The Inhibitory Potential of Ferulic Acid Derivatives against the SARS-CoV-2 Main Protease: Molecular Docking, Molecular Dynamics, and ADMET Evaluation
Abstract
1. Introduction
2. Materials and Methods
2.1. Ligand and Receptor Preparation for Docking Simulations
2.2. Molecular Docking Simulation and Data Output
2.3. Validation of the Docking Method
2.4. Visualization of Binding Modes and Mpro–Ligand Interactions
2.5. ADMET Prediction
2.6. Molecular Dynamics Simulation
3. Results and Discussion
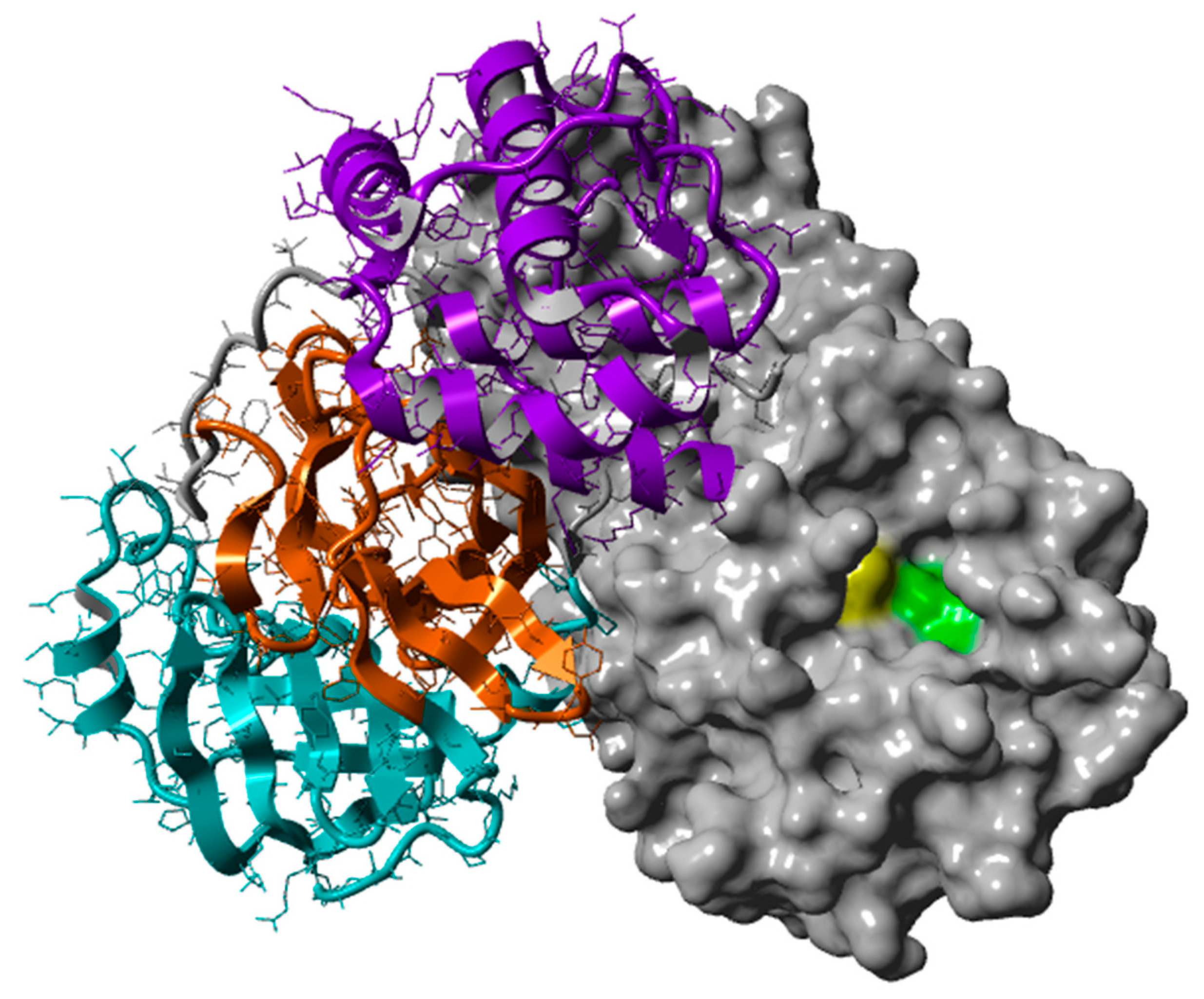
3.1. Mpro as a Receptor for Docking Simulations
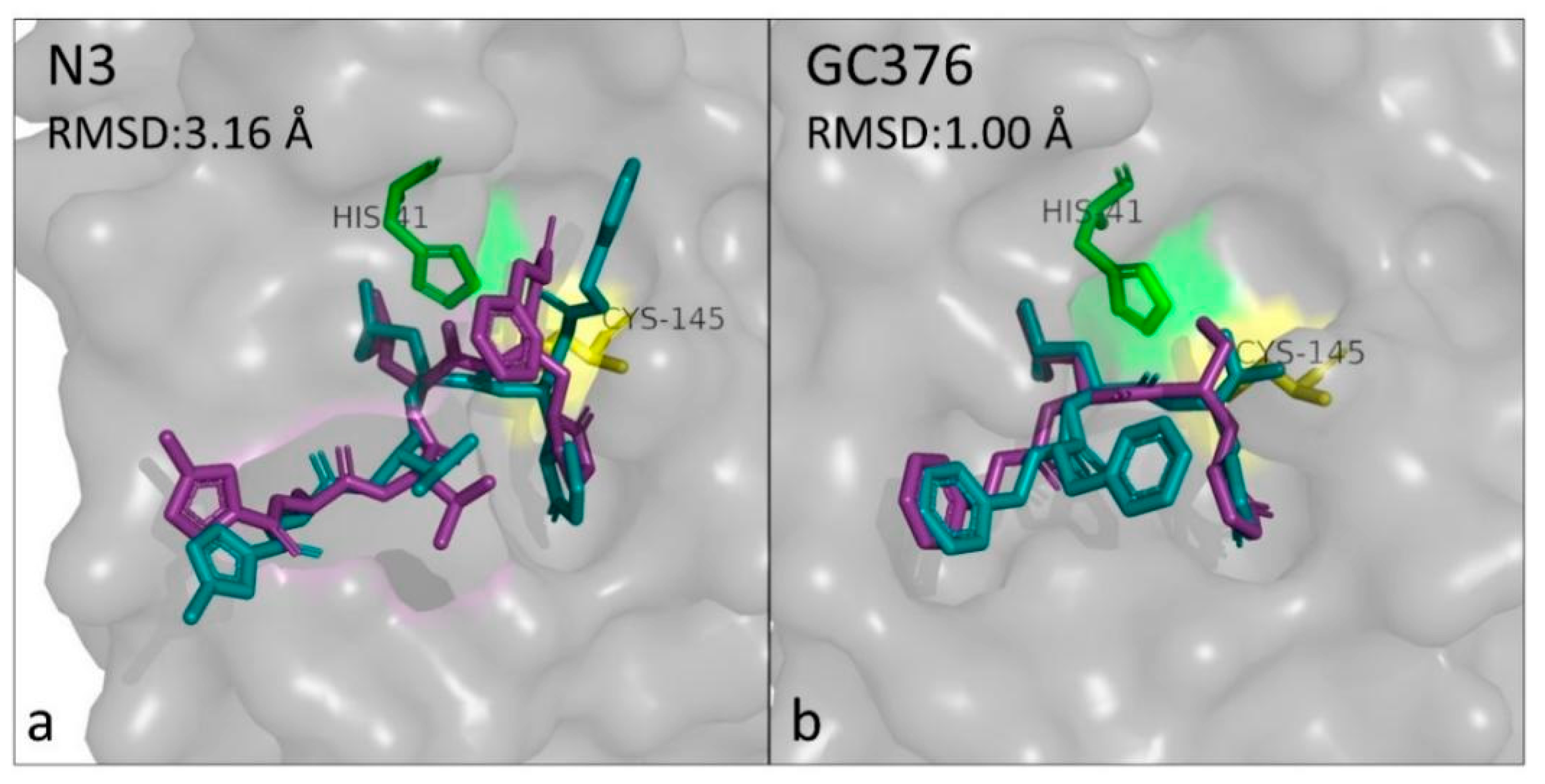
3.2. Docking Validation
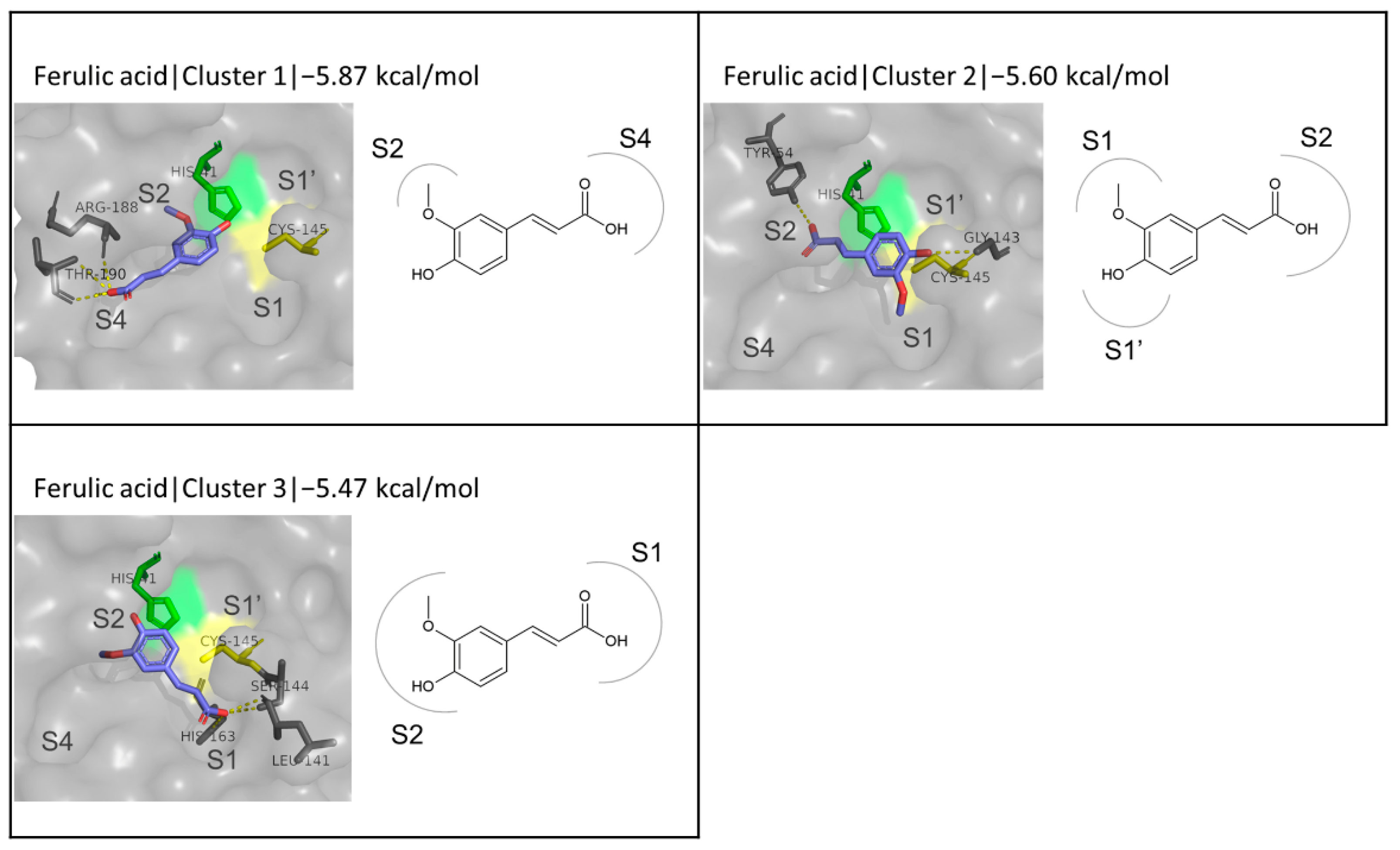
3.3. FA as a ‘Reference’ Ligand
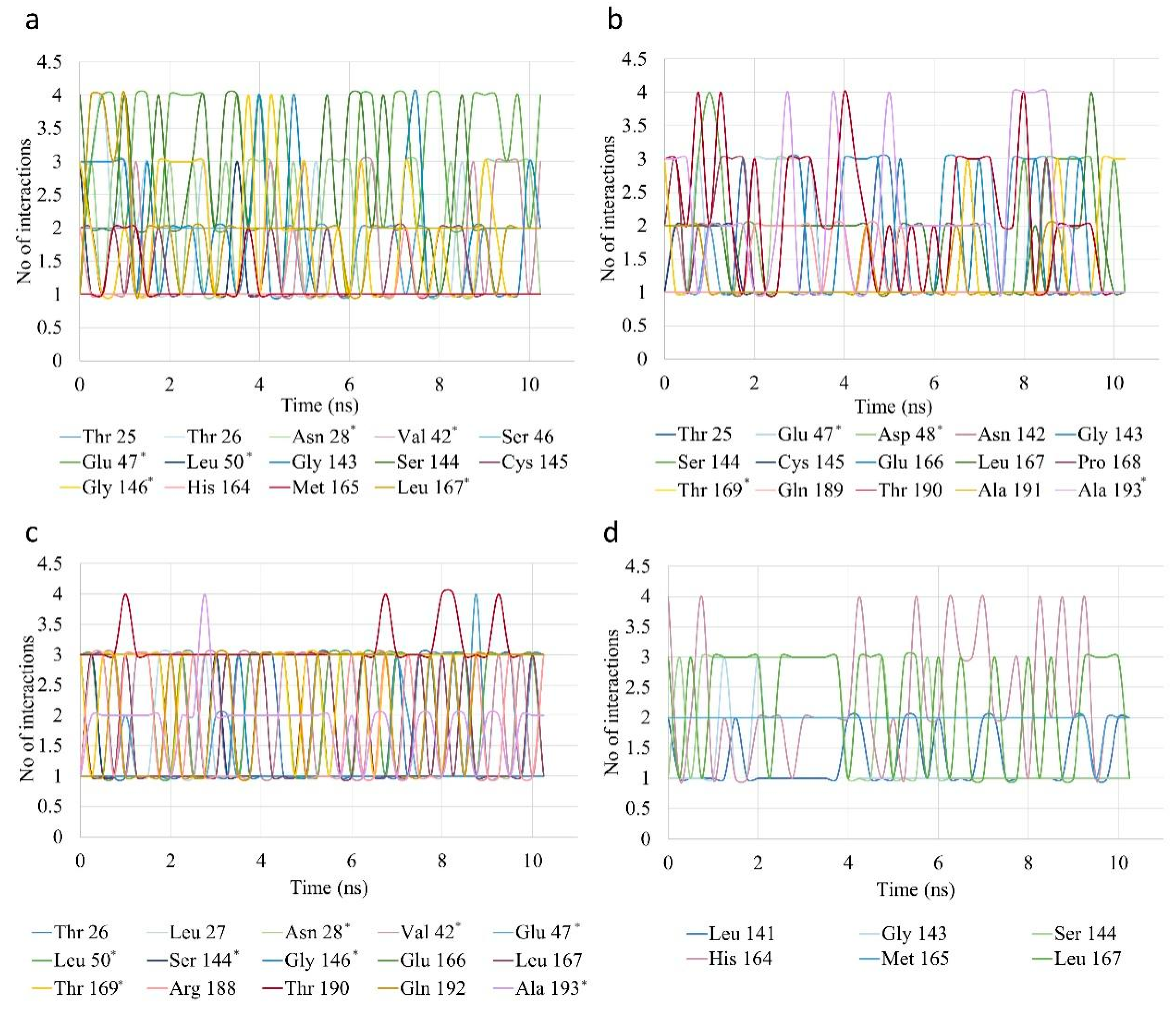
3.4. Docking of Enzymatically Synthesized FA Derivatives
3.4.1. Alkyl and Alkenyl Esters of FA
3.4.2. Fatty Esters of FA and Other Related Esters
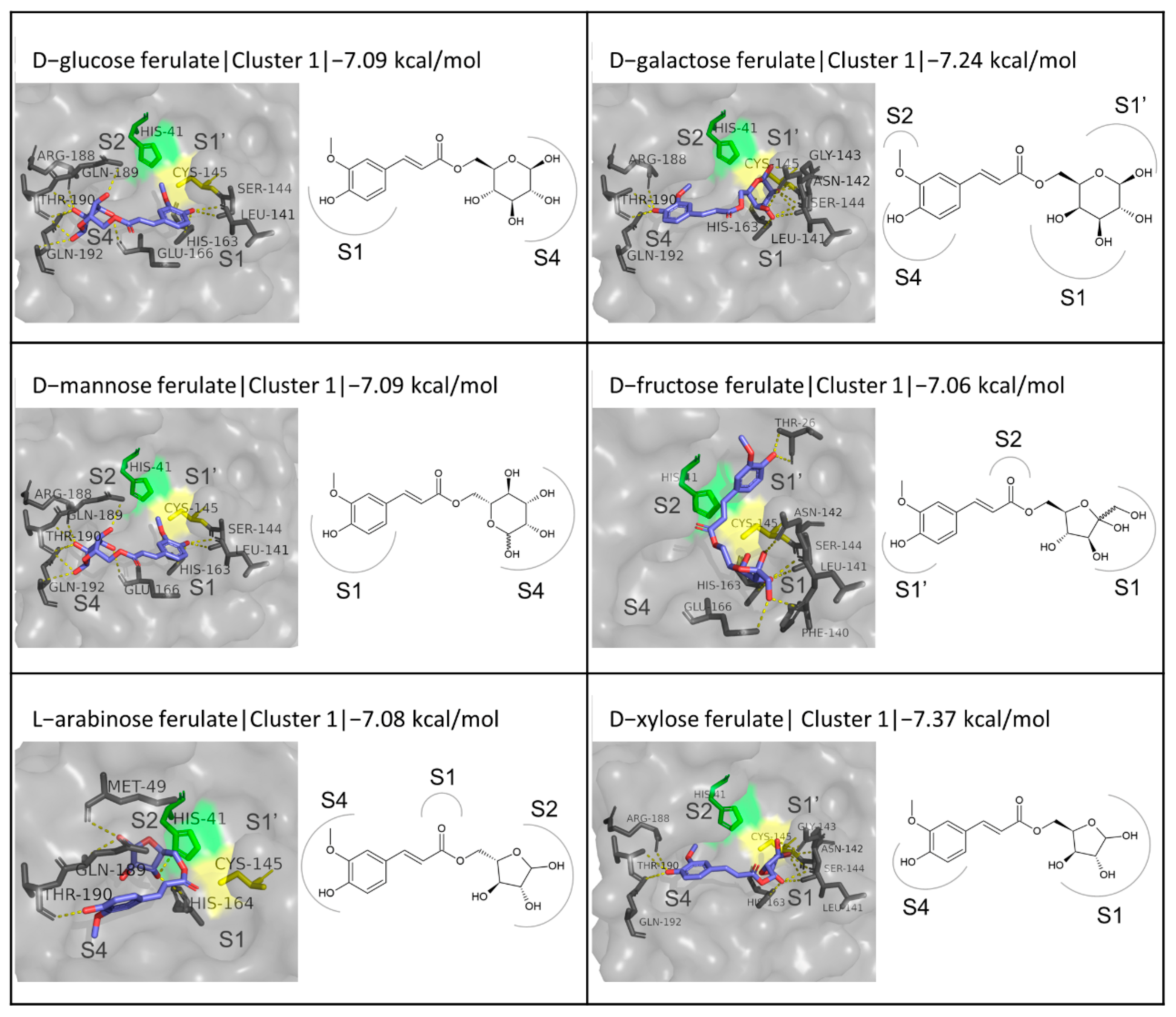
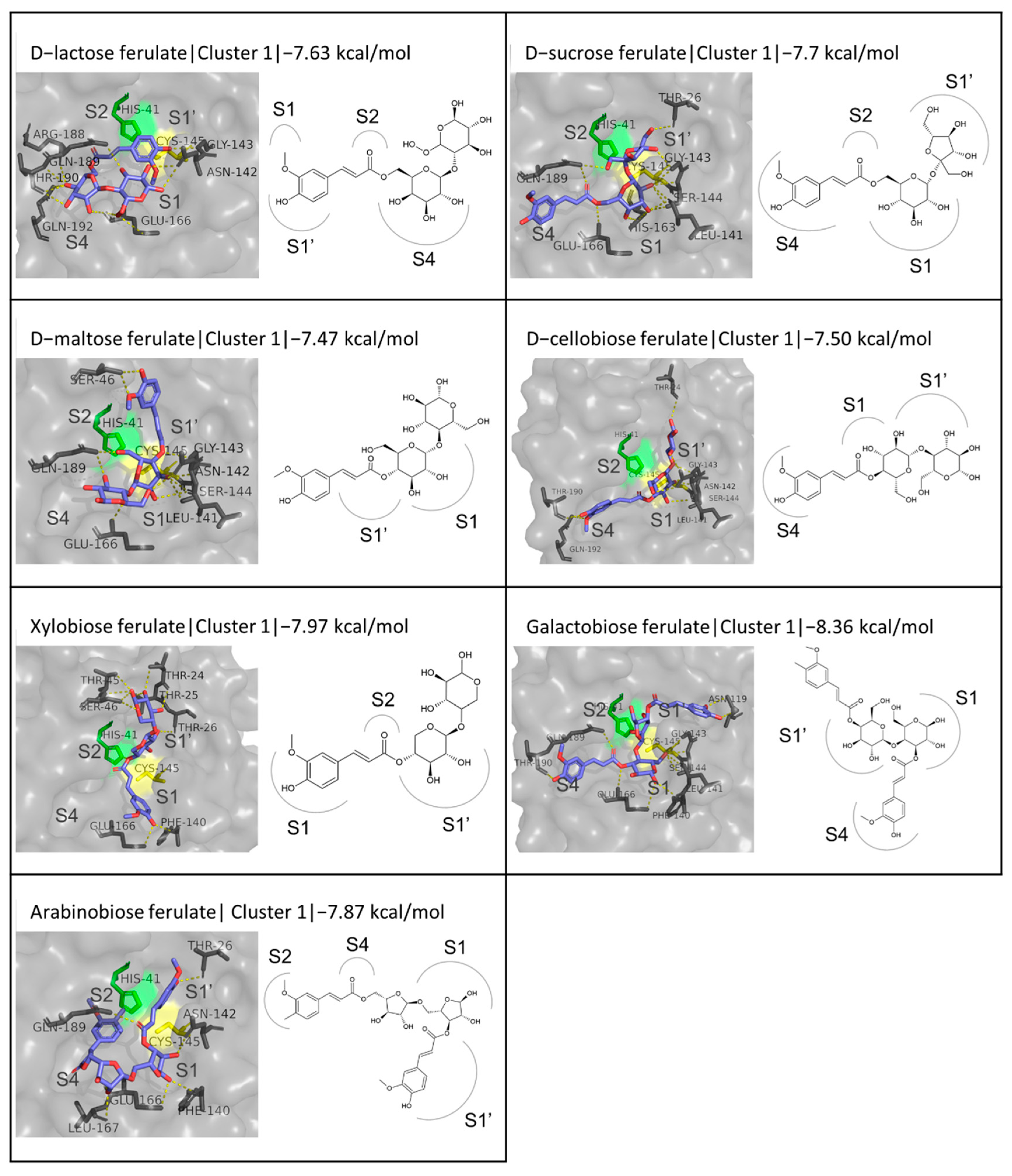
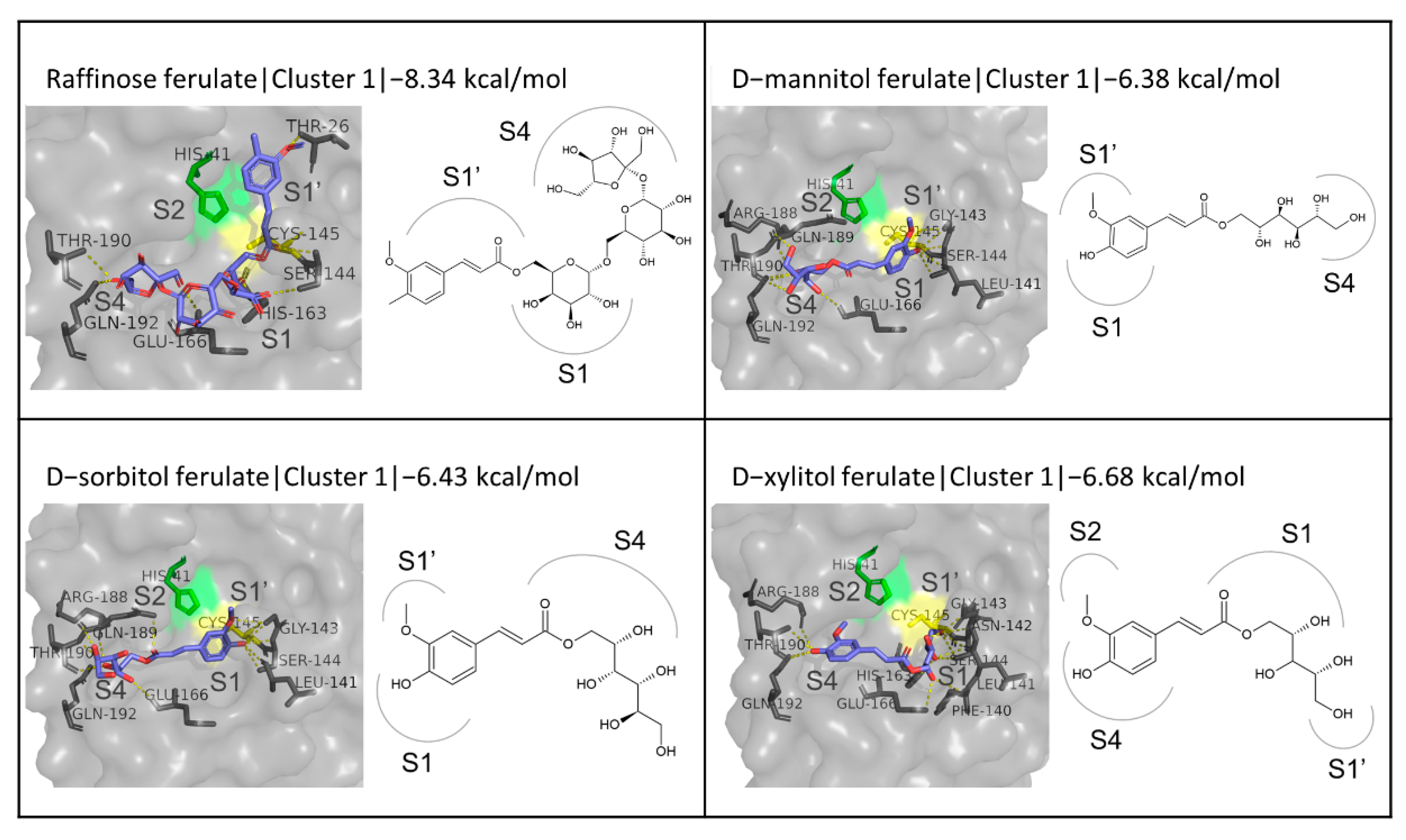
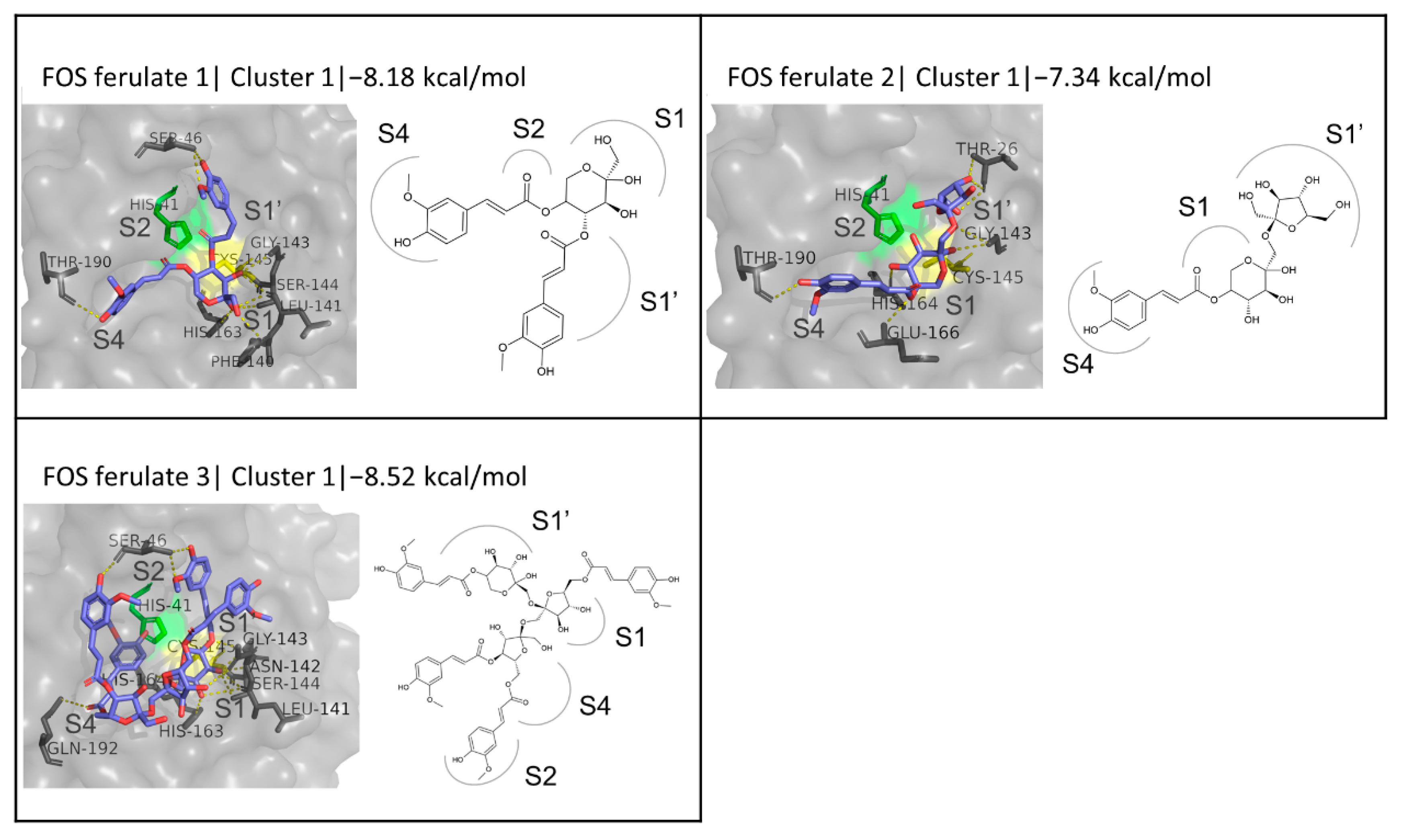
3.4.3. Sugar Esters of FA
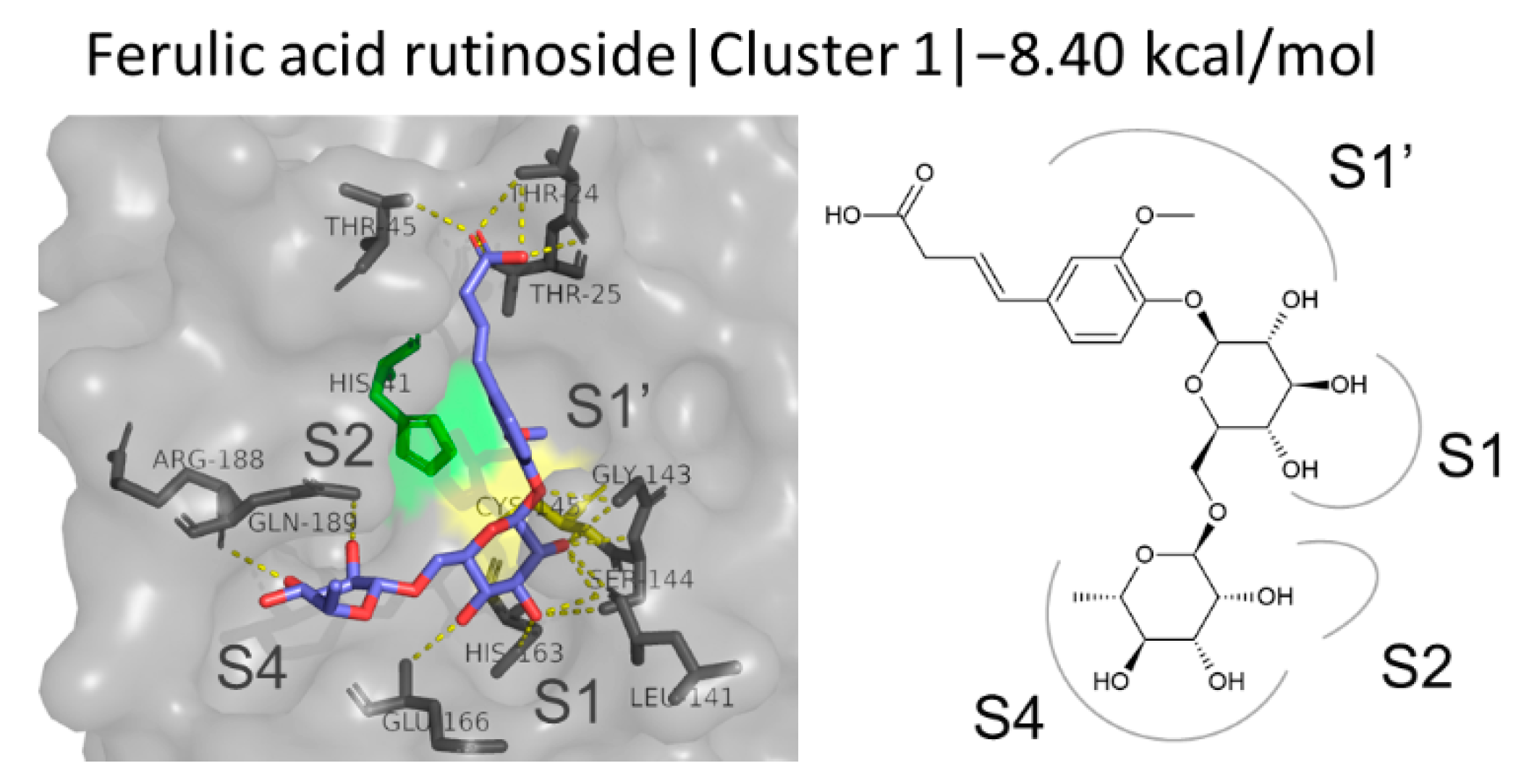
3.4.4. FA Glycosides
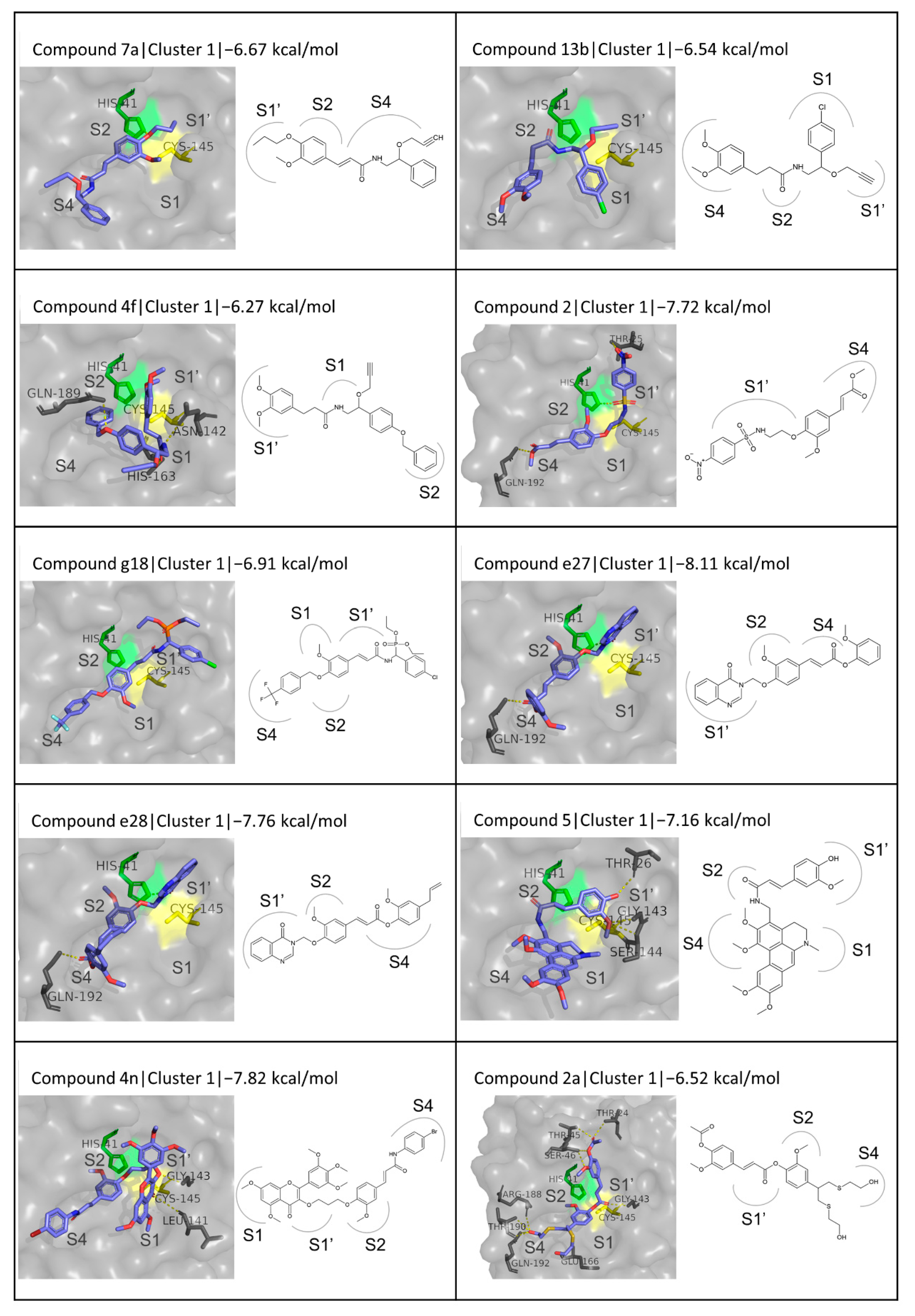
3.5. Docking of Chemically Synthesized FA Derivatives
3.6. Summary of Docking Results
3.7. ADMET Properties of the Selected FA Derivatives
3.7.1. Bioavailability and Druglikeness
3.7.2. Pharmacokinetics
3.7.3. Toxicity Profile
3.8. Summary of the ADMET Properties of the Most Promising Compounds
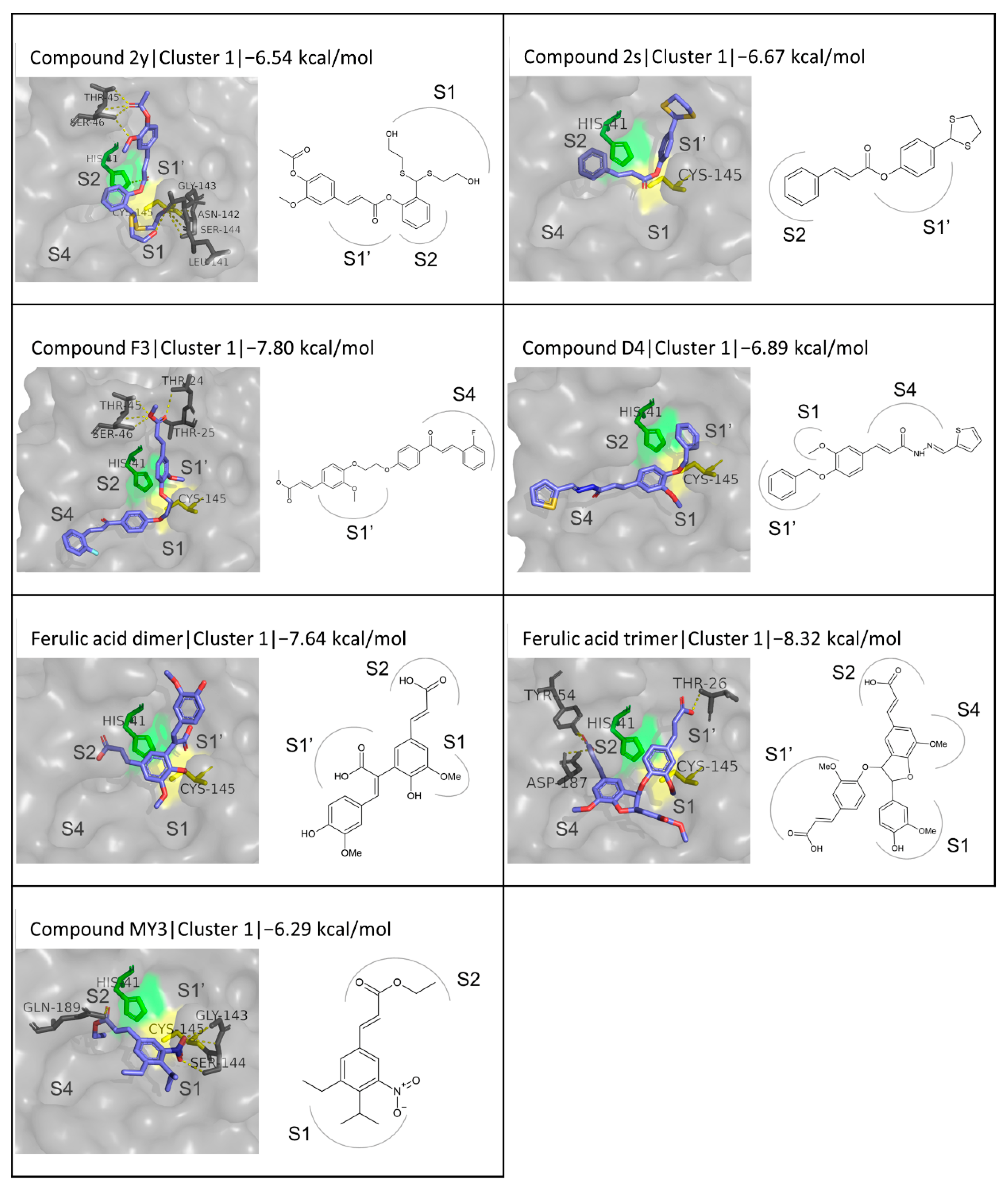
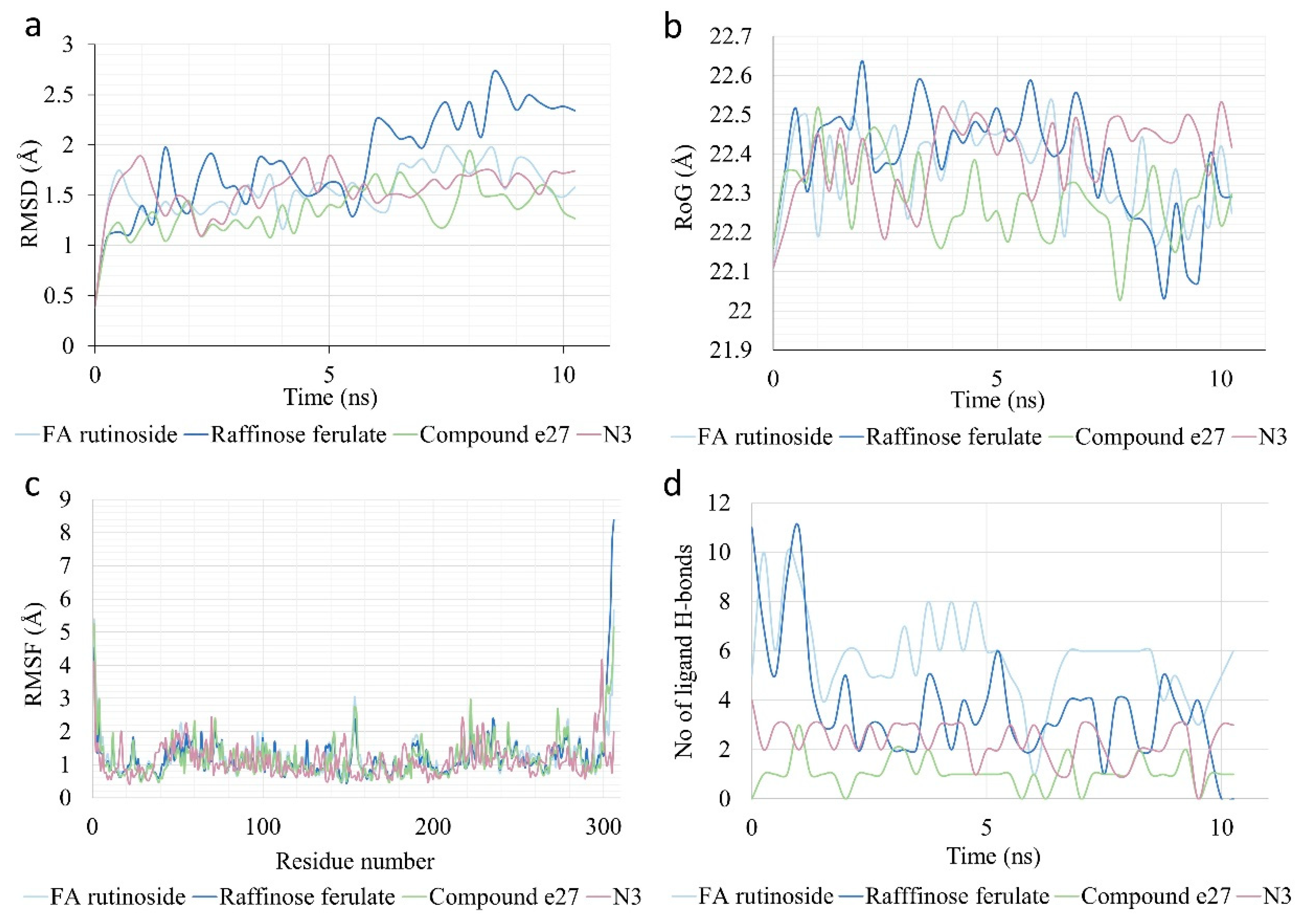
3.9. MD Simulation of Selected Derivatives
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 10 March 2022).
- Stoddard, S.V.; Stoddard, S.D.; Oelkers, B.K.; Fitts, K.; Whalum, K.; Whalum, K.; Hemphill, A.D.; Manikonda, J.; Martinez, L.M.; Riley, E.G.; et al. Optimization Rules for SARS-CoV-2 Mpro Antivirals: Ensemble Docking and Exploration of the Coronavirus Protease Active Site. Viruses 2020, 12, 942. [Google Scholar] [CrossRef]
- Tregoning, J.S.; Flight, K.E.; Higham, S.L.; Wang, Z.; Pierce, B.F. Progress of the COVID-19 Vaccine Effort: Viruses, Vaccines and Variants versus Efficacy, Effectiveness and Escape. Nat. Rev. Immunol. 2021, 21, 626–636. [Google Scholar] [CrossRef]
- Rubin, D.; Chan-Tack, K.; Farley, J.; Sherwat, A. FDA Approval of Remdesivir—A Step in the Right Direction. N. Engl. J. Med. 2020, 383, 2598–2600. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration. Emergency Use Authorization. Available online: https://www.fda.gov/emergency-preparedness-and-response/mcm-legal-regulatory-and-policy-framework/emergency-use-authorization#coviddrugs (accessed on 12 March 2022).
- European Centre for Disease Prevention and Control. SARS-CoV-2 Variants of Concern as of 11 March 2022. Available online: https://www.ecdc.europa.eu/en/COVID-19/variants-concern (accessed on 14 March 2022).
- Mohapatra, R.K.; Tiwari, R.; Sarangi, A.K.; Islam, R.; Chakraborty, C.; Dhama, K. Omicron (B.1.1.529) Variant of SARS-CoV-2: Concerns, Challenges, and Recent Updates. J. Med. Virol. 2022, 94, 2336–2342. [Google Scholar] [CrossRef]
- Sun, C.; Kang, Y.-F.; Liu, Y.-T.; Kong, X.-W.; Xu, H.-Q.; Xiong, D.; Xie, C.; Liu, Y.-H.; Peng, S.; Feng, G.-K.; et al. Parallel Profiling of Antigenicity Alteration and Immune Escape of SARS-CoV-2 Omicron and Other Variants. Signal Transduct. Target. Ther. 2022, 7, 42. [Google Scholar] [CrossRef]
- Świderek, K.; Moliner, V. Revealing the Molecular Mechanisms of Proteolysis of SARS-CoV-2 Mpro by QM/MM Computational Methods. Chem. Sci. 2020, 11, 10626–10630. [Google Scholar] [CrossRef]
- Zhang, L.; Lin, D.; Sun, X.; Curth, U.; Drosten, C.; Sauerhering, L.; Becker, S.; Rox, K.; Hilgenfeld, R. Crystal Structure of SARS-CoV-2 Main Protease Provides a Basis for Design of Improved a-Ketoamide Inhibitors. Science 2020, 368, 409–412. [Google Scholar] [CrossRef]
- Parvez, S.A.; Saha, M.K.; Araf, Y.; Islam, T.; Ohtsuki, G.; Hosen, M.J. Insights from a Computational Analysis of the SARS-CoV-2 Omicron Variant: Host-Pathogen Interaction, Pathogenicity, and Possible Therapeutics. Immun. Inflamm. Dis. 2022, 10, e639. [Google Scholar] [CrossRef]
- Nikolaidis, M.; Papakyriakou, A.; Chlichlia, K.; Markoulatos, P.; Oliver, S.G.; Amoutzias, G.D. Comparative Analysis of SARS-CoV-2 Variants of Concern, Including Omicron, Highlights Their Common and Distinctive Amino Acid Substitution Patterns, Especially at the Spike ORF. Viruses 2022, 14, 707. [Google Scholar] [CrossRef]
- Ullrich, S.; Ekanayake, K.B.; Otting, G.; Nitsche, C. Main Protease Mutants of SARS-CoV-2 Variants Remain Susceptible to Nirmatrelvir. Bioorganic Med. Chem. Lett. 2022, 62, 128629. [Google Scholar] [CrossRef]
- Yoshino, R.; Yasuo, N.; Sekijima, M. Identification of Key Interactions between SARS-CoV-2 Main Protease and Inhibitor Drug Candidates. Sci. Rep. 2020, 10, 12493. [Google Scholar] [CrossRef]
- Macdonald, E.A.; Frey, G.; Namchuk, M.N.; Harrison, S.C.; Hinshaw, S.M.; Windsor, I.W. Recognition of Divergent Viral Substrates by the SARS-CoV-2 Main Protease. Infect. Dis. 2021, 7, 2591–2595. [Google Scholar] [CrossRef]
- Lin, L.-T.; Hsu, W.-C.; Lin, C.-C. Antiviral Natural Products and Herbal Medicines. J. Tradit. Complement. Med. 2014, 4, 24–35. [Google Scholar] [CrossRef]
- Omrani, M.; Keshavarz, M.; Nejad Ebrahimi, S.; Mehrabi, M.; McGaw, L.J.; Ali Abdalla, M.; Mehrbod, P. Potential Natural Products against Respiratory Viruses: A Perspective to Develop Anti-COVID-19 Medicines. Front. Pharmacol. 2021, 11, 586993. [Google Scholar] [CrossRef]
- Antonopoulou, I.; Sapountzaki, E.; Rova, U.; Christakopoulos, P. Inhibition of the Main Protease of SARS-CoV-2 (Mpro) by Repurposing/Designing Drug-like Substances and Utilizing Nature’s Toolbox of Bioactive Compounds. Comput. Struct. Biotechnol. J. 2022, 20, 1306–1344. [Google Scholar] [CrossRef]
- Katsimpouras, C.; Antonopoulou, I.; Christakopoulos, P.; Topakas, E. Role and Applications of Feruloyl Esterases in Biomass Bioconversion. In Microbial Enzymes in Bioconversions of Biomass; Gupta, V.K., Ed.; Springer International Publishing: Cham, Switzerland, 2016; pp. 79–123. ISBN 978-3-319-43679-1. [Google Scholar]
- Stompor-Gorący, M.; Machaczka, M. Recent Advances in Biological Activity, New Formulations and Prodrugs of Ferulic Acid. Int. J. Mol. Sci. 2021, 22, 12889. [Google Scholar] [CrossRef]
- Srinivasan, M.; Sudheer, A.R.; Menon, V.P. Recent Advances in Indian Herbal Drug Research Guest Editor: Thomas Paul Asir Devasagayam Ferulic Acid: Therapeutic Potential Through Its Antioxidant Property. J. Clin. Biochem. Nutr. 2007, 40, 92–100. [Google Scholar] [CrossRef]
- Antonopoulou, I.; Sapountzaki, E.; Rova, U.; Christakopoulos, P. Ferulic Acid from Plant Biomass: A Phytochemical with Promising Antiviral Properties. Front. Nutr. 2022, 8, 777576. [Google Scholar] [CrossRef]
- Salman, S.; Shah, F.H.; Idrees, J.; Idrees, F.; Velagala, S.; Ali, J.; Khan, A.A. Virtual Screening of Immunomodulatory Medicinal Compounds as Promising Anti-SARS-CoV-2 Inhibitors. Future Virol. 2020, 15, 267–275. [Google Scholar] [CrossRef]
- Mancuso, C.; Santangelo, R. Ferulic Acid: Pharmacological and Toxicological Aspects. Food Chem. Toxicol. 2014, 65, 185–195. [Google Scholar] [CrossRef]
- Bourne, L.C.; Rice-Evans, C. Bioavailability of Ferulic Acid. Biochem. Biophys. Res. Commun. 1998, 253, 222–227. [Google Scholar] [CrossRef]
- Zhao, Z.; Moghadasian, M.H. Chemistry, Natural Sources, Dietary Intake and Pharmacokinetic Properties of Ferulic Acid: A Review. Food Chem. 2008, 109, 691–702. [Google Scholar] [CrossRef]
- Li, D.; Rui, Y.; Guo, S.; Luan, F.; Liu, R.; Zeng, N. Ferulic Acid: A Review of Its Pharmacology, Pharmacokinetics and Derivatives. Life Sci. 2021, 284, 119921. [Google Scholar] [CrossRef]
- Kumar, N.; Pruthi, V. Potential Applications of Ferulic Acid from Natural Sources. Biotechnol. Rep. 2014, 4, 86–93. [Google Scholar] [CrossRef]
- de Oliveira Silva, E.; Batista, R. Ferulic Acid and Naturally Occurring Compounds Bearing a Feruloyl Moiety: A Review on Their Structures, Occurrence, and Potential Health Benefits. Compr. Rev. Food Sci. Food Saf. 2017, 16, 580–616. [Google Scholar] [CrossRef]
- Mathew, S.; Abraham, T. Ferulic Acid: An Antioxidant Found Naturally in Plant Cell Walls and Feruloyl Esterases Involved in Its Release and Their Applications. Crit. Rev. Biotechnol. 2004, 24, 59–83. [Google Scholar] [CrossRef]
- Meryl Smith, M.; Hartley, R. Occurence and Nature of Ferulic Acid Substitution of Cell-Wall Polysacchariddes in Graminaceous Plants. Carbohydr. Res. 1983, 118, 65–80. [Google Scholar] [CrossRef]
- Huang, G.Y.; Cui, C.; Wang, Z.P.; Li, Y.Q.; Xiong, L.X.; Wang, L.Z.; Yu, S.J.; Li, Z.M.; Zhao, W.G. Synthesis and Characteristics of (Hydrogenated) Ferulic Acid Derivatives as Potential Antiviral Agents with Insecticidal Activity. Chem. Cent. J. 2013, 7, 33. [Google Scholar] [CrossRef]
- Ren, X.; Li, X.; Yin, L.; Jiang, D.; Hu, D. Design, Synthesis, Antiviral Bioactivity, and Mechanism of the Ferulic Acid Ester-Containing Sulfonamide Moiety. ACS Omega 2020, 5, 19721–19726. [Google Scholar] [CrossRef]
- Wang, Y.; He, F.; Wu, S.; Luo, Y.; Wu, R.; Hu, D.; Song, B. Design, Synthesis, Anti-TMV Activity, and Preliminary Mechanism of Cinnamic Acid Derivatives Containing Dithioacetal Moiety. Pestic. Biochem. Physiol. 2020, 164, 115–121. [Google Scholar] [CrossRef]
- Katayama, S.; Ohno, F.; Yamauchi, Y.; Kato, M.; Makabe, H.; Nakamura, S. Enzymatic Synthesis of Novel Phenol Acid Rutinosides Using Rutinase and Their Antiviral Activity in Vitro. J. Agric. Food Chem. 2013, 61, 9617–9622. [Google Scholar] [CrossRef]
- Antonopoulou, I.; Varriale, S.; Topakas, E.; Rova, U.; Christakopoulos, P.; Faraco, V. Enzymatic Synthesis of Bioactive Compounds with High Potential for Cosmeceutical Application. Appl. Microbiol. Biotechnol. 2016, 100, 6519–6543. [Google Scholar] [CrossRef]
- Krieger, E.; Vriend, G. YASARA View—Molecular Graphics for All Devices—From Smartphones to Workstations. Bioinformatics 2014, 30, 2981–2982. [Google Scholar] [CrossRef]
