Effects of Community-Based Programs on Integration into the Mental Health and Non-Mental Health Communities
Abstract
:1. Introduction
2. Method
2.1. Participants
2.2. Measures
2.2.1. Integration into the Mental Health Community
2.2.2. Integration into the Non-Mental Health Community
Physical Integration
Social Integration
Psychological Integration
2.2.3. Community-Based Program Environment
Program Atmosphere
Relationships with Patients and Staff
Program Involvement
2.2.4. Sociodemographic and Clinical Variables
2.3. Statistical Analysis
3. Results
3.1. Effects of Sociodemographic and Clinical Variables on Integration into the Mental Health and Non-Mental Health Communities
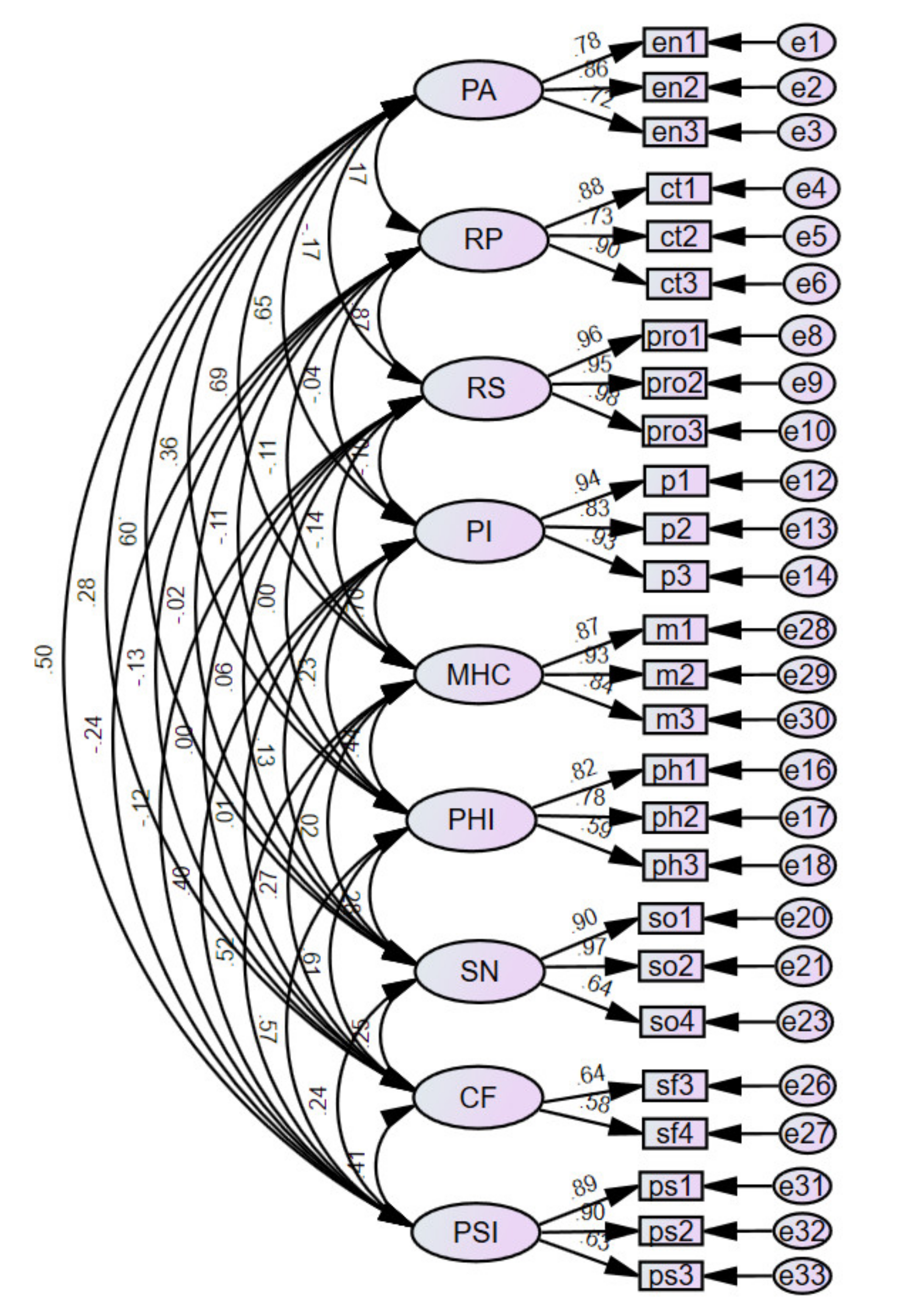
3.2. Confirmatory Factor Analysis
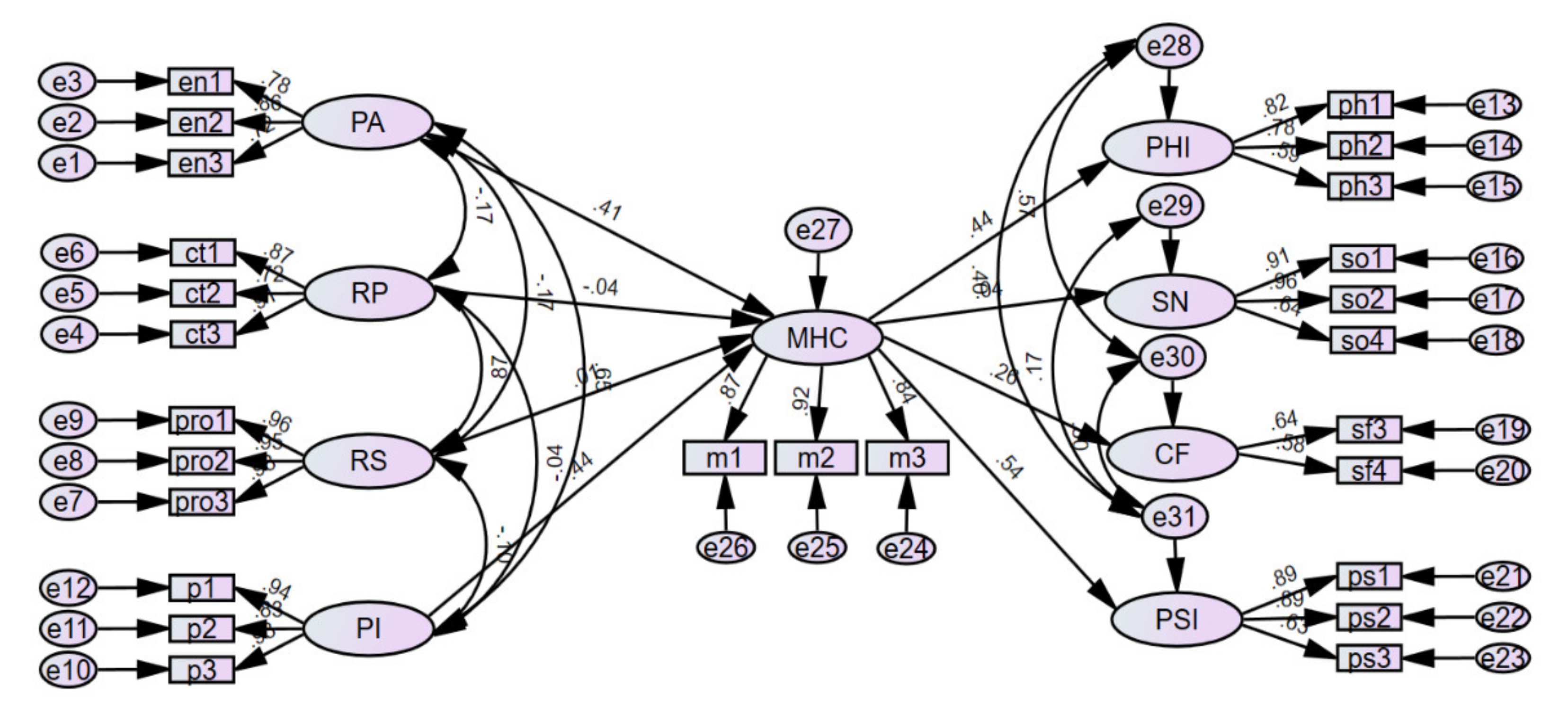
3.3. Research Model Verification
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Davidson, L.; Roe, D. Recovery from versus recovery in serious mental illness: One strategy for lessening confusion plaguing recovery. J. Ment. Health 2007, 16, 459–470. [Google Scholar] [CrossRef]
- Abdallah, C.; Cohen, C.I.; Sanchez-Almira, M.; Reyes, P.; Ramirez, P. Community integration and associated factors among older adults with schizophrenia. Psychiatr. Serv. 2009, 60, 1642–1648. [Google Scholar] [CrossRef]
- Bond, G.R.; Salyers, M.P.; Rollins, A.L.; Rapp, C.A.; Zipple, A.M. How evidence-based practices contribute to community integration. Community Ment. Health J. 2004, 40, 569–588. [Google Scholar] [CrossRef]
- Wong, Y.L.I.; Solomon, P.L. Community integration of persons with psychiatric disabilities in supportive independent housing: A conceptual model and methodological considerations. Ment. Health Serv. Res. 2002, 4, 13–28. [Google Scholar] [CrossRef]
- Cooper, A.E.; Corrigan, P.W.; Watson, A.C. Mental illness stigma and care-seeking. J. Nerv. Ment. Dis. 2003, 191, 339–341. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.H.; Seo, M.K. Community Integration of Persons with Mental Disorders Compared with the General Population. Int. J. Environ. Res. Public Health 2020, 17, 1596. [Google Scholar] [CrossRef] [Green Version]
- Wheat, K.; Brohan, E.; Henderson, C.; Thornicroft, G. Mental illness and the workplace: Conceal or reveal? J. R. Soc. Med. 2010, 103, 83–86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Korea Employment Agency for Persons with Disabilities (KEAD) & Employment Development Institute (EDI). 2020 Economic Activity Survey for the Disabled. Press Release on 18 December 2020. Available online: https://edi.kead.or.kr/BoardType01.do?bid=36&mid=220 (accessed on 2 August 2021).
