Abstract
Low birth weight (LBW) and accelerated growth during lactation are associated with cardiometabolic disease development. LBW offspring from rats exposed to undernutrition during gestation (MUN) develops hypertension. In this rat model, we tested if slower postnatal growth improves early cardiometabolic alterations. MUN dams were fed ad libitum during gestation days 1–10, with 50% of the daily intake during days 11–21 and ad libitum during lactation. Control dams were always fed ad libitum. Pups were maintained with their own mother or cross-fostered. Body weight and length were recorded weekly, and breastmilk was obtained. At weaning, the heart was evaluated by echocardiography, and aorta structure and adipocytes in white perivascular fat were studied by confocal microscopy (size, % beige-adipocytes by Mitotracker staining). Breastmilk protein and fat content were not significantly different between groups. Compared to controls, MUN males significantly accelerated body weight gain during the exclusive lactation period (days 1–14) while females accelerated during the last week; length growth was slower in MUN rats from both sexes. By weaning, MUN males, but not females, showed reduced diastolic function and hypertrophy in the heart, aorta, and adipocytes; the percentage of beige-type adipocytes was smaller in MUN males and females. Fostering MUN offspring on control dams significantly reduced weight gain rate, cardiovascular, and fat hypertrophy, increasing beige-adipocyte proportion. Control offspring nursed by MUN mothers reduced body growth gain, without cardiovascular modifications. In conclusion, slower growth during lactation can rescue early cardiovascular alterations induced by fetal undernutrition. Exclusive lactation was a key period, despite no modifications in breastmilk macronutrients, suggesting the role of bioactive components. Our data support that lactation is a key period to counteract cardiometabolic disease programming in LBW and a potential intervention window for the mother.
1. Introduction
Adverse environmental conditions during the intrauterine period increase the risk to develop cardiometabolic diseases (CMD), a process known as fetal programming [,]. Exposure to the fetus to insufficient nutrients is one of the key programming factors, widely demonstrated in human populations by the association between low birth weight (LBW) and higher rates of hypertension, coronary heart disease, or type 2 diabetes mellitus [,,]. Fetal programming has also been validated in animal models [,,]. The postnatal period seems to be a second critical window for programming, particularly after exposure to a fetal stressor. During this period, LBW individuals frequently experience a rapid weight gain, and compelling evidence indicates that this growth pattern is also deleterious. Adolescents born prematurely with a quick postnatal growth have a lower flow-mediated-endothelial dilatation compared to those with slower weight gain and a higher risk of hypertension []; quick growth and elevated central adiposity in infancy also contribute to the future development of metabolic disorders [,]. A systematic review highlights that rapid postnatal catch-up growth is a more important factor than LBW alone for the development of cardiovascular disease and its risk factors [].
Nutrition in LBW individuals represents a challenge to ensure a postnatal growth pattern adequate to achieve brain and bone development while preventing CMD []. In this context, the lactation period has been proposed as a critical window to counteract alterations initiated during fetal life [], since human breast milk is recognized as the gold standard for infant nutrition tailored to provide the nutrients and bioactive factors for healthy growth []. Breastfeeding provides protection against CMD, is associated with lower blood pressure levels and a lower risk of overweight in children [,], and a systematic review evidences slower rates of weight gain in preterm and LBW infants fed with breastmilk compared to the formula [].
Animal models provide the tools to analyze the influence of both intrauterine and lactation periods in a controlled environment. In a rat model of fetal programming induced by maternal undernutrition during gestation (MUN), we have demonstrated that LBW offspring accelerate growth during lactation, reaching the same body weight as control counterparts by wearing. This catch-up trajectory in MUN rats leads to excessive growth of cardiovascular organs in males [,] and white adipose tissue (WAT) deposits in both sexes [].
In this study, we aim to demonstrate in an animal model of LBW if a slower growth during the lactation period can rescue the cardiometabolic alterations induced by undernutrition. To test this hypothesis, in MUN rats we have modified the lactation environment using a cross-fostering protocol and analyzed the impact on (1) body weight and length growth pattern during the first three weeks of postnatal life, (2) milk macronutrient composition, and (3) heart, aorta and perivascular adipose tissue growth and cardiac function at weaning, assessing the influence of sex in the abovementioned parameters.
2. Materials and Methods
Experiments were performed on Sprague Dawley rats from the colony bred at the Animal House of Universidad Autónoma de Madrid (ES-28079-0000097). This study was performed in accordance with European Union Guidelines for the Care and Use of Laboratory Animals (Directive 2010/63/EU and Spanish RD 1201/2005) and was approved by the Ethics Review Board of Universidad Autónoma de Madrid and by the local government (Comunidad Autónoma de Madrid, Spain; PROEX 004-19, approved on 7 May 2019).
The rats were housed in buckets 36.5 × I21.5 × 18.5 cm (length×width×height) on aspen wood bedding, maintained under controlled conditions of temperature and 12/12 light/dark photoperiod, and the welfare of the animals was monitored daily by staff. The animals were fed with a EuroRodent breeding diet (5LF5; Labdiet, Madrid, Spain) containing 22.0% protein, 4.4% fat, 55.0% carbohydrates, 4.1% fiber, and 5.4% mineral (sodium content 0.26%) and drinking water were provided ad libitum.
2.1. Maternal Undernutrition (MUN) Model and Cross-Fostering Protocol
We used a rat model of fetal programming induced by maternal global nutrient restriction during the second part of gestation, as previously described []. After observation of sperm in the vaginal smear (gestation = day 0) the dam was allocated to either MUN or the control group. Control dams were fed ad libitum throughout pregnancy and lactation; MUN dams were fed ad libitum from day 1–10 and with 50% of the averaged control daily intake (previously calculated as 24 g/day) from day 11 to the end of gestation, returning to ad libitum diet during lactation. 24 h after birth the pups were sexed and weighed individually and the litter was standardized to 12 individuals, 6 males, and 6 females if possible (smaller litters were not used for this work, being used for other studies). Control and MUN litters were left with their mothers or cross-fostered.
Cross-fostering protocol. We used a protocol similar to [] with some modifications. Two dams were mated at the same time, ensuring the same gestation day 0, and those with birth on the same day were cross-fostered. On postnatal day 1, the entire litter was exchanged to the foster’s dam cage with bedding from the original mother to avoid rejection. The litter was standardized to 12 individuals and the pups were sexed. The rats were not individually marked to help acceptance (no rejection was detected in any of the groups).
The name of the groups was “pup type–on–mother type” (i.e., M-on-C refers to a pup from a MUN dam fostered by a control mother). Four experimental groups were studied: control-on-control (C-on-C; n = 6 mothers), MUN-on-MUN (M-on-M; n = 6 mothers); control-on-MUN (C-on-M, n = 4 mothers), MUN-on-control (M-on-C; n = 4 mothers).
2.2. Experimental Protocols
The entire offspring from the four groups were weighted and head-to-tail length measured at days 1, 14, and 21 of the lactation periods with an analytical balance (Conecta, Barcelona, Spain) and a digital caliper (Conecta, Barcelona, Spain), respectively. The body weight gain from day 1 to 14 was calculated as Formula (1). A similar formula was used to assess body weight gain during the last week and length gain in both lactation periods. Weigh gain was expressed as g/day and length gain as cm/day.