- Trott, O.; Olson, A.J. AutoDock Vina: Improving the Speed and Accuracy of Docking with a New Scoring Function, Efficient Optimization, and Multithreading. J. Comput. Chem. 2010, 31, 455–461. [Google Scholar] [CrossRef]
- Schrödinger, L. The PyMOL Molecular Graphics System. Version 2.4.1. Schrödinger: New York, NY, USA, 2020. [Google Scholar]
- Wallace, A.C.; Laskowski, R.A.; Thornton, J.M. LIGPLOT: A Program to Generate Schematic Diagrams of Protein-Ligand Interactions. Protein Eng. Des. Sel. 1995, 8, 127–134. [Google Scholar] [CrossRef]
- Krieger, E.; Nielsen, J.E.; Spronk, C.A.E.M.; Vriend, G. Fast Empirical PKa Prediction by Ewald Summation. J. Mol. Graph. Model. 2006, 25, 481–486. [Google Scholar] [CrossRef]
- Krieger, E.; Dunbrack, R.L.J.; Hooft, R.W.W.; Krieger, B. Assignment of Protonation States in Proteins and Ligands: Combining PKa Prediction with Hydrogen Bonding Network Optimization. Methods Mol Biol 2012, 819, 405–421. [Google Scholar] [CrossRef]
- Maier, J.A.; Martinez, C.; Kasavajhala, K.; Wickstrom, L.; Hauser, K.E.; Simmerling, C. Ff14SB: Improving the Accuracy of Protein Side Chain and Backbone Parameters from Ff99SB. J. Chem. Theory Comput. 2015, 11, 3696–3713. [Google Scholar] [CrossRef]
- Hornak, V.; Abel, R.; Okur, A.; Strockbine, B.; Roitberg, A.; Simmerling, C. Comparison of Multiple Amber Force Fields and Development of Improved Protein Backbone Parameters. Proteins 2006, 65, 712–725. [Google Scholar] [CrossRef]
- Essmann, U.; Perera, L.; Berkowitz, M.L.; Darden, T.; Lee, H.; Pedersen, L.G. A Smooth Particle Mesh Ewald Method. J. Chem. Phys. 1995, 103, 8577–8593. [Google Scholar] [CrossRef]
- Krieger, E.; Vriend, G. New Ways to Boost Molecular Dynamics Simulations. J. Comput. Chem. 2015, 36, 996–1007. [Google Scholar] [CrossRef] [PubMed]
- Koudelka, T.; Boger, J.; Henkel, A.; Schönherr, R.; Krantz, S.; Fuchs, S.; Rodríguez, E.; Redecke, L.; Tholey, A. N-Terminomics for the Identification of In Vitro Substrates and Cleavage Site Specificity of the SARS-CoV-2 Main Protease. Proteomics 2021, 21, 2000246. [Google Scholar] [CrossRef] [PubMed]
- Hegyi, A.; Ziebuhr, J. Conservation of Substrate Specificities among Coronavirus Main Proteases. J. Gen. Virol. 2002, 83, 595–599. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Worrall, L.J.; Vuckovic, M.; Rosell, F.I.; Gentile, F.; Ton, A.-T.; Caveney, N.A.; Ban, F.; Cherkasov, A.; Paetzel, M.; et al. Crystallographic Structure of Wild-Type SARS-CoV-2 Main Protease Acyl-Enzyme Intermediate with Physiological C-Terminal Autoprocessing Site. Nat. Commun. 2020, 11, 5877. [Google Scholar] [CrossRef]
- Kneller, D.W.; Phillips, G.; O’Neill, H.M.; Jedrzejczak, R.; Stols, L.; Langan, P.; Joachimiak, A.; Coates, L.; Kovalevsky, A. Structural Plasticity of SARS-CoV-2 3CL Mpro Active Site Cavity Revealed by Room Temperature X-Ray Crystallography. Nat. Commun. 2020, 11, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Jin, Z.; Du, X.; Xu, Y.; Deng, Y.; Liu, M.; Zhao, Y.; Zhang, B.; Li, X.; Zhang, L.; Peng, C.; et al. Structure of M pro from SARS-CoV-2 and Discovery of Its Inhibitors. Nature 2020, 582, 289–293. [Google Scholar] [CrossRef]
- Sacco, M.D.; Ma, C.; Lagarias, P.; Gao, A.; Townsend, J.A.; Meng, X.; Dube, P.; Zhang, X.; Hu, Y.; Kitamura, N.; et al. Structure and Inhibition of the SARS-CoV-2 Main Protease Reveals Strategy for Developing Dual Inhibitors against Mpro and Cathepsin L. bioRxiv 2020. [Google Scholar] [CrossRef]
- Kneller, D.W.; Galanie, S.; Phillips, G.; Neill, H.M.O.; Coates, L.; Kovalevsky, A.; Kneller, D.W.; Galanie, S.; Phillips, G.; Neill, H.M.O.; et al. Malleability of the SARS-CoV-2 3CL Mpro Active-Site Cavity Facilitates Binding of Clinical Antivirals. Struct./Fold. Des. 2020, 28, 1313–1320.e3. [Google Scholar] [CrossRef]
- Bharadwaj, S.; Azhar, E.I.; Kamal, M.A.; Bajrai, H.; Dubey, A.; Jha, K.; Yadava, U.; Kang, S.G. SARS-CoV-2 M Inhibitors : Identification of Anti- SARS-CoV-2 M Compounds from FDA Approved Drugs. J. Biomol. Struct. Dyn. 2022, 40, 2769–2784. [Google Scholar] [CrossRef]
- Arafet, K.; Serrano-Aparicio, N.; Lodola, A.; Mulholland, A.J.; González, F.V.; Świderek, K.; Moliner, V. Mechanism of Inhibition of SARS-CoV-2 Mpro by N3 peptidyl Michael Acceptor Explained by QM/MM Simulations and Design of New Derivatives with Tunable Chemical Reactivity. Chem. Sci. 2021, 12, 1433–1444. [Google Scholar] [CrossRef]
- Das, P.; Majumder, R.; Mandal, M.; Basak, P. In-Silico Approach for Identification of Effective and Stable Inhibitors for COVID-19 Main Protease (Mpro) from Flavonoid Based Phytochemical Constituents of Calendula Officinalis. J. Biomol. Struct. Dyn. 2021, 39, 6265–6280. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Id, C.; Merzouk, H.; Mokhtari-Soulimane, N. Potential Bioactive Glycosylated Flavonoids as SARS-CoV-2 Main Protease Inhibitors: A Molecular Docking and Simulation Studies. PLoS ONE 2020, 15, e0240653. [Google Scholar] [CrossRef]
- Hu, Y.; Ma, C.; Szeto, T.; Hurst, B.; Tarbet, B.; Wang, J. Boceprevir, Calpain Inhibitors II and XII, and GC-376 Have Broad-Spectrum Antiviral Activity against Coronaviruses. ACS Infect. Dis. 2021, 7, 586–597. [Google Scholar] [CrossRef] [PubMed]
- Rakib, A.; Nain, Z.; Sami, S.A.; Mahmud, S.; Islam, A.; Ahmed, S.; Siddiqui, A.B.F.; Babu, S.M.O.F.; Hossain, P.; Shahriar, A.; et al. A Molecular Modelling Approach for Identifying Antiviral Selenium-Containing Heterocyclic Compounds That Inhibit the Main Protease of SARS-CoV-2: An in Silico Investigation. Brief. Bioinform. 2021, 22, 1476–1498. [Google Scholar] [CrossRef]
- Allam, A.E.; Amen, Y.; Ashour, A.; Assaf, H.K.; Hassan, H.A.; Abdel-Rahman, I.M.; Sayed, A.M.; Shimizu, K. In Silico Study of Natural Compounds from Sesame against COVID-19 by Targeting Mpro, PLpro and RdRp. RSC Adv. 2021, 11, 22398–22408. [Google Scholar] [CrossRef]
- El Gizawy, H.A.; Boshra, S.A.; Mostafa, A.; Mahmoud, S.H.; Ismail, M.I.; Alsfouk, A.A.; Taher, A.T.; Al-Karmalawy, A.A. Pimenta dioica (L.) Merr. Bioactive Constituents Exert Anti-SARS-CoV-2 and Anti-Inflammatory Activities: Molecular Docking and Dynamics, In Vitro, and In Vivo Studies. Molecules 2021, 26, 5844. [Google Scholar] [CrossRef]
- Saeed, A.; Ahmad, B.; Majaz, S.; Nouroz, F.; Ahmad, A.; Xie, Y. Targeting Omicron and Other Reported SARS-CoV-2 Lineages by Potent Inhibitors of Main Protease 3CL Mpro: Molecular Simulation Analysis. J. Infect. 2022, 84, e133–e136. [Google Scholar] [CrossRef]
- Joshi, T.; Bhat, S.; Pundir, H.; Chandra, S. Identification of Berbamine, Oxyacanthine and Rutin from Berberis Asiatica as Anti-SARS-CoV-2 Compounds: An in Silico Study. J. Mol. Graph. Model. 2021, 109, 108028. [Google Scholar] [CrossRef]
- Oliveira, D.M.; Mota, T.R.; Oliva, B.; Segato, F.; Marchiosi, R.; Ferrarese-Filho, O.; Faulds, C.B.; dos Santos, W.D. Feruloyl Esterases: Biocatalysts to Overcome Biomass Recalcitrance and for the Production of Bioactive Compounds. Bioresour. Technol. 2019, 278, 408–423. [Google Scholar] [CrossRef]
- Grajales-Hernández, D.A.; Armendáriz-Ruiz, M.A.; Gallego, F.L.; Mateos-Díaz, J.C. Approaches for the Enzymatic Synthesis of Alkyl Hydroxycinnamates and Applications Thereof. Appl. Microbiol. Biotechnol. 2021, 105, 3901–3917. [Google Scholar] [CrossRef]
- Cerullo, G.; Varriale, S.; Bozonnet, S.; Antonopoulou, I.; Christakopoulos, P.; Rova, U.; Gherbovet, O.; Fauré, R.; Piechot, A.; Jütten, P.; et al. Directed Evolution of the Type C Feruloyl Esterase from Fusarium Oxysporum FoFaeC and Molecular Docking Analysis of Its Improved Variants. New Biotechnol. 2019, 51, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Karnaouri, A.; Antonopoulou, I.; Zerva, A.; Dimarogona, M.; Topakas, E.; Rova, U.; Christakopoulos, P. Thermophilic Enzyme Systems for Efficient Conversion of Lignocellulose to Valuable Products: Structural Insights and Future Perspectives for Esterases and Oxidative Catalysts. Bioresour. Technol. 2019, 279, 362–372. [Google Scholar] [CrossRef] [PubMed]
- Hunt, C.J.; Antonopoulou, I.; Tanksale, A.; Rova, U.; Christakopoulos, P.; Haritos, V.S. Insights into Substrate Binding of Ferulic Acid Esterases by Arabinose and Methyl Hydroxycinnamate Esters and Molecular Docking. Sci. Rep. 2017, 7, 17315. [Google Scholar] [CrossRef] [PubMed]
- Antonopoulou, I.; Hunt, C.; Cerullo, G.; Varriale, S.; Gerogianni, A.; Faraco, V.; Rova, U.; Christakopoulos, P. Tailoring the Specificity of the Type C Feruloyl Esterase FoFaeC from Fusarium Oxysporum towards Methyl Sinapate by Rational Redesign Based on Small Molecule Docking Simulations. PLoS ONE 2018, 13, e0198127. [Google Scholar] [CrossRef]
- Varriale, S.; Cerullo, G.; Antonopoulou, I.; Christakopoulos, P.; Rova, U.; Tron, T.; Fauré, R.; Jütten, P.; Piechot, A.; Brás, J.L.A.; et al. Evolution of the Feruloyl Esterase MtFae1a from Myceliophthora Thermophila towards Improved Catalysts for Antioxidants Synthesis. Appl. Microbiol. Biotechnol. 2018, 102, 5185–5196. [Google Scholar] [CrossRef]
- Grajales-Hernández, D.; Armendáriz-Ruiz, M.; Velasco-Lozano, S.; López-Gallego, F.; Mateos-Díaz, J.C. Chitosan-Based CLEAs from Aspergillus Niger Type A Feruloyl Esterase: High-Productivity Biocatalyst for Alkyl Ferulate Synthesis. Appl. Microbiol. Biotechnol. 2020, 104, 10033–10045. [Google Scholar] [CrossRef]
- Katsoura, M.H.; Polydera, A.C.; Tsironis, L.D.; Petraki, M.P.; Rajačić, S.K.; Tselepis, A.D.; Stamatis, H. Efficient Enzymatic Preparation of Hydroxycinnamates in Ionic Liquids Enhances Their Antioxidant Effect on Lipoproteins Oxidative Modification. New Biotechnol. 2009, 26, 83–91. [Google Scholar] [CrossRef]
- Schär, A.; Nyström, L. Enzymatic Synthesis of Steryl Ferulates. Eur. J. Lipid Sci. Technol. 2016, 118, 1557–1565. [Google Scholar] [CrossRef]
- Topakas, E.; Stamatis, H.; Biely, P.; Kekos, D.; Macris, B.J.; Christakopoulos, P. Purification and Characterization of a Feruloyl Esterase from Fusarium Oxysporum Catalyzing Esterification of Phenolic Acids in Ternary Water–Organic Solvent Mixtures. J. Biotechnol. 2003, 102, 33–44. [Google Scholar] [CrossRef]