- Ministry of Health and Welfare. National Mental Health Annual Report 2017; Ministry of Health and Welfare: Sejong, Korea, 2017.
- Callard, F.; Sartorius, N.; Arboleda-Flórez, J.; Bartlett, P.; Helmchen, H.; Stuart, H.; Taborda, J.; Thornicroft, G. Mental Illness, Discrimination, and the Law: Fighting for Social Justice; Wiley-Blackwell: Hoboken, NJ, USA, 2012; ISBN 978-1-119-95354-8. [Google Scholar]
- Sullivan, G.; Han, X.; Moore, S.; Kotrla, K. Disparities in hospitalization for diabetes among persons with and without co-occurring mental disorders. Psychiatr. Serv. 2006, 57, 1126–1131. [Google Scholar] [CrossRef] [PubMed]
- Wong, Y.L.I.; Sands, R.G.; Solomon, P.L. Conceptualizing community: The experience of mental health consumers. Qual. Health Res. 2010, 20, 654–667. [Google Scholar] [CrossRef]
- Mandiberg, J.M. The sword of reform has two sharp edges: Normalcy, normalization, and the destruction of the social group. New Dir. Ment. Health Serv. 2006, 1999, 31–44. [Google Scholar] [CrossRef] [PubMed]
- Mandiberg, J.M. Commentary: The failure of social inclusion: An alternative approach through community development. Psychiatr. Serv. 2012, 63, 458–460. [Google Scholar] [CrossRef] [PubMed]
- Lefley, H.P. What does “community” mean for persons with mental illness? New Dir. Ment. Health Serv. 2006, 1999, 3–12. [Google Scholar] [CrossRef]
- Corrigan, P.W.; Watson, A.C. The paradox of self-stigma and mental illness. Clin. Psychol. Sci. Pract. 2002, 9, 35–53. [Google Scholar] [CrossRef]
- Kruzich, J.M. Community integration of the mentally III in residential facilities. Am. J. Community Psychol. 1985, 13, 553–564. [Google Scholar] [CrossRef] [PubMed]
- Prince, P.N.; Prince, C.R. Perceived stigma and community integration among clients of assertive community treatment. Psychiatr. Rehabil. J. 2002, 25, 323–331. [Google Scholar] [CrossRef]
- Townley, G.; Miller, H.; Kloos, B. A little goes a long way: The impact of distal social support on community integration and recovery of individuals with psychiatric disabilities. Am. J. Community Psychol. 2013, 52, 84–96. [Google Scholar] [CrossRef]
