Reliability and Validity of the Korean Late-Life Function and Disability Instrument
Abstract
:1. Background
2. Methods
2.1. Subjects
2.2. Assessment Tool: Late-Life Function and Disability Instrument (LLFDI)
2.3. Procedure
2.4. Stage 1: Translation and Back-Translation of the LLFDI
2.5. Stage 2: Cultural Adaptation
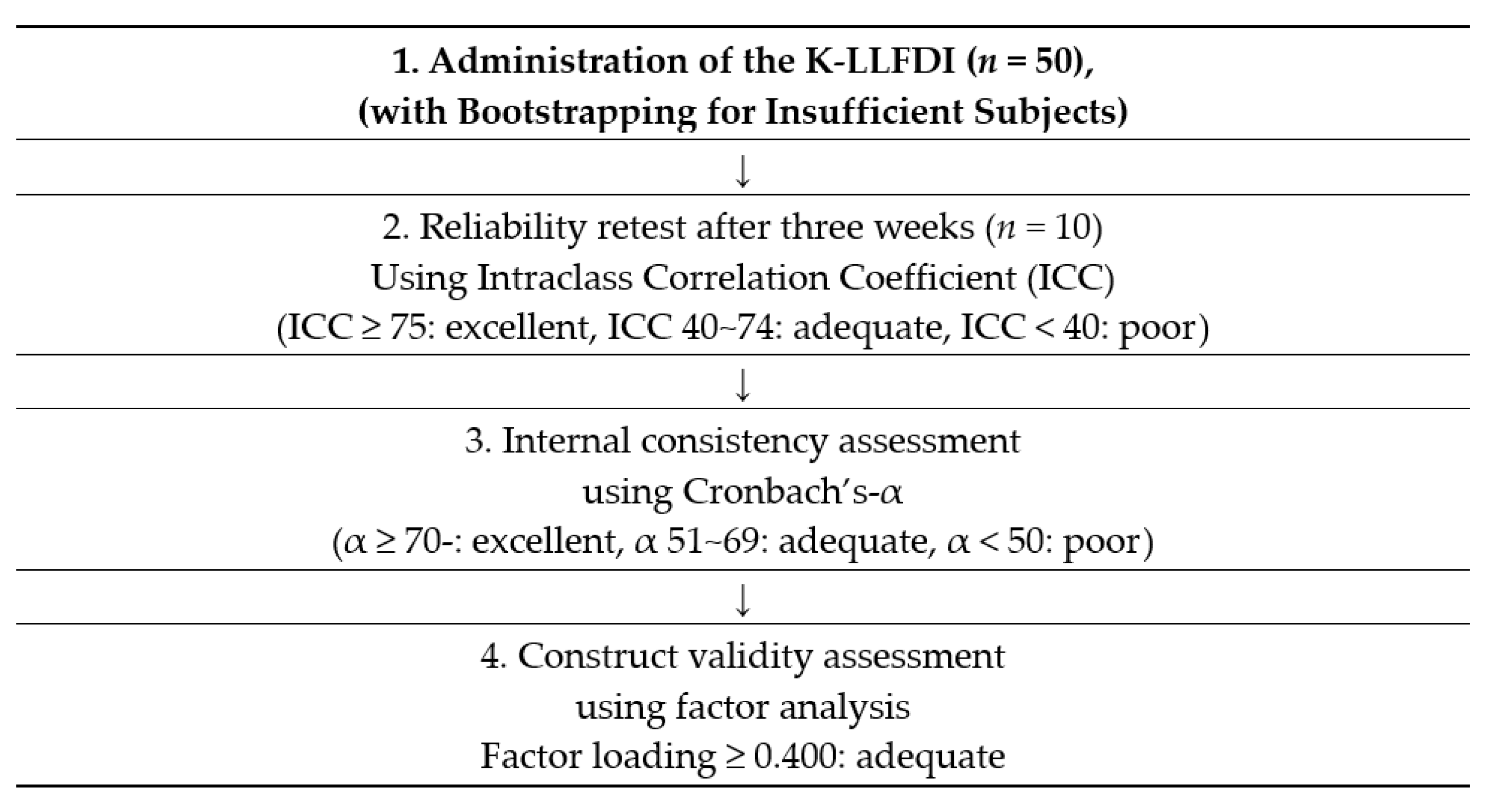
2.6. Stage 3: Reliability and Validity Analysis
2.7. Statistical Analysis
3. Results
3.1. Cultural Adaptation
3.2. Reliability Analysis
3.2.1. Test–Retest Reliability
3.2.2. Internal Consistency
3.3. Validity Analysis
Construct Validity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Korean Educational Psychology Association. Glossary of Educational Psychology; Hakjisa: Seoul, Korea, 2000. [Google Scholar]
- Kim, T.H.; Kim, D.B.; Kim, M.H.; Lee, Y.J.; Kim, A.S. A study on improvement of the quality of life for the aged. J. Korean Gerontol. Soc. 1999, 19, 61–81. [Google Scholar]
- Kim, S.Y.; Han, M.J. Mortality Forecasting for 2016 Korean Population Projection. Korea J. Popul. Stud. 2017, 40, 1–25. [Google Scholar]
- Balzi, D.; Lauretani, F.; Barchielli, A.; Ferrucci, L.; Banindelli, S.; Buiatti, A.; Guralnik, J.M. Risk factors for disability in older persons over 3-year follow-up. Age Ageing 2010, 39, 92–98. [Google Scholar] [CrossRef] [Green Version]
- Milan-Calenti, J.C.; Tubio, J.; Pita-Fernandez, S.; Gonzalez-Abraldes, I.; Lorenzo, T.; Fernabdez-Arruty, T.; Maseda, A. Prevalence of functional disability in activities of daily living (ADL), instrumental activities of daily living (IADL) and associated factors, as predictors of morbidity and mortality. Arch. Gerontol. Geriatr. 2010, 50, 306–310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keeler, E.; Guralnik, J.M.; Tian, H.; Wallace, R.B.; Reuben, D.B. The impact of functional status on life expectancy in older persons. J. Gerontol. Med. Sci. 2010, 65, 727–733. [Google Scholar] [CrossRef] [Green Version]
- Zanghì, A.; Avolio, C.; Amato, M.P.; Filippi, M.; Trojano, M.; Patti, F.; Emanuele, D.; Italian MS Register. First-line therapies in late-onset multiple sclerosis: An Italian registry study. Eur. J. Neurol. 2021, 1–7. [Google Scholar] [CrossRef]
- Crews, D.E.; Zavotka, S. Aging, disability, and frailty: Implications for universal design. J. Physiol. Anthropol. 2006, 25, 113118. [Google Scholar] [CrossRef] [Green Version]
- Guralnik, J.M.; Ferrucci, L. Assessing the building blocks of function. American. J. Prev. Med. 2003, 25, 112–121. [Google Scholar] [CrossRef]