- Guyot, B.; Bosquette, B.; Pina, M.; Graille, J. Esterification of Phenolic Acids from Green Coffee with an Immobilized Lipase from Candida antarctica in Solvent-Free Medium. Biotechnol. Lett. 1997, 19, 529–532. [Google Scholar] [CrossRef]
- Romero-Borbón, E.; Grajales-Hernández, D.; Armendáriz-Ruiz, M.; Ramírez-Velasco, L.; Rodríguez-González, J.A.; Cira-Chávez, L.A.; Estrada-Alvarado, M.I.; Mateos-Díaz, J.C. Type C Feruloyl Esterase from Aspergillus Ochraceus: A Butanol Specific Biocatalyst for the Synthesis of Hydroxycinnamates in a Ternary Solvent System. Electron. J. Biotechnol. 2018, 35, 1–9. [Google Scholar] [CrossRef]
- Hüttner, S.; Zezzi Do Valle Gomes, M.; Iancu, L.; Palmqvist, A.; Olsson, L. Immobilisation on Mesoporous Silica and Solvent Rinsing Improve the Transesterification Abilities of Feruloyl Esterases from Myceliophthora Thermophila. Bioresour. Technol. 2017, 239, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Thörn, C.; Gustafsson, H.; Olsson, L. Immobilization of Feruloyl Esterases in Mesoporous Materials Leads to Improved Transesterification Yield. J. Mol. Catal. B Enzym. 2011, 72, 57–64. [Google Scholar] [CrossRef]
- Vafiadi, C.; Topakas, E.; Christakopoulos, P. Preparation of Multipurpose Cross-Linked Enzyme Aggregates and Their Application to Production of Alkyl Ferulates. J. Mol. Catal. B Enzym. 2008, 54, 35–41. [Google Scholar] [CrossRef]
- Topakas, E.; Stamatis, H.; Mastihubova, M.; Biely, P.; Kekos, D.; Macris, B.J.; Christakopoulos, P. Purification and Characterization of a Fusarium Oxysporum Feruloyl Esterase (FoFAE-I) Catalysing Transesterification of Phenolic Acid Esters. Enzym. Microb. Technol. 2003, 33, 729–737. [Google Scholar] [CrossRef]
- Giuliani, S.; Piana, C.; Setti, L.; Hochkoeppler, A.; Pifferi, P.G.; Williamson, G.; Faulds, C.B. Synthesis of Pentylferulate by a Feruloyl Esterase from Aspergillus Niger Using Water-in-Oil Microemulsions. Biotechnol. Lett. 2001, 23, 325–330. [Google Scholar] [CrossRef]
- Antonopoulou, I.; Iancu, L.; Jütten, P.; Piechot, A.; Rova, U.; Christakopoulos, P. Screening of Novel Feruloyl Esterases from Talaromyces Wortmannii for the Development of Efficient and Sustainable Syntheses of Feruloyl Derivatives. Enzym. Microb. Technol. 2019, 120, 124–135. [Google Scholar] [CrossRef]
- Zerva, A.; Antonopoulou, I.; Enman, J.; Iancu, L.; Jütten, P.; Rova, U.; Christakopoulos, P. Optimization of Transesterification Reactions with CLEA-Immobilized Feruloyl Esterases from Thermothelomyces Thermophila and Talaromyces Wortmannii. Molecules 2018, 23, 2403. [Google Scholar] [CrossRef]
- Antonopoulou, I.; Iancu, L.; Jütten, P.; Piechot, A.; Rova, U.; Christakopoulos, P. Optimized Enzymatic Synthesis of Feruloyl Derivatives Catalyzed by Three Novel Feruloyl Esterases from Talaromyces Wortmannii in Detergentless Microemulsions. Comput. Struct. Biotechnol. J. 2018, 16, 361–369. [Google Scholar] [CrossRef]
- Antonopoulou, I.; Leonov, L.; Jütten, P.; Cerullo, G.; Faraco, V.; Papadopoulou, A.; Kletsas, D.; Ralli, M.; Rova, U.; Christakopoulos, P. Optimized Synthesis of Novel Prenyl Ferulate Performed by Feruloyl Esterases from Myceliophthora Thermophila in Microemulsions. Appl. Microbiol. Biotechnol. 2017, 101, 3213–3226. [Google Scholar] [CrossRef]
- Huang, S.M.; Wu, P.Y.; Chen, J.H.; Kuo, C.H.; Shieh, C.J. Developing a High-Temperature Solvent-Free System for Efficient Biocatalysis of Octyl Ferulate. Catalysts 2018, 8, 338. [Google Scholar] [CrossRef]
- Chen, B.; Liu, H.; Guo, Z.; Huang, J.; Wang, M.; Xu, X.; Zheng, L. Lipase-Catalyzed Esterification of Ferulic Acid with Oleyl Alcohol in Ionic Liquid/Isooctane Binary Systems. J. Agric. Food Chem. 2011, 59, 1256–1263. [Google Scholar] [CrossRef] [PubMed]
- Sun, S.; Qin, F.; Bi, Y.; Chen, J.; Yang, G.; Liu, W. Enhanced Transesterification of Ethyl Ferulate with Glycerol for Preparing Glyceryl Diferulate Using a Lipase in Ionic Liquids as Reaction Medium. Biotechnol. Lett. 2013, 35, 1449–1454. [Google Scholar] [CrossRef] [PubMed]
- Matsuo, T.; Kobayashi, T.; Kimura, Y.; Hosoda, A.; Taniguchi, H.; Adachi, S. Continuous Synthesis of Glyceryl Ferulate Using Immobilized Candida antarctica Lipase. J. Oleo Sci. 2008, 57, 375–380. [Google Scholar] [CrossRef][Green Version]
- Tsuchiyama, M.; Sakamoto, T.; Fujita, T.; Murata, S.; Kawasaki, H. Esterification of Ferulic Acid with Polyols Using a Ferulic Acid Esterase from Aspergillus Niger. Biochim. Biophys. Acta-Gen. Subj. 2006, 1760, 1071–1079. [Google Scholar] [CrossRef]
- Kikugawa, M.; Tsuchiyama, M.; Kai, K.; Sakamoto, T. Synthesis of Highly Water-Soluble Feruloyl Diglycerols by Esterification of an Aspergillus Niger Feruloyl Esterase. Appl. Microbiol. Biotechnol. 2012, 95, 615–622. [Google Scholar] [CrossRef]
- Xin, J.-y.; Chen, L.-l.; Zhang, Y.x.; Wen, R.-r.; Zhao, D.-m.; Xia, C.-g. Lipase-Catalyzed Synthesis of α-Tocopheryl Ferulate. Food Biotechnol. 2011, 25, 43–57. [Google Scholar] [CrossRef]
- Tan, Z.; Shahidi, F. Chemoenzymatic Synthesis of Phytosteryl Ferulates and Evaluation of Their Antioxidant Activity. J. Agric. Food Chem. 2011, 59, 12375–12383. [Google Scholar] [CrossRef]
- Antonopoulou, I.; Dilokpimol, A.; Iancu, L.; Mäkelä, M.R.; Varriale, S.; Cerullo, G.; Hüttner, S.; Uthoff, S.; Jütten, P.; Piechot, A.; et al. The Synthetic Potential of Fungal Feruloyl Esterases: A Correlation with Current Classification Systems and Predicted Structural Properties. Catalysts 2018, 8, 242. [Google Scholar] [CrossRef]
- Couto, J.; Karboune, S.; Mathew, R. Regioselective Synthesis of Feruloylated Glycosides Using the Feruloyl Esterases Expressed in Selected Commercial Multi-Enzymatic Preparations as Biocatalysts. Biocatal. Biotransformation 2010, 28, 235–244. [Google Scholar] [CrossRef]
- Antonopoulou, I.; Papadopoulou, A.; Iancu, L.; Cerullo, G.; Ralli, M.; Jütten, P.; Piechot, A.; Faraco, V.; Kletsas, D.; Rova, U.; et al. Optimization of Enzymatic Synthesis of L-Arabinose Ferulate Catalyzed by Feruloyl Esterases from Myceliophthora Thermophila in Detergentless Microemulsions and Assessment of Its Antioxidant and Cytotoxicity Activities. Process Biochem. 2018, 65, 100–108. [Google Scholar] [CrossRef]
- Vafiadi, C.; Topakas, E.; Alderwick, L.J.; Besra, G.S.; Christakopoulos, P. Chemoenzymatic Synthesis of Feruloyl D-Arabinose as a Potential Anti-Mycobacterial Agent. Biotechnol. Lett. 2007, 29, 1771–1774. [Google Scholar] [CrossRef] [PubMed]
- Topakas, E.; Vafiadi, C.; Stamatis, H.; Christakopoulos, P. Sporotrichum Thermophile Type C Feruloyl Esterase (StFaeC): Purification, Characterization, and Its Use for Phenolic Acid (Sugar) Ester Synthesis. Enzym. Microb. Technol. 2005, 36, 729–736. [Google Scholar] [CrossRef]
- Couto, J.; St-Louis, R.; Karboune, S. Optimization of Feruloyl Esterase-Catalyzed Synthesis of Feruloylated Oligosaccharides by Response Surface Methodology. J. Mol. Catal. B Enzym. 2011, 73, 53–62. [Google Scholar] [CrossRef]
- Fitriani, I.N.; Utami, W. Potential Phytochemical Inhibitor from Allium Cepa for the Medication of COVID-19. Alkimia J. Ilmu Kim. Dan Terap. 2021, 4, 80–87. [Google Scholar] [CrossRef]
- Bondhon, T.A.; Mahamud, R.A.; Jannat, K.; Hasan, A.; Jahan, R.; Rahmatullah, M. In Silico Binding Studies with B-Sitosterol and Some of Its Fatty Acid Esters to 3C-like Protease of SARS-CoV-2. J. Med. Plants Stud. 2020, 8, 86–90. [Google Scholar] [CrossRef]
- Sabater-Molina, M.; Larqué, E.; Torrella, F.; Zamora, S. Dietary Fructooligosaccharides and Potential Benefits on Health. J. Physiol. Biochem. 2009, 65, 315–328. [Google Scholar] [CrossRef]
- Cui, C.; Wang, Z.P.; Du, X.J.; Wang, L.Z.; Yu, S.J.; Liu, X.H.; Li, Z.M.; Zhao, W.G. Synthesis and Antiviral Activity of Hydrogenated Ferulic Acid Derivatives. J. Chem. 2013, 2013, 269434. [Google Scholar] [CrossRef]
- Lan, X.; Xie, D.; Yin, L.; Wang, Z.; Chen, J.; Zhang, A.; Song, B.; Hu, D. Novel α,β-Unsaturated Amide Derivatives Bearing α-Amino Phosphonate Moiety as Potential Antiviral Agents. Bioorganic Med. Chem. Lett. 2017, 27, 4270–4273. [Google Scholar] [CrossRef]
- Wu, Z.; Zhang, J.; Chen, J.; Pan, J.; Zhao, L.; Liu, D.; Zhang, A.; Chen, J.; Hu, D.; Song, B. Design, Synthesis, Antiviral Bioactivity and Three-Dimensional Quantitative Structure–Activity Relationship Study of Novel Ferulic Acid Ester Derivatives Containing Quinazoline Moiety. Pest Manag. Sci. 2017, 73, 2079–2089. [Google Scholar] [CrossRef]
- Spasova, M.; Philipov, S.; Nikolaeva-Glomb, L.; Galabov, A.S.; Milkova, T. Cinnamoyl- and Hydroxycinnamoyl Amides of Glaucine and Their Antioxidative and Antiviral Activities. Bioorg. Med. Chem. 2008, 16, 7457–7461. [Google Scholar] [CrossRef] [PubMed]
- Tang, X.; Zhang, C.; Chen, M.; Xue, Y.; Liu, T.; Xue, W. Synthesis and Antiviral Activity of Novel Myricetin Derivatives Containing Ferulic Acid Amide Scaffolds. New J. Chem. 2020, 44, 2374–2379. [Google Scholar] [CrossRef]
- Gan, X.; Hu, D.; Wang, Y.; Yu, L.; Song, B. Novel Trans-Ferulic Acid Derivatives Containing a Chalcone Moiety as Potential Activator for Plant Resistance Induction. J. Agric. Food Chem. 2017, 65, 4367–4377. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Xie, D.; Gan, X.; Zeng, S.; Zhang, A.; Yin, L.; Song, B.; Jin, L.; Hu, D. Synthesis, Antiviral Activity, and Molecular Docking Study of Trans-Ferulic Acid Derivatives Containing Acylhydrazone Moiety. Bioorg. Med. Chem. Lett. 2017, 27, 4096–4100. [Google Scholar] [CrossRef]
- Ichimura, T.; Otake, T.; Mori, H.; Maruyama, S. HIV-1 Protease Inhibition and Anti-HIV Effect of Natural and Synthetic Water-Soluble Lignin-like Substances. Biosci. Biotechnol. Biochem. 1999, 63, 2202–2204. [Google Scholar] [CrossRef]
- Hariono, M.; Abdullah, N.; Damodaran, K.V.; Kamarulzaman, E.E.; Mohamed, N.; Hassan, S.S.; Shamsuddin, S.; Wahab, H.A. Potential New H1N1 Neuraminidase Inhibitors from Ferulic Acid and Vanillin: Molecular Modelling, Synthesis and in Vitro Assay. Sci. Rep. 2016, 6, 38692. [Google Scholar] [CrossRef]