Breast milk was collected from MUN and control dams on days 12 and 14 of lactation (see protocol below). On day 21 (weaning), 1–2 males and 1–2 females from each litter were studied and the remaining animals were used for other studies according to the 3Rs rule for experimental animals. Firstly, cardiac structure and function were evaluated by echocardiography. Thereafter, the rats were placed in a CO2 chamber and killed by exsanguination. Then, the thoracic aorta and mesenteric bed were removed and stored in a cold saline solution. The aorta was cleaned, and the aortic arch and immediate region were fixed in 4% paraformaldehyde solution (PFA). Perivascular adipocytes from the mesenteric bed were also dissected and fixed in PFA. Both tissues were stored for later confocal microscopy analysis. Figure 1 shows a summary of experimental protocols.
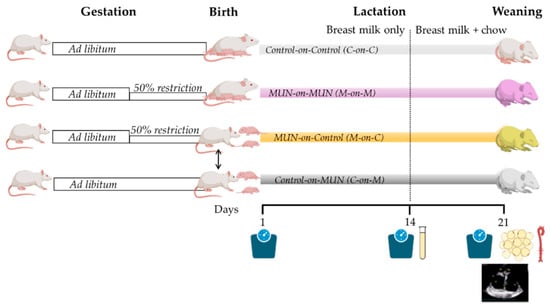
Figure 1.
Experimental protocol diagram. MUN, maternal undernutrition during gestation; C-on-C, control pups fostered by a control mother (n = 6 dams); M-on-M, MUN rats fostered by their own mothers (n = 6 dams); C-on-M control rats fostered by a MUN mother (n = 4 dams); MUN-on-C, MUN rats fostered by a control mother (n = 4 dams).
2.3. Breast Milk Collection and Measurements
Breast milk was collected on day 12th and day 14th of lactation (the period of maximal milk yield) and was pooled, allowing the mother and pups to recover during day 13. On the day of collection, the pups were separated from the mother for 3 h; the dam was anesthetized with isoflurane inhalation anesthesia (1000 mg/g; Isoflutek, Karizoo Lab., Barcelona, Spain) and injected with 0.1–0.15 mL of oxytocin i.p. depending on rat body weight (10 UI/mL; Syntocinon, Mylan Products Ltd., Hertfordshire, UK). A 1.0–1.5 mL volume of breast milk was obtained by gentle massage of the mammary glands and collection by a glass micropipette in Eppendorf tubes. The dam was milked for a maximum of 1 h. Each breastmilk sample was divided into two aliquots, one to assess total fat and the second one to assess total proteins.
Total fat content. Fat was analyzed by the Mojonnier method [] with modifications. Briefly, a 0.5 mL volume of breast milk was mixed with 0.5 mL of ammonium hydroxide, followed by the addition of 50 µL of ethanolic phenolphthalein solution (0.5% w/v) and shaken. Thereafter, 2.5 mL of ethanol, 2.5 mL of petroleum ether, and 2.5 mL of ethyl ether were added and vigorously mixed for 30 s. Thereafter, the mix was centrifuged at 4000× g (3 min, RT) and the upper phase containing the fat was stored. This process was repeated three times with the remaining aqueous phase, adding the ethanol, ethyl ether, and petroleum ether. Thereafter, the fat from the 3 centrifugation was pooled, and to evaporate the ether solvent, it was placed overnight in a gravity convection oven at 50 °C, uncapped. Finally, the total fat content in the sample was measured by gravimetry and expressed as mg/mL of BM. A blank reaction was performed by substituting the 0.5 mL breast milk volume with H2O-Q.
Total protein level. Protein quantification was carried out in the defatted phase of breast milk using the Bradford method []. It has to be noted that centrifugated breast milk samples continue to contain proteins such as caseins. Briefly, 10 µL of BM (1:50 v/v in H2O-Q) were mixed in a microplate with a 200 µL volume of Coomassie-blue dye (1:4 v/v in H2O-Q; Bio-Rad Lab., Hercules, CA, USA). After shaking the mix for 1 min, the absorbance was measured at 595 nm in a microplate reader (Synergy HT Multimode; BioTek Instruments, Winooski, VT, USA). Total protein levels were expressed as mg of BSA/mL. BSA (Sigma-Aldrich, St. Louis, MO, USA) was used for the standard curve (range 0.1–0.5 mg/mL) and Coomassie-blue dye was substituted by H2O-Q for the blank curve.
2.4. Transthoracic Echocardiography
Transthoracic echocardiography was performed in 21 days-old rats using the VIVID q-system (GE Healthcare, Munich, Germany) equipped with a 13 MHz probe (12S-RS, GE Healthcare, Munich, Germany) as previously described []. Briefly, the rats were anesthetized by i.p injection with 80 mg/kg Ketamine hydrochloride (AuroMedics Pharma LLC., Dublin, Ireland) and 10 mg/kg Diazepam (Hospira, Inc., Lake Forest, IL, USA). The images were acquired with the animals in left lateral decubitus. M-mode imaging of the parasternal short-axis (papillary level) view allowed measurement of end-diastolic (mm) and end-systolic (mm) internal diameter, posterior wall thickness (mm), and interventricular septum thickness (mm) at diastole. Additionally, it was calculated the systolic functionality as the ejection fraction (%). The pulsed-wave Doppler early-to-late transmitral peak diastolic flow velocity ratio (E/A ratio; arbitrary units) was measured to assess diastolic function (E, mitral peak early-filling velocity and A, mitral peak flow velocity at atrial contraction). The transmitral flow velocity profile was determined by positioning a sample volume at the tip of the mitral valve on the para-apical long-axis view. The E-wave deceleration time was measured as the time interval between peak E-wave velocity and the point where the descending E-wave (or its extrapolation) intercepted the zero line. Values were determined by averaging the measurements of three consecutive cardiac cycles.
2.5. Aorta Structure by Confocal Microscopy
Aorta structure was assessed in a ring cut from the PFA fixed thoracic aorta proximal to the aortic arch. The ring was mounted intact on a slide provided with a small well, to avoid compression containing Citifluor AF2 mounting medium (Aname, Madrid, Spain), as previously described []. The ring was visualized with a ×20 objective with a laser scanning confocal microscope (Leica TCS SP2, Leica Microsystems, Barcelona, Spain) at Excitation = 488 nm/Emission = 500–560 nm, the wavelength at which elastin can be detected by its autofluorescence allowing to detect the medial layer. Single images were captured with a ×20 air objective, ensuring the elastic lamellae were clearly visible. Quantification was performed with FIJI software [], measuring internal and external perimeters (µm); from these measurements medial cross-sectional areas (CSAs) were calculated in μm2, assuming the sections were circular.