- Wong, Y.L.I.; Matejkowski, J.; Lee, S. Social integration of people with serious mental illness: Network transactions and satisfaction. J. Behav. Health Serv. Res. 2011, 38, 51–67. [Google Scholar] [CrossRef] [Green Version]
- Gulcur, L.; Tsemberis, S.; Stefancic, A.; Greenwood, R.M. Community integration of adults with psychiatric disabilities and histories of homelessness. Community Ment. Health J. 2007, 43, 211–228. [Google Scholar] [CrossRef] [PubMed]
- Yanos, P.T.; Barrow, S.M.; Tsemberis, S. Community integration in the early phase of housing among homeless persons diagnosed with severe mental illness: Successes and challenges. Community Ment. Health J. 2004, 40, 133–150. [Google Scholar] [CrossRef] [PubMed]
- Min, S.Y. The process of predictors of community integration among persons with mental illnesses. Ment. Health Soc. Work 2009, 33, 36–68. [Google Scholar]
- Min, S.Y. The moderating effect of community cohesion on the relationship between neighborhood disorder and community integration among persons with mental illnesses. Korean J. Soc. Welf. 2015, 67, 57–82. [Google Scholar]
- Dickerson, F.B.; Sommerville, J.; Origoni, A.E.; Ringel, N.B.; Parente, F. Experiences of stigma among outpatients with schizophrenia. Schizophr. Bull. 2002, 28, 143–155. [Google Scholar] [CrossRef] [Green Version]
- Sherman, S.R.; Frenkel, E.R.; Newman, E.S. Community participation of mentally ill adults in foster family care. J. Community Psychol. 1986, 14, 120–133. [Google Scholar] [CrossRef]
- McColl, M.A.; Davies, D.; Carlson, P.; Johnston, J.; Minnes, P. The community integration measure: Development and preliminary validation. Arch. Phys. Med. Rehabil. 2001, 82, 429–434. [Google Scholar] [CrossRef]
- Segal, S.P.; Aviram, U. The Mentally Ill in Community-Based Sheltered Care; Wiley: New York, NY, USA, 1978; ISBN 0471774006. [Google Scholar]
- Aubry, T.; Myner, J. Community integration and quality of life: A comparison of persons with psychiatric disabilities in housing programs and community residents who are neighbours. Can. J. Community Ment. Health 1996, 15, 5–20. [Google Scholar] [CrossRef]
- Choi, Y.J. Recovery Strategies for the Person with Psychiatric Disabilities through Community Integration. Ph.D. Thesis, Pusan National University, Pusan, Korea, 2010. [Google Scholar]
- Buckner, J.C. The development of an instrument to measure neighborhood cohesion. Am. J. Community Psychol. 1988, 16, 771–791. [Google Scholar] [CrossRef]