- Nguyen, D.D.; Gao, K.; Chen, J.; Wang, R.; Wei, G.-W. Unveiling the Molecular Mechanism of SARS-CoV-2 Main Protease Inhibition from 137 Crystal Structures Using Algebraic Topology and Deep Learning. Chem. Sci. 2020, 11, 12036–12046. [Google Scholar] [CrossRef]
- Arnott, J.A.; Planey, S.L. The Influence of Lipophilicity in Drug Discovery and Design. Expert Opin. Drug Discov. 2012, 7, 863–875. [Google Scholar] [CrossRef]
- Coimbra, J.T.S.; Feghali, R.; Ribeiro, R.P.; Ramos, M.J.; Fernandes, P.A. The Importance of Intramolecular Hydrogen Bonds on the Translocation of the Small Drug Piracetam through a Lipid Bilayer. RSC Adv. 2021, 11, 899–908. [Google Scholar] [CrossRef]
- Daina, A.; Michielin, O.; Zoete, V. SwissADME: A Free Web Tool to Evaluate Pharmacokinetics, Drug-Likeness and Medicinal Chemistry Friendliness of Small Molecules. Sci. Rep. 2017, 7, 42717. [Google Scholar] [CrossRef]
- Benet, L.Z.; Hosey, C.M.; Ursu, O.; Oprea, T.I. BDDCS, the Rule of 5 and Drugability. Adv. Drug Deliv. Rev. 2016, 101, 89–98. [Google Scholar] [CrossRef] [PubMed]
- Molsoft LLC About Molecular Properties Prediction. Available online: https://www.molsoft.com/mpropdesc.html (accessed on 1 May 2022).
- Zhang, L.; Zhou, L.; Bao, L.; Liu, J.; Zhu, H.; Lv, Q.; Liu, R.; Chen, W.; Tong, W.; Wei, Q.; et al. SARS-CoV-2 Crosses the Blood–Brain Barrier Accompanied with Basement Membrane Disruption without Tight Junctions Alteration. Signal Transduct. Target. Ther. 2021, 6, 337. [Google Scholar] [CrossRef] [PubMed]
- Ghahremanian, S.; Rashidi, M.M.; Raeisi, K.; Toghraie, D. Molecular Dynamics Simulation Approach for Discovering Potential Inhibitors against SARS-CoV-2: A Structural Review. J. Mol. Liq. 2022, 354, 118901. [Google Scholar] [CrossRef] [PubMed]
- Mahmud, S.; Mita, M.A.; Biswas, S.; Paul, G.K.; Promi, M.M.; Afrose, S.; Hasan, R.; Shimu, S.S.; Zaman, S.; Uddin, S.; et al. Molecular Docking and Dynamics Study to Explore Phytochemical Ligand Molecules against the Main Protease of SARS-CoV-2 from Extensive Phytochemical Datasets. Expert Rev. Clin. Pharmacol. 2021, 14, 1305–1315. [Google Scholar] [CrossRef] [PubMed]
- Khan, J.; Sakib, S.A.; Mahmud, S.; Khan, Z.; Islam, M.N.; Sakib, M.A.; Emran, T.B.; Simal-Gandara, J. Identification of Potential Phytochemicals from Citrus Limon against Main Protease of SARS-CoV-2: Molecular Docking, Molecular Dynamic Simulations and Quantum Computations. J. Biomol. Struct. Dyn. 2021, 1–12. [Google Scholar] [CrossRef]
- Biswas, S.; Mahmud, S.; Mita, M.A.; Afrose, S.; Hasan, R.; Sultana Shimu, M.S.; Saleh, A.; Mostafa-Hedeab, G.; Alqarni, M.; Obaidullah, A.J.; et al. Molecular Docking and Dynamics Studies to Explore Effective Inhibitory Peptides against the Spike Receptor Binding Domain of SARS-CoV-2. Front. Mol. Biosci. 2022, 8, 791642. [Google Scholar] [CrossRef] [PubMed]


| Compound | Reaction | Donor | Acceptor | Enzyme | Solvent System | Yield (Time) | T (°C) | Reference |
|---|---|---|---|---|---|---|---|---|
| Methyl ferulate | Esterification | FA | Methanol | CLEAs AnFaeA | Solvent-free (containing buffer) | 20.6% (24 h) | 30 | [71] |
| Esterification | Methanol | FA | Immobilized CALB | [bmim]PF6 | 41.7% (72 h) | 60 | [72] | |
| Ethyl ferulate | Esterification | FA | Ethanol | CLEAs AnFaeA | Solvent-free (containing buffer) | 50.5% (24 h) | 30 | [71] |
| Esterification | Ethanol | FA | RML | Hexane | 76.2% (72 h) | 61 | [73] | |
| Esterification | Ethanol | FA | Immobilized CALB | [bmim]PF6 | 40.7% (72 h) | 60 | [72] | |
| Propyl ferulate | Esterification | FA | Propanol | CLEAs AnFaeA | Solvent-free (containing buffer) | 98.8% (24 h) | 30 | [71] |
| Esterification | Propanol | FA | Immobilized RML | [bmim]PF6 | 48.2% (72 h) | 60 | [72] | |
| Transesterification | MFA | Propanol | FoFae-II | n-Hexane:1-propanol: water | 16% (224 h) | 30 | [74] | |
| Butyl ferulate | Esterification | FA | Butanol | CLEAs AnFaeA | Solvent-free (containing buffer) | 99.5% (24 h) | 30 | [71] |
| Esterification | Butanol | FA | Immobilized RML | [bmim]PF6 | 52.6% (72 h) | 60 | [72] | |
| Esterification | Butanol | FA | Novozym 435 | Solvent-free | Traces (15 d) | 60 | [75] | |
| Transesterification | MFA | Butanol | AocFaeC | Isooctane: butanol: buffer | n.q. | 30 | [76] | |
| Transesterification | MFA | 1-Butanol | C1 FAEs immobilized on mesoporous silica | Solvent-free (containing buffer) | n.q. | 30 | [77] | |
| Transesterification | MFA | 1-Butanol | Depol 740 L | Solvent-free (containing buffer) | Up to 90% (6 d) | 37 | [78] | |
| Transesterification | MFA | 1-Butanol | CLEAs Ultraflo L | Hexane: 1-butanol: buffer | 97% (144 h) | 37 | [79] | |
| Transesterification | MFA | 1-Butanol | FoFae-I | Hexane:1-butanol: buffer | ∼13% (144 h) | 35 | [80] | |
| Isobutyl ferulate | Esterification | FA | Isobutanol | CLEAs AnFaeA | Solvent-free (containing buffer) | 98.4% (24 h) | 30 | [71] |
| Pentyl ferulate | Esterification | FA | Pentanol | CLEAs AnFaeA | Solvent-free (containing buffer) | 99.4% (24 h) | 30 | [71] |
| Esterification | FA | 1-Pentanol | FAEA | CTAB: hexane: pentanol: buffer | 60% (n/q) | 40 | [81] | |
| Isopentyl ferulate | Esterification | FA | Isopentanol | CLEAs AnFaeA | Solvent-free (containing buffer) | 97.0% (24 h) | 30 | [71] |
| Prenyl ferulate | Transesterification | VFA | Prenol | Fae125 | n-Hexane: buffer: DMSO | 92.5% (24 h) | 25 | [82] |
| Transesterification | VFA | Prenol | CLEAs Fae125 | n-Hexane: buffer | 83.7% (34.3 h) | 32 | [83] | |
| Transesterification | VFA | Prenol | Fae125 | n-Hexane: t-butanol: buffer | 81.1% (24 h) | 40 | [84] | |
| Transesterification | VFA | Prenol | C1FaeB2 | n-Hexane: t-butanol: buffer | 71.5% (24 h) | 30 | [85] | |
| Hexyl ferulate | Esterification | FA | Hexanol | CLEAs AnFaeA | Solvent-free (containing buffer) | 98.5% (24 h) | 30 | [71] |
| Esterification | Hexanol | FA | Immobilized RML | [bmim]PF6 | 38.1% (72 h) | 60 | [72] | |
| Octyl ferulate | Esterification | FA | Octanol | CLEAs AnFaeA | Solvent-free (containing buffer) | 99.3% (24 h) | 30 | [71] |
| Esterification | Octanol | FA | Novozym 435 | Solvent-free | 93.2% (72 h) | 92.2 | [86] | |
| Esterification | Octanol | FA | Immobilized RML | [bmim]PF6 | 34.9% (72 h) | 60 | [72] | |
| Esterification | Octanol | FA | Novozym 435 | Solvent free | 13% (15 d) | 60 | [75] | |
| Dodecyl (or lauryl) ferulate | Esterification | FA | Dodecanol | CLEAs AnFaeA | Solvent-free (containing buffer) | 96.6% (24 h) | 30 | [71] |
| Esterification | Dodecanol | FA | Novozym 435 | Solvent-free | 10% (15 d) | 60 | [75] | |
| Octadecyl (or stearyl) ferulate | Esterification | Octadecanol | FA | Immobilized RML | Hexane | n.q. (72 h) | 61 | [73] |
| Oleyl ferulate | Esterification | FA | Oleyl alcohol | CLEAs AnFaeA | Solvent-free (containing buffer) | 100% (24 h) | 30 | [71] |
| Transesterification | Oleyl alcohol | FA | Novozym 435 | Hexane | 99.17% (4 d) | 60 | [87] | |
| Glyceryl ferulate | Transesterification | Glycerol | EFA | Novozym 435 | EMIMTF2N | 100% (12 h) | 70 | [88] |
| Esterification | FA | Glycerol | Chirazyme L2 C-2 | Solvent-free | 80% (>3 h) | 80 | [89] | |
| Esterification | FA | Glycerol | FAE-PL | Glycerol: DMSO: buffer | 81% (n.q.) | 50 | [90] | |
| Diglyceryl ferulate | Esterification | FA | Diglycerin S | FAE-PL | Diglycerin S: DMSO: buffer | 95% (12 h) | 50 | [91] |
| Tocopheryl ferulate | Transesterification | Vitamin E | EFA | Novozym 435 | Solvent-free | 25.2% (72 h) | 60 | [92] |
| Sitosteryl ferulate | Transesterification Esterification | Sitosterol | EFA FA | CRL | Hexane | 55% (5 d) 35% (5 d) | 63 | [73] |
| Transesterification | Sitosterol | VFA | CRL | Hexane: 2 butanone | ∼55% (10 d) | 45 | [93] | |
| d-glucose ferulate | Transesterification | VFA | D-glucose | Fae125 | n-Hexane: t-butanol: buffer | 22.5% (8 h) | 45 | [94] |
| d-galactose ferulate | Transesterification | VFA | D-galactose | C1FaeA1 | n-Hexane: t-butanol: buffer | 22.8% (8 h) | 45 | [94] |
| Esterification | FA | D-galactose | Flavourzyme | Hexane: t-butanol: buffer | 41.9% (144 h) | 35 | [95] | |
| d-mannose ferulate | Transesterification | VFA | D-mannose | C1FaeA1 | n-Hexane: t-butanol: buffer | 21.5% (8 h) | 45 | [94] |
| d-fructose ferulate | Transesterification | VFA | D-fructose | C1FaeA1 | n-Hexane: t-butanol: buffer | 29.4% (8 h) | 45 | [94] |
| Arabinose ferulate | Transesterification | VFA | L-Arabinose | Fae125 | n Hexane: buffer: DMSO | 56.2% (24 h) | 40 | [82] |
| Transesterification | VFA | L-Arabinose | Fae125 | n-Hexane: t-butanol: buffer | 33.0% | 40 | [96] | |
| Transesterification | VFA | L-Arabinose | C1FaeA1 | n-Hexane: t-butanol: buffer | 52.2% (8 h) | 55 | [84] | |
| Transesterification | VFA | L-arabinose | CLEAs Fae125 | n-Hexane: buffer | 58.1% (10 h) | 32 | [83] | |
| Esterification | FA | D-Arabinose | Multifect P3000 | Hexane: t-butanol: buffer | 36.7% (144 h) | 35 | [95] | |
| Transesterification | MFA | D-arabinose | StFae-C | Hexane: t-butanol: buffer | 45% (n.q.) | 35 | [97] | |
| Transesterification | MFA EFA | L-arabinose | StFae-C | Hexane: t-butanol: buffer | Up to 50% (120 h) 6.3% (n.q.) | 35 | [98] | |
| d-xylose ferulate | Transesterification | VFA | D-xylose | C1FaeA1 | n-Hexane: t-butanol: buffer | 7.5% (8 h) | 45 | [94] |
| Esterification | FA | D-xylose | Multifect P3000 | Hexane: t-butanol: buffer | 30.8% (144 h) | 35 | [95] | |
| d-lactose ferulate | Transesterification | VFA | D-lactose | C1FaeA1 | n-Hexane: t-butanol: buffer | <2% (8 h) | 45 | [94] |
| Esterification | FA | Lactose | Depol 740 L | n-Hexane: 2-butanone: buffer | 4.4% (n.q.) | 35 | [99] | |
| d-sucrose ferulate | Transesterification | VFA | D-sucrose | FaeA1 | n-Hexane: t-butanol: buffer | 8.2% (8 h) | 45 | [94] |
| Esterification | FA | D-sucrose | Depol 740 L | n-Hexane: 2-butanone: buffer | 13.2% (n.q.) | 35 | [99] | |
| d-maltose ferulate | Transesterification | VFA | D-maltose | C1FaeA1 | n-Hexane: t-butanol: buffer | 8.9% (8 h) | 45 | [94] |
