Current Understanding of Pain Neurophysiology among Physiotherapists Practicing in Saudi Arabia
Abstract
:1. Introduction
2. Methods and Materials
2.1. Data Collection
2.1.1. Participants
2.1.2. Procedure
2.1.3. Sample Size Calculation
2.1.4. Analysis
3. Results
3.1. Demographics
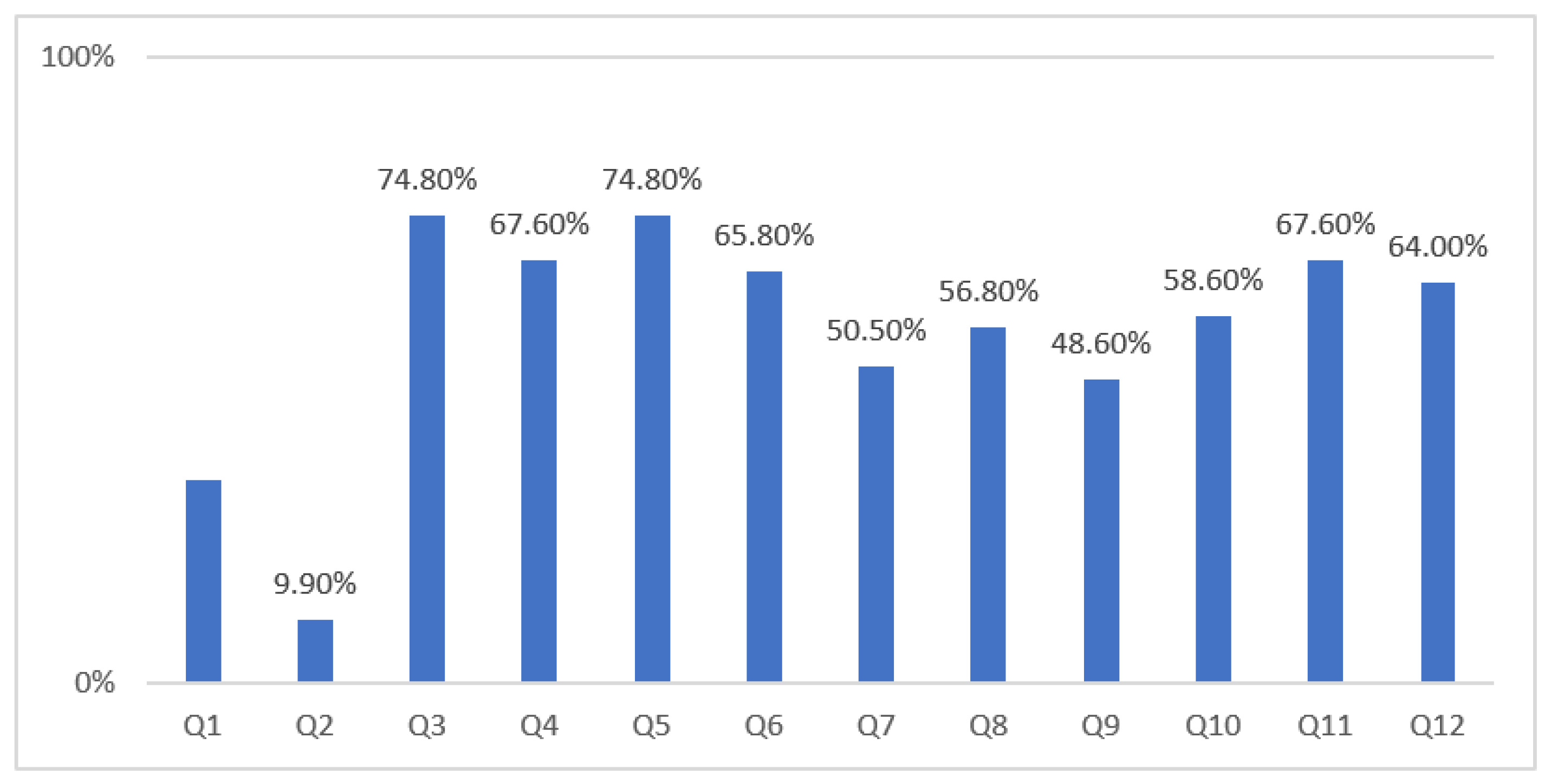
3.2. RNPQ Scores
3.3. RNPQ Scores Based on PTs’ Personal and Professional Characteristics
4. Discussion
Clinical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Leeuw, M.; Goossens, M.E.; Linton, S.J.; Crombez, G.; Boersma, K.; Vlaeyen, J.W. The fear-avoidance model of musculoskeletal pain: Current state of scientific evidence. J. Behav. Med. 2007, 30, 77–94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eccleston, C.; Crombez, G. Worry and chronic pain: A misdirected problem solving model. Pain 2007, 132, 233–236. [Google Scholar] [CrossRef]
- Moseley, G.L. Reconceptualising pain according to modern pain science. Phys. Ther. Rev. 2007, 12, 169–178. [Google Scholar] [CrossRef]
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef] [Green Version]
- Moseley, G.L.; Nicholas, M.K.; Hodges, P.W. A randomized controlled trial of intensive neurophysiology education in chronic low back pain. Clin. J. Pain 2004, 20, 324–330. [Google Scholar] [CrossRef]
- Louw, A.; Diener, I.; Butler, D.S.; Puentedura, E.J. The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Arch. Phys. Med. Rehabil. 2011, 92, 2041–2056. [Google Scholar] [CrossRef]
- Moayedi, M.; Davis, K.D. Theories of pain: From specificity to gate control. J. Neurophysiol. 2013, 109, 5–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moseley, G.L.; Butler, D.S. Fifteen years of explaining pain: The past, present, and future. J. Pain 2015, 16, 807–813. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- King, R.; Robinson, V.; Elliott-Button, H.L.; Watson, J.A.; Ryan, C.G.; Martin, D.J. Pain reconceptualisation after pain neurophysiology education in adults with chronic low back pain: A qualitative study. Pain Res. Manag. 2018, 12, 3745651. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nijs, J.; Roussel, N.; van Wilgen, C.P.; Köke, A.; Smeets, R. Thinking beyond muscles and joints: Therapists’ and patients’ attitudes and beliefs regarding chronic musculoskeletal pain are key to applying effective treatment. Man. Ther. 2013, 18, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Adillón, C.; Lozano, È.; Salvat, I. Comparison of pain neurophysiology knowledge among health sciences students: A cross-sectional study. BMC Res. Notes 2015, 8, 592. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alodaibi, F.; Alhowimel, A.; Alsobayel, H. Pain neurophysiology knowledge among physical therapy students in Saudi Arabia: A cross-sectional study. BMC Med. Educ. 2018, 18, 228–233. [Google Scholar] [CrossRef]
- Strong, J.; Tooth, L.; Unruh, A. Knowledge about pain among newly graduated occupational therapists: Relevance for curriculum development. Can. J. Occup. Ther. 1999, 66, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.M.; Wyant, S.L. Pain management content in curricula of US schools of pharmacy. J. Am. Pharm. Assoc. 2003, 43, 34–40. [Google Scholar]
- Watt-Watson, J.; Hunter, J.; Pennefather, P. An integrated undergraduate pain curriculum, based on IASP curricula, for six health science faculties. Pain 2004, 110, 140–148. [Google Scholar] [CrossRef] [PubMed]
- Watt-Watson, J.; McGillion, M.; Hunter, J. A survey of prelicensure pain curricula in health science faculties in Canadian universities. Pain Res. Manag. 2009, 14, 439–444. [Google Scholar] [CrossRef] [PubMed]
- Briggs, E.V.; Carrl, E.C.; Whittaker, M.S. Survey of undergraduate pain curricula for healthcare professionals in the United Kingdom. Eur. J. Pain 2011, 15, 789–795. [Google Scholar] [CrossRef] [PubMed]
- Bement, M.K.H.; Sluka, K.A. The current state of physical therapy pain curricula in the United States: A faculty survey. J. Pain 2015, 16, 144–152. [Google Scholar] [CrossRef] [Green Version]
- El-Metwally, A.; Shaikh, Q.; Aldiab, A. The prevalence of chronic pain and its associated factors among Saudi Al-Kharj population; a cross sectional study. BMC Musculoskelet. Disord. 2019, 20, 177–186. [Google Scholar] [CrossRef] [PubMed]
- Almalki, M.T.; BinBaz, S.S.; Alamri, S.S. Prevalence of chronic pain and high-impact chronic pain in Saudi Arabia. Saudi Med. J. 2019, 40, 1256. [Google Scholar] [CrossRef]
- Catley, M.J.; O’Connell, N.E.; Moseley, G.L. How good is the neurophysiology of pain questionnaire? A Rasch analysis of psychometric properties. J. Pain 2013, 14, 818–827. [Google Scholar] [CrossRef]
- Saudi Commission for Health Specialties. Health Workforce. 2018. Available online: https://www.scfhs.org.sa/Media/DigitalLibrary/DocumentLibrary/OtherPublications/Pages/default.aspx (accessed on 3 August 2021).
