From Child to Adulthood, a Multidisciplinary Approach of Multiple Microdontia Associated with Hypodontia: Case Report Relating a 15 Year-Long Management and Follow-Up
Abstract
1. Introduction
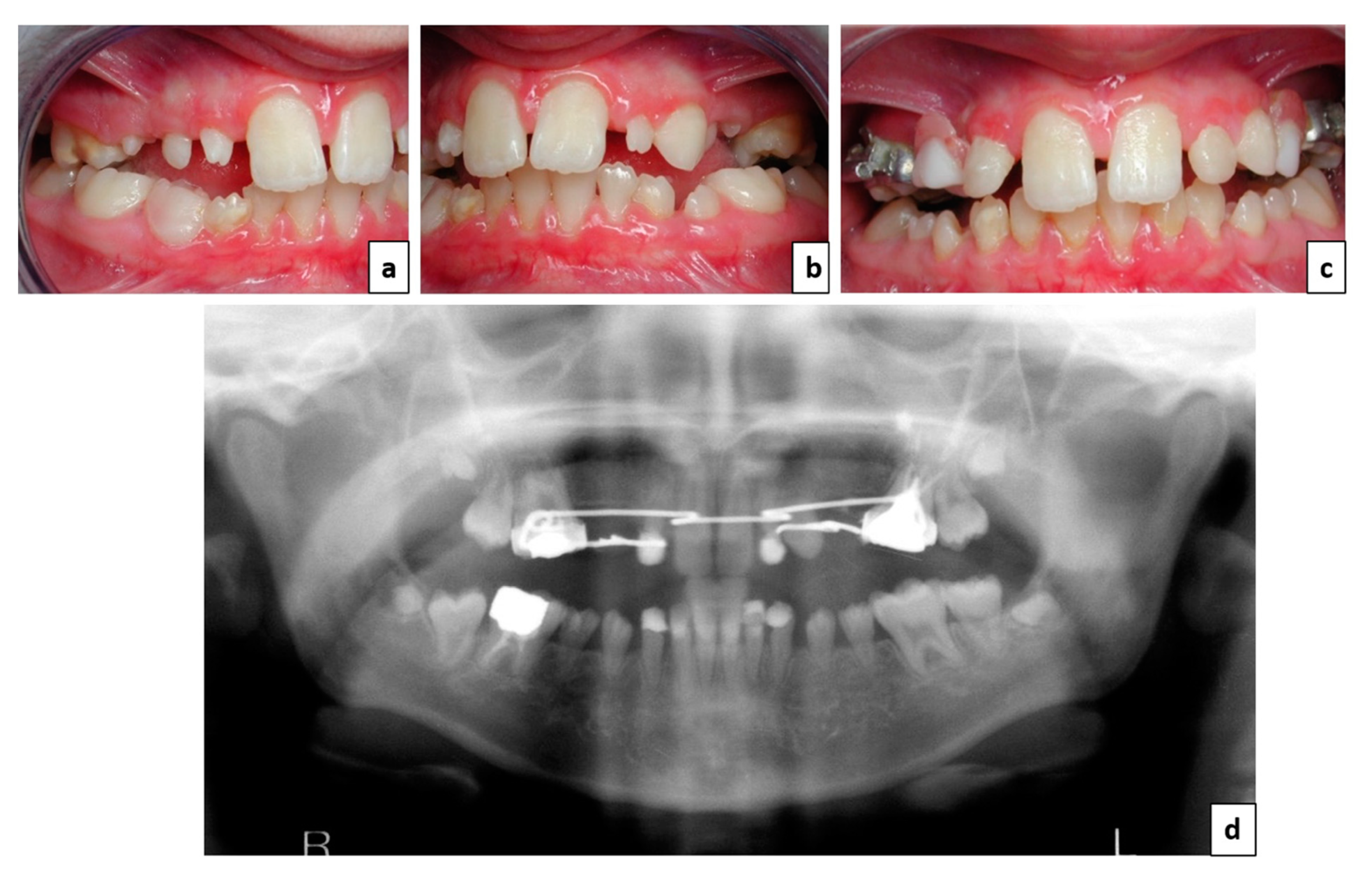
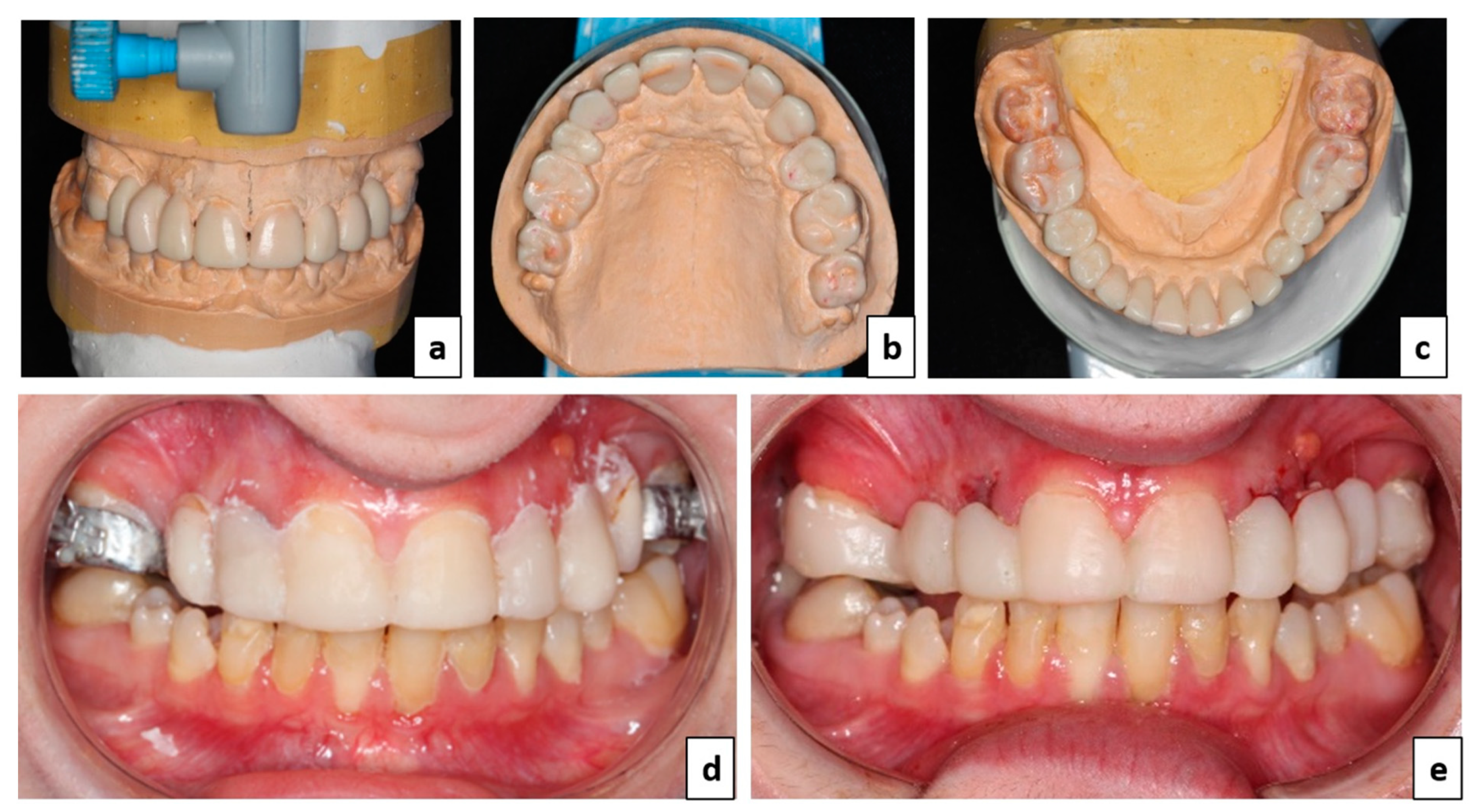
2. Case Report
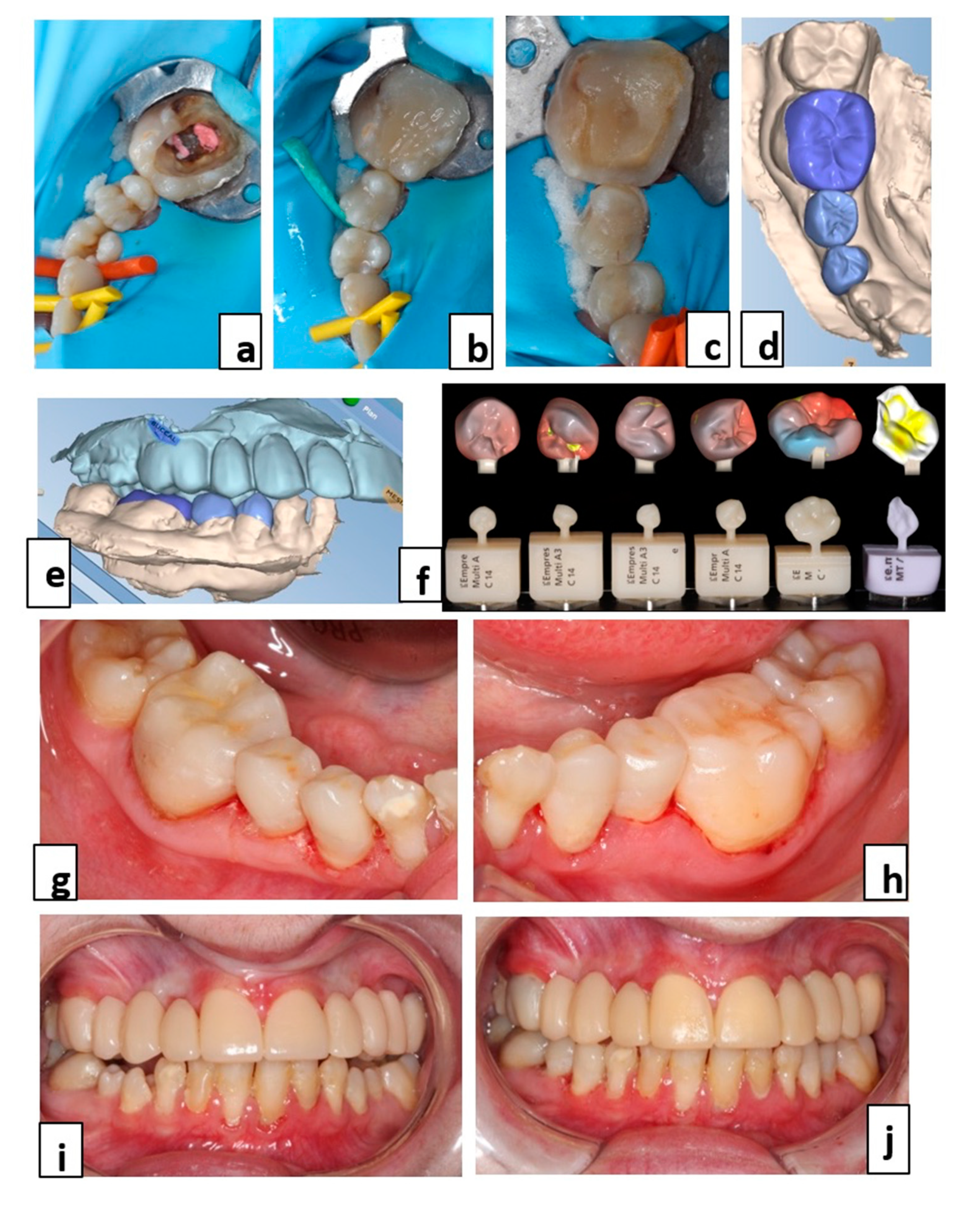
3. Treatment Plan
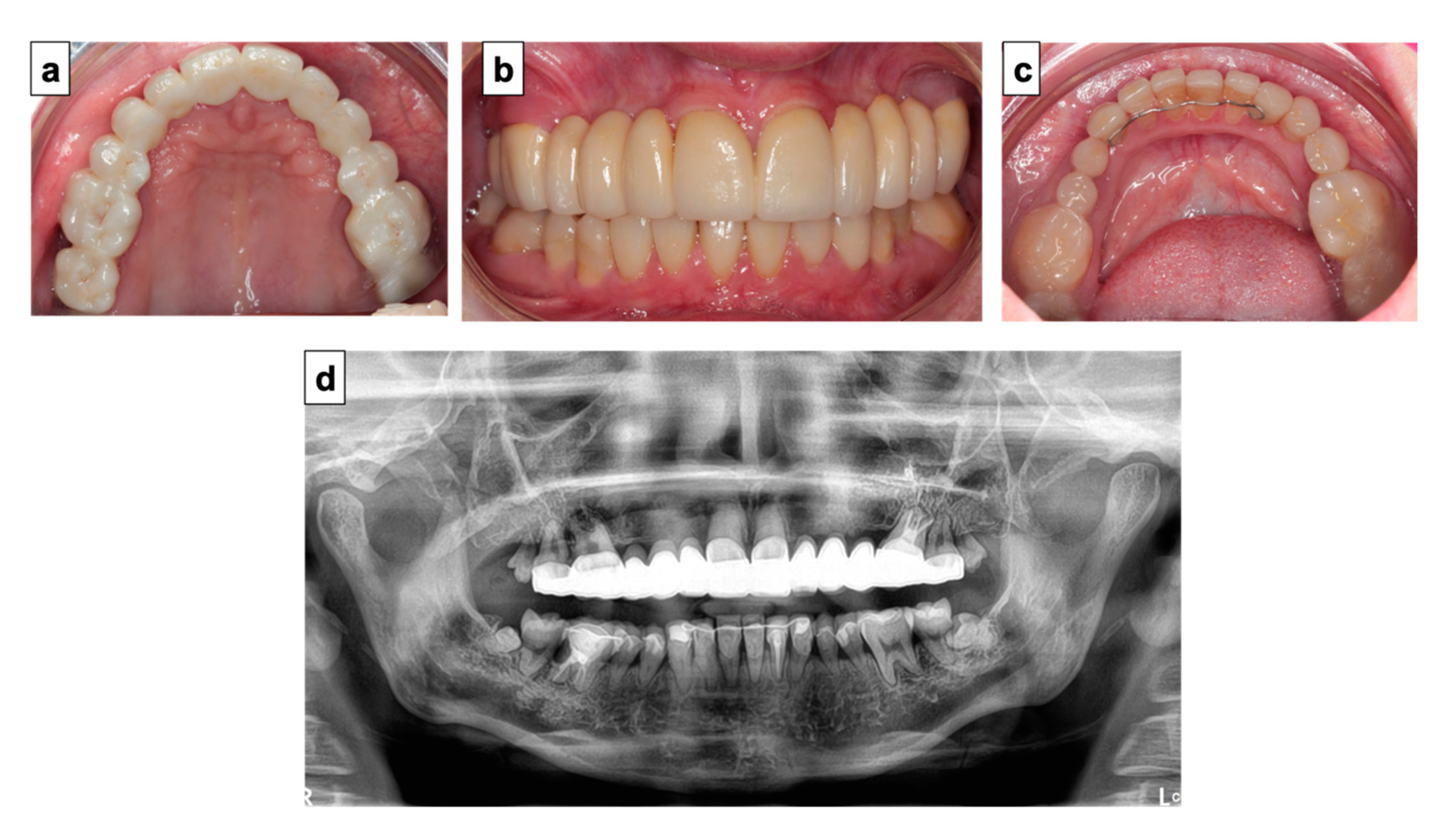
4. Therapeutic Management
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Chen, Y.; Zhou, F.; Peng, Y.; Chen, L.; Wang, Y. Non-syndromic occurrence of true generalized microdontia with hypodontia. Medicine 2019, 98, e16283. [Google Scholar] [CrossRef]
- Villa, A.; Albonico, A.; Villa, F. Hypodontia and microdontia: Clinical features of a rare syndrome. J. Can. Dent. Assoc. 2011, 77, b115. [Google Scholar]
- Bargale, S.D.; Kiran, S.D.P. Non-syndromic occurrence of true generalized microdontia with mandibular mesiodens—A rare case. Head Face Med. 2011, 7, 19. [Google Scholar] [CrossRef]
- Oguz, A.; Karadeniz, C.; Alpaslan, G.; Alpaslan, C.; Pinarli, F.G.; Çetiner, S. Long-term effects of chemotherapy on orodental structures in children with non-Hodgkin’s lymphoma. Eur. J. Oral Sci. 2004, 112, 8–11. