Heated Humidified High-Flow Nasal Cannula in Children: State of the Art
Abstract
:1. Introduction
2. Device and Mechanism of Action
2.1. Flow Generator
2.2. Humidifying Devices
2.3. Inspiratory Limb
2.4. Interface
3. Clinical Indications
3.1. Acute Bronchiolitis
| Reference | Study Design | Study Population | Comparison | Main Findings |
|---|---|---|---|---|
| Franklin et al. [11] | RCT | 1472 patients < 12 months with bronchiolitis | HFNC vs. COT |
|
| Kepreotes et al. [14] | RCT | 202 patients < 24 months with moderate bronchiolitis | HFNC vs. COT |
|
| Lin et al. [12] | Systematic review | 2121 patients with bronchiolitis | HFNC vs. other oxygen therapies (COT, CPAP) |
|
| Dafydd et al. [13] | Systematic review and meta-analysis | 1159 children up to 24 months of age with bronchiolitis | HFNC vs. other oxygen therapies (COT, nCPAP) |
|
| Moreel et al. [15] | Meta-analysis | 213 infants < 24 months | HFNC vs. nCPAP |
|
3.2. Asthma
3.3. Congenital Heart Diseases
3.4. Obstructive Sleep Apnea
3.5. Pneumonia
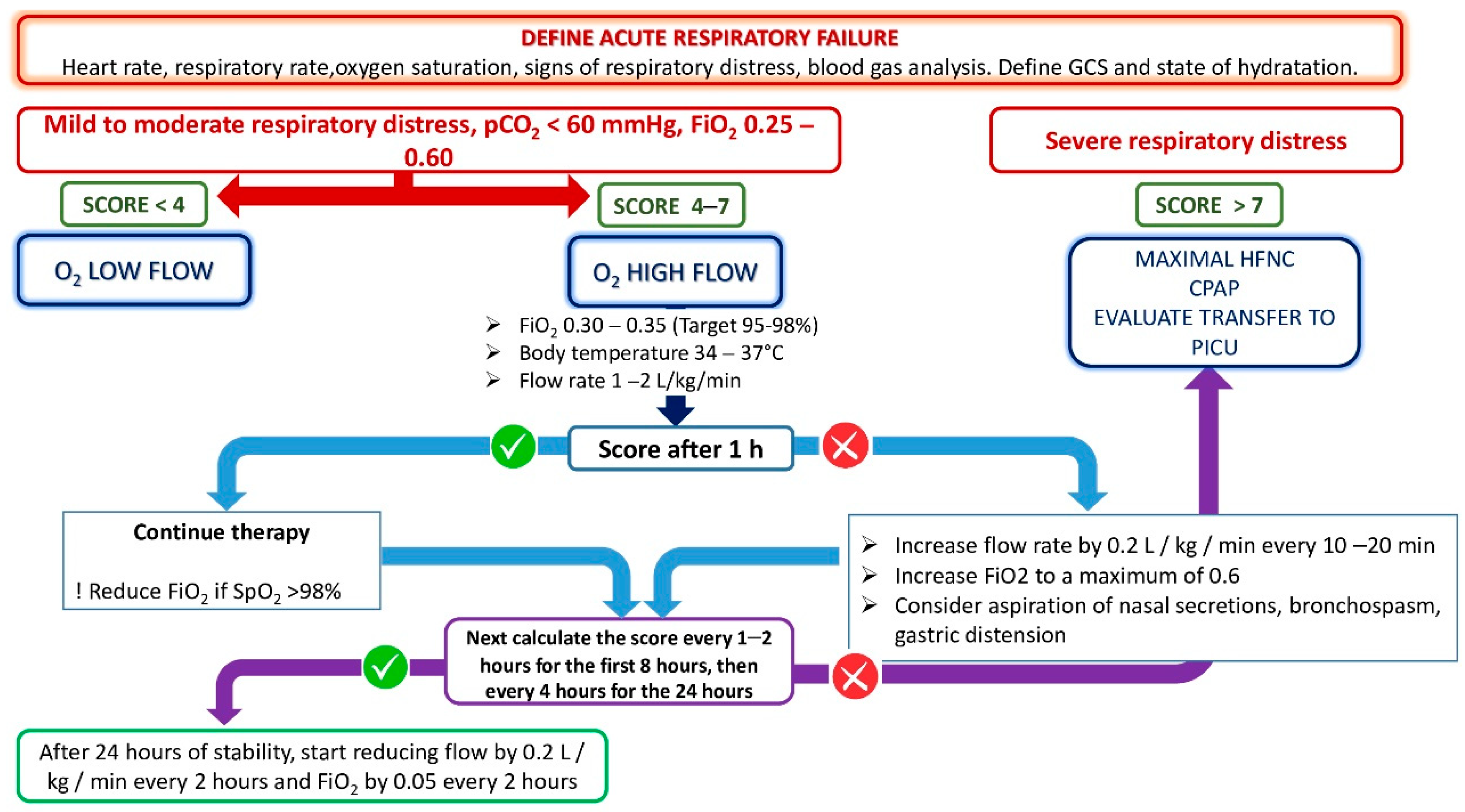
4. HFNC Setting: Initiation, Maintenance, and Weaning
- -
- Temperature: between 34–37 °C, with an ideal value of 34 °C for the pediatric patient.