- Mukoka, G.; Olivier, B.; Ravat, S. Level of knowledge, attitudes and beliefs towards patients with chronic low back pain among final School of Therapeutic Sciences students at the University of the Witwatersrand–a cross-sectional study. South African Journal of Physiotherapy 2019, 75, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Marques, E.S.; Xarles, T.; Antunes, T.M. Evaluation of physiologic pain knowledge by physiotherapy students. Rev. Dor 2016, 17, 29–33. [Google Scholar] [CrossRef]
- Moseley, G.L. Unraveling the barriers to reconceptualization of the problem in chronic pain: The actual and perceived ability of patients and health professionals to understand the neurophysiology. J. Pain 2003, 4, 184–189. [Google Scholar] [CrossRef]
- Buchbinder, R.; Jolley, D.; Wyatt, M. Population based intervention to change back pain beliefs and disability: Three-part evaluation. BMJ 2001, 322, 1516–1520. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burton, A.K.; Waddell, G.; Tillotson, K.M.; Summerton, N. Information and advice to patients with back pain can have a positive effect: A randomized controlled trial of a novel educational booklet in primary care. Spine 1999, 24, 2484–2491. [Google Scholar] [CrossRef] [PubMed]
- Pitance, L.; Brasseur, P.; Rondeaux, C. Does a two-day postgraduate course on the management of chronic musculo-skeletal pain increases the physiotherapists’ pain neurophysiology knowledge? Man. Ther. 2016, 25, e165–e166. [Google Scholar] [CrossRef]
- Latimer, J.; Maher, C.; Refshauge, K. The attitudes and beliefs of physiotherapy students to chronic back pain. Clin. J. Pain 2004, 20, 45–50. [Google Scholar] [CrossRef]
- Cox, T.; Louw, A.; Puentedura, E.J. An abbreviated therapeutic neuroscience education session improves pain knowledge in first-year physical therapy students but does not change attitudes or beliefs. J. Man. Manip. Ther. 2017, 25, 11–21. [Google Scholar] [CrossRef] [Green Version]
- Colleary, G.; O’Sullivan, K.; Griffin, D.; Ryan, C.G.; Martin, D.J. Effect of pain neurophysiology education on physiotherapy students’ understanding of chronic pain, clinical recommendations and attitudes towards people with chronic pain: A randomised controlled trial. Physiotherapy 2017, 103, 423–429. [Google Scholar] [CrossRef] [Green Version]
- Ferreira, P.S.; Corrêa, L.A.; Bittencourt, J.V.; Reis, F.J.; Meziat-Filho, N.; Nogueira, L.A. Patients with chronic musculoskeletal pain present low level of the knowledge about the neurophysiology of pain. Eur. J. Physiother. 2019, 11, 1–6. [Google Scholar] [CrossRef]
- Lee, H.; McAuley, J.H.; Hübscher, M. Does changing pain related knowledge reduce pain and improve function through changes in catastrophizing? Pain 2016, 157, 922–930. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fletcher, C.; Bradnam, L.; Barr, C. The relationship between knowledge of pain neurophysiology and fear avoidance in people with chronic pain: A point in time, observational study. Physiother. Theory Pract. 2016, 32, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Meeus, M.; Nijs, J.; Van Oosterwijck, J. Pain physiology education improves pain beliefs in patients with chronic fatigue syndrome compared with pacing and self-management education: A double-blind randomized controlled trial. Arch. Phys. Med. Rehabil. 2010, 91, 1153–1159. [Google Scholar] [CrossRef]