2.6. Adipocyte Size and Browning
PFA-fixed adipocytes from the perivascular tissue of the mesenteric bed were incubated with Mitotracker red FM (Invitrogen, ThermoFisher, Madrid, Spain) prepared in phosphate buffer saline (PBS) to stain mitochondria-positive cells [], evaluating the percentage of beige adipocytes, since they are rich in mitochondria. Adipocytes were incubated for 60 min (1:4000 v/v, RT, darkness) and washed 3 times for 10 min in PBS. Thereafter, they were incubated for 15 min in a solution of DAPI (Invitrogen, ThermoFisher, Madrid, Spain) to stain nuclei (1:500 v/v from stock solution, RT, darkness,) followed by 3 washes in PBS for 10 min each at RT. The samples were mounted intact on a slide with a small well and were visualized with a Laser Scanning Confocal Microscope (Leica TCS SP2, Leica Microsystems, Barcelona, Spain). Five regions were randomly chosen based on DAPI wavelength and single images were captured with a ×40 objective at three wavelengths: Excitation = 405 nm/Emission = 410–475 nm to visualize nuclei, Excitation = 488 nm/Emission = 500–560 nm to visualize adipocyte size by autofluorescence [], and Excitation = 581 nm/Emission = 644 nm to visualize mitochondria-positive cells.
The quantification of adipocyte size and proportion of mitochondria-positive cells was performed by FIJI software. The total number and area occupied by the adipocytes were quantified in the Excitation = 488 nm/Emission = 500–560 nm wavelength images (autofluorescence), and the average adipocyte size was calculated in each image. To assess Mitotracker-positive cells in perivascular WAT, the area occupied by adipocytes was measured in autofluorescent images, Mitotracker-positive areas were measured in the same region in the red wavelength images, and the percentage was calculated.
2.7. Statistical Analysis
Statistical analysis was performed with R software (version 3.6.0, 2018, R Core Team, Vienna; Austria) within the R Studio interface using rio, dplyr, compareGroups, ggpubr, devtools, and ggplot2 packages. Data was expressed as the median and interquartile range [Q1; Q3]. The differences in macronutrients of breast milk between control and MUN were performed by Mann-Whitney’s U test. The Kruskal–Wallis test by ranks was used to test the independent experimental groups. The significant Kruskal–Wallis test was used with Dunn’s test with directed pairwise comparison using C-on-C as a reference group. Second, it was considered the comparison between M-on-M versus M-on-C to determine, if pups with prior fetal programming, the lactation could reverse the modification. A p-value (p) < 0.05 was considered significant.
3. Results
3.1. Proteins and Fats in Breast Milk
No differences between control and MUN were detected in breast milk proteins (Control = 125.0 [113.0; 129.0] mg eq. BSA/mL, n = 12 rats; MUN = 117.0 [111.0; 123.0] mg eq. BSA/mL, n = 10 rats; p-Value=0.539). Fat levels in MUN milk tended to be lower but did not reach statistical significance (Control = 98.5 [89.3; 113.0] mg/mL, n = 12 rats; MUN = 84.0 [66.7; 107.0] mg/mL, n = 10 rats; p-Value = 0.090).
3.2. Body Growth Gain
From day 1 to 14 of lactation (exclusive lactation period), male rats from the M-on-M group exhibited a significantly higher increase in body weight gain compared to the C-on-C group. MUN males fostered by a C mother (M-on-C group) did not show differences compared C-on-C group, being significantly smaller compared to M-on-M males. Males from the C-on-M group had a significantly lower body weight gain compared to C-on-C (Figure 2A). By contrast, during the first lactation period, M-on-M female rats did not show differences in body weight gain compared to C-on-C or compared to M-on-C. As observed in males, control females nourished by a MUN mother (C-on-M) showed a lower body weight gain compared to C-on-C females (Figure 2A).
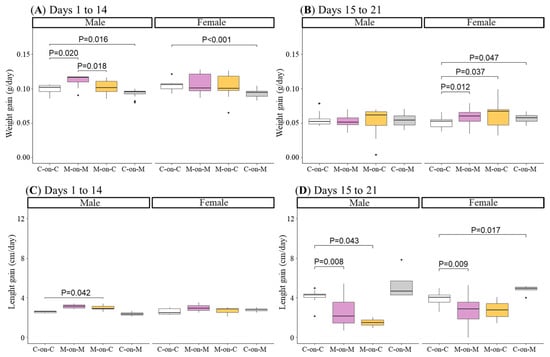
Figure 2.
Body weight from day 1 to 14 of lactation (A) and from day 15 to 21 of lactation (B), and body length gain from day 1 to 14 of lactation (C) and from day 15 to 21 of lactation (D) in male and female rats from MUN and Control mothers. MUN, maternal undernutrition during gestation; C-on-C, control pups fostered by their mothers (34 males and 38 females); M-on-M, MUN rats fostered by their mothers (32 males and 40 females); C-on-M, control rats fostered by MUN mothers (21 males and 27 females); M-on-C, MUN rats fostered by a control mother (25 males and 23 females). Data show the median and interquartile range [Q1; Q3] and the showed p-Value (P) was extracted from Dunnett’s post-hoc pairwise comparison test when the Kruskal-Wallis test was P < 0.05. Dots show outliers.
From day 15 to 21, when the pups suckle from mothers and eat by themselves, male M-on-M did not show statistical differences in body weight gain compared to C-on-C, or M-on-C males. However, M-on-M females accelerated growth during this period, as shown by the higher weight gain compared to C-on-C female rats. M-on-C rats also had higher weight gain compared to C-on-C females (Figure 2B).
From day 1 to 14, males of M-on-M length gain tended to be smaller compared to the C-on-C group but did not reach statistical significance (p-Value = 0.083). Cross-fostered MUN males (M-on-C) had a significantly higher length gain compared to the C-on-C group. In female rats, no differences were detected in any of the experimental groups in length gain during the exclusive lactation period (Figure 2C).
From day 15 to 21 length gain was significantly lower in M-on-M males and females compared to C-on-C control sex-matched counterparts. M-on-C males maintained a lower length gain, while M-on-C females improved the length rate, not significantly different from C-on-C females (Figure 2D).
3.3. Perivascular Adipocyte Size and Type
WAT adipocyte size was assessed in perivascular fat from the mesenteric bed obtained from 21-day-old offspring. M-on-M males had significantly larger adipocytes compared to C-on-C rats (Figure 3A). Adipocytes from MUN males fostered by a control mother (M-on-C) were of similar size compared to C-on-C males and significantly smaller compared to M-on-M. Control males fostered by a MUN mother (C-on-M) also showed smaller adipocytes size compared to C-on-C males (Figure 3A).
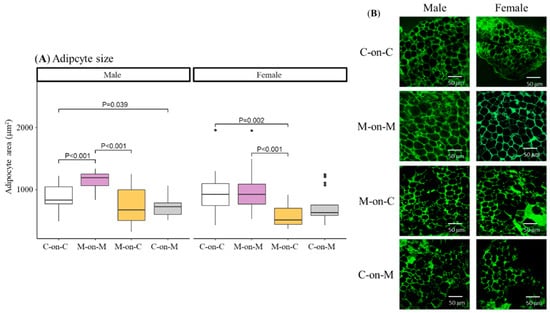
Figure 3.
Average size of perivascular adipocytes (A) and representative images obtained by confocal microscopy (B) of 21-day-old male and female offspring from MUN and Control mothers. MUN, maternal undernutrition during gestation; C-on-C, control pups fostered by their mothers (6 males and 6 females); M-on-M, MUN rats fostered by their mothers (6 males and 6 females); C-on-M, control rats fostered by MUN mothers (6 males and 6 females); M-on-C, MUN rats fostered by a control mother (6 males and 6 females). Data show the median and interquartile range [Q1; Q3], and the showed p-Value (P) was extracted from Dunnett’s post-hoc pairwise comparison test when the Kruskal-Wallis test was P < 0.05. Images were acquired with a Leica TCS SP2 confocal microscope, ×40 objective at Ex = 488 nm/Em = 500–560 nm wavelength; scale bar = 50 μm. Dots shown outliers.