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, S.; Bernardi, S.; Belli, M.; Varvara, G.; Macchiarelli, G. Exposure to persistent organic pollutants during tooth formation: Molecular mechanisms and clinical findings. Rev. Environ. Health 2020, 35, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Guo, H.; Zhang, L.; Wei, K.; Zhao, J.; Wang, Y.; Jin, F.; Xuan, K. Exposure to a continuous low dose of tetrachlorodibenzo-p-dioxin impairs the development of the tooth root in lactational rats and alters the function of apical papilla-derived stem cells. Arch. Oral Biol. 2015, 60, 199–207. [Google Scholar] [CrossRef]
- Hobkirk, J.A.; Goodman, J.R.; Jones, S.P. Presenting complaints and findings in a group of patients attending a hypodontia clinic. Br. Dent. J. 1994, 177, 337–339. [Google Scholar] [CrossRef] [PubMed]
- Al-Ani, A.H.; Antoun, J.S.; Thomson, W.M.; Merriman, T.R.; Farella, M. Hypodontia: An Update on Its Etiology, Classification, and Clinical Management. BioMed Res. Int. 2017, 2017, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Laing, E.; Cunningham, S.; Jones, S.; Moles, D.; Gill, D. Psychosocial impact of hypodontia in children. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Favot, L.-M.; Cuzin, J.-F.; Schouver, J.; Pongas, D.; Tisserand, A.; Penaud, J. Transitional prosthodontic treatment on implant: A new orthodontic proposal. Int. Orthod. 2010, 8, 399–408. [Google Scholar] [CrossRef]
- Yin, W.; Bian, Z. The Gene Network Underlying Hypodontia. J. Dent. Res. 2015, 94, 878–885. [Google Scholar] [CrossRef] [PubMed]