- -
- Flow: can be set up to 60 L/min. In the most of pediatric studies, the flow is set up on the basis of body weight (1–2 L/kg/min). In bronchiolitis, a flow of 2 L/kg/min seems to offer maximum efficacy with minimal risk of adverse events.
- -
- FiO2: set up with the aim of obtaining a saturation of 95–97%.
5. Advantages of the Use of HFNC
6. Adverse Side Effects and Contraindications
7. Comparison with Other Ventilation Techniques
8. Clinical Predictive Scores
9. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pierce, H.C.; Mansbach, J.M.; Fisher, E.S.; Macias, C.G.; Pate, B.M.; Piedra, P.A.; Sullivan, A.F.; Espinola, J.A.; Camargo, C.A. Variability of Intensive Care Management for Children with Bronchiolitis. Hosp. Pediatr. 2015, 5, 175–184. [Google Scholar] [CrossRef]
- Nishimura, M. High-Flow Nasal Cannula Oxygen Therapy Devices. Respir. Care 2019, 64, 735–742. [Google Scholar] [CrossRef] [PubMed]
- Parke, R.; McGuinness, S.; Eccleston, M. Nasal High-Flow Therapy Delivers Low Level Positive Airway Pressure. Br. J. Anaesth. 2009, 103, 886–890. [Google Scholar] [CrossRef]
- Sreenan, C.; Lemke, R.P.; Hudson-Mason, A.; Osiovich, H. High-Flow Nasal Cannulae in the Management of Apnea of Prematurity: A Comparison with Conventional Nasal Continuous Positive Airway Pressure. Pediatrics 2001, 107, 1081–1083. [Google Scholar] [CrossRef] [PubMed]
- Mikalsen, I.B.; Davis, P.; Øymar, K. High Flow Nasal Cannula in Children: A Literature Review. Scand. J. Trauma. Resusc. Emerg. Med. 2016, 24, 93. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, M. High-Flow Nasal Cannula Oxygen Therapy in Adults: Physiological Benefits, Indication, Clinical Benefits, and Adverse Effects. Respir. Care 2016, 61, 529–541. [Google Scholar] [CrossRef]
- D’Amato, M.; Molino, A.; Calabrese, G.; Cecchi, L.; Annesi-Maesano, I.; D’Amato, G. The Impact of Cold on the Respiratory Tract and Its Consequences to Respiratory Health. Clin. Transl. Allergy 2018, 8, 20. [Google Scholar] [CrossRef] [PubMed]
- Al Ashry, H.S.; Modrykamien, A.M. Humidification during Mechanical Ventilation in the Adult Patient. Biomed Res. Int. 2014, 2014, 715434. [Google Scholar] [CrossRef] [PubMed]
- Fainardi, V.; Abelli, L.; Muscarà, M.; Pisi, G.; Principi, N.; Esposito, S. Update on the Role of High-Flow Nasal Cannula in Infants with Bronchiolitis. Children 2021, 8, 66. [Google Scholar] [CrossRef] [PubMed]
- Ryu, J.H.; Azadeh, N.; Samhouri, B.; Yi, E. Recent Advances in the Understanding of Bronchiolitis in Adults. F1000Research 2020, 9, 568. [Google Scholar] [CrossRef]
- Franklin, D.; Shellshear, D.; Babl, F.E.; Hendrickson, R.; Williams, A.; Gibbons, K.; McEnery, K.; Kennedy, M.; Pham, T.M.T.; Acworth, J.; et al. High Flow in Children with Respiratory Failure: A Randomised Controlled Pilot Trial—A Paediatric Acute Respiratory Intervention Study. J. Paediatr. Child Health 2021, 57, 273–281. [Google Scholar] [CrossRef]
- Lin, J.; Zhang, Y.; Xiong, L.; Liu, S.; Gong, C.; Dai, J. High-Flow Nasal Cannula Therapy for Children with Bronchiolitis: A Systematic Review and Meta-Analysis. Arch. Dis. Child. 2019, 104, 564–576. [Google Scholar] [CrossRef]
- Dafydd, C.; Saunders, B.J.; Kotecha, S.J.; Edwards, M.O. Efficacy and Safety of High Flow Nasal Oxygen for Children with Bronchiolitis: Systematic Review and Meta-Analysis. BMJ Open Respir. Res. 2021, 8, e000844. [Google Scholar] [CrossRef]
