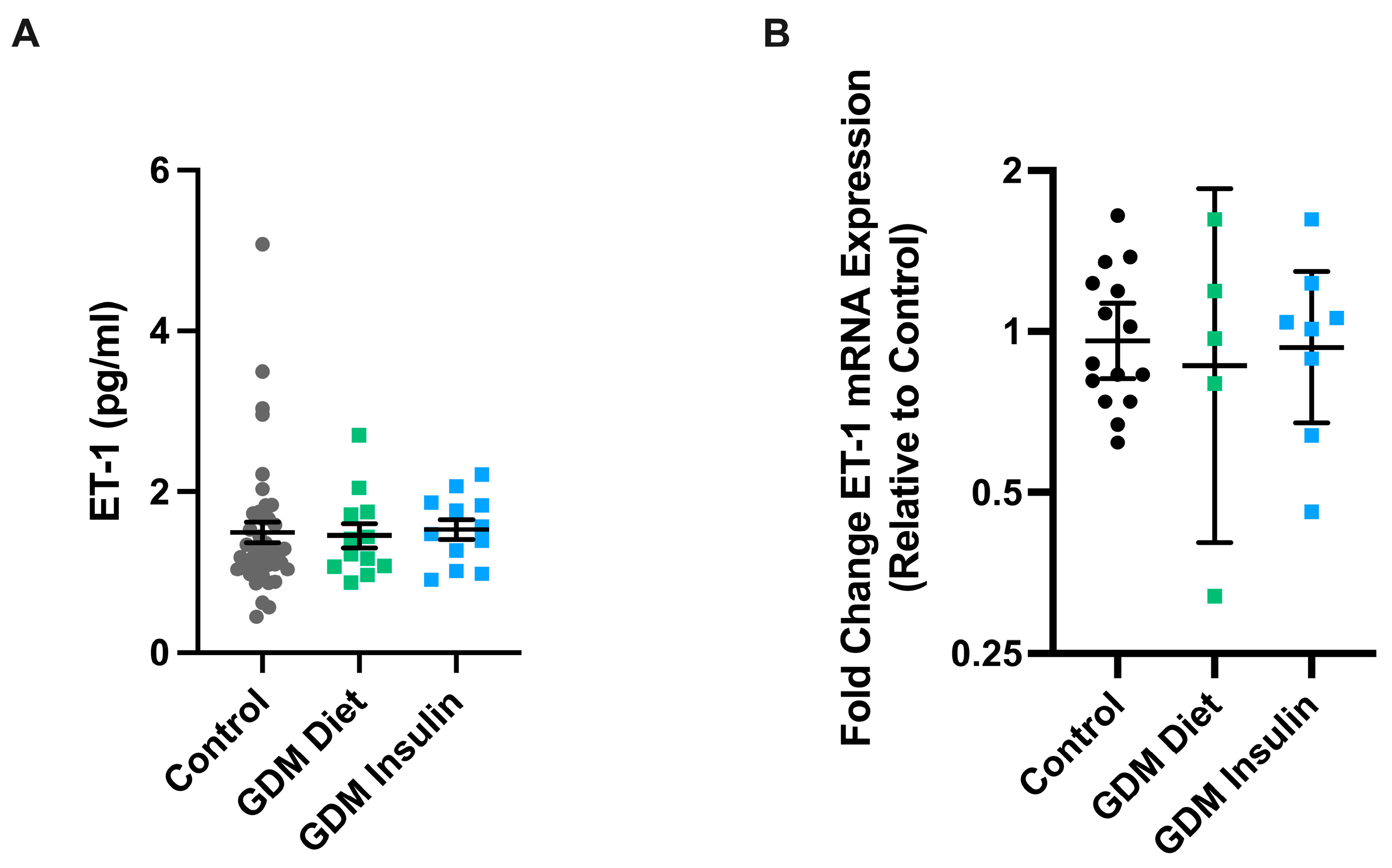
3.1. Circulating ET-1 Levels and Vascular ET-1 mRNA Expression Is Not Altered in Pregnancies Complicated by GDM Compared to Healthy Gestation-Matched Controls
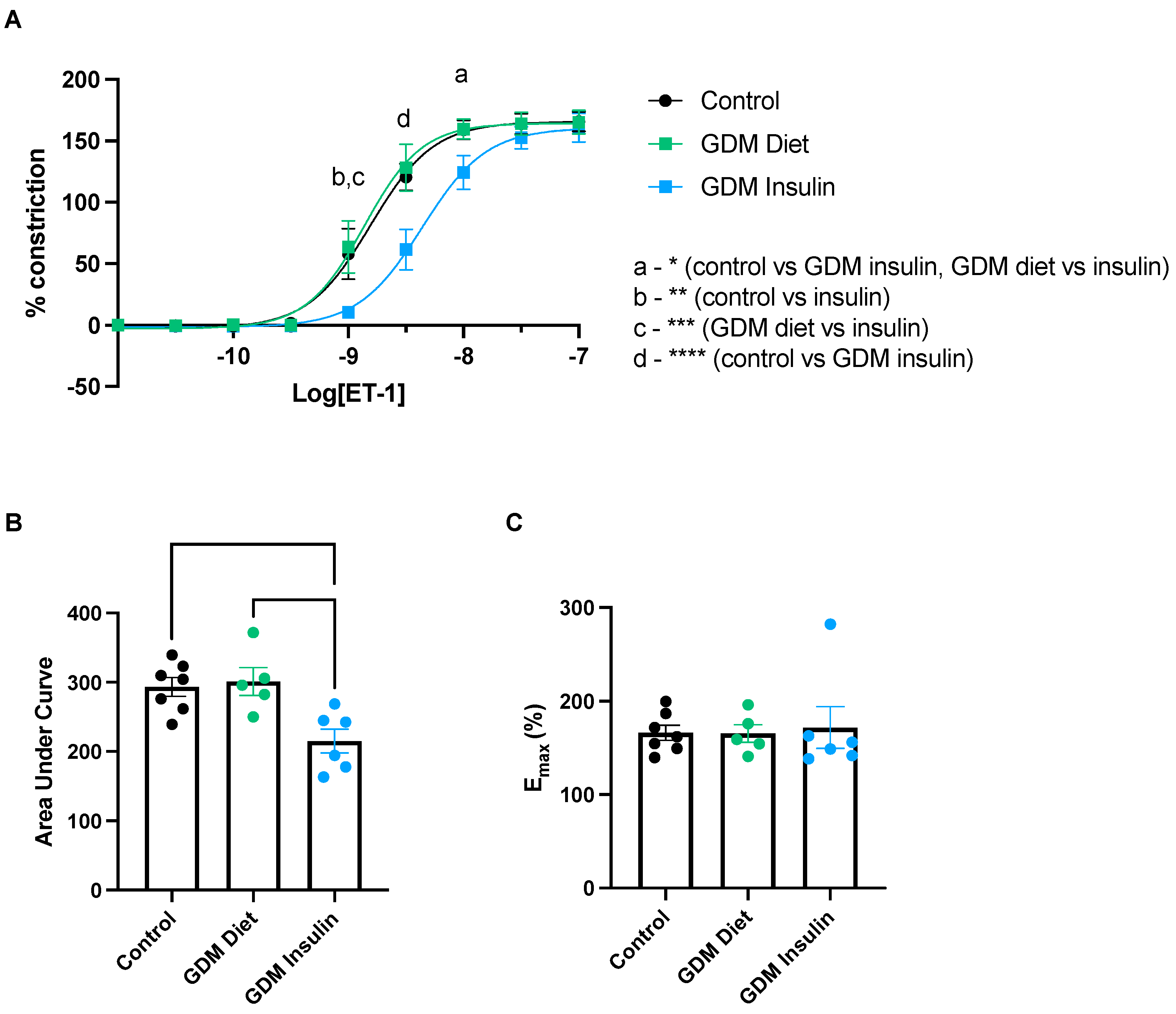
3.2. Omental Arteries Collected from Pregnancies Complicated by GDM and Treated with Insulin Demonstrated Reduced Constriction Compared to Arteries from Pregnancies Managed with Diet or Healthy Controls
3.3. ET-1 Antagonists, BQ123 and BQ788, Inhibit ET-1 Induced Constriction in Omental Arteries from Healthy Pregnancies and Those Complicated by GDM
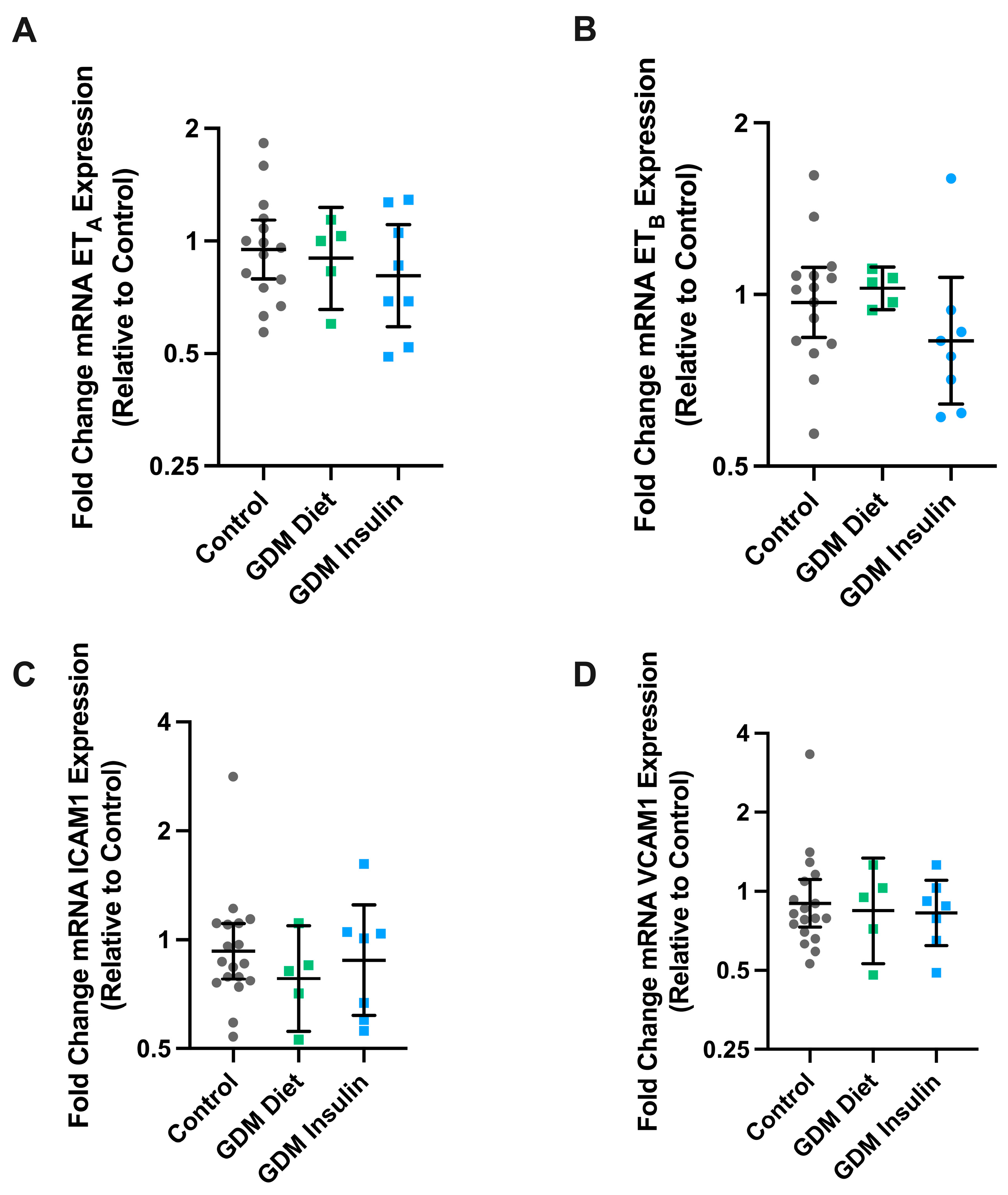
3.4. The mRNA Expression of ETA, ETB, VCAM, and ICAM in Maternal Omental Arteries Is Not Altered in GDM
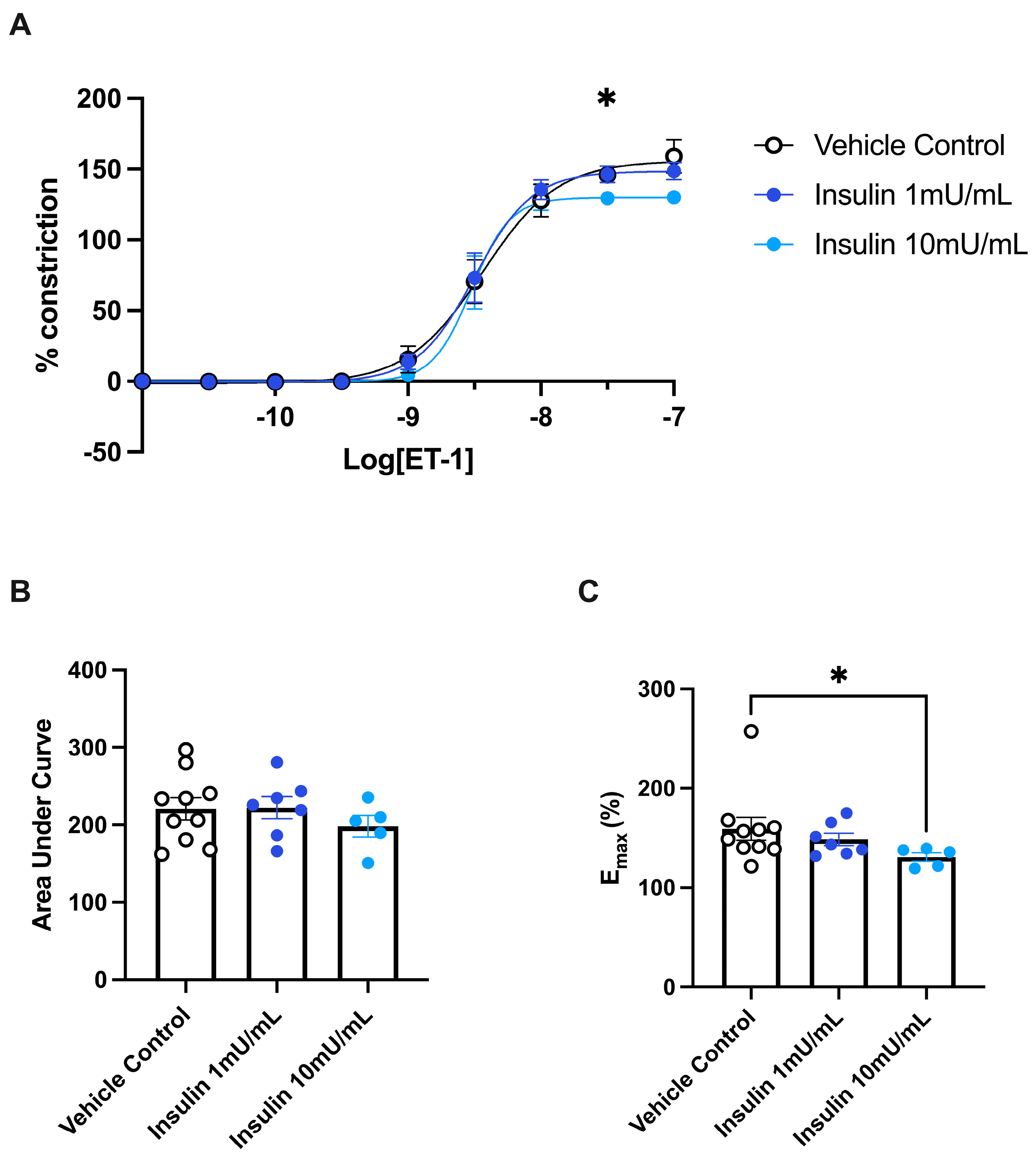
3.5. ET-1 Induced Constriction of Omental Arteries Is Reduced by Exposure to Insulin
3.6. Models of Endothelial Dysfunction and Treatment with Insulin
3.7. Conditioned Media Obtained from Placental Tissue Exposed to High Glucose Does Not Alter Omental Artery Vasoconstriction to ET-1
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Plows, J.F.; Stanley, J.L.; Baker, P.N.; Reynolds, C.M.; Vickers, M.H. The Pathophysiology of Gestational Diabetes Mellitus. Int. J. Mol. Sci. 2018, 19, 3342. [Google Scholar] [CrossRef]
- Zhu, Y.; Zhang, C. Prevalence of Gestational Diabetes and Risk of Progression to Type 2 Diabetes: A Global Perspective. Curr. Diabetes Rep. 2016, 16, 7. [Google Scholar] [CrossRef]
- Saravanan, P.; Magee, L.A.; Banerjee, A.; Coleman, M.A.; Von Dadelszen, P.; Denison, F.; Farmer, A.; Finer, S.; Fox-Rushby, J.; Holt, R.; et al. Gestational diabetes: Opportunities for improving maternal and child health. Lancet Diabetes Endocrinol. 2020, 8, 793–800. [Google Scholar] [CrossRef] [PubMed]
- Garrison, A. Screening, diagnosis, and management of gestational diabetes mellitus. Am. Fam. Physician 2015, 91, 460–467. [Google Scholar] [PubMed]