- Khalil, S.; Eid, E.; Hamieh, L.; Bardawil, T.; Moujaes, Z.; Khalil, W.; Abbas, O.; Kurban, M. Genodermatoses with teeth abnormalities. Oral Dis. 2020, 26, 1032–1044. [Google Scholar] [CrossRef] [PubMed]
- Thesleff, I. From understanding tooth development to bioengineering of teeth. Eur. J. Oral Sci. 2018, 126, 67–71. [Google Scholar] [CrossRef]
- Nunn, J.; Carter, N.E.; Gillgrass, T.J.; Hobson, R.S.; Jepson, N.J.; Meechan, J.G.; Nohl, F.S. The interdisciplinary management of hypodontia: Background and role of paediatric dentistry. Br. Dent. J. 2003, 194, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Gill, D.S.; Barker, C.S. The multidisciplinary management of hypodontia: A team approach. Br. Dent. J. 2015, 218, 143–149. [Google Scholar] [CrossRef]
- Hobson, R.S.; Carter, N.E.; Gillgrass, T.J.; Jepson, N.J.A.; Meechan, J.G.; Nohl, F.; Nunn, J. The interdisciplinary management of hypodontia: The relationship between an interdisciplinary team and the general dental practitioner. Br. Dent. J. 2003, 194, 479–482. [Google Scholar] [CrossRef]
- Alnuaimi, R.; Mansoor, M. Prosthetic rehabilitation with fixed prosthesis of a 5-year-old child with Hypohidrotic Ectodermal Dysplasia and Oligodontia: A case report. J. Med. Case Rep. 2019, 13, 1–6. [Google Scholar] [CrossRef]
- Hagege, F.J.; Dersot, J.-M. Les facteurs de risques en implantologie: Conséquences orthodontiques. Int. Orthod. 2007, 5, 407–424. [Google Scholar] [CrossRef]