- Kepreotes, E.; Whitehead, B.; Attia, J.; Oldmeadow, C.; Collison, A.; Searles, A.; Goddard, B.; Hilton, J.; Lee, M.; Mattes, J. High-Flow Warm Humidified Oxygen versus Standard Low-Flow Nasal Cannula Oxygen for Moderate Bronchiolitis (HFWHO RCT): An Open, Phase 4, Randomised Controlled Trial. Lancet 2017, 389, 930–939. [Google Scholar] [CrossRef]
- Sarkar, M.; Sinha, R.; Roychowdhoury, S.; Mukhopadhyay, S.; Ghosh, P.; Dutta, K.; Ghosh, S. Comparative Study between Noninvasive Continuous Positive Airway Pressure and Hot Humidified High-Flow Nasal Cannulae as a Mode of Respiratory Support in Infants with Acute Bronchiolitis in Pediatric Intensive Care Unit of a Tertiary Care Hospital. Indian J. Crit. Care Med. 2018, 22, 85–90. [Google Scholar] [CrossRef]
- Vahlkvist, S.; Jürgensen, L.; la Cour, A.; Markoew, S.; Petersen, T.H.; Kofoed, P.E. High Flow Nasal Cannula and Continuous Positive Airway Pressure Therapy in Treatment of Viral Bronchiolitis: A Randomized Clinical Trial. Eur. J. Pediatr. 2020, 179, 513–518. [Google Scholar] [CrossRef] [PubMed]
- Milési, C.; Essouri, S.; Pouyau, R.; Liet, J.M.; Afanetti, M.; Portefaix, A.; Baleine, J.; Durand, S.; Combes, C.; Douillard, A.; et al. High Flow Nasal Cannula (HFNC) versus Nasal Continuous Positive Airway Pressure (NCPAP) for the Initial Respiratory Management of Acute Viral Bronchiolitis in Young Infants: A Multicenter Randomized Controlled Trial (TRAMONTANE Study). Intensive Care Med. 2017, 43, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Dharmage, S.C.; Perret, J.L.; Custovic, A. Epidemiology of Asthma in Children and Adults. Front. Pediatr. 2019, 7, 246. [Google Scholar] [CrossRef] [PubMed]
- Basnet, S.; Mander, G.; Andoh, J.; Klaska, H.; Verhulst, S.; Koirala, J. Safety, Efficacy, and Tolerability of Early Initiation of Noninvasive Positive Pressure Ventilation in Pediatric Patients Admitted with Status Asthmaticus: A Pilot Study. Pediatr. Crit. Care Med. 2012, 13, 393–398. [Google Scholar] [CrossRef] [PubMed]
- Baudin, F.; Buisson, A.; Vanel, B.; Massenavette, B.; Pouyau, R.; Javouhey, E. Nasal High Flow in Management of Children with Status Asthmaticus: A Retrospective Observational Study. Ann. Intensive Care 2017, 7, 55. [Google Scholar] [CrossRef] [PubMed]
- González Martínez, F.; González Sánchez, M.I.; Toledo del Castillo, B.; Pérez Moreno, J.; Medina Muñoz, M.; Rodríguez Jiménez, C.; Rodríguez Fernández, R. Treatment with High-Flow Oxygen Therapy in Asthma Exacerbations in a Paediatric Hospital Ward: Experience from 2012 to 2016. An. Pediatr. 2019, 90, 72–78. [Google Scholar] [CrossRef]
- Ballestero, Y.; De Pedro, J.; Portillo, N.; Martinez-Mugica, O.; Arana-Arri, E.; Benito, J. Pilot Clinical Trial of High-Flow Oxygen Therapy in Children with Asthma in the Emergency Service. J. Pediatr. 2018, 194, 204–210.e3. [Google Scholar] [CrossRef] [PubMed]
- Duan, X.; Wei, N.; Wei, J.; Zhu, Y.; Kang, Y.; He, Y.; Huang, J.; Wang, S. Effect of High-Flow Nasal Cannula Oxygen Therapy on Pediatric Patients With Congenital Heart Disease in Procedural Sedation: A Prospective, Randomized Trial. J. Cardiothorac. Vasc. Anesth. 2021, 35, 2913–2919. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.H.; Choi, J.H.; Lee, J. The Changes of Central Venous Pressure by Body Posture and Positive End-Expiratory Pressure. Korean J. Anesthesiol. 2009, 57, 723–728. [Google Scholar] [CrossRef]