Regarding females, M-on-M rats had similar adipocytes compared to C-on-C. M-on-C females showed significantly smaller adipocyte size compared to C-on-C females and also compared to M-on-M. No differences were detected between control rats fostered by a MUN mother (C-on-M) and C-on-C females (Figure 3A).
We used Mitotracker, a dye that stains mitochondria, to evaluate beige-type adipocytes within perivascular WAT. Mitotracker-positive cells showed an intense stain. M-on-M males had a smaller percentage of Mitotracker-positive cells compared to C-on-C controls (Figure 4). MUN males fostered by a control dam (M-on-C) had a similar % compared to C-on-C males, being larger compared to M-on-M offspring. Control rats fostered by a MUN mother had lower Mitotracker-positive stained areas compared to C-on-C males.
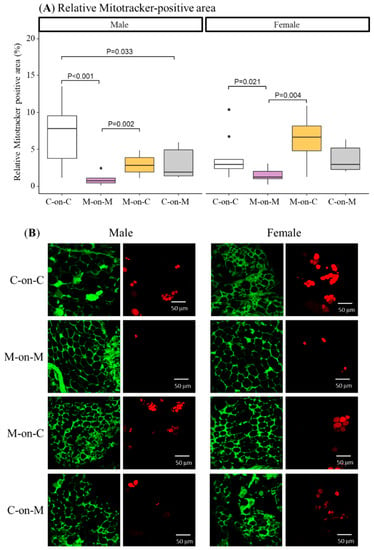
Figure 4.
Percentage of Mitotracker-positive adipocytes in perivascular fat (A) and representative images obtained by confocal microscopy (B) of 21-day-old male and female offspring from MUN and Control mothers. MUN, maternal undernutrition during gestation; C-on-C, control pups fostered by their mothers (6 males and 6 females); M-on-M, MUN rats fostered by their mothers (6 males and 6 females); C-on-M, control rats fostered by MUN mothers (6 males and 6 females); M-on-C, MUN rats fostered by a control mother (6 males and 6 females). Data show the median and interquartile range [Q1; Q3], and the showed p-Value (P) was extracted from Dunnett’s post-hoc pairwise comparison test when the Kruskal-Wallis test was P < 0.05. Images were acquired with a Leica TCS SP2 confocal microscope, ×40 objective at Ex = 488 nm/Em = 500–560 nm (green images) and Ex = 581 nm/Em = 644 nm (red images); scale bar = 50 μm. Dots show outliers.
As observed in males, M-on-M females had significantly lower Mitotracker positive area compared to C-on-C females. MUN rats fostered by a control mother (M-on-C) had a similar % compared to C-on-C offspring, being significantly larger compared to M-on-M rats (Figure 4).
3.4. Heart Structure and Function
Heart structure and function were assessed by transthoracic echocardiography at the end of the lactation period. In male M-on-M rats, posterior wall thickness tended to be higher and interventricular septum was significantly higher compared to C-on-C males. MUN males fostered by a control mother (M-on-C) did not show differences with C-on-C males. Female pups did not show significant differences in any of the studied parameters (Figure 5a,b).
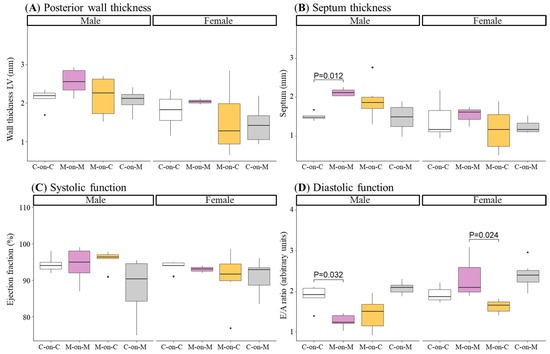
Figure 5.
Posterior wall thickness (A), septum thickness (B), ejection fraction (C), and E/A ratio (D) of 21-day-old male and female offspring from MUN and Control mothers. MUN, maternal undernutrition during gestation; C-on-C, control pups fostered by their mothers (6 males and 6 females); M-on-M, MUN rats fostered by their mothers (6 males and 6 females); C-on-M, control rats fostered by MUN mothers (6 males and 6 females); M-on-C, MUN rats fostered by a control mother (6 males and 6 females); LV, left ventricle. Data show the median and interquartile range [Q1; Q3], and the showed p-Value (P) was extracted from Dunnett’s post-hoc pairwise comparison test when the Kruskal-Wallis test was P < 0.05. Dots show outliers.
Systolic function, assessed as ejection fraction, was not different between groups (Figure 5C). However, diastolic function, assessed as the ratio of E/A waves, was significantly reduced in M-on-M males compared to C-on-C counterparts. No significant differences were found in MUN males fostered by a C mother (M-on-C) compared to C-on-C (Figure 5D). Female M-on-M did not show significant differences in any of these parameters compared to C-on-C. However, the E/A ratio was significantly decreased in female M-on-C compared to female M-on-M (Figure 5D).
End-systolic and end-diastolic diameters were not significantly different between C-on-C and any of the other groups (Table 1).

Table 1.
End left ventricle dimensions of heart cycles of the offspring at day 21.
3.5. Thoracic Aorta Structure
In M-on-M males’ internal and external diameter, and wall cross-sectional area (CSA) were significantly larger compared to C-on-C. In M-on-C males the studied parameters were not different from C-on-C males and external diameter and CSA were significantly smaller compared to M-on-M rats (Figure 6).
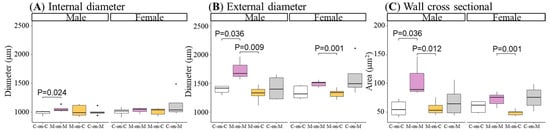
Figure 6.
Internal (A) and external diameters (B), and wall cross-sectional (C) of the thoracic aorta in 21-day-old male and female offspring from MUN and Control mothers. MUN, maternal undernutrition during gestation; C-on-C, control pups fostered by their mothers (6 males and 6 females); M-on-M, MUN rats fostered by their mothers (6 males and 6 females); C-on-M, control rats fostered by MUN mothers (6 males and 6 females); M-on-C, MUN rats fostered by a control mother (6 males and 6 females). Data show the median and interquartile range [Q1; Q3], and the showed p-Value (p) was extracted from Dunnett’s post-hoc pairwise comparison test when the Kruskal-Wallis test was p < 0.05. Dot show outliers.
M-on-M females tended to have larger parameters compared to C-on-C, without statistical significance. However, MUN females fostered by a control mother (M-on-C) had a smaller external diameter and CSA than M-on-M rats (Figure 6).