- Durey, K.; Carter, L.; Chan, M. The management of severe hypodontia. Part 2: Bone augmentation and the provision of implant supported prostheses. Br. Dent. J. 2014, 216, 63–68. [Google Scholar] [CrossRef][Green Version]
- Bergendal, B. When should we extract deciduous teeth and place implants in young individuals with tooth agenesis? J. Oral Rehabil. 2008, 35, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Jepson, N.J.; Nohl, F.S.; Carter, N.E.; Gillgrass, T.J.; Meechan, J.G.; Hobson, R.S.; Nunn, J. The interdisciplinary management of hypodontia: Restorative dentistry. Br. Dent. J. 2003, 194, 299–304. [Google Scholar] [CrossRef] [PubMed]
- Filius, M.A.; Cune, M.S.; Raghoebar, G.M.; Vissink, A.; Visser, A. Prosthetic treatment outcome in patients with severe hypodontia: A systematic review. J. Oral Rehabil. 2016, 43, 373–387. [Google Scholar] [CrossRef]
- Apelian, N.; Vergnes, J.N.; Hovey, R.; Bedos, C. How can we provide person-centred dental care? Br. Dent. J. 2017, 223, 419–424. [Google Scholar] [CrossRef]
- Durey, K.; Cook, P.; Chan, M. The management of severe hypodontia. Part 1: Considerations and conventional restorative options. Br. Dent. J. 2014, 216, 25–29. [Google Scholar] [CrossRef]
- Locker, D.; Jokovic, A.; Prakash, P.; Tompson, B. Oral health-related quality of life of children with oligodontia. Int. J. Paediatr. Dent. 2010, 20, 8–14. [Google Scholar] [CrossRef]