- Dysart, K.; Miller, T.L.; Wolfson, M.R.; Shaffer, T.H. Research in High Flow Therapy: Mechanisms of Action. Respir. Med. 2009, 103, 1400–1405. [Google Scholar] [CrossRef] [PubMed]
- Shioji, N.; Kanazawa, T.; Iwasaki, T.; Shimizu, K.; Suemori, T.; Kuroe, Y.; Morimatsu, H. High-Flow Nasal Cannula versus Noninvasive Ventilation for Postextubation Acute Respiratory Failure after Pediatric Cardiac Surgery. Acta Med. Okayama 2019, 73, 15–20. [Google Scholar] [CrossRef]
- McGinley, B.; Halbower, A.; Schwartz, A.R.; Smith, P.L.; Patil, S.P.; Schneider, H. Effect of a High-Flow Open Nasal Cannula System on Obstructive Sleep Apnea in Children. Pediatrics 2009, 124, 179–188. [Google Scholar] [CrossRef]
- Ignatiuk, D.; Schaer, B.; McGinley, B. High Flow Nasal Cannula Treatment for Obstructive Sleep Apnea in Infants and Young Children. Pediatr. Pulmonol. 2020, 55, 2791–2798. [Google Scholar] [CrossRef]
- Hawkins, S.; Huston, S.; Campbell, K.; Halbower, A. High-Flow, Heated, Humidified Air via Nasal Cannula Treats CPAP-Intolerant Children with Obstructive Sleep Apnea. J. Clin. Sleep Med. 2017, 13, 981–989. [Google Scholar] [CrossRef]
- Joseph, L.; Goldberg, S.; Shitrit, M.; Picard, E. High-Flow Nasal Cannula Therapy for Obstructive Sleep Apnea in Children. J. Clin. Sleep Med. 2015, 11, 1007–1010. [Google Scholar] [CrossRef] [Green Version]
- Jain, S.; Williams, D.J.; Arnold, S.R.; Ampofo, K.; Bramley, A.M.; Reed, C.; Stockmann, C.; Anderson, E.J.; Grijalva, C.G.; Self, W.H.; et al. Community-Acquired Pneumonia Requiring Hospitalization among U.S. Children. N. Engl. J. Med. 2015, 372, 835–845. [Google Scholar] [CrossRef] [PubMed]
- Kwon, J.W. High-Flow Nasal Cannula Oxygen Therapy in Children: A Clinical Review. Korean J. Pediatr. 2020, 63, 3–7. [Google Scholar] [CrossRef] [PubMed]
- 33. Liu, C.; Cheng, W.Y.; Li, J.S.; Tang, T.; Tan, P.L.; Yang, L. High-Flow Nasal Cannula vs. Continuous Positive Airway Pressure Therapy for the Treatment of Children <2 Years With Mild to Moderate Respiratory Failure Due to Pneumonia. Front. Pediatr. 2020, 8, 590906. [Google Scholar] [CrossRef]
- Wiser, R.K.; Smith, A.C.; Ma, B.B.K.; Chen, J.G. A Pediatric High-Flow Nasal Cannula Protocol Standardized Initial Flow and Expedites Weaning. Pediatr Pulmonol. 2021, 56, 1189–1197. [Google Scholar] [CrossRef]
- Sayan, İ.; Altınay, M.; Çınar, A.S.; Türk, H.Ş.; Peker, N.; Şahin, K.; Coşkun, N.; Demir, G.D. Impact of HFNC Application on Mortality and Intensive Care Length of Stay in Acute Respiratory Failure Secondary to COVID-19 Pneumonia. Hear. Lung 2021, 50, 425–429. [Google Scholar] [CrossRef] [PubMed]
- Moreel, L.; Proesmans, M. High Flow Nasal Cannula as Respiratory Support in Treating Infant Bronchiolitis: A Systematic Review. Eur. J. Pediatr. 2020, 179, 711–718. [Google Scholar] [CrossRef]
- Lodeserto, F.J.; Lettich, T.M.; Rezaie, S.R. High-Flow Nasal Cannula: Mechanisms of Action and Adult and Pediatric Indications. Cureus 2018, 10, e3639. [Google Scholar] [CrossRef]
- Möller, W.; Celik, G.; Feng, S.; Bartenstein, P.; Meyer, G.; Eickelberg, O.; Schmid, O.; Tatkov, S. Nasal High Flow Clears Anatomical Dead Space in Upper Airway Models. J. Appl. Physiol. 2015, 118, 1525–1532. [Google Scholar] [CrossRef]