| Variabe | Category | n | % |
|---|---|---|---|
| Gender | Male | 65 | 58.6 |
| Female | 46 | 41.4 | |
| Age | 20–25 | 16 | 14.4 |
| 26–30 | 35 | 31.5 | |
| 31–35 | 25 | 22.5 | |
| 36–40 | 23 | 20.7 | |
| 41–45 | 4 | 3.6 | |
| 46–50 | 7 | 6.3 | |
| Above 50 | 1 | 0.9 | |
| Job title | Physical therapist I | 65 | 58.6 |
| Physical therapist II | 33 | 29.7 | |
| Consultant | 13 | 11.7 | |
| Level of education | BSc | 57 | 52.3 |
| MSc | 34 | 29.7 | |
| PhD | 16 | 14.4 | |
| DPT | 4 | 3.6 | |
| Country from which the highest degree qualification was acquired | Saudi Arabia | 68 | 62.2 |
| US | 14 | 12.6 | |
| UK | 19 | 16.2 | |
| Australia | 2 | 1.8 | |
| Other | 8 | 7.2 | |
| Workplace | Governmental hospital/clinic | 65 | 55.1 |
| Academia/university | 21 | 17.8 | |
| Private hospital/clinic | 32 | 27.1 | |
| Years of experience | Less than 2 years | 27 | 24.3 |
| 2–5 | 28 | 25.2 | |
| 6–10 | 18 | 16.2 | |
| 11–15 | 26 | 23.4 | |
| 16–20 | 4 | 3.6 | |
| More than 20 years | 8 | 7.2 | |
| Province/region of practice | Central region (Riyadh) | 57 | 51.4 |
| Central region (out of Riyadh) | 11 | 9.9 | |
| Northern region | 3 | 2.7 | |
| Western region | 19 | 17.1 | |
| Eastern region | 10 | 9.0 | |
| Southern region | 11 | 9.9 |
| Variabe | Category | n | Mean ± SD | p * |
|---|---|---|---|---|
| Sex | Male | 65 | 6.8 ± 2.3 | 0.61 |
| Female | 46 | 6.6 ± 2.1 | ||
| Level of education | BSc | 58 | 6.4 ± 2.1 | 0.43 |
| MSc | 33 | 7.1 ± 2.0 | ||
| PhD | 16 | 7.1 ± 2.8 | ||
| DPT | 4 | 6.3 ± 2.2 | ||
| Country from which the highest degree qualification was acquired | Saudi Arabia | 69 | 6.5 ± 2.1 | 0.16 |
| US | 14 | 7.6 ± 2.0 | ||
| UK | 18 | 6.6 ± 2.6 | ||
| Australia | 2 | 9.5 ± 0.7 | ||
| Other | 8 | 7.0 ± 2.0 | ||
| Province/region of practice | Central region (Riyadh) | 57 | 7.2 ± 2.4 | 0.05 |
| Central region (out of Riyadh) | 11 | 6.0 ± 1.8 | ||
| Northern region | 3 | 7.3 ± 1.2 | ||
| Western region | 19 | 5.8 ± 1.9 | ||
| Eastern region | 10 | 7.5 ± 1.8 | ||
| Southern region | 11 | 5.6 ± 1.4 | ||
| Years of experience | Less than 2 years | 27 | 6.5± 1.5 | 0.93 |
| 2–5 | 28 | 6.9± 2.5 | ||
| 6–10 | 18 | 6.7± 2.3 | ||
| 11–15 | 26 | 6.8± 2.1 | ||
| 16–20 | 4 | 5.8± 2.2 | ||
| More than 20 years | 8 | 6.7± 3.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alhowimel, A.; Alodiabi, F.; Alamam, D.; Alotaibi, M.; Fritz, J. Current Understanding of Pain Neurophysiology among Physiotherapists Practicing in Saudi Arabia. Healthcare 2021, 9, 1242. https://doi.org/10.3390/healthcare9091242
Alhowimel A, Alodiabi F, Alamam D, Alotaibi M, Fritz J. Current Understanding of Pain Neurophysiology among Physiotherapists Practicing in Saudi Arabia. Healthcare. 2021; 9(9):1242. https://doi.org/10.3390/healthcare9091242
Chicago/Turabian StyleAlhowimel, Ahmed, Faris Alodiabi, Dalyah Alamam, Mazyad Alotaibi, and Julie Fritz. 2021. "Current Understanding of Pain Neurophysiology among Physiotherapists Practicing in Saudi Arabia" Healthcare 9, no. 9: 1242. https://doi.org/10.3390/healthcare9091242
APA StyleAlhowimel, A., Alodiabi, F., Alamam, D., Alotaibi, M., & Fritz, J. (2021). Current Understanding of Pain Neurophysiology among Physiotherapists Practicing in Saudi Arabia. Healthcare, 9(9), 1242. https://doi.org/10.3390/healthcare9091242