- Fu, J.; Retnakaran, R. The life course perspective of gestational diabetes: An opportunity for the prevention of diabetes and heart disease in women. EClinicalMedicine 2022, 45, 101294. [Google Scholar] [CrossRef] [PubMed]
- McKenzie-Sampson, S.; Paradis, G.; Healy-Profitós, J.; St-Pierre, F.; Auger, N. Gestational diabetes and risk of cardiovascular disease up to 25 years after pregnancy: A retrospective cohort study. Acta Diabetol. 2018, 55, 315–322. [Google Scholar] [CrossRef]
- Carpenter, M.W. Gestational Diabetes, Pregnancy Hypertension, and Late Vascular Disease. Diabetes Care 2007, 30 (Suppl. 2), S246–S250. [Google Scholar] [CrossRef]
- Kornacki, J.; Gutaj, P.; Kalantarova, A.; Sibiak, R.; Jankowski, M.; Wender-Ozegowska, E. Endothelial Dysfunction in Pregnancy Complications. Biomedicines 2021, 9, 1756. [Google Scholar] [CrossRef]
- Hynynen, M.M.; Khalil, R.A. The vascular endothelin system in hypertension--recent patents and discoveries. Recent. Pat. Cardiovasc. Drug Discov. 2006, 1, 95–108. [Google Scholar] [CrossRef]
- Arai, H.; Hori, S.; Aramori, I.; Ohkubo, H.; Nakanishi, S. Cloning and expression of a cDNA encoding an endothelin receptor. Nature 1990, 348, 730–732. [Google Scholar] [CrossRef]
- Clozel, M.; Gray, G.A.; Breu, V.; Löffler, B.M.; Osterwalder, R. The endothelin ETB receptor mediates both vasodilation and vasoconstriction in vivo. Biochem. Biophys. Res. Commun. 1992, 186, 867–873. [Google Scholar] [CrossRef] [PubMed]
- Khalil, R.A. Modulators of the vascular endothelin receptor in blood pressure regulation and hypertension. Curr. Mol. Pharmacol. 2011, 4, 176–186. [Google Scholar] [CrossRef] [PubMed]
- Fukuroda, T.; Ozaki, S.; Ihara, M.; Ishikawa, K.; Yano, M.; Nishikibe, M. Synergistic inhibition by BQ-123 and BQ-788 of endothelin-1-induced contractions of the rabbit pulmonary artery. Br. J. Pharmacol. 1994, 113, 336–338. [Google Scholar] [CrossRef] [PubMed]
- Kowalczyk, A.; Kleniewska, P.; Kolodziejczyk, M.; Skibska, B.; Goraca, A. The role of endothelin-1 and endothelin receptor antagonists in inflammatory response and sepsis. Arch. Immunol. Ther. Exp. 2015, 63, 41–52. [Google Scholar] [CrossRef]