4. Discussion
In this study, we aimed to evaluate the impact of lactation environment on body, cardiovascular and adipose tissue growth in rats with LBW induced by undernutrition during fetal life (MUN offspring). The main findings of the study are summarized in Table 2. During lactation, MUN offspring accelerate body weight gain, while length growth is slower. In males, this growth pattern occurs during the exclusive lactation period, while in females takes place during the last week before weaning, when the rats suckle and eat chow. By weaning, MUN males but not females, exhibit diastolic dysfunction, and heart, aorta, and perivascular white adipocyte hypertrophy; a lower proportion of beige-type adipocytes was found in MUN offspring from both sexes. These sex-dependent alterations may set the basis for the observed hypertension development in MUN males and can predispose to obesity in males and females. We also demonstrated that nursing MUN rats with a controlling mother rescues the hypertrophy alterations, in parallel with a slower weight gain, while nursing control pups, one MUN mother did not have a hypertrophic effect. These data suggest that both MUN rats, in the fetal and perinatal periods, are required to develop phenotypic alterations. In addition, the alterations programmed during the fetal period may be counteracted during lactation by reducing the growth rate. The period of exclusive lactation seems to be more relevant for the observed hypertrophy, even though no major modifications in breastmilk macronutrients were detected between MUN and Control dams, suggesting the role of breastmilk bioactive factors. In summary, the present data provide experimental evidence of the link between accelerated growth during early postnatal life in LBW individuals and higher-risk cardiometabolic diseases and support that modulation of growth during the lactation period can be an effective strategy to counteract alterations induced during fetal life.

Table 2.
Summary of main findings.
Catch-up growth has been proposed to be deleterious for cardiometabolic health in individuals with LBW. We addressed the role of growth during lactation in a rat model of LBW induced by fetal undernutrition, which develops hypertension and cardiac alterations in adult life. In rats, suckling is the only source of nutrition until day 16 of lactation, while from day 17 to weaning there is an increasing content of chow in the stomach of the pups []. Therefore, we analyzed growth patterns during both periods of lactation. We found a sexual dimorphism in the growth pattern. In males, accelerated weight gain was observed during the period of exclusive lactation, while in female offspring catch-up growth was observed in the last week of lactation. We also observed that control rats fed on MUN mothers had a slower weight gain both in males and females. To explain these data, we considered differences in milk composition. However, we did not find significant variations in protein or fat content although a tendency toward lower values was observed in MUN dams. It is possible that the milk from MUN dams had lower macronutrient levels at birth, as we have evidenced in plasma [], but they may normalize along lactation, since the rat returns to an ad libitum diet. In other rodent models of programming, milk protein content was found to be unaffected if the dam was fed with low protein [,] or with high energy diets [] during gestation or lactation. We also observed a slower length gain during the last week of the lactation period, during which the rats suckle and also eat chow. We do not think this is related to the lower mineral content of the milk, since minerals seem to be relatively stable [] and it is possible that there was a prior bone deficiency induced by undernutrition. We also discarded a lower milk yield due to compromised mammary gland development, observed in a rat model of fetal programming induced by uteroplacental insufficiency [], since it would not explain the quicker weight gain in M-on-M offspring. Growth acceleration in MUN males could be explained by hyperphagia which can be programmed [], is associated with increased neonatal growth rates and visceral adiposity [], and it has been described in offspring from protein-restricted dams []. We do not think dam behavioral alterations, which have been described in SHR and WKY cross-fostering [], explain our data since all the MUN and Control dams accepted the pups from the other mother successfully. The main influence on growth rate was observed during the period of exclusive lactation; since no major alterations in macronutrients were observed, we suggest the role of milk bioactive components, such as hormones or growth factors. This hypothesis is supported by metabolomic analysis of milk from rats exposed to mild caloric restriction during lactation showing changes in several compounds related to metabolic pathways [], and the evidence that leptin supplementation during the suckling period reverses some of the metabolic alterations induced by a moderate maternal calorie restriction during gestation []. It would be interesting to conduct an in-depth milk metabolomic study on the alterations induced by undernutrition in our rat model.
Rapid growth gain has been related to increased adiposity and obesity development, and therefore, we analyzed possible alterations in body fat. We found that, in parallel with accelerated weight gain, by weaning M-on-M males exhibited hypertrophied perivascular WAT adipocytes compared to controls, an alteration reversed by nursing MUN offspring on a control dam. Similar results were found in a model of obesity programming induced by monosodium glutamate, where cross-fostering also mitigates obesity development []. In addition to energy-storing WAT, adipose tissue also comprises thermogenic brown adipose tissue (BAT), and beige adipocytes, an inducible form of thermogenic adipocytes interspersed within WAT [] recruited postnatally in a process called browning []. Browning or “beigeing” has recently gained attention, since beige adipose tissue has a larger energy expenditure capacity, and induced browning in newborn rats decreases adipogenesis in adult life, suggesting a possible way through which the neonatal period can influence obesity development []. Therefore, we analyzed the proportion of beige adipocytes within the perivascular WAT in our experimental model, using Mitotracker, a specific dye for mitochondria, since beige adipocytes possess abundant cristae-dense mitochondria [,]. MUN rats had a very small proportion of beige-type adipocytes, which may be related to mitochondrial alterations induced by undernutrition, since mitochondrion is a very sensitive organelle and programming has been demonstrated in response to several intrauterine stress factors []. A reduction in beige thermogenic tissue could disbalance energetics and facilitate lipid accumulation, leading to the observed increased WAT adipocyte size. It was interesting that beige-type adipocytes increased by fostering MUN rats on a control mother. It has been demonstrated that beige adipose tissue appears spontaneously in WAT during early postnatal development with a peak of expression observed at 21 days []. Therefore, the lactation period is an important window during which adipose tissue type may be modulated. It would be interesting to analyze in MUN rats the effect of the lactation environment on adipocyte progenitor markers, such as mesenchymal cell antigen 1 (MSCA1), which has been positively correlated to obesity, adipocyte hypertrophy, and inflammation in children []. It is interesting to note that, increased browning occurred in MUN rats exposed to a control lactation environment, while it decreased in control rats exposed to a MUN mother. Therefore, unlike cardiovascular hypertrophy, which seems to require the first hit being during intrauterine life, adipose tissue may be regulated by the lactation environment alone. This is evidenced by our previous study showing that accelerated growth during lactation induced by reducing litter size, without prior programming, also increases WAT deposits []. Prolonged retention of thermogenic beige adipocytes maintains high whole-body energy expenditure and protects mice from diet-induced obesity []. Therefore, it would be interesting to evaluate if cross-fostered MUN rats retain this characteristic in adult life. Our finding of beige adipocytes within the WAT perivascular tissue is interesting, since, in mice, beige adipocytes are enriched within subcutaneous fat depots, and are rarely detected in visceral depots []. Perivascular WAT also plays a role in vascular tone and maintenance of normal structure [], which is dysregulated by excess fat, as we have reported in obese mice []. A reduced proportion of beige-adipocytes may play a role in vascular dysfunction, an alteration observed in several animal models of fetal programming []. These alterations may be due to the pro-oxidant and proinflammatory environment associated with excess fat, favoring the local release of vasoactive factors. Thus, alterations in the proportion of beige-to-WAT perivascular adipose tissue may contribute to the association between obesity and cardiovascular disease [], an aspect that deserves further attention. The cardioprotective effect of beige adipose tissue is suggested by the fact that individuals with detectable thermogenic adipose tissues have lower odds of hypertension and coronary heart disease [].