| d-cellobiose ferulate | Transesterification | VFA | D-cellobiose | C1FaeA1 | n-Hexane: t-butanol: buffer | <2% (8 h) | 45 | [94] |
| Xylobiose ferulate | Esterification | FA | Xylobiose | Depol 740 L | n-Hexane: 2-butanone: buffer | 9.4% (n.q.) | 35 | [99] |
| Galactobiose ferulate | Esterification | FA | Galactobiose | Depol 740 L | n-Hexane: 2-butanone: buffer | 5.4% (n.q) | 35 | [99] |
| Arabinobiose ferulate | Esterification | FA | Arabinobiose | Depol 740 L | n-Hexane: 2-butanone: buffer | 7.9% (n.q) | 35 | [99] |
| Raffinose ferulate | Esterification | FA | Raffinose | Depol 740 L | n-Hexane: 2-butanone: buffer | 11.9% (7 d) | 35 | [99] |
| FOS ferulate | Esterification | FA | FOS | Depol 740 L | n-Hexane: 2-butanone: buffer | 9.6% (n.q.) | 35 | [99] |
| d-mannitol ferulate | Transesterification | VFA | D-mannitol | C1FaeA1 | n-Hexane: t-butanol: buffer | 26.7% (8 h) | 45 | [94] |
| d-sorbitol ferulate | Transesterification | VFA | D-sorbitol | C1FaeA1 | n-Hexane: t-butanol: buffer | 50.0% (8 h) | 45 | [94] |
| d-xylitol ferulate | Transesterification | VFA | D-xylitol | C1FaeA1 | n-Hexane: t-butanol: buffer | 43.3% (8 h) | 45 | [94] |
| FA rutinoside | Transglycosylation | Rutin | FA | Rutinase derived from tartary buckwheat | Buffer | ∼4.5 μmol (48 h) | 40 | [35] |
| Compound | Binding Energy (kcal/mol) 1 | No of Interactions | Total Contacting Residues | ||
|---|---|---|---|---|---|
| H-Bond 2 | Hydrophobic 3 | Pi-Pi | |||
| Ferulic acid | −5.87 | 3 (ARG 188, THR 190 × 2) | 1 (GLN 189) | 1 (HIS 41) | HIS 41, MET 49, TYR 54, CYS 145, HIS 164, MET 165, GLU 166, ASP 187, ARG 188, GLN 189, THR 190, GLN 192 |
| Methyl ferulate | −5.73 | 4 (GLY 143 × 2, SER 144, CYS 145) | 1 (MET 165) | 1 (HIS 163) | LEU 27, HIS 41, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, MET 165, GLU 166, ARG 188, GLN 189, GLN 192 |
| Ethyl ferulate | −5.87 | 7 (LEU 141, GLY 143 × 2, SER 144 × 2, CYS 145, GLN 189) | 1 (GLN 189) | 1 (HIS 163) | LEU 27, HIS 41, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, ARG 188, GLN 189, THR 190, GLN 192 |
| Propyl ferulate | −5.98 | 6 (LEU 141, GLY 143 × 2, SER 144 × 2, CYS 145) | 1 (MET 165) | 1 (HIS 163) | LEU 27, HIS 41, CYS 44, MET 49, TYR 54, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, ASP 187, ARG 188, GLN 189 |
| Butyl ferulate | −6.02 | 6 (LEU 141, GLY 143 × 2, SER 144 × 2, CYS 145) | 1 (MET 165) | 1 (HIS 163) | HIS 41, CYS 44, MET 49, PRO 52, TYR 54, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, ASP 187, ARG 188, GLN 189 |
| Isobutyl ferulate | −6.30 | 7 (LEU 141, GLY 143 × 2, SER 144 × 2, CYS 145, GLN 189) | 1 (MET 165) | 1 (HIS 163) | HIS 41, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, MET 165, GLU 166, LEU 167, PRO 168, ARG 188, GLN 189, THR 190, GLN 192 |
| Pentyl ferulate | −5.92 | 2 (THR 190, GLN 192) | 1 (MET 165) | 1 (HIS 41) | HIS 41, MET 49, TYR 54, CYS 145, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, ASP 187, ARG 188, GLN 189, THR 190, GLN 192 |
| Isopentyl ferulate | −6.58 | 6 (LEU 141, GLY 143 × 2, SER 144 × 2, CYS 145) | 1 (MET 49) | 1 (HIS 163) | LEU 27, HIS 41, CYS 44, MET 49, PRO 52, TYR 54, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, ASP 187, ARG 188, GLN 189 |
| Prenyl ferulate | −6.75 | 6 (LEU 141, GLY 143 × 2, SER 144 × 2, CYS 145) | 1 (GLN 189) | 1 (HIS 163) | LEU 27, HIS 41, CYS 44, MET 49, PRO 52, TYR 54, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, ASP 187, ARG 188, GLN 189 |
| Hexyl ferulate | −6.47 | 7 (LEU 141, GLY 143 × 2, SER 144 × 2, CYS 145, GLN 189) | 1 (GLN 189) | 1 (HIS 163) | HIS 41, MET 49, PRO 52, TYR 54, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, HIS 172, ASP 187, ARG 188, GLN 189 |
| Octyl ferulate | −6.20 | 6 (LEU 141, GLY 143 × 2, SER 144 × 2, CYS 145) | 1 (HIS 41) | 1 (HIS 163) | HIS 41, MET 49, TYR 54, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, ASP 187, ARG 188, GLN 189, THR 190 |
| Dodecyl ferulate | −5.56 | 3 (ARG 188, THR 190 × 2) | 1 (GLU 166) | 1 (HIS 41) | HIS 41, MET 49, PHE 140, LEU 141, ASN 142, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, HIS 172, PHE 181, ASP 187, ARG 188, GLN 189, THR 190, ALA 191, GLN 192 |
| Octadecyl ferulate | −5.20 | 4 (ARG 188, THR 190 × 2, GLN 192) | 1 (MET 49) | 0 | THR 25, THR 26, LEU 27, HIS 41, MET 49, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, PRO 168, HIS 172, ARG 188, GLN 189, THR 190, ALA 191, GLN 192 |
| Oleyl ferulate | −5.17 | 4 (ARG 188 × 2, THR 190 × 2) | 1 (MET 49) | 1 (HIS 41) | THR 24, THR 25, THR 26, LEU 27, HIS 41, MET 49, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, PRO 168, HIS 172, ASP 187, ARG 188, GLN 189, THR 190, GLN 192 |
| Glyceryl ferulate | −6.55 | 12 (LEU 141, GLY 143 × 2, SER 144 × 2, CYS 145, GLU 166, ARG 188, GLN 189, THR 190 × 2, GLN 192) | 1 (MET 165) | 1 (HIS 163) | LEU 27, HIS 41, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, MET 165, GLU 166, LEU 167, PRO 168, ARG 188, GLN 189, THR 190, GLN 192 |
| Diglyceryl ferulate | −6.61 | 10 (TYR 54, LEU 141, GLY 143 × 2, SER 144 × 2, CYS 145, HIS 164, ARG 188, GLN 189) | 1 (GLN 189) | 1 (HIS 163) | HIS 41, CYS 44, MET 49, PRO 52, TYR 54, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, HIS 172, ASP 187, ARG 188, GLN 189, THR 190, GLN 192 |
| Tocopheryl ferulate | −6.91 | 2 (SER 46, GLN 189) | 1 (GLN 189) | THR 25, LEU 27, HIS 41, SER 46, GLU 47, MET 49, LEU 50, TYR 54, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, PRO 168, HIS 172, ASP 187, ARG 188, GLN 189, THR 190 | |
| Sitosteryl ferulate | −7.81 | 3 (THR 25, HIS 41, GLY 143) | 1 (PRO 168) | 1 (HIS 41) | THR 24, THR 25, THR 26, LEU 27, HIS 41, CYS 44, THR 45, SER 46, MET 49, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, ARG 188, GLN 189, THR 190, ALA 191, GLN 192 |
| d-glucose ferulate | −7.09 | 11 (LEU 141, SER 144, HIS 163, GLU 166, ARG 188, GLN 189, THR 190 × 3, GLN 192 × 2) | 1 (GLU 166) | 1 (HIS 163) | HIS 41, PHE 140, LEU 141, ASN 142, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, ARG 188, GLN 189, THR 190, ALA 191, GLN 192 |
| d-galactose ferulate | −7.24 | 13 (LEU 141 × 2, ASN 142, GLY 143, SER 144 × 3, CYS 145, HIS 163, ARG 188, THR 190 × 2, GLN 192) | 1 (GLN 189) | 0 | PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, MET 165, GLU 166, PRO 168, ASP 187, ARG 188, GLN 189, THR 190, ALA 191, GLN 192 |
| d-mannose ferulate | −7.09 | 11 (LEU 141, SER 144, HIS 163, GLU 166, ARG 188, GLN 189, THR 190 × 3, GLN 192 × 2) | 1 (GLU 166) | 1 (HIS 163) | HIS 41, PHE 140, LEU 141, ASN 142, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, ARG 188, GLN 189, THR 190, ALA 191, GLN 192 |
| d-fructose ferulate | −7.06 | 8 (THR 26 × 2, PHE 140, LEU 141, ASN 142, SER 144, HIS 163, GLU 166) | 1 (HIS 41) | 1 (HIS 41) | THR 24, THR 25, THR 26, LEU 27, HIS 41, THR 45, MET 49, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, HIS 172, GLN 189 |
| l-arabinose ferulate | −7.08 | 5 (HIS 41, MET 49, HIS 164, GLN 189, THR 190) | 1 (LEU 167) | 0 | HIS 41, MET 49, TYR 54, CYS 145, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, ASP 187, ARG 188, GLN 189, THR 190, ALA 191, GLN 192 |
| d-xylose ferulate | −7.37 | 13 (LEU 141 × 2, ASN 142, GLY 143, SER 144 × 3, CYS 145, HIS 163, ARG 188, THR 190 × 2, GLN 192) | 1 (ΜΕΤ 165) | 1 (HIS 163) | PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, PRO 168, ASP 187, ARG 188, GLN 189, THR 190, GLN 192 |
| d-lactose ferulate | −7.63 | 12 (ASN 142 × 2, GLY 143, GLU 166 × 3, ARG 188, GLN 189, THR 190 × 3, GLN 192) | 1 (ΜΕΤ 165) | 1 (HIS 41) | HIS 41, MET 49, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, ASP 187, ARG 188, GLN 189, THR 190, ALA 191, GLN 192 |
| d-sucrose ferulate | −7.77 | 14 (THR 26, LEU 141 × 2, GLY 143 × 2, SER 144 × 3, CYS 145, HIS 163 × 2, GLU 166, GLN 189 × 2) | 1 (GLN 189) | 0 | THR 25, THR 26, LEU 27, HIS 41, MET 49, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, HIS 172, GLN 189, THR 190, ALA 191, GLN 192 |
| d-maltose ferulate | −7.47 | 13 (SER 46 × 2, LEU 141 × 2, ASN 142, GLY 143 × 2, SER 144 × 2, CYS 145, GLU 166, GLN 189 × 2) | 1 (THR 25) | 0 | THR 24, THR 25, THR 26, LEU 27, HIS 41, THR 45, SER 46, MET 49, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, GLN 189 |
| d-cellobiose ferulate | −7.50 | 9 (THR 24, LEU 141, ASN 142 × 2, GLY 143 × 2, SER 144, THR 190, GLN 192) | 1 (ΜΕΤ 165) | 0 | THR 24, THR 25, THR 26, LEU 27, HIS 41, MET 49, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, ARG 188, GLN 189, THR 190, ALA 191, GLN 192 |
| Xylobiose ferulate | −7.97 | 11 (THR 24 × 2, THR 25, THR 26, THR 45 × 2, THR 46 × 2, HIS 41, PHE 140, GLU 166) | 1 (GLU 166) | 1 (HIS 163) | THR 24, THR 25, THR 26, LEU 27, HIS 41, THR 45, SER 46, MET 49, PHE 140, LEU 141, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, HIS 172, GLN 189 |
| Galactobiose ferulate | −8.36 | 12 (ASN 119 × 2, PHE 140, LEU 141, GLY 143, SER 144 × 2, CYS 145, GLU 166 × 2, GLN 189, THR 190) | 1 (GLN 189) | 0 | GLN 19, THR 25, THR 26, LEU 27, HIS 41, MET 49, TYR 118, ASN 119, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, HIS 172, GLN 189, THR 190, ALA 191, GLN 192 |
| Arabinobiose ferulate | −7.88 | 7 (THR 26, PHE 140, ASN 142, GLU 166 × 2, LEU 167, GLN 189) | 1 (GLN 189) | 1 (HIS 41) | THR 24, THR 25, THR 26, LEU 27, HIS 41, MET 49, PRO 52, TYR 54, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, HIS 172, ASP 187, ARG 188, GLN 189, THR 190, GLN 192 |
| Raffinose ferulate | −8.34 | 8 (THR 26, SER 144 × 2, CYS 145, HIS 163, GLU 166, THR 190, GLN 192) | 1 (MET 49) | 0 | THR 24, THR 25, THR 26, LEU 27, THR 45, MET 49, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, HIS 172, ARG 188, GLN 189, THR 190, ALA 191, GLN 192 |
| FOS ferulate 1 | −8.18 | 9 (SER 46 × 2, PHE 140, LEU 141 × 2, GLY 143, SER 144, HIS 163, THR 190) | 1 (GLN 189) | 0 | THR 25, THR 26, HIS 41, THR 45, SER 46, MET 49, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, ARG 188, GLN 189, THR 190, ALA 191, GLN 192 |