- Al-Subu, A.M.; Hagen, S.; Eldridge, M.; Boriosi, J. Aerosol Therapy through High Flow Nasal Cannula in Pediatric Patients. Expert Rev. Respir. Med. 2017, 11, 945–953. [Google Scholar] [CrossRef]
- Claure, N.; D’Ugard, C.; Bancalari, E. Elimination of Ventilator Dead Space during Synchronized Ventilation in Premature Infants. J. Pediatr. 2003, 143, 315–320. [Google Scholar] [CrossRef]
- Dassieu, G.; Brochard, L.; Benani, M.; Avenel, S.; Danan, C. Continuous Tracheal Gas Insufflation in Preterm Infants with Hyaline Membrane Disease: A Prospective Randomized Trial. Am. J. Respir. Crit. Care Med. 2000, 162, 826–831. [Google Scholar] [CrossRef] [PubMed]
- Danan, C.; Dassieu, G.; Janaud, J.C.; Brochard, L. Efficacy of Dead-Space Washout in Mechanically Ventilated Premature Newborns. Am. J. Respir. Crit. Care Med. 1996, 153, 1571–1576. [Google Scholar] [CrossRef] [PubMed]
- Liew, Z.; Fenton, A.C.; Harigopal, S.; Gopalakaje, S.; Brodlie, M.; O’Brien, C.J. Physiological Effects of High-Flow Nasal Cannula Therapy in Preterm Infants. Arch. Dis. Child. Fetal Neonatal Ed. 2020, 105, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Nahum, A. Animal and Lung Model Studies of Tracheal Gas Insufflation. Respir. Care 2001, 46, 149–157. [Google Scholar] [PubMed]
- Saslow, J.G.; Aghai, Z.H.; Nakhla, T.A.; Hart, J.J.; Lawrysh, R.; Stahl, G.E.; Pyon, K.H. Work of Breathing Using High-Flow Nasal Cannula in Preterm Infants. J. Perinatol. 2006, 26, 476–480. [Google Scholar] [CrossRef] [PubMed]
- Shepard, J.W.; Burger, C.D. Nasal and Oral Flow-Volume Loops in Normal Subjects and Patients with Obstructive Sleep Apnea. Am. Rev. Respir. Dis. 1990, 142, 1288–1293. [Google Scholar] [CrossRef]
- Luo, J.; Duke, T.; Chisti, M.J.; Kepreotes, E.; Kalinowski, V.; Li, J. Efficacy of High-Flow Nasal Cannula vs. Standard Oxygen Therapy or Nasal Continuous Positive Airway Pressure in Children with Respiratory Distress: A Meta-Analysis. J. Pediatr. 2019, 215, 199–208.e8. [Google Scholar] [CrossRef]
- Habra, B.; Janahi, I.A.; Dauleh, H.; Chandra, P.; Veten, A. A Comparison between High-Flow Nasal Cannula and Noninvasive Ventilation in the Management of Infants and Young Children with Acute Bronchiolitis in the PICU. Pediatr. Pulmonol. 2020, 55, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Di Filippo, P.; Dodi, G.; Ciarelli, F.; Di Pillo, S.; Chiarelli, F.; Attanasi, M. Lifelong Lung Sequelae of Prematurity. Int. J. Environ. Res. Public Health 2022, 19, 5273. [Google Scholar] [CrossRef]
- Mayfield, S.; Jauncey-Cooke, J.; Hough, J.L.; Schibler, A.; Gibbons, K.; Bogossian, F. High-Flow Nasal Cannula Therapy for Respiratory Support in Children. Cochrane Database Syst. Rev. 2014, 2014, CD009850. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Myers, L.C.; Mark, D.; Ley, B.; Guarnieri, M.; Hofmeister, M.; Paulson, S.; Marelich, G.; Liu, V.X. Validation of Respiratory Rate-Oxygenation Index in Patients With COVID-19–Related Respiratory Failure. Crit. Care Med. 2022, 50, e638–e642. [Google Scholar] [CrossRef] [PubMed]
- Yildizdas, D.; Yontem, A.; Iplik, G.; Horoz, O.O.; Ekinci, F. Predicting Nasal High-Flow Therapy Failure by Pediatric Respiratory Rate-Oxygenation Index and Pediatric Respiratory Rate-Oxygenation Index Variation in Children. Eur. J. Pediatr. 2021, 180, 1099–1106. [Google Scholar] [CrossRef] [PubMed]