- Moos, R. Assessment of the psychosocial environments of community-oriented psychiatric treatment programs. J. Abnorm. Psychol. 1972, 79, 9–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Booth, M.E. Effects of Program Factors on Client Outcomes: Evaluation of Three Clubhouse Programs for Persons with Severe Mental Illness. Ph.D. Thesis, Virginia Commonwealth University, Richmond, VA, USA, 1994. [Google Scholar]
- Lee, J.H. The Effects of Community Mental Health Program on the Social Integration of the Mentally Ill. Master’s Thesis, Gyeongsang National University, Jinju, Korea, 2005. [Google Scholar]
- Kim, S.I. A Study on Social Integration of the Mental Disorders Attend at Day Hospital: Focus on Environment Traits. Master’s Thesis, Ewha Woman’s University, Seoul, Korea, 1999. [Google Scholar]
- Lee, J.H.; Seo, M.K. A Study on effects of coercion by family and experts on the recovery attitude of the persons with mental illness. J. Korean Neuropsychiatr. Assoc. 2011, 50, 54–61. [Google Scholar]
- Bengtsson-Tops, A.; Hansson, L. Quantitative and qualitative aspects of the social network in schizophrenic patients living in the community. Relationship to sociodemographic characteristics and clinical factors and subjective quality of life. Int. J. Soc. Psychiatry 2001, 47, 67–77. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.C. A Study on the factors affecting community integration of persons with mental illness at home. J. Soc. Sci. 2013, 39, 151–177. [Google Scholar]
- Cabral, J.; Barreto Carvalho, C.; Motta, C.; Sousa, M. Characterization and predictors of community integration of people with psychiatric problems: Comparisons with the general population. Int. J. Soc. Behav. Educ. Econ. Manag. Eng. 2015, 9, 1748–1757. [Google Scholar] [CrossRef]
- Metraux, S.; Brusilovskiy, E.; Prvu-Bettger, J.A.; Wong, Y.L.I.; Salzer, M.S. Geographic access to and availability of community resources for persons diagnosed with severe mental illness in Philadelphia, USA. Health Place 2012, 18, 621–629. [Google Scholar] [CrossRef] [PubMed]
- Pahwa, R.; Bromley, E.; Brekke, B.; Gabrielian, S.; Braslow, J.T.; Brekke, J.S. Relationship of community integration of persons with severe mental illness and mental health service intensity. Psychiatr. Serv. 2014, 65, 822–825. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Seo, M.K. Effects of involvement in the programs and program environments on social adjustment and life satisfaction of the mental illness. Korean J. Soc. Welf. Stud. 2007, 35, 67–92. [Google Scholar]