- Pantham, P.; Aye, I.L.; Powell, T.L. Inflammation in maternal obesity and gestational diabetes mellitus. Placenta 2015, 36, 709–715. [Google Scholar] [CrossRef]
- Lygnos, M.C.; Pappa, K.I.; Papadaki, H.A.; Relakis, C.; Koumantakis, E.; Anagnou, N.P.; Eliopoulos, G.D. Changes in maternal plasma levels of VEGF, bFGF, TGF-beta1, ET-1 and sKL during uncomplicated pregnancy, hypertensive pregnancy and gestational diabetes. In Vivo 2006, 20, 157–163. [Google Scholar] [PubMed]
- Wolff, K.; Carlstrom, K.; Fyhrquist, F.; Hemsén, A.; Lunell, N.O.; Nisell, H. Plasma endothelin in normal and diabetic pregnancy. Diabetes Care 1997, 20, 653–656. [Google Scholar] [CrossRef] [PubMed]
- Telejko, B.; Zonenberg, A.; Kuzmicki, M.; Modzelewska, A.; Niedziolko-Bagniuk, K.; Ponurkiewicz, A.; Nikolajuk, A.; Gorska, M. Circulating asymmetric dimethylarginine, endothelin-1 and cell adhesion molecules in women with gestational diabetes. Acta Diabetol. 2009, 46, 303–308. [Google Scholar] [CrossRef]
- Hoffman, L.; Nolan, C.; Wilson, J.D.; Oats, J.J.; Simmons, D. Gestational diabetes mellitus—Management guidelines. The Australasian Diabetes in Pregnancy Society. Med. J. Aust. 1998, 169, 93–97. [Google Scholar] [CrossRef]
- Fato, B.R.; de Alwis, N.; Beard, S.; Binder, N.K.; Pritchard, N.; Tong, S.; Kaitu’u-Lino, T.J.; Hannan, N.J. Serum Collected from Preeclamptic Pregnancies Drives Vasoconstriction of Human Omental Arteries-A Novel Ex Vivo Model of Preeclampsia for Therapeutic Development. Int. J. Mol. Sci. 2022, 23, 10852. [Google Scholar] [CrossRef]
- de Alwis, N.; Fato, B.R.; Beard, S.; Binder, N.K.; Kaitu’u-Lino, T.u.J.; Onda, K.; Hannan, N.J. Assessment of the Proton Pump Inhibitor, Esomeprazole Magnesium Hydrate and Trihydrate, on Pathophysiological Markers of Preeclampsia in Preclinical Human Models of Disease. Int. J. Mol. Sci. 2022, 23, 9533. [Google Scholar] [CrossRef] [PubMed]