- Tavajohi-Kermani, H.; Kapur, R.; Sciote, J.J. Tooth agenesis and craniofacial morphology in an orthodontic population. Am. J. Orthod. Dentofac. Orthop. 2002, 122, 39–47. [Google Scholar] [CrossRef]
- Kotsiomiti, E.; Arapostathis, K.; Kapari, D.; Konstantinidis, A. Removable prosthodontic treatment for the primary and mixed dentition. J. Clin. Pediatr. Dent. 2000, 24, 83–89. [Google Scholar]
- Worsaae, N.; Jensen, B.; Holm, B.; Holsko, J. Treatment of severe hypodontia–oligodontia—An interdisciplinary concept. Int. J. Oral Maxillofac. Surg. 2007, 36, 473–480. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, M.; O’Connell, B.C. Multidiscipunary Management of Hypodontia. Prim. Dent. J. 2017, 6, 62–73. [Google Scholar] [CrossRef]
- Hartlev, J.; Sandberg, M.; Jensen, A.-S.; Gjørup, H.; Nørholt, S. Multidisciplinary Treatment Intervention in 24 Patients with Oligodontia: A Case-Cohort Study. Int. J. Prosthodont. 2018, 32, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Bohner, L.O.L.; Hanisch, M.; Kleinheinz, J.; Jung, S. Dental implants in growing patients: A systematic review. Br. J. Oral Maxillofac. Surg. 2019, 57, 397–406. [Google Scholar] [CrossRef]