| FOS ferulate 2 | −7.34 | 8 (THR 26 × 3, GLY 143 × 2, HIS 164, GLU 166, THR 190) | 1 (LEU 27) | 0 | THR 25, THR 26, LEU 27, HIS 41, VAL 42, MET 49, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, ARG 188, GLN 189, THR 190, GLN 192 |
| FOS ferulate 3 | −8.52 | 14 (SER 46 × 3, LEU 141 × 2, ASN 142, GLY 143 × 2, SER 144 × 2, CYS 145, HIS 163, HIS 164, GLN 192) | 1 (LEU 50) | 0 | THR 24, THR 25, THR 26, LEU 27, HIS 41, CYS 44, THR 45, SER 46, GLU 47, MET 49, LEU 50, PRO 52, TYR 54, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, HIS 172, ASP 187, ARG 188, GLN 189, THR 190, ALA 191, GLN 192 |
| d-mannitol ferulate | −6.38 | 12 (LEU 141, GLY 143 × 2, SER 144 × 2, CYS 145, GLU 166, ARG 188, GLN 189, THR 190 × 2, GLN 192) | 1 (ΜΕΤ 165) | 1 (HIS 163) | PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, MET 165, GLU 166, LEU 167, PRO 168, HIS 172, ARG 188, GLN 189, THR 190, ALA 191, GLN 192 |
| d-sorbitol ferulate | −6.43 | 13 (LEU 141, GLY 143 × 2, SER 144 × 2, CYS 145, GLU 166, ARG 188, GLN 189 × 2, THR 190 × 2, GLN 192) | 1 (ΜΕΤ 165) | 1 (HIS 163) | PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, ARG 188, GLN 189, THR 190, ALA 191, GLN 192 |
| d-xylitol ferulate | −6.68 | 15 (PHE 140, LEU 141 × 2, ASN 142, GLY 143, SER 144 × 3, CYS 145, HIS 163, GLU 166, ARG 188, THR 190 × 2, GLN 192) | 1 (GLN 189) | 0 | PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, MET 165, GLU 166, PRO 168, HIS 172, ASP 187, ARG 188, GLN 189, THR 190, GLN 192 |
| FA rutinoside | −8.40 | 16 (THR 24 × 3, THR 25, THR 45, LEU 141 × 2, GLY 143 × 3, SER 144 × 2, CYS 145, HIS 163, GLU 166, ARG 188, GLN 189) | 1 (MET 49) | 0 | THR 24, THR 25, THR 26, LEU 27, HIS 41, CYS 44, THR 45, SER 46, MET 49, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, HIS 172, ARG 188, GLN 189, THR 190, GLN 192 |
| N3 | −8.26 | 4 (CYS 145, GLU 166, GLN 189) | 1 (MET 49) | 1(HIS 41) | THR 25, LEU 27, HIS 41, MET 49, LEU 50, TYR 54, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, HIS 172, ASP 187, ARG 188, GLN 189, THR 190, ALA 191, GLN 192 |
| GC376 | −7.80 | 5 (HIS 41, PHE 140, HIS 163, GLU 166, GLN 189) | 1 (ASP 187) | 0 | HIS 41, MET 49, TYR 54, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, HIS 172, ASP 187, ARG 188, GLN 189, THR 190, ALA 191, GLN 192 |
| Category | Code 1 | Name | Derivatization Method | Yield | NoD 2 | Reference |
|---|---|---|---|---|---|---|
| FA amide | 7a | Not given | Six steps: acetylation with acetic anhydride in aqueous sodium hydroxide solution, reaction with thionyl chloride, reaction with a substituted 2-amino-1-phenylethanone, reduction to the corresponding alcohol with sodium borohydride and hydrolyzation of the acetyl group with NaOH, alkylation of the phenolic hydroxyl group, and alkylation with a bromoalkane in the presence of NaH. | Not given | 16 | [32] |
| Hydrogenated FA amides (A) | 13b | Not given | Four steps: catalytic hydrogenation of FA using Pd/C and H2 in the presence of HCl, multi-step reaction involving an acid chloride intermediate (including hydrolysis, hydroxyl protection, acyl chloride formation, amidation, and deprotection) and microwave radiation, alkylation of the phenolic hydroxyl group with bromoalkene and NaOH, reaction with bromoalkane, and deprotonation with NaOH. | 71% | 9 | [32] |
| Hydrogenated FA amides (B) | 4f | N-(2-(4-(Benzyloxy)phenyl)-2-(prop-2-yn-1-yloxy)ethyl)-3-(3,4-dimethoxyphenyl)propanamide | Three steps: catalytic hydrogenation of FA with Pd/C and H2 towards ethyl ferulate, substitution with 2-amino-1-phenylethanol under microwave radiation at 130 oC, alkylation with bromoalkane. | 68% | 7 | [103] |
| FA sulfonamide | 2 | €-3-(4-(2-((4-acetamidophenyl)sulfonamido)ethoxy)-3-methoxyphenyl)acrylate methyl | Two parallel steps: reaction of FA with alcohol catalyzed by sulfuric acid, and reaction of sulfonyl chloride and bromoethylamine hydrobromide in dichloromethane in the presence of triethylamine. Dissolvation of intermediate A in acetonitrile and potassium carbonate and combination with the other intermediate towards the target compound. | 45% | 16 | [33] |
| α,β-Unsaturated amide derivatives of FA with an α-aminophosphonate moiety | g18 | (E)-((4-chlorophenyl)(3-(3-methoxy-4-((4-(trifluoromethyl)benzyl)oxy)phenyl)acrylamido)methyl)phosphonate | Two parallel routes towards two intermediates, which are then combined via dehydration condensation reaction towards the final product. The first intermediate involves treatment of an aromatic aldehyde with ammonia, reaction with diethyl phosphite, and then hydrolysis to diethyl 1-aminoarylmethylphosphonate. The second intermediate is also produced in three steps, starting from FA, which is methylated in with methyl alcohol in the presence of sulfuric acid, then esterification with benzyl halide in the presence of potassium carbonate and acetonitrile, and then hydrolyzation with NaOH. | 53.60% | 26 | [104] |
| FA derivatives with a quinazoline moiety (A) | e27 | 2-methoxyphen€(E)-3-(3-methoxy-4-((4-oxoquinazolin-3(4H)-yl)methoxy)phenyl)acrylate | The first step of the derivatization involves esterification of FA, either with the appropriate alcohol in the presence of sulfuric acid, or by reaction with acetic anhydride, NaOH, and then with thionyl chloride towards an O-acetyl ferulic acid chloride, and finally mixture with tetrahydrofuran, triethylamine, and the appropriate phenol. Then, the intermediate was mixed with 3-chloromethyl-4(3H)-quinazolinone, potassium carbonate, potassium iodide, and acetronitrile toward the final product. | 50.80% | 28 | [105] |
| FA derivatives with a quinazoline moiety (B) | e28 | 4-allyl-2-methoxyp€yl-(E)-3-(3-methoxy-4-((4-oxoquinazolin-3(4H)-yl)methoxy)phenyl)acrylate | The first step of the derivatization involves esterification of FA, either with the appropriate alcohol in the presence of sulfuric acid, or by reaction with acetic anhydride, NaOH, and then with thionyl chloride towards an O-acetyl ferulic acid chloride, and finally mixture with tetrahydrofuran, triethylamine, and the appropriate phenol. Then, the intermediate was mixed with 3-chloromethyl-4(3H)-quinazolinone, potassium carbonate, potassium iodide, and acetronitrile toward the final product. | 64.80% | 28 | [105] |
| FA amide of 3-aminomethyl glaucine | 5 | Feruloyl amide of 3-aminomethylglaucine | Peptide chemistry methods using EDC/HOBt to link 3-aminomethylglaucine to FA. 3-aminomethylglaucine was produced from glaucine through reaction with N-(hydroxymethyl)acetamide in acidic media and subsequent hydrolyzation. | 61.60% | 1 | [106] |
| Myricetin derivatives with a FA amide scaffold | 4n | (E)-N-(4-bromophenyl)-3-(4-(3-((5,7-dimethoxy-4-oxo-2-(3,4,5-trimethoxyphenyl)-4Hchromen-3-yl)oxy)propoxy)-3-methoxyphenyl)acrylamide | Synthesis of two intermediates, which are then combined using DMF and potassium carbonate. The first one is derived from FA, involving reaction with acetic anhydride in the presence of NaOH, then amidation through a reaction with a phenylamine in the presence of HOBt and EDCl and lastly dissolution in acetonitrile and hydrazine hydrate. The second is a myricitrin derivative occurring from reaction with DMF, potassium carbonate, and methyl iodide in the presence of hydrochloride and then with DMF and dibromoalkanes. | 67.92% | 22 | [107] |
| FA derivatives containing dithioacetal moiety (A) | 2a | 4-(bis((2-Hydroxyethyl)thio)methyl)-2-methoxyphenyl(E)-3-(4-acetoxy-3-methoxyphenyl)acrylate | Reaction of FA with acetic anhydride and NaOH towards O-acetyl FA, then reaction with thionyl chloride and mixing of the respective chloride with 1,2 dioxane, triethylamine, and hydroxy aldehyde. The synthesized intermediate was mixed with thiol, NaHSO4·SiO2, and dichloromethane towards the final product. | 69.30% | 17 | [34] |
| FA derivatives containing dithioacetal moiety (B) | 2y | Not given | Reaction of FA with acetic anhydride and NaOH towards O-acetyl FA, then reaction with thionyl chloride and mixing of the respective chloride with 1,2 dioxane, triethylamine, and hydroxy aldehyde. The synthesized intermediate was mixed with thiol, NaHSO4·SiO2, and dichloromethane towards the final product. | Not given | 8 | [34] |
| FA derivatives containing dithioacetal moiety (C) | 2s | Not given | Reaction of FA with acetic anhydride and NaOH towards O-acetyl FA, then reaction with thionyl chloride and mixing of the respective chloride with 1,2 dioxane, triethylamine, and hydroxy aldehyde. The synthesized intermediate was mixed with thiol, NaHSO4·SiO2, and dichloromethane towards the final product. | Not given | 2 | [34] |
| Trans-FA esters with a chalcone group | F3 | (E)-methyl-3-(4-(2-(4-((E)-3-(2-fluorophenyl)acryloyl)phenoxy)ethoxy)-3-methoxyphenyl)acrylate | Esterification of FA with the appropriate alcohol in the presence of sulfuric acid and reaction with potassium carbonate in butanone with the addition of 1,2, dibromoethane towards an intermediate compound. Reaction of 4-hydroxyacetophenone with the appropriate aromatic aldehyde and reaction of the product with the previously mentioned intermediate and potassium carbonate in dimethylformamide. | 92.60% | 35 | [108] |
| Trans-Fa derivatives containing acylhydrazone moiety | D4 | (E)-3-(4-(benzyloxy)-3-methoxyphenyl)-N’-(thiophen-2-ylmethylene)acrylohydrazide | Starting with trans-ferulic acid, through four steps, including substitution, using RX in potassium carbonate and dimethylformamide, hydrolysis, using KOH and methanol, hydrazinoly-sis, using hydroxybenzotriazole (HoBt/EDCl) in DMF, and condensation, involving an appropriate aldehyde and methanol. | 80.80% | 23 | [109] |
| DiFA | Diferulic acid | Fractionation of dehydrogenated polymers of FA by ultrafiltration (synthesized with horseradish peroxidase from FA). | Not given | n.d. | [110] | |
| TriFA | Triferulic acid | Fractionation of dehydrogenated polymers of FA by ultrafiltration (synthesized with horseradish peroxidase from FA). | Not given | n.d. | [110] | |