- Onda, K.; Tong, S.; Beard, S.; Binder, N.; Muto, M.; Senadheera, S.N.; Parry, L.; Dilworth, M.; Renshall, L.; Brownfoot, F.; et al. Proton Pump Inhibitors Decrease Soluble fms-Like Tyrosine Kinase-1 and Soluble Endoglin Secretion, Decrease Hypertension, and Rescue Endothelial Dysfunction. Hypertension 2017, 69, 457–468. [Google Scholar] [CrossRef]
- Tong, S.; Kaitu’u-Lino, T.U.J.; Onda, K.; Beard, S.; Hastie, R.; Binder, N.K.; Cluver, C.; Tuohey, L.; Whitehead, C.; Brownfoot, F.; et al. Heme Oxygenase-1 Is Not Decreased in Preeclamptic Placenta and Does Not Negatively Regulate Placental Soluble fms-Like Tyrosine Kinase-1 or Soluble Endoglin Secretion. Hypertension 2015, 66, 1073–1081. [Google Scholar] [CrossRef] [PubMed]
- Sena, C.M.; Pereira, A.M.; Seiça, R. Endothelial dysfunction—A major mediator of diabetic vascular disease. Biochim. Biophys. Acta (BBA) Mol. Basis Dis. 2013, 1832, 2216–2231. [Google Scholar] [CrossRef] [PubMed]
- Göbl, C.S.; Bozkurt, L.; Yarragudi, R.; Prikoszovich, T.; Tura, A.; Pacini, G.; Koppensteiner, R.; Kautzky-Willer, A. Biomarkers of endothelial dysfunction in relation to impaired carbohydrate metabolism following pregnancy with gestational diabetes mellitus. Cardiovasc. Diabetol. 2014, 13, 138. [Google Scholar] [CrossRef] [PubMed]
- Mordwinkin, N.M.; Ouzounian, J.G.; Yedigarova, L.; Montoro, M.N.; Louie, S.G.; Rodgers, K.E. Alteration of endothelial function markers in women with gestational diabetes and their fetuses. J. Matern. Fetal Neonatal Med. 2013, 26, 507–512. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, K.; George, T.P.; Nawaz, S.S.; Joy, S.S. VCAM-1, ICAM-1 and selectins in gestational diabetes mellitus and the risk for vascular disorders. Future Cardiol. 2019, 15, 339–346. [Google Scholar] [CrossRef]
- Gungor, O.; Gazi, E.; Ozkececi, G.; Cakir Gungor, A.N.; Cevizci, S.; Hacivelioglu, S.; Temiz, A.; Mert, N.; Koken, G. Is abnormal glucose metabolism during pregnancy related to endothelial dysfunction? J. Matern. Fetal Neonatal Med. 2015, 28, 182–185. [Google Scholar] [CrossRef]
- Lan, Q.; Zhou, Y.; Zhang, J.; Qi, L.; Dong, Y.; Zhou, H.; Li, Y. Vascular endothelial dysfunction in gestational diabetes mellitus. Steroids 2022, 184, 108993. [Google Scholar] [CrossRef]