- World Health Organization. Men, Ageing and Health: Achieving Health Across the Life Span (No. WHO/NMH/NPH/01.2); WHO: Geneva, Switzerland, 2001. [Google Scholar]
- Lee, C.G.; Park, H.; Cho, H.J. Comparison of the functional evaluation scales in rehabilitation medicine. J. Korean Acad. Rehabil. Med. 1994, 18, 7. [Google Scholar]
- Lee, J.H.; Hwang, C.M.; Kim, H.S.; Ahn, K.H. Comparison study for the Modified Barthel Index (MBI) and Functional Independence Measure (FIM) in patients with CVA. Ann. Rehabil. Med. 1995, 19, 271–280. [Google Scholar]
- Chaves, G.F.S.; Oliveira, A.M.; Forlenza, O.V.; Nunes, P.V. Evaluation scales for occupational therapy in Brazil. Rev. De Ter. Ocup. Da Univ. De Sao Paulo 2010, 21, 240–246. [Google Scholar]
- Jette, A.M.; Haley, S.M.; Coster, W.J.; Kooyoomjian, J.T.; Levenson, S.; Heeren, T.; Ashba, J. Late Life Function and Disability Instrument: I. Development and evaluation of the disability component. J. Gerontol. 2002, 57, 209–216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gignac, M.A.; Cao, X.; Mcalpine, J.; Badley, E.M. Measures of disability: Arthritis impact measurement scales. Arthritis Care Res. 2011, 63, 308–324. [Google Scholar] [CrossRef] [PubMed]
- Melzer, I.; Kurz, I.; Sarid, O.; Jette, A.M. Relationship between self-reported function and disability and balance performance measures in the elderly. J. Rehabil. Res. Dev. 2007, 44, 685–691. [Google Scholar] [CrossRef] [PubMed]
- Roaldsen, K.S.; Halvarsson, A.; Sarlija, B.; Franzen, E.; Staåhle, A. Self-reported function and disability in late life—Cross-cultural adaptation and validation of the Swedish version of the Late-Life Function and Disability Instrument. Disabil. Rehabil. 2014, 36, 813–817. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sakakibara, B.M.; Routhier, F.; Lavoie, M.P.; Miller, W.C. Reliability and validity of the French-Canadian Late Life Function and Disability Instrument in community-living wheelchair-users. Scand. J. Occup. Ther. 2013, 20, 365–373. [Google Scholar] [CrossRef]
- de Almeida, M.H.M.; Toldrá, R.C.; Batista, M.P.P.; Souto, A.C.F. Reliability and validity of the Brazilian version of the Late-Life Function and Disability Instrument. Am. J. Occup. Ther. 2016, 70, 7002290050. [Google Scholar]
- Song, H. Content and cultural validity of scales within the Korean context. Korean J. Child Stud. 2017, 38, 1–3. [Google Scholar] [CrossRef] [Green Version]