| FA 3-amino derivatives | MY3 | (E)-ethyl 3-(4-isopropoxy-3-methoxy-5-nitrophenyl)acrylate | Nitration of FA with acetic and nitric acid, esterification of the product with the corresponding alcohol in sulfuric acid, and mixture of the derived compound with sodium carbonate in DMF. Addition of the corresponding alkyl bromide and tetra-butylammonium iodide in DMF to the previously described solution to yield the final product. | 9% | 23 | [111] |
| Compound | Binding Energy 1 (kcal/mol) | No of Interactions | Total Contacting Residues | ||
|---|---|---|---|---|---|
| H-Bond 2 | Hydrophobic 3 | Pi-Pi | |||
| 7a | −6.67 | 1 (HIS 41) | 1 (MET 165) | 1 (HIS 41) | THR 25, THR 26, LEU 27, HIS 41, MET 49, LEU 141, ASN 142, GLY 143, CYS 145, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, ARG 188, GLN 189, THR 190, ALA 191, GLN 192 |
| 13b | −6.54 | 0 | 1 (GLN 189) | 0 | THR 26, LEU 27, HIS 41, MET 49, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, HIS 172, ASP 187, ARG 188, GLN 189, THR 190, ALA 191, GLN 192 |
| 4f | −6.27 | 3 (ASN 142, HIS 163, GLN 189) | 1 (GLN 189) | 1 (HIS 41) | THR 25, THR 26, LEU 27, HIS 41, VAL 42, MET 49, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, HIS 172, ASP 187, ARG 188, GLN 189 |
| 2 | −7.72 | 3 (THR 25, HIS 41, GLN 192) | 1 (THR 25) | 0 | THR 24, THR 25, THR 26, LEU 27, HIS 41, THR 45, MET 49, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, ARG 188, GLN 189, THR 190, GLN 192 |
| g18 | −6.91 | 0 | 1 (GLY 143) | 1 (HIS 41) | THR 24, THR 25, THR 26, LEU 27, HIS 41, MET 49, ASN 119, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, HIS 172, ARG 188, GLN 189, THR 190, ALA 191, GLN 192 |
| e27 | −8.11 | 2 (HIS 41, GLN 192) | 1 (GLN 189) | 1 (HIS 41) | THR 24, THR 25, THR 26, LEU 27, HIS 41, CYS 44, MET 49, PRO 52, TYR 54, GLY 143, CYS 145, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, ASP 187, ARG 188, GLN 189, THR 190, GLN 192 |
| e28 | −7.76 | 2 (HIS 41, GLN 192) | 1 (GLN 189) | 1 (HIS 41) | THR 25, THR 26, LEU 27, HIS 41, CYS 44, MET 49, PRO 52, TYR 54, GLY 143, CYS 145, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, ASP 187, ARG 188, GLN 189, THR 190, GLN 192 |
| 5 | −7.16 | 4 (THR 26, GLY 143, SER 144, CYS 145) | 1 (MET 49) | 1 (HIS 41) | THR 25, THR 26, LEU 27, HIS 41, MET 49, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, PRO 168, HIS 172, ARG 188, GLN 189, THR 190, GLN 192 |
| 4n | −7.82 | 2 (LEU 141, GLY 143) | 1 (MET 165) | 0 | LEU 27, HIS 41, SER 46, MET 49, TYR 54, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, PRO 168, HIS 172, ASP 187, ARG 188, GLN 189, THR 190, ALA 191 |
| 2a | −6.52 | 10 (THR 24, THR 45, THR 46 × 2, GLY 143, GLU 166, ARG 188, THR 190 × 2, GLN 192) | 1 (THR 25) | 0 | THR 24, THR 25, THR 26, HIS 41, CYS 44, THR 45, SER 46, MET 49, ASN 142, GLY 143, SER 144, CYS 145, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, ARG 188, GLN 189, THR 190, GLN 192 |
| 2y | −6.54 | 11 (HIS 41, THR 45, SER 46 × 3, LEU 141, ASN 142, GLY 143, SER 144 × 2, CYS 145) | 1 (HIS 41) | 1 (HIS 41) | THR 24, THR 25, THR 26, LEU 27, HIS 41, THR 45, SER 46, MET 49, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, GLN 189 |
| 2s | −6.67 | 0 | 1 (MET 165) | 1 (HIS 41) | THR 24, THR 25, THR 26, LEU 27, HIS 41, MET 49, TYR 54, ASN 142, GLY 143, CYS 145, HIS 164, MET 165, ASP 187, ARG 188, GLN 189 |
| F3 | −7.80 | 5 (THR 24, THR 25, THR 45 × 2, SER 46) | 1 (MET 165) | 2 (HIS 41 × 2) | THR 24, THR 25, THR 26, LEU 27, HIS 41, THR 45, SER 46, MET 49, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, ARG 188, GLN 189, THR 190 |
| D4 | −6.89 | 0 | 1 (MET 165) | 1 (HIS 41) | THR 25, THR 26, LEU 27, HIS 41, VAL 42, MET 49, LEU 50, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, PRO 168, HIS 172, GLN 189, THR 190, ALA 191 |
| diFA | −7.64 | 0 | 1 (HIS 41) | 1 (HIS 41) | THR 24, THR 25, THR 26, LEU 27, HIS 41, CYS 44, THR 45, SER 46, MET 49, TYR 54, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 164, MET 165, GLU 166, ASP 187, ARG 188, GLN 189 |
| triFA | −8.32 | 4 (THR 26, TYR 54 × 2, ASP 187) | 1 (MET 165) | 0 | THR 24, THR 25, THR 26, LEU 27, HIS 41, CYS 44, MET 49, PRO 52, TYR 54, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, ASP 187, ARG 188, GLN 189, THR 190, GLN 192 |
| MY3 | −6.29 | 4 (GLY 143, SER 144 × 2, GLN 189) | 1 (MET 165) | 0 | HIS 41, MET 49, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, HIS 172, PHE 181, VAL 186, ASP 187, ARG 188, GLN 189 |
| N3 | −8.26 | 4 (CYS 145, GLU 166, GLN 189) | 1 (MET 49) | 1(HIS 41) | THR 25, LEU 27, HIS 41, MET 49, LEU 50, TYR 54, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, HIS 172, ASP 187, ARG 188, GLN 189, THR 190, ALA 191, GLN 192 |
| GC376 | −7.80 | 5 (HIS 41, PHE 140, HIS 163, GLU 166, GLN 189) | 1 (ASP 187) | 0 | HIS 41, MET 49, TYR 54, PHE 140, LEU 141, ASN 142, GLY 143, SER 144, CYS 145, HIS 163, HIS 164, MET 165, GLU 166, LEU 167, PRO 168, HIS 172, ASP 187, ARG 188, GLN 189, THR 190, ALA 191, GLN 192 |
| Physicochemical Properties | Lipophilicity/Solubility | Bioavailability and Druglikeness | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Compound Name | Formula | MW 1 (g/mol) | RB 2 | HBA 3 | HBD 4 | Fraction C sp3 5 | TPSA 6 (Ų) | pKa of Most Basic/Acidic Group 7 | Log Po/w 8 | LogS 9 | Lipinski 10 | Bioavailability Score 11 | Druglikeness Score 12 |
| FA | C10H10O4 | 194.18 | 3 | 4 | 2 | 0.1 | 66.76 | <0./4.54 | 1.51 | −2.11 | Yes (0) | 0.85 | −0.61 |
| Methyl ferulate | C11H12O4 | 208.21 | 4 | 4 | 1 | 0.18 | 55.76 | <0./9.69 | 1.84 | −2.32 | Yes (0) | 0.55 | −0.76 |
| Ethyl ferulate | C12H14O4 | 222.24 | 5 | 4 | 1 | 0.25 | 55.76 | <0./9.69 | 2.2 | −2.55 | Yes (0) | 0.55 | −0.55 |
| Propyl ferulate | C13H16O4 | 236.26 | 6 | 4 | 1 | 0.31 | 55.76 | <0./9.69 | 2.73 | −2.89 | Yes (0) | 0.55 | −0.34 |
| Butyl ferulate | C14H18O4 | 250.29 | 7 | 4 | 1 | 0.36 | 55.76 | <0./9.69 | 3.09 | −3.12 | Yes (0) | 0.55 | −0.42 |
| Isobutyl ferulate | C14H18O4 | 250.29 | 6 | 4 | 1 | 0.36 | 55.76 | <0./9.69 | 3.17 | −3.24 | Yes (0) | 0.55 | −0.1 |
| Pentyl ferulate | C15H20O4 | 264.32 | 8 | 4 | 1 | 0.4 | 55.76 | <0./9.69 | 3.63 | −3.47 | Yes (0) | 0.55 | −0.51 |
| Isopentyl ferulate | C15H20O4 | 264.32 | 7 | 4 | 1 | 0.4 | 55.76 | <0./9.69 | 3.52 | −3.47 | Yes (0) | 0.55 | −0.01 |
| Prenyl ferulate | C15H18O4 | 262.3 | 6 | 4 | 1 | 0.27 | 55.76 | <0./9.69 | 3.34 | −3.41 | Yes (0) | 0.55 | −0.49 |
| Hexyl ferulate | C16H22O4 | 278.34 | 9 | 4 | 1 | 0.44 | 55.76 | <0./9.69 | 4.17 | −3.82 | Yes (0) | 0.55 | −0.51 |
| Octyl ferulate | C18H26O4 | 306.4 | 11 | 4 | 1 | 0.5 | 55.76 | <0./9.69 | 5.25 | −4.52 | Yes (0) | 0.55 | −0.51 |
| Dodecyl ferulate | C22H34O4 | 362.5 | 15 | 4 | 1 | 0.59 | 55.76 | <0./9.69 | 7.42 | −5.94 | Yes (0) | 0.55 | −0.51 |
| Octadecyl ferulate | C28H46O4 | 446.66 | 21 | 4 | 1 | 0.68 | 55.76 | <0./9.68 | 10.67 | −8.08 | Yes; (1, logP) | 0.55 | −0.51 |
| Oleyl ferulate | C28H44O4 | 444.65 | 20 | 4 | 1 | 0.61 | 55.76 | <0./9.69 | 9.74 | −7.55 | Yes (1, logP) | 0.55 | −0.45 |
| Glyceryl ferulate | C13H16O6 | 268.26 | 7 | 6 | 3 | 0.31 | 96.22 | <0./9.69 | 0.53 | −1.61 | Yes (0) | 0.55 | −0.05 |
| Diglyceryl ferulate | C16H22O8 | 342.34 | 11 | 8 | 4 | 0.44 | 125.68 | <0./9.70 | −0.23 | −1.28 | Yes (0) | 0.55 | −0.11 |
| Tocopheryl ferulate | C39H58O5 | 606.87 | 17 | 5 | 1 | 0.62 | 64.99 | <0./9.69 | 12.51 | −10.56 | No (2, MW, logP) | 0.17 | 1.14 |
| Sitosteryl ferulate | C39H58O4 | 590.88 | 11 | 4 | 1 | 0.72 | 55.76 | <0./9.69 | 11.61 | −10.19 | No (2, MW, logP) | 0.17 | 1.21 |
| D-glucose ferulate | C16H20O9 | 356.32 | 6 | 9 | 5 | 0.44 | 145.91 | <0./9.69 | −0.87 | −1.28 | Yes (0) | 0.55 | −0.15 |
| D-galactose ferulate | C16H20O9 | 356.32 | 6 | 9 | 5 | 0.44 | 145.91 | <0./9.69 | −0.87 | −1.28 | Yes (0) | 0.55 | −0.15 |
| D-mannose ferulate | C16H20O9 | 356.32 | 6 | 9 | 5 | 0.44 | 145.91 | <0./9.69 | −0.87 | −1.28 | Yes (0) | 0.55 | −0.15 |
| D-fructose ferulate | C16H20O9 | 356.32 | 7 | 9 | 5 | 0.44 | 145.91 | <0./9.69 | −0.56 | −1.41 | Yes (0) | 0.55 | −0.24 |
| L-arabinose ferulate | C15H18O8 | 326.3 | 6 | 8 | 4 | 0.4 | 125.68 | <0./9.69 | −0.25 | −1.5 | Yes (0) | 0.55 | −0.18 |
| D-xylose ferulate | C15H18O8 | 326.3 | 6 | 8 | 4 | 0.4 | 125.68 | <0./9.69 | −0.25 | −1.5 | Yes (0) | 0.55 | −0.18 |
| FOS ferulate 1 | C26H28O12 | 532.49 | 11 | 12 | 5 | 0.31 | 181.44 | <0./9.69 | 1.71 | −3.73 | No (2; MW, HBD) | 0.17 | 0.58 |
| D-lactose ferulate | C21H28O15 | 520.44 | 9 | 15 | 8 | 0.57 | 234.29 | <0./9.69 | −2.87 | −0.79 | No (3; MW, HBD, HBA) | 0.17 | −0.02 |
| D-sucrose ferulate | C22H30O14 | 518.47 | 10 | 14 | 8 | 0.59 | 225.06 | <0./9.69 | −1.98 | −1.27 | No (3; MW, HBD, HBA) | 0.17 | 0.01 |
| D-maltose ferulate | C22H30O14 | 518.47 | 10 | 14 | 8 | 0.59 | 225.06 | <0./9.69 | −3.01 | −0.69 | No (3; MW, HBD, HBA) | 0.17 | 0.03 |
| D-cellobiose ferulate | C22H30O14 | 518.47 | 9 | 14 | 8 | 0.59 | 225.06 | <0./9.69 | −3.01 | −0.69 | No (3; MW, HBD, HBA) | 0.17 | 0.03 |
| Xylobiose ferulate | C20H26O12 | 458.41 | 7 | 12 | 6 | 0.55 | 184.6 | <0./9.69 | −1.78 | −1.24 | No (2; HBD, HBA) | 0.17 | 0.33 |
| FOS ferulate 2 | C22H30O14 | 518.47 | 10 | 14 | 8 | 0.59 | 225.06 | <0./9.69 | −2.4 | −1.01 | No (3; MW, HBD, HBA) | 0.17 | 0.27 |
| Galactobiose ferulate | C32H38O17 | 694.63 | 14 | 17 | 8 | 0.44 | 260.59 | <0./9.69 | −0.74 | −2.94 | No (3; MW, HBD, HBA) | 0.17 | 0.03 |
| Arabinobiose ferulate | C31H36O14 | 632.61 | 14 | 14 | 5 | 0.42 | 199.9 | <0./9.69 | 1.22 | −3.8 | No (2; MW, HBA) | 0.17 | 0.07 |
| Raffinose ferulate | C29H42O18 | 678.63 | 13 | 18 | 10 | 0.69 | 283.98 | <0./12.89 | −3.58 | −1.03 | No; (3; MW, HBD, HBA) | 0.17 | −0.21 |
| FOS ferulate 3 | C58H64O28 | 1209.1 | 29 | 28 | 11 | 0.38 | 410.8 | <0./9.69 | 1.47 | −6.56 | No (3; MW, HBD, HBA) | 0.17 | 0.27 |
| d-mannitol ferulate | C16H22O9 | 358.34 | 10 | 9 | 6 | 0.44 | 156.91 | <0./9.69 | −1.32 | −0.75 | Yes (1; HBD) | 0.55 | −0.26 |
| d-sorbitol ferulate | C16H22O9 | 358.34 | 10 | 9 | 6 | 0.44 | 156.91 | <0./9.69 | −1.32 | −0.75 | Yes (1; HBD) | 0.55 | −0.26 |
| d-xylitol ferulate | C15H20O8 | 328.31 | 9 | 8 | 5 | 0.40 | 136.68 | <0./9.69 | −0.7 | −1.03 | Yes (0) | 0.55 | −0.26 |