- Al-Ofi, E.; Alrafiah, A.; Maidi, S.; Almaghrabi, S.; Hakami, N. Altered Expression of Angiogenic Biomarkers in Pregnancy Associated with Gestational Diabetes. Int. J. Gen. Med. 2021, 14, 3367–3375. [Google Scholar] [CrossRef]
- LaMarca, B.B.D.; Cockrell, K.; Sullivan, E.; Bennett, W.; Granger, J.P. Role of Endothelin in Mediating Tumor Necrosis Factor-Induced Hypertension in Pregnant Rats. Hypertension 2005, 46, 82–86. [Google Scholar] [CrossRef] [PubMed]
- Baksu, B.; Davas, I.; Baksu, A.; Akyol, A.; Gulbaba, G. Plasma nitric oxide, endothelin-1 and urinary nitric oxide and cyclic guanosine monophosphate levels in hypertensive pregnant women. Int. J. Gynecol. Obstet. 2005, 90, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.-P.; Hasan, A.A.; Zeng, S.; Hocher, B. Plasma ET-1 Concentrations Are Elevated in Pregnant Women with Hypertension -Meta-Analysis of Clinical Studies. Kidney Blood Press. Res. 2017, 42, 654–663. [Google Scholar] [CrossRef] [PubMed]
- Lappas, M. Markers of endothelial cell dysfunction are increased in human omental adipose tissue from women with pre-existing maternal obesity and gestational diabetes. Metabolism 2014, 63, 860–873. [Google Scholar] [CrossRef]
- Swiderski, S.; Celewicz, Z.; Miazgowski, T.; Ogonowski, J. Maternal endothelin-1 and cyclic guanosine monophosphate concentrations in pregnancies complicated by pregravid and gestational diabetes mellitus. Gynecol. Obstet. Investig. 2010, 69, 46–50. [Google Scholar] [CrossRef]
- Knock, G.A.; McCarthy, A.L.; Lowy, C.; Poston, L. Association of gestational diabetes with abnormal maternal vascular endothelial function. Br. J. Obstet. Gynaecol. 1997, 104, 229–234. [Google Scholar] [CrossRef]
- Chirayath, H.H.; Wareing, M.; Taggart, M.J.; Baker, P.N. Endothelial dysfunction in myometrial arteries of women with gestational diabetes. Diabetes Res. Clin. Pract. 2010, 89, 134–140. [Google Scholar] [CrossRef]