Accelerated body growth gain in MUN males was paralleled by a hypertrophic response in the cardiovascular system observed in the aorta and the heart. The characteristics of the structural alteration in the aorta are compatible with an outward hypertrophic remodeling, with an increase in wall mass due to expansion of the external diameter. Females show a better adaptation, although the data also evidence a tendency towards a larger growth, as we have previously described in resistance arteries []. Undernutrition induced marked heart alterations by weaning, in addition to ventricular hypertrophy, a reduced diastolic function was also observed, suggesting that cardiac tissue has a high susceptibility to programming, also observed in guinea pigs exposed to undernutrition, which show a permanent deficiency in cardiomyocyte number []. We did not explore molecular markers of hypertrophy, such as BNP; we have evidence that this factor is not elevated in MUN offspring by weaning, but it is increased in aging in MUN males along with hypertension development and further cardiac hypertrophy []. The role of sex in heart alterations induced by undernutrition may be related to the lower efficiency of MUN male placenta, associated with poor vascularization [], which may be particularly detrimental for the heart due to the unique feature of cardiomyocytes as non-dividing cells []. Cardiovascular hypertrophy in MUN males was rescued by cross-fostering, reinforcing the role of lactation in reprogramming cardiovascular disease. The importance of this period for future cardiometabolic health is supported by data in the genetic model of essential hypertension, the SHR rat, which reduces blood pressure levels in adult life if cross-fostered to a control dam []. It is worth mentioning that this model of essential hypertension also exhibits sexual dimorphism and we have found several common features with the MUN model [].
5. Conclusions
The lactation period acts as a second hit consolidating programming initiated by fetal undernutrition in a sex-dependent manner, inducing cardiovascular and adipocyte hypertrophy.
The alterations programmed during fetal life may be counteracted during the perinatal period avoiding accelerated growth and thus, lactation and can be a window of intervention to reverse fetal programming.
The exclusive lactation period seems to play a key role in organ hypertrophy, despite no differences in breastmilk macronutrients, suggesting the role of bioactive factors, which deserves in-depth analysis.
Author Contributions
Conceptualization, S.M.A., P.R.-R., I.M.-C. and D.R.-C.; methodology, P.R.-R., I.M.-C., S.P., B.Q.-V., A.G.-R. and S.C.; software, I.M.-C. and D.R.-C.; validation, P.R.-R., I.M.-C., D.R.-C., S.P., B.Q.-V., A.G.-R. and S.M.A.; formal analysis, D.R.-C.; investigation, P.R.-R., I.M.-C., S.P., B.Q.-V., A.G.-R. and S.C.; resources, S.M.A.; data curation, P.R.-R., I.M.-C., S.R. and S.P.; writing—original draft preparation, S.M.A. and D.R.-C.; writing—review and editing, P.R.-R., I.M.-C., S.P., B.Q.-V., S.R., A.G.-R., S.C., D.R.-C. and S.M.A.; visualization, P.R.-R., I.M.-C., D.R.-C. and S.M.A.; supervision, S.M.A.; funding acquisition, S.M.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Ministerio de Ciencia, Innovación y Universidades (Spain; grant number RTI2018-097504-B-I00), co-financed with FEDER funds.
Institutional Review Board Statement
The animal study protocol was approved by the Institutional Review Board of Universidad Autónoma de Madrid and Comunidad Autónoma de Madrid (Spain, protocol code PROEX 004-19 and approved on 7 May 2019).
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The availability of the data is restricted to investigators based in academic institutions.
Conflicts of Interest
The funders had no role in the design of the study; in the collection, analysis, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Barker, D.; Osmond, C. Infant Mortality, Childhood Nutrition, and Ischaemic Heart Disease in England and Wales. Lancet 1986, 1, 1077–1081. [Google Scholar] [CrossRef]
- Barker, D. Fetal Origins of Coronary Heart Disease. BMJ 1995, 311, 171–174. [Google Scholar] [CrossRef] [PubMed]
- Hult, M.; Tornhammar, P.; Ueda, P.; Chima, C.; Bonamy, A.-K.E.; Ozumba, B.; Norman, M. Hypertension, Diabetes and Overweight: Looming Legacies of the Biafran Famine. PLoS ONE 2010, 5, e13582. [Google Scholar] [CrossRef] [PubMed]
- Roseboom, T.J.; van der Meulen, J.H.; Osmond, C.; Barker, D.J.; Ravelli, A.C.; Schroeder-Tanka, J.M.; van Montfrans, G.A.; Michels, R.P.; Bleker, O.P. Coronary Heart Disease after Prenatal Exposure to the Dutch Famine, 1944–1945. Heart 2000, 84, 595–598. [Google Scholar] [CrossRef]
- Wu, L.; Feng, X.; He, A.; Ding, Y.; Zhou, X.; Xu, Z. Prenatal Exposure to the Great Chinese Famine and Mid-Age Hypertension. PLoS ONE 2017, 12, e0176413. [Google Scholar] [CrossRef]
- Ashton, N. Perinatal Development and Adult Blood Pressure. Braz. J. Med. Biol. Res. 2000, 33, 731–740. [Google Scholar] [CrossRef]
- Morton, J.S.; Cooke, C.-L.; Davidge, S.T. In Utero Origins of Hypertension: Mechanisms and Targets for Therapy. Physiol. Rev. 2016, 96, 549–603. [Google Scholar] [CrossRef]
- Singhal, A.; Cole, T.J.; Fewtrell, M.; Deanfield, J.; Lucas, A. Is Slower Early Growth Beneficial for Long-Term Cardiovascular Health? Circulation 2004, 109, 1108–1113. [Google Scholar] [CrossRef]
- Eriksson, J.G. Early Growth and Coronary Heart Disease and Type 2 Diabetes: Findings from the Helsinki Birth Cohort Study (HBCS). Am. J. Clin. Nutr. 2011, 94, 1799S–1802S. [Google Scholar] [CrossRef]
- Woo, J.G. Infant Growth and Long-Term Cardiometabolic Health: A Review of Recent Findings. Curr. Nutr. Rep. 2019, 8, 29–41. [Google Scholar] [CrossRef]