- Polit, D.F.; Beck, C.T. The content validity index: Are you sure you know what’s being reported? Critique and recommendations. Res. Nurs. Health 2006, 29, 489–497. [Google Scholar] [CrossRef] [Green Version]
- Lynn, M.R. Determination and quantification of content validity. Nurs. Res. 1986, 35, 382–385. [Google Scholar] [CrossRef]
- Waltz, C.F.; Strickland, O.L.; Lenz, E.R. (Eds.) Measurement in Nursing and Health Research; Springer: Berlin/Heidelberg, Germany, 2010. [Google Scholar]
- de Vet, H.C.; Terwee, C.B.; Mokkink, L.B.; Knol, D.L. Measurement in Medicine: A Practical Guide; Cambridge University Press: Cambridge, UK, 2011. [Google Scholar]
- Samuel, B.G.; Robert, W.; Lissitz Stanlen, A.M. Limitations of Coefficient Alpha as an Index of Test Unidimensionality. Educ. P Sychological Meas. 1977, 37, 827–838. [Google Scholar]
- Haley, S.M.; Ludlow, L.; Coster, W.; Langmuir, L. Self-reporting of capable versus typical functional activity performance in community dwelling older adults: Is there a difference? J. Geriatr. Phys. Ther. 2002, 25, 3–10. [Google Scholar] [CrossRef]
| Categories | M(SD) | |
|---|---|---|
| Disability component | Social role | 19.18(6.681) |
| Personal role | 21.36(4.685) | |
| Instrumental role | 35.36(11.933) | |
| Management role | 11.58(3.970) | |
| Function component | Upper extremity | 31.56(3.913) |
| Basic lower extremity | 57.04(10.785) | |
| Advanced lower extremity | 35.44(13.135) | |
| Test–Retest, ICC [95% CI] | ||||
|---|---|---|---|---|
| Domain | Original | Swedish | Brazilian | Korean |
| Disability component | ||||
| Frequency | ||||
| Social role | 0.753 | 0.82 | 0.81 [0.52, 0.93] | 0.948 [0.816, 0.987] |
| Personal role | 0.633 | 0.53 [0.00, 0.82] | 0.795 [0.397, 0.944] | |
| Limitation | ||||
| Instrumental role | 0.833 | 0.91 | 0.59 [0.12, 0.85] | 0.904 [0.680, 0.975] |
| Management role | 0.435 | 0.27 [0.00, 0.70] | 0.964 [0.871, 0.991] | |
| Function component | ||||
| Upper extremity | 0.912 | 0.87 | 0.95 [0.86, 0.98] | 0.565 [-0.025, 0.869] |
| Basic lower extremity | 0.976 | 0.89 | 0.93 [0.81, 0.98] | 0.781 [0.366, 0.940] |
| Advanced lower extremity | 0.966 | 0.91 | 0.78 [0.44, 0.93] | 0.971 [0.895, 0.993] |
| Internal Consistency, Cronbach’s α | ||||
|---|---|---|---|---|
| Domain | Original | Swedish | Brazilian | Korean |
| Disability component | ||||
| Frequency | ||||
| Social role | 0.80 | 0.90 | 0.807 | 0.862 |
| Personal role | 0.73 | 0.601 | 0.725 | |
| Limitation | ||||
| Instrumental role | 0.92 | 0.95 | 0.856 | 0.914 |