- Eklund, M.; Hansson, L. Social network among people with persistent mental illness: Associations with sociodemographic, clinical and health-related factors. Int. J. Soc. Psychiatry 2007, 53, 293–305. [Google Scholar] [CrossRef]
| Variable | Category | Frequency | Percentage (%) |
|---|---|---|---|
| Gender | Male | 104 | 54.7 |
| Female | 86 | 45.3 | |
| Age | 20–29 | 33 | 17.4 |
| 30–39 | 40 | 21.1 | |
| 40–49 | 54 | 28.4 | |
| 50–59 | 53 | 27.9 | |
| Over 60 | 10 | 5.3 | |
| Education level | Middle school or below | 19 | 10.0 |
| High school | 109 | 57.4 | |
| University or over | 60 | 31.6 | |
| Other | 2 | 1.0 | |
| Diagnosis | Schizophrenia | 157 | 82.6 |
| Major depression | 15 | 7.9 | |
| Bipolar disorder | 13 | 6.8 | |
| Other | 5 | 2.6 | |
| Employment status | Vocational rehabilitation | 13 | 6.8 |
| Part time | 26 | 13.7 | |
| Full time | 12 | 6.3 | |
| No job | 139 | 73.2 | |
| City size | Large cities | 130 | 68.4 |
| Small cities | 60 | 31.6 |
| Variables | Mental Health Community Integration (1) | Non-Mental Health Community Integration | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Physical Integration (2) | Social Integration | Psychological Integration (5) | ||||||||||||||
| Social Network Size (3) | Social Contact Frequency (4) | |||||||||||||||
| β | t | p | β | t | p | β | t | p | β | t | p | β | t | p | ||
| Sociodemographic | ||||||||||||||||
| Gender | −0.030 | −0.512 | 0.609 | −0.101 | −1.656 | 0.099 | −0.032 | −0.470 | 0.639 | −0.055 | −0.768 | 0.443 | −0.095 | −1.446 | 0.150 | |
| Age | 0.054 | 0.884 | 0.378 | 0.020 | 0.324 | 0.746 | 0.029 | 0.413 | 0.680 | −0.025 | −0.332 | 0.740 | 0.084 | 1.245 | 0.215 | |
| Years of education | −0.034 | −0.558 | 0.577 | 0.072 | 1.158 | 0.248 | 0.212 | 3.036 | 0.003 | 0.135 | 1.840 | 0.067 | 0.068 | 1.019 | 0.310 | |
| City size | 0.047 | 0.798 | 0.426 | 0.188 | 3.088 | 0.002 | 0.006 | 0.089 | 0.929 | 0.037 | 0.513 | 0.609 | 0.092 | 1.410 | 0.160 | |
| Resource accessibility | 0.537 | 8.479 | <0.000 | 0.468 | 7.160 | <0.000 | 0.238 | 3.277 | 0.001 | 0.241 | 3.150 | 0.002 | 0.331 | 4.722 | <0.000 | |
| Clinical | ||||||||||||||||
| Diagnosis | −0.059 | −0.956 | 0.340 | 0.039 | 0.615 | 0.539 | 0.038 | 0.541 | 0.589 | 0.032 | 0.433 | 0.666 | 0.058 | 0.858 | 0.392 | |