- Markos, F.; Shortt, C.M.; Edge, D.; Ruane-O’Hora, T.; Noble, M.I. Immediate direct peripheral vasoconstriction in response to hyperinsulinemia and metformin in the anesthetized pig. Physiol. Res. 2014, 63, 559–566. [Google Scholar] [CrossRef]
- Kalani, M. The importance of endothelin-1 for microvascular dysfunction in diabetes. Vasc. Health Risk Manag. 2008, 4, 1061–1068. [Google Scholar] [CrossRef]
- Worm, J. Insulin and insulin-like growth factor-1 inhibit release of endothelin-1 from mouse micro-vascular endothelial cells. Atherosclerosis 2014, 235, e96–e97. [Google Scholar] [CrossRef]
- McNally, P.G.; Lawrence, I.G.; Watt, P.A.; Hillier, C.; Burden, A.C.; Thurston, H. The effect of insulin on the vascular reactivity of isolated resistance arteries taken from healthy volunteers. Diabetologia 1995, 38, 467–473. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Muñoz, G.; Martín, R.S.; Farías, M.; Cea, L.; Vecchiola, A.; Casanello, P.; Sobrevia, L. Insulin restores glucose inhibition of adenosine transport by increasing the expression and activity of the equilibrative nucleoside transporter 2 in human umbilical vein endothelium. J. Cell. Physiol. 2006, 209, 826–835. [Google Scholar] [CrossRef] [PubMed]
- Westermeier, F.; Salomón, C.; González, M.; Puebla, C.; Guzmán-Gutiérrez, E.; Cifuentes, F.; Leiva, A.; Casanello, P.; Sobrevia, L. Insulin restores gestational diabetes mellitus-reduced adenosine transport involving differential expression of insulin receptor isoforms in human umbilical vein endothelium. Diabetes 2011, 60, 1677–1687. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Reed, L.C.; Estrada, S.M.; Walton, R.B.; Napolitano, P.G.; Ieronimakis, N. Evaluating maternal hyperglycemic exposure and fetal placental arterial dysfunction in a dual cotyledon, dual perfusion model. Placenta 2018, 69, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-L.; Rosa, R.H., Jr.; Kuo, L.; Hein, T.W. Hyperglycemia Augments Endothelin-1–Induced Constriction of Human Retinal Venules. Transl. Vis. Sci. Technol. 2020, 9, 1. [Google Scholar] [CrossRef]