| FA rutinoside | C23H32O13 | 516.49 | 9 | 13 | 7 | 0.61 | 204.83 | <0./4.07 | −1.81 | −1.43 | No (3; MW, HBD, HBA) | 0.11 | −0.22 |
| Compound 7a | C24H27NO4 | 393.48 | 12 | 4 | 1 | 0.29 | 56.79 | −1.12/15.25 | 3.96 | −4.29 | Yes (0) | 0.55 | 0.81 |
| Compound 13b | C22H24ClNO4 | 401.88 | 11 | 4 | 1 | 0.32 | 56.79 | −1.89/13.89 | 3.5 | −4.13 | Yes (0) | 0.55 | 0.92 |
| Compound 4f | C29H31NO5 | 473.56 | 14 | 5 | 1 | 0.28 | 66.02 | −1.89/13.89 | 4.33 | −4.96 | Yes (0) | 0.55 | 0.42 |
| Compound 2 | C21H23NO8S | 449.47 | 12 | 8 | 0 | 0.29 | 133.1 | <0./17.65 | 3.63 | −4.41 | Yes (0) | 0.55 | −0.54 |
| Compound g18 | C29H30ClF3NO6P | 611.97 | 15 | 9 | 1 | 0.28 | 92.9 | −5.09/12.64 | 6.18 | −6.86 | No (2; MW, logP) | 0.17 | 0.37 |
| Compound e27 | C26H22N2O6 | 458.46 | 9 | 7 | 0 | 0.12 | 88.88 | 2.31/25.16 | 4.43 | −5.36 | Yes (0) | 0.55 | 0.59 |
| Compound e28 | C29H26N2O6 | 498.53 | 11 | 7 | 0 | 0.14 | 88.88 | 2.31/19.29 | 5.5 | −6.11 | Yes (0) | 0.55 | 0.54 |
| Compound 5 | C32H34N2O7 | 558.62 | 10 | 7 | 2 | 0.28 | 98.72 | 6.30/9.69 | 5.28 | −6.33 | Yes (1; MW) | 0.55 | 1.4 |
| Compound 4n | C39H38BrNO11 | 776.62 | 17 | 11 | 1 | 0.23 | 133.15 | 1.05/13.50 | 7.16 | −8.44 | No (2; MW, HBA) | 0.17 | 0.6 |
| Compound 2a | C26H32O8S2 | 536.66 | 17 | 8 | 2 | 0.38 | 162.12 | <0./15.39 | 3.44 | −4.46 | Yes (1; MW) | 0.55 | 0.84 |
| Compound 2y | C23H26O7S2 | 478.58 | 14 | 7 | 2 | 0.30 | 152.89 | <0./15.39 | 3.34 | −4.26 | Yes (0) | 0.55 | 0.45 |
| Compound 2s | C18H16O2S2 | 328.45 | 5 | 2 | 0 | 0.17 | 76.9 | <0./25.90 | 4.76 | −4.95 | Yes (1; logP) | 0.55 | 0.05 |
| Compound F3 | C28H25FO6 | 476.49 | 12 | 7 | 0 | 0.14 | 71.06 | <0./27.89 | 5.68 | −5.96 | Yes (0) | 0.55 | 0.02 |
| Compound D4 | C22H20N2O3S | 392.47 | 9 | 4 | 1 | 0.09 | 88.16 | 1.11/13.72 | 4.71 | −5.1 | Yes (0) | 0.55 | −0.42 |
| DiFA | C20H18O8 | 386.35 | 7 | 8 | 4 | 0.10 | 133.52 | <0./4.54 | 2.69 | −3.79 | Yes (0) | 0.56 | 0 |
| TriFA | C29H26O10 | 534.51 | 10 | 10 | 3 | 0.17 | 140.98 | <0./4.54 | 4.16 | −5.46 | Yes (1; MW) | 0.56 | 0.32 |
| Compound MY3 | C16H21NO4 | 291.34 | 7 | 4 | 0 | 0.44 | 72.12 | <0./20.14 | 4.32 | −4.12 | Yes (0) | 0.55 | −0.61 |
| Compound Name | GI Absorption 1 | BBB 2 Permeant | P-gp Substrate 3 | CYP1A2 Inhibitor | CYP2C19 Inhibitor | CYP2C9 Inhibitor | CYP2D6 Inhibitor | CYP3A4 Inhibitor | Log Kp 4 (cm/s) | LD50 5 (mg/kg) | Hepatotoxicity | Carcinogenicity | Mutagenicity | Cytotoxicity | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A 6 | P 7 | A | P | A | P | A | P | |||||||||||
| FA | High | Yes | No | No | No | No | No | No | −6.41 | 1772 | 0.51 | 0.61 | 0.96 | 0.88 | ||||
| Methyl ferulate | High | Yes | No | No | No | No | No | No | −6.26 | 978 | 0.56 | 0.67 | 0.89 | 0.94 | ||||
| Ethyl ferulate | High | Yes | No | Yes | No | No | No | No | −6.09 | 978 | 0.67 | 0.73 | 0.82 | 0.91 | ||||
| Propyl ferulate | High | Yes | No | Yes | Yes | No | No | No | −5.8 | 978 | 0.6 | 0.77 | 0.81 | 0.87 | ||||
| Butyl ferulate | High | Yes | No | Yes | Yes | No | No | No | −5.63 | 9600 | 0.6 | 0.78 | 0.8 | 0.86 | ||||
| Isobutyl ferulate | High | Yes | No | Yes | Yes | No | No | No | −5.58 | 978 | 0.6 | 0.7 | 0.81 | 0.84 | ||||
| Pentyl ferulate | High | Yes | No | Yes | Yes | No | No | No | −5.34 | 9600 | 0.72 | 0.74 | 0.77 | 0.85 | ||||
| Isopentyl ferulate | High | Yes | No | Yes | Yes | No | No | No | −5.41 | 9600 | 0.53 | 0.69 | 0.79 | 0.81 | ||||
| Prenyl ferulate | High | Yes | No | Yes | Yes | No | No | No | −5.53 | 978 | 0.57 | 0.68 | 0.7 | 0.75 | ||||
| Hexyl ferulate | High | Yes | No | Yes | Yes | No | No | No | −5.04 | 9600 | 0.8 | 0.76 | 0.72 | 0.82 | ||||
| Octyl ferulate | High | Yes | No | Yes | No | Yes | Yes | No | −4.44 | 9600 | 0.8 | 0.76 | 0.72 | 0.82 | ||||
| Dodecyl ferulate | High | No | No | Yes | No | Yes | Yes | No | −3.24 | 9600 | 0.8 | 0.76 | 0.72 | 0.82 | ||||
| Octadecyl ferulate | Low | No | No | No | Yes | No | No | No | −1.45 | 9600 | 0.8 | 0.76 | 0.72 | 0.82 | ||||
| Oleyl ferulate | Low | No | No | No | No | No | No | Yes | −2.1 | 9600 | 0.8 | 0.76 | 0.72 | 0.82 | ||||
| Glyceryl ferulate | High | No | No | No | No | No | No | No | −7.56 | 978 | 0.89 | 0.83 | 0.76 | 0.86 | ||||
| Diglyceryl ferulate | High | No | No | No | No | No | No | No | −8.55 | 978 | 0.9 | 0.83 | 0.77 | 0.83 | ||||
| Tocopheryl ferulate | Low | No | Yes | No | No | No | No | No | −1.12 | 5000 | 0.74 | 0.68 | 0.73 | 0.81 | ||||
| Sitosteryl ferulate | Low | No | No | No | No | No | No | No | −1.66 | 9600 | 0.74 | 0.66 | 0.93 | 0.79 | ||||
| D-glucose ferulate | Low | No | No | No | No | No | No | No | −9.09 | 5000 | 0.78 | 0.8 | 0.77 | 0.83 | ||||
| D-galactose ferulate | Low | No | No | No | No | No | No | No | −9.09 | 5000 | 0.78 | 0.8 | 0.77 | 0.83 | ||||
| D-mannose ferulate | Low | No | No | No | No | No | No | No | −9.09 | 5000 | 0.78 | 0.8 | 0.77 | 0.83 | ||||
| D-fructose ferulate | Low | No | No | No | No | No | No | No | −8.87 | 5000 | 0.89 | 0.84 | 0.74 | 0.82 | ||||
| L-arabinose ferulate | High | No | No | No | No | No | No | No | −8.47 | 5000 | 0.76 | 0.76 | 0.69 | 0.85 | ||||
| D-xylose ferulate | High | No | No | No | No | No | No | No | −8.47 | 5000 | 0.76 | 0.76 | 0.69 | 0.85 | ||||
| FOS ferulate 1 | Low | No | Yes | No | No | No | No | No | −8.33 | 5000 | 0.87 | 0.84 | 0.77 | 0.76 | ||||
| D-lactose ferulate | Low | No | No | No | No | No | No | No | −11.51 | 5000 | 0.75 | 0.81 | 0.69 | 0.72 | ||||
| D-sucrose ferulate | Low | No | No | No | No | No | No | No | −10.87 | 5000 | 0.87 | 0.83 | 0.77 | 0.79 | ||||
| D-maltose ferulate | Low | No | No | No | No | No | No | No | −11.6 | 5000 | 0.81 | 0.81 | 0.79 | 0.78 | ||||
| D-cellobiose ferulate | Low | No | No | No | No | No | No | No | −11.6 | 5000 | 0.81 | 0.81 | 0.79 | 0.78 | ||||
| Xylobiose ferulate | Low | No | No | No | No | No | No | No | −10.36 | 5000 | 0.77 | 0.76 | 0.8 | 0.75 | ||||
| FOS ferulate 2 | Low | No | No | No | No | No | No | No | −11.17 | n.a. | 0.91 | 0.84 | 0.77 | 0.77 | ||||
| Galactobiose ferulate | Low | No | Yes | No | No | No | No | No | −11.06 | 5000 | 0.83 | 0.8 | 0.81 | 0.79 | ||||
| Arabinobiose ferulate | Low | No | Yes | No | No | No | No | No | −9.29 | 5000 | 0.77 | 0.74 | 0.78 | 0.76 | ||||
| Raffinose ferulate | Low | No | No | No | No | No | No | No | −12.98 | 5000 | 0.87 | 0.86 | 0.79 | 0.77 | ||||
| FOS ferulate 3 | Low | No | Yes | No | No | No | No | No | −12.63 | n.a. | 0.88 | 0.83 | 0.76 | 0.73 | ||||
| D-mannitol ferulate | Low | No | No | No | No | No | No | No | −9.42 | 9600 | 0.87 | 0.86 | 0.77 | 0.84 | ||||
| D-sorbitol ferulate | Low | No | No | No | No | No | No | No | −9.42 | 9600 | 0.87 | 0.86 | 0.77 | 0.84 | ||||
| D-xylitol ferulate | Low | No | No | No | No | No | No | No | −8.8 | 9600 | 0.9 | 0.87 | 0.77 | 0.84 | ||||
| FA rutinoside | Low | No | No | No | No | No | No | No | −10.74 | 4000 | 0.82 | 0.86 | 0.82 | 0.73 | ||||
| Compound 7a | High | Yes | Yes | Yes | No | Yes | Yes | Yes | −5.89 | 1500 | 0.76 | 0.53 | 0.69 | 0.78 | ||||
| Compound 13b | High | Yes | Yes | Yes | Yes | Yes | Yes | Yes | −6.27 | 1200 | 0.83 | 0.59 | 0.73 | 0.7 | ||||
| Compound 4f | High | Yes | Yes | No | Yes | Yes | Yes | Yes | −6.11 | 5300 | 0.88 | 0.56 | 0.72 | 0.74 | ||||
| Compound 2 | Low | No | Yes | No | Yes | Yes | Yes | Yes | −6.46 | 1000 | 0.51 | 0.66 | 0.69 | 0.72 | ||||
| Compound g18 | Low | No | Yes | No | Yes | Yes | Yes | Yes | −5.65 | 1500 | 0.67 | 0.65 | 0.66 | 0.72 | ||||
| Compound e27 | High | No | No | No | Yes | Yes | No | Yes | −5.95 | 1000 | 0.76 | 0.52 | 0.53 | 0.63 | ||||
| Compound e28 | High | No | No | No | Yes | Yes | No | Yes | −5.44 | 1000 | 0.75 | 0.51 | 0.55 | 0.62 | ||||
| Compound 5 | High | No | Yes | No | Yes | Yes | No | No | −5.96 | 600 | 0.86 | 0.57 | 0.58 | 0.57 | ||||
| Compound 4n | Low | No | No | No | No | No | No | No | −5.95 | 5000 | 0.51 | 0.52 | 0.6 | 0.59 | ||||
| Compound 2a | Low | No | No | No | Yes | No | Yes | No | −7.13 | 1772 | 0.84 | 0.68 | 0.81 | 0.79 | ||||
| Compound 2y | Low | No | No | No | Yes | Yes | Yes | No | −6.85 | 1000 | 0.76 | 0.75 | 0.84 | 0.79 | ||||
| Compound 2s | High | No | No | Yes | Yes | Yes | No | No | −4.92 | 3150 | 0.54 | 0.55 | 0.74 | 0.74 | ||||
| Compound F3 | High | No | Yes | No | No | Yes | No | Yes | −5.17 | 2100 | 0.58 | 0.68 | 0.82 | 0.62 | ||||
| Compound D4 | High | No | No | Yes | Yes | Yes | No | Yes | −5.35 | 3506 | 0.61 | 0.59 | 0.52 | 0.72 | ||||
| DiFA | High | No | No | No | No | No | No | No | −6.75 | 1100 | 0.52 | 0.67 | 0.83 | 0.63 | ||||
| TriFA | Low | No | No | No | No | Yes | No | No | −6.61 | 1772 | 0.65 | 0.51 | 0.58 | 0.79 | ||||
| Compound MY3 | High | Yes | No | Yes | Yes | No | No | No | −5.01 | 5000 | 0.64 | 0.6 | 0.61 | 0.71 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Antonopoulou, I.; Sapountzaki, E.; Rova, U.; Christakopoulos, P. The Inhibitory Potential of Ferulic Acid Derivatives against the SARS-CoV-2 Main Protease: Molecular Docking, Molecular Dynamics, and ADMET Evaluation. Biomedicines 2022, 10, 1787. https://doi.org/10.3390/biomedicines10081787
Antonopoulou I, Sapountzaki E, Rova U, Christakopoulos P. The Inhibitory Potential of Ferulic Acid Derivatives against the SARS-CoV-2 Main Protease: Molecular Docking, Molecular Dynamics, and ADMET Evaluation. Biomedicines. 2022; 10(8):1787. https://doi.org/10.3390/biomedicines10081787
Chicago/Turabian StyleAntonopoulou, Io, Eleftheria Sapountzaki, Ulrika Rova, and Paul Christakopoulos. 2022. "The Inhibitory Potential of Ferulic Acid Derivatives against the SARS-CoV-2 Main Protease: Molecular Docking, Molecular Dynamics, and ADMET Evaluation" Biomedicines 10, no. 8: 1787. https://doi.org/10.3390/biomedicines10081787
APA StyleAntonopoulou, I., Sapountzaki, E., Rova, U., & Christakopoulos, P. (2022). The Inhibitory Potential of Ferulic Acid Derivatives against the SARS-CoV-2 Main Protease: Molecular Docking, Molecular Dynamics, and ADMET Evaluation. Biomedicines, 10(8), 1787. https://doi.org/10.3390/biomedicines10081787