- Kelishadi, R.; Haghdoost, A.A.; Jamshidi, F.; Aliramezany, M.; Moosazadeh, M. Low Birthweight or Rapid Catch-up Growth: Which Is More Associated with Cardiovascular Disease and Its Risk Factors in Later Life? A Systematic Review and Cryptanalysis. Paediatr. Int. Child. Health 2015, 35, 110–123. [Google Scholar] [CrossRef]
- Kesavan, K.; Devaskar, S.U. Intrauterine Growth Restriction: Postnatal Monitoring and Outcomes. Pediatr. Clin. N. Am. 2019, 66, 403–423. [Google Scholar] [CrossRef] [PubMed]
- Picó, C.; Reis, F.; Egas, C.; Mathias, P.; Matafome, P. Lactation as a Programming Window for Metabolic Syndrome. Eur J. Clin. Investig. 2021, 51, e13482. [Google Scholar] [CrossRef] [PubMed]
- Gila-Diaz, A.; Arribas, S.M.; Algara, A.; Martín-Cabrejas, M.A.; López de Pablo, Á.L.; Sáenz de Pipaón, M.; Ramiro-Cortijo, D. A Review of Bioactive Factors in Human Breastmilk: A Focus on Prematurity. Nutrients 2019, 11, 1307. [Google Scholar] [CrossRef] [PubMed]
- Wong, P.D.; Anderson, L.N.; Dai, D.D.W.; Parkin, P.C.; Maguire, J.L.; Birken, C.S.; TARGet Kids! Collaboration The Association of Breastfeeding Duration and Early Childhood Cardiometabolic Risk. J. Pediatr. 2018, 192, 80–85.e1. [Google Scholar] [CrossRef] [PubMed]
- Pluymen, L.P.M.; Wijga, A.H.; Gehring, U.; Koppelman, G.H.; Smit, H.A.; van Rossem, L. Breastfeeding and Cardiometabolic Markers at Age 12: A Population-Based Birth Cohort Study. Int. J. Obes. 2019, 43, 1568–1577. [Google Scholar] [CrossRef]
- Quigley, M.; Embleton, N.D.; McGuire, W. Formula versus Donor Breast Milk for Feeding Preterm or Low Birth Weight Infants. Cochrane Database Syst. Rev. 2018, 6, CD002971. [Google Scholar] [CrossRef]
- Rodríguez-Rodríguez, P.; López De Pablo, A.L.; García-Prieto, C.F.; Somoza, B.; Quintana-Villamandos, B.; Gómez De Diego, J.J.; Gutierrez-Arzapalo, P.Y.; Ramiro-Cortijo, D.; González, M.C.; Arribas, S.M. Long Term Effects of Fetal Undernutrition on Rat Heart. Role of Hypertension and Oxidative Stress. PLoS ONE 2017, 12, e0171544. [Google Scholar] [CrossRef]
- Gutiérrez-Arzapalo, P.Y.; Rodríguez-Rodríguez, P.; Ramiro-Cortijo, D.; López de Pablo, A.L.; López-Giménez, M.R.; Condezo-Hoyos, L.; Greenwald, S.E.; González, M.d.C.; Arribas, S.M. Role of Fetal Nutrient Restriction and Postnatal Catch-up Growth on Structural and Mechanical Alterations of Rat Aorta. J. Physiol. 2018, 596, 5791–5806. [Google Scholar] [CrossRef] [PubMed]
- Munoz-Valverde, D.; Rodríguez-Rodríguez, P.; Gutierrez-Arzapalo, P.Y.; López de Pablo, A.L.; Carmen González, M.; López-Giménez, R.; Somoza, B.; Arribas, S.M. Effect of Fetal Undernutrition and Postnatal Overfeeding on Rat Adipose Tissue and Organ Growth at Early Stages of Postnatal Development. Physiol. Res. 2015, 64, 547–559. [Google Scholar] [CrossRef]
- Rodríguez-Rodríguez, P.; López de Pablo, A.L.; Condezo-Hoyos, L.; Martín-Cabrejas, M.A.; Aguilera, Y.; Ruiz-Hurtado, G.; Gutierrez-Arzapalo, P.Y.; Ramiro-Cortijo, D.; Fernández-Alfonso, M.S.; González, M.D.C.; et al. Fetal Undernutrition Is Associated with Perinatal Sex-Dependent Alterations in Oxidative Status. J. Nutr. Biochem. 2015, 26, 1650–1659. [Google Scholar] [CrossRef]
- Miranda, R.A.; da Silva Franco, C.C.; de Oliveira, J.C.; Barella, L.F.; Tófolo, L.P.; Ribeiro, T.A.; Pavanello, A.; da Conceição, E.P.S.; Torrezan, R.; Armitage, J.; et al. Cross-Fostering Reduces Obesity Induced by Early Exposure to Monosodium Glutamate in Male Rats. Endocrine 2017, 55, 101–112. [Google Scholar] [CrossRef]
- Herreid, E.O.; Harmon, C. A Study of Methods of Obtaining Milk Samples for Estimating Milk Fat by the Mojonnier Method. J. Dairy Sci. 1944, 27, 33–38. [Google Scholar] [CrossRef]
- Bradford, M.M. A Rapid and Sensitive Method for the Quantitation of Microgram Quantities of Protein Utilizing the Principle of Protein-Dye Binding. Anal. Biochem. 1976, 72, 248–254. [Google Scholar] [CrossRef]
- Quintana-Villamandos, B.; Gomez de Diego, J.J.; Delgado-Martos, M.J.; Muñoz-Valverde, D.; Soto-Montenegro, M.L.; Desco, M.; Delgado-Baeza, E. Dronedarone Produces Early Regression of Myocardial Remodelling in Structural Heart Disease. PLoS ONE 2017, 12, e0188442. [Google Scholar] [CrossRef] [PubMed]
- Schindelin, J.; Arganda-Carreras, I.; Frise, E.; Kaynig, V.; Longair, M.; Pietzsch, T.; Preibisch, S.; Rueden, C.; Saalfeld, S.; Schmid, B.; et al. Fiji: An Open-Source Platform for Biological-Image Analysis. Nat. Methods 2012, 9, 676–682. [Google Scholar] [CrossRef]
- Chazotte, B. Labeling Mitochondria with MitoTracker Dyes. Cold Spring Harb. Protoc. 2011, 2011, 990–992. [Google Scholar] [CrossRef] [PubMed]
- Henning, S.J.; Chang, S.S.; Gisel, E.G. Ontogeny of Feeding Controls in Suckling and Weanling Rats. Am. J. Physiol 1979, 237, R187–R191. [Google Scholar] [CrossRef]
- Phuthong, S.; Reyes-Hernández, C.G.; Rodríguez-Rodríguez, P.; Ramiro-Cortijo, D.; Gil-Ortega, M.; González-Blázquez, R.; González, M.C.; López de Pablo, A.L.; Arribas, S.M. Sex Differences in Placental Protein Expression and Efficiency in a Rat Model of Fetal Programming Induced by Maternal Undernutrition. Int. J. Mol. Sci 2020, 22, 237. [Google Scholar] [CrossRef] [PubMed]
- Prentice, A.M.; Goldberg, G.R.; Prentice, A. Body Mass Index and Lactation Performance. Eur. J. Clin. Nutr. 1994, 48 (Suppl. 3), S78–S86; discussion S86–S89. [Google Scholar]
- Kugananthan, S.; Gridneva, Z.; Lai, C.T.; Hepworth, A.R.; Mark, P.J.; Kakulas, F.; Geddes, D.T. Associations between Maternal Body Composition and Appetite Hormones and Macronutrients in Human Milk. Nutrients 2017, 9, 252. [Google Scholar] [CrossRef] [PubMed]
- Palou, M.; Torrens, J.M.; Castillo, P.; Sánchez, J.; Palou, A.; Picó, C. Metabolomic Approach in Milk from Calorie-Restricted Rats during Lactation: A Potential Link to the Programming of a Healthy Phenotype in Offspring. Eur. J. Nutr 2020, 59, 1191–1204. [Google Scholar] [CrossRef] [PubMed]