| Reference | Study design | Study Population | Comparison | Main Results |
|---|---|---|---|---|
| Baudin et al. [20] | Retrospective observational study | 73 PICU patients aged 1 to 18 years with severe asthma | HFNC vs. COT | Lower heart, better respiratory rates and blood gas in the first 24 h in the HFNC group |
| Martinez et al. [21] | Observational study | 536 children aged 4–5 years with moderate-to-severe asthma exacerbation | HFNC vs. COT | Lower PICU admissions in the HFNC group |
| Ballestero et al. [22] | Randomized pilot trial | 62 children aged 1 to 14 years with asthma exacerbation | HFNC vs. COT | Improvement in respiratory dynamics after two hours in the HFNC group compared with the COT group |
| Disease | Reference | Study Design | Study Population | Comparison | Main Results |
|---|---|---|---|---|---|
| Congenital heart diseases | Shioji et al. [26] | Retrospective study | 35 children with congenital heart disease surgically corrected and acute respiratory failure | HFNC and NIV |
|
| OSAS | McGinley et al. [27] | Retrospective study | 12 children with a mean age of 10 years with mild-to-severe OSAS | HFNC vs. CPAP | Similar reductions in AHI in both groups |
| Ignatiuk et al. [28] | Retrospective study | 22 children with poor surgical candidacy or residual OSAS after surgery | HFNC vs. no intervention | Significant reduction in AHI with HFNC | |
| Hawkins et al. [29] | Observational study | 10 school-aged patients with OSAS treated with HFNC | HFNC vs. no intervention |
| |
| Pneumonia | Liu et al. [33] | RCT | 84 children < 2 years with pneumonia and mild to moderate respiratory failure | HFNC and CPAP |
|
| Standard Oxygen Therapy | High-Flow Nasal Cannula | Continuous Positive Airway Pressure | |
|---|---|---|---|
| Optimal gas conditioning | / | +++ | + |
| Generation of positive end-expiratory pressure | / | + | +++ |
| Wash-out of nasopharyngeal dead space | / | +++ | + |
| Improvement in mucociliary clearance | / | +++ | / |
| Flow and oxygen concentration setting | / | +++ | +++ |
| Reduced breathing effort | / | ++ | +++ |
| Reduction in upper airway resistance | / | + | +++ |
| Patient’s comfort | ++ | + | / |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Venanzi, A.; Di Filippo, P.; Santagata, C.; Di Pillo, S.; Chiarelli, F.; Attanasi, M. Heated Humidified High-Flow Nasal Cannula in Children: State of the Art. Biomedicines 2022, 10, 2353. https://doi.org/10.3390/biomedicines10102353
Venanzi A, Di Filippo P, Santagata C, Di Pillo S, Chiarelli F, Attanasi M. Heated Humidified High-Flow Nasal Cannula in Children: State of the Art. Biomedicines. 2022; 10(10):2353. https://doi.org/10.3390/biomedicines10102353
Chicago/Turabian StyleVenanzi, Annamaria, Paola Di Filippo, Chiara Santagata, Sabrina Di Pillo, Francesco Chiarelli, and Marina Attanasi. 2022. "Heated Humidified High-Flow Nasal Cannula in Children: State of the Art" Biomedicines 10, no. 10: 2353. https://doi.org/10.3390/biomedicines10102353
APA StyleVenanzi, A., Di Filippo, P., Santagata, C., Di Pillo, S., Chiarelli, F., & Attanasi, M. (2022). Heated Humidified High-Flow Nasal Cannula in Children: State of the Art. Biomedicines, 10(10), 2353. https://doi.org/10.3390/biomedicines10102353