- Zhou, J.; Ni, X.; Huang, X.; Yao, J.; He, Q.; Wang, K.; Duan, T. Potential Role of Hyperglycemia in Fetoplacental Endothelial Dysfunction in Gestational Diabetes Mellitus. Cell Physiol. Biochem. 2016, 39, 1317–1328. [Google Scholar] [CrossRef]


| Control | GDM Diet | p Value | GDM Insulin | p Value | |
|---|---|---|---|---|---|
| n | 42 | 12 | 13 | ||
| Body Mass Index (BMI) (median [IQR]) | 25.86 [22.45, 29.38] | 29.41 [25.05, 32.15] | 0.120 | 31.23 [25.3, 38.3] | 0.009 |
| Gestation at delivery (median [IQR]) | 39.59 [39.00, 40.43] | 37.70 [38.04, 38.93] | <0.001 | 38.54 [38.14, 39] | 0.049 |
| Highest Systolic Blood Pressure during admission (mmHg) (median [IQR]) | 118.21 [110.00, 120.00] | 120.83 [113.75, 126.25] | 0.594 | 121.92 [115.00, 125.00] | 0.339 |
| Highest Diastolic Blood Pressure during admission (mmHg) (median [IQR]) | 72.21 [70.00, 78.75] | 76.25 [70.00, 80.00] | 0.187 | 75.77 [70.00, 80.00] | 0.247 |
| Birthweight (mean (SD)) | 3474.62 (661.33) | 3361.92 (724.49) | 0.829 | 3807.85 (451) | 0.196 |
| Parity (%) | 0.019 | 0.308 | |||
| 0 | 14 (33.3) | 4 (33.4) | 3 (23.1) | ||
| 1 | 24 (57.1) | 6 (50) | 4 (30.8) | ||
| 2 | 4 (9.6) | 1 (8.3) | 5 (38.4) | ||
| 3 | 0 (0) | 1 (8.3) | 1 (7.7) | ||
| Fetal sex (%) | 0.513 | >0.999 | |||
| Female | 18 (32.9) | 7 (58.3) | 5 (38.5) | ||
| Male | 24 (57.1) | 5 (41.7) | 8 (61.5) |
| Control | GDM Diet | p Value | GDM Insulin | p Value | |
|---|---|---|---|---|---|
| n | 36 | 9 | 21 | ||
| Body Mass Index (BMI) (median [IQR]) | 23.38 [21.79, 29.48] | 29.29 [27.35, 32.56] | 0.025 | 27.54 [26.25, 32.89] | 0.019 |
| Gestation at delivery (median [IQR]) | 39.00 [38.50, 39.10] | 38.60 [38.50, 39.00] | 0.605 | 38.60 [38.20, 39.00] | 0.046 |
| Highest Systolic Blood Pressure during admission (mmHg) (median [IQR]) | 120.00 [120.00, 130.00] | 120.00 [120.00, 125.00] | 0.965 | 125.00 [120.00, 130.00] | 0.125 |
| Highest Diastolic Blood Pressure during admission (mmHg) (median [IQR]) | 75.00 [70.00, 80.00] | 75.00 [70.00, 75.00] | 0.895 | 75.00 [75.00, 80.00] | 0.198 |