- Hvaring, C.L.; Øgaard, B.; Birkeland, K. Tooth replacements in young adults with severe hypodontia: Orthodontic space closure, dental implants, and tooth-supported fixed dental prostheses. A follow-up study. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 620–626. [Google Scholar] [CrossRef] [PubMed]
- Laverty, D.P.; Fairbrother, K.; Addison, O. The Current Evidence on Retaining or Prosthodontically Replacing Retained Deciduous Teeth in the Adult Hypodontia Patient: A Systematic Review. Eur. J. Prosthodont. Restor. Dent. 2018, 26, 2–15. [Google Scholar] [PubMed]
- Créton, M.; Cune, M.; Verhoeven, W.; Muradin, M.; Wismeijer, D.; Meijer, G. Implant Treatment in Patients With Severe Hypodontia: A Retrospective Evaluation. J. Oral Maxillofac. Surg. 2010, 68, 530–538. [Google Scholar] [CrossRef] [PubMed]
- Terheyden, H.; Wüsthoff, F. Occlusal rehabilitation in patients with congenitally missing teeth—Dental implants, conventional prosthetics, tooth autotransplants, and preservation of deciduous teeth—A systematic review. Int. J. Implant. Dent. 2015, 1, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Allen, P.F.; Lee, S.; Brady, P. Clinical and subjective evaluation of implants in patients with hypodontia: A two-year observation study. Clin. Oral Implant. Res. 2016, 28, 1258–1262. [Google Scholar] [CrossRef]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thomas, C.; Vaysse, F.; Courset, T.; Nasr, K.; Courtois, B.; L’Homme, A.; Chassaing, N.; Vinel, A.; Bailleul-Forestier, I.; Raynaldy