- Briffa, J.F.; O’Dowd, R.; Moritz, K.M.; Romano, T.; Jedwab, L.R.; McAinch, A.J.; Hryciw, D.H.; Wlodek, M.E. Uteroplacental Insufficiency Reduces Rat Plasma Leptin Concentrations and Alters Placental Leptin Transporters: Ameliorated with Enhanced Milk Intake and Nutrition. J. Physiol. 2017, 595, 3389–3407. [Google Scholar] [CrossRef]
- Langley-Evans, S.C.; Bellinger, L.; McMullen, S. Animal Models of Programming: Early Life Influences on Appetite and Feeding Behaviour. Matern. Child. Nutr. 2005, 1, 142–148. [Google Scholar] [CrossRef]
- de Blasio, M.J.; Gatford, K.L.; Robinson, J.S.; Owens, J.A. Placental Restriction of Fetal Growth Reduces Size at Birth and Alters Postnatal Growth, Feeding Activity, and Adiposity in the Young Lamb. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2007, 292, R875–R886. [Google Scholar] [CrossRef]
- Bellinger, L.; Sculley, D.V.; Langley-Evans, S.C. Exposure to Undernutrition in Fetal Life Determines Fat Distribution, Locomotor Activity and Food Intake in Ageing Rats. Int J. Obes. 2006, 30, 729–738. [Google Scholar] [CrossRef]
- Gouldsborough, I.; Black, V.; Johnson, I.T.; Ashton, N. Maternal Nursing Behaviour and the Delivery of Milk to the Neonatal Spontaneously Hypertensive Rat. Acta Physiol. Scand. 1998, 162, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Konieczna, J.; García, A.P.; Sánchez, J.; Palou, M.; Palou, A.; Picó, C. Oral Leptin Treatment in Suckling Rats Ameliorates Detrimental Effects in Hypothalamic Structure and Function Caused by Maternal Caloric Restriction during Gestation. PLoS ONE 2013, 8, e81906. [Google Scholar] [CrossRef]
- Schuster, S.; Hechler, C.; Gebauer, C.; Kiess, W.; Kratzsch, J. Leptin in Maternal Serum and Breast Milk: Association with Infants’ Body Weight Gain in a Longitudinal Study over 6 Months of Lactation. Pediatr. Res. 2011, 70, 633–637. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, K.; Maretich, P.; Kajimura, S. The Common and Distinct Features of Brown and Beige Adipocytes. Trends Endocrinol. Metab. 2018, 29, 191–200. [Google Scholar] [CrossRef]
- Kuryłowicz, A.; Puzianowska-Kuźnicka, M. Induction of Adipose Tissue Browning as a Strategy to Combat Obesity. Int. J. Mol. Sci 2020, 21, 6241. [Google Scholar] [CrossRef]
- Ying, T.; Golden, T.; Cheng, L.; Ishibashi, J.; Seale, P.; Simmons, R.A. Neonatal IL-4 Exposure Decreases Adipogenesis of Male Rats into Adulthood. Am. J. Physiol. Endocrinol. Metab. 2021, 320, E1148–E1157. [Google Scholar] [CrossRef]
- Koenen, M.; Hill, M.A.; Cohen, P.; Sowers, J.R. Obesity, Adipose Tissue and Vascular Dysfunction. Circ. Res. 2021, 128, 951–968. [Google Scholar] [CrossRef]
- Rodríguez-Rodríguez, P.; Ramiro-Cortijo, D.; Reyes-Hernández, C.G.; López de Pablo, A.L.; González, M.C.; Arribas, S.M. Implication of Oxidative Stress in Fetal Programming of Cardiovascular Disease. Front. Physiol. 2018, 9, 602. [Google Scholar] [CrossRef]
- Chabowska-Kita, A.; Kozak, L.P. The Critical Period for Brown Adipocyte Development: Genetic and Environmental Influences. Obesity 2016, 24, 283–290. [Google Scholar] [CrossRef]
- Hanschkow, M.; Boulet, N.; Kempf, E.; Bouloumié, A.; Kiess, W.; Stein, R.; Körner, A.; Landgraf, K. Expression of the Adipocyte Progenitor Markers MSCA1 and CD36 Is Associated With Adipose Tissue Function in Children. J. Clin. Endocrinol. Metab. 2022, 107, e836–e851. [Google Scholar] [CrossRef]
- Loncar, D. Convertible Adipose Tissue in Mice. Cell Tissue Res. 1991, 266, 149–161. [Google Scholar] [CrossRef]
- Gil-Ortega, M.; Martín-Ramos, M.; Arribas, S.M.; González, M.C.; Aránguez, I.; Ruiz-Gayo, M.; Somoza, B.; Fernández-Alfonso, M.S. Arterial Stiffness Is Associated with Adipokine Dysregulation in Non-Hypertensive Obese Mice. Vascul Pharmacol. 2016, 77, 38–47. [Google Scholar] [CrossRef]
- Feng, X.; Yu, T.; Zhang, Y.; Li, L.; Qu, M.; Wang, J.; Dong, F.; Zhang, L.; Wang, F.; Zhang, F.; et al. Prenatal High-Sucrose Diet Induced Vascular Dysfunction in Thoracic Artery of Fetal Offspring. Mol. Nutr. Food Res. 2021, 65, e2100072. [Google Scholar] [CrossRef]
- Villarroya, F.; Cereijo, R.; Gavaldà-Navarro, A.; Villarroya, J.; Giralt, M. Inflammation of Brown/Beige Adipose Tissues in Obesity and Metabolic Disease. J. Intern. Med. 2018, 284, 492–504. [Google Scholar] [CrossRef]
- Becher, T.; Palanisamy, S.; Kramer, D.J.; Eljalby, M.; Marx, S.J.; Wibmer, A.G.; Butler, S.D.; Jiang, C.S.; Vaughan, R.; Schöder, H.; et al. Brown Adipose Tissue Is Associated with Cardiometabolic Health. Nat. Med. 2021, 27, 58–65. [Google Scholar] [CrossRef]
- Gutiérrez-Arzapalo, P.Y.; Rodríguez-Rodríguez, P.; Ramiro-Cortijo, D.; Gil-Ortega, M.; Somoza, B.; de Pablo, Á.L.L.; González, M.C.; Arribas, S.M. Fetal Undernutrition Induces Resistance Artery Remodeling and Stiffness in Male and Female Rats Independent of Hypertension. Biomedicines 2020, 8, 424. [Google Scholar] [CrossRef]
- Masoumy, E.P.; Sawyer, A.A.; Sharma, S.; Patel, J.A.; Gordon, P.M.K.; Regnault, T.R.H.; Matushewski, B.; Weintraub, N.L.; Richardson, B.; Thompson, J.A.; et al. The Lifelong Impact of Fetal Growth Restriction on Cardiac Development. Pediatr. Res. 2018, 84, 537–544. [Google Scholar] [CrossRef]
- Arima, Y.; Fukuoka, H. Developmental Origins of Health and Disease Theory in Cardiology. J. Cardiol. 2020, 76, 14–17. [Google Scholar] [CrossRef]
- Vieira-Rocha, M.S.; Sousa, J.B.; Rodríguez-Rodríguez, P.; Arribas, S.M.; Diniz, C. Elevated Vascular Sympathetic Neurotransmission and Remodelling Is a Common Feature in a Rat Model of Foetal Programming of Hypertension and SHR. Biomedicines 2022, 10, 1902. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).