| Birthweight (mean (SD)) | 3527.17 (407.89) | 3676.67 (271.11) | 0.305 | 3681.57 (683.76) | 0.289 |
| Parity (%) | 0.154 | 0.512 | |||
| 1 | 5 (14.3) | 0 (0.0) | 2 (9.5) | ||
| 2 | 21 (60.0) | 6 (66.7) | 11 (52.4) | ||
| 3 | 9 (25.7) | 2 (22.2) | 7 (33.3) | ||
| 4 | 0 (0.0) | 1 (11.1) | 1 (4.8) | ||
| Fasting Glucose (median (SD)) | 4.40 (0.38) | 4.90 (0.58) | 0.005 | 5.20 (0.48) | <0.001 |
| Glucose Tolerance Test; 1 h (mean (SD)) | 7.19 (1.26) | 10.52 (1.12) | <0.001 | 10.47 (2.22) | <0.001 |
| Glucose Tolerance Test; 2 h (mean (SD)) | 5.98 (1.13) | 7.87 (2.41) | 0.001 | 8.18 (2.14) | <0.001 |
| Fetal sex (%) | 0.941 | 0.654 | |||
| Female | 19 (52.8) | 4 (44.4) | 9 (42.9) | ||
| Male | 17 (47.2) | 5 (55.6) | 12 (57.1) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fato, B.R.; Beard, S.; Binder, N.K.; Pritchard, N.; Kaitu’u-Lino, T.J.; de Alwis, N.; Hannan, N.J. The Regulation of Endothelin-1 in Pregnancies Complicated by Gestational Diabetes: Uncovering the Vascular Effects of Insulin. Biomedicines 2023, 11, 2660. https://doi.org/10.3390/biomedicines11102660
Fato BR, Beard S, Binder NK, Pritchard N, Kaitu’u-Lino TJ, de Alwis N, Hannan NJ. The Regulation of Endothelin-1 in Pregnancies Complicated by Gestational Diabetes: Uncovering the Vascular Effects of Insulin. Biomedicines. 2023; 11(10):2660. https://doi.org/10.3390/biomedicines11102660
Chicago/Turabian StyleFato, Bianca R., Sally Beard, Natalie K. Binder, Natasha Pritchard, Tu’uhevaha J. Kaitu’u-Lino, Natasha de Alwis, and Natalie J. Hannan. 2023. "The Regulation of Endothelin-1 in Pregnancies Complicated by Gestational Diabetes: Uncovering the Vascular Effects of Insulin" Biomedicines 11, no. 10: 2660. https://doi.org/10.3390/biomedicines11102660
APA StyleFato, B. R., Beard, S., Binder, N. K., Pritchard, N., Kaitu’u-Lino, T. J., de Alwis, N., & Hannan, N. J. (2023). The Regulation of Endothelin-1 in Pregnancies Complicated by Gestational Diabetes: Uncovering the Vascular Effects of Insulin. Biomedicines, 11(10), 2660. https://doi.org/10.3390/biomedicines11102660