| Symptoms | −0.191 | −3.154 | 0.002 | −0.136 | −2.181 | 0.031 | −0.232 | −3.332 | 0.001 | −0.084 | −1.145 | 0.254 | −0.264 | −3.934 | <0.000 | |
| Goodness-of-Fit Measure | Level of Acceptable Fit | Fit Statistics | |
|---|---|---|---|
| Absolute fit | /df | <3 good | 1.619 |
| GFI | >0.8 acceptable, >0.9 good | 0.858 | |
| AGFI | >0.8 acceptable, >0.9 good | 0.810 | |
| RMSEA | <0.08 good | 0.057 | |
| Incremental fit | NFI | >0.9 good | 0.894 |
| RFI | >0.9 good | 0.869 | |
| IFI | >0.9 good | 0.957 | |
| TLI | >0.9 good | 0.946 | |
| CFI | >0.9 good | 0.956 | |
| Goodness-of-Fit Measure | Level of Acceptable Fit | Fit Statistics | |
|---|---|---|---|
| Absolute fit | /df | <3 good | 1.703 |
| GFI | >0.8 acceptable, >0.9 good | 0.842 | |
| AGFI | >0.8 acceptable, >0.9 good | 0.803 | |
| RMSEA | <0.08 good | 0.061 | |
| Incremental fit | NFI | >0.9 good | 0.881 |
| RFI | >0.9 good | 0.863 | |
| IFI | >0.9 good | 0.947 | |
| TLI | >0.9 good | 0.938 | |
| CFI | >0.9 good | 0.947 | |
| B | β | S.E. | C.R. | p | |||
|---|---|---|---|---|---|---|---|
| PA | → | MHC | 0.460 | 0.410 | 0.102 | 4.517 | <0.001 |
| RP | → | MHC | −0.021 | −0.041 | 0.069 | −0.300 | 0.764 |
| RS | → | MHC | 0.004 | 0.009 | 0.050 | 0.071 | 0.943 |
| PI | → | MHC | 0.278 | 0.439 | 0.053 | 5.285 | <0.001 |
| MHC | → | PHI | 0.624 | 0.441 | 0.118 | 5.282 | <0.001 |
| MHC | → | SN | 0.508 | 0.045 | 0.884 | 0.575 | 0.566 |
| MHC | → | CF | 0.843 | 0.260 | 0.340 | 2.483 | 0.013 |
| MHC | → | PSI | 0.637 | 0.542 | 0.090 | 7.087 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seo, M.K.; Lee, M.H. Effects of Community-Based Programs on Integration into the Mental Health and Non-Mental Health Communities. Healthcare 2021, 9, 1181. https://doi.org/10.3390/healthcare9091181
Seo MK, Lee MH. Effects of Community-Based Programs on Integration into the Mental Health and Non-Mental Health Communities. Healthcare. 2021; 9(9):1181. https://doi.org/10.3390/healthcare9091181
Chicago/Turabian StyleSeo, Mi Kyung, and Min Hwa Lee. 2021. "Effects of Community-Based Programs on Integration into the Mental Health and Non-Mental Health Communities" Healthcare 9, no. 9: 1181. https://doi.org/10.3390/healthcare9091181
APA StyleSeo, M. K., & Lee, M. H. (2021). Effects of Community-Based Programs on Integration into the Mental Health and Non-Mental Health Communities. Healthcare, 9(9), 1181. https://doi.org/10.3390/healthcare9091181