| Management role | 0.63 | 0.611 | 0.771 | |
| Function component | ||||
| Upper extremity | 0.912 | 0.87 | 0.819 | 0.775 |
| Basic lower extremity | 0.976 | 0.89 | 0.889 | 0.929 |
| Advanced lower extremity | 0.966 | 0.91 | 0.914 | 0.956 |
| Disability Component | ||
|---|---|---|
| Domain | Item No. | Factor Loading |
| Social role | D1F | 0.440 |
| D2F | 0.533 | |
| D3F | 0.489 | |
| D5F | 0.901 | |
| D6F | 0.785 | |
| D9F | 0.780 | |
| D11F | 0.898 | |
| D12F | 0.620 | |
| D14F | 0.326 | |
| Personal role | D4F | 0.384 |
| D7F | 0.891 | |
| D8F | 0.152 | |
| D10F | 0.429 | |
| D13F | 0.506 | |
| D15F | 0.690 | |
| D16F | 0.460 | |
| Instrumental role | D2L | 0.797 |
| D3L | 0.624 | |
| D4L | 0.519 | |
| D5L | 0.905 | |
| D6L | 0.875 | |
| D9L | 0.771 | |
| D10L | 0.714 | |
| D12L | 0.651 | |
| D13L | 0.422 | |
| D14L | 0.469 | |
| D15L | 0.770 | |
| D16L | 0.400 | |
| Management role | D1L | 0.466 |
| D7L | 0.936 | |
| D8L | 0.327 | |
| D11L | 0.904 | |
| Function Component | ||
|---|---|---|
| Domain | Item No. | Factor Loading |
| Upper extremity | F1 | 0.543 |
| F3 | 0.313 | |
| F5 | 0.769 | |
| F6 | 0.575 | |
| F13 | 0.469 | |
| F16 | 0.619 | |
| F17 | 0.798 | |
| Basic lower extremity | F2 | 0.716 |
| F10 | 0.445 | |
| F11 | 0.762 | |
| F12 | 0.383 | |
| F14 | 0.812 | |
| F15 | 0.626 | |
| F18 | 0.801 | |
| F21 | 0.703 | |
| F22 | 0.866 | |
| F23 | 0.610 | |
| F25 | 0.698 | |
| F26 | 0.808 | |
| F28 | 0.790 | |
| F31 | 0.835 | |
| Advanced lower extremity | F4 | 0.854 |
| F7 | 0.785 | |
| F8 | 0.814 | |
| F9 | 0.931 | |
| F19 | 0.858 | |
| F20 | 0.964 | |
| F24 | 0.852 | |
| F27 | 0.637 | |
| F29 | 0.772 | |
| F30 | 0.827 | |
| F32 | 0.730 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, D.S.; Park, H.Y. Reliability and Validity of the Korean Late-Life Function and Disability Instrument. Healthcare 2021, 9, 1200. https://doi.org/10.3390/healthcare9091200
Park DS, Park HY. Reliability and Validity of the Korean Late-Life Function and Disability Instrument. Healthcare. 2021; 9(9):1200. https://doi.org/10.3390/healthcare9091200
Chicago/Turabian StylePark, Da Sol, and Hae Yean Park. 2021. "Reliability and Validity of the Korean Late-Life Function and Disability Instrument" Healthcare 9, no. 9: 1200. https://doi.org/10.3390/healthcare9091200
APA StylePark, D. S., & Park, H. Y. (2021). Reliability and Validity of the Korean Late-Life Function and Disability Instrument. Healthcare, 9(9), 1200. https://doi.org/10.3390/healthcare9091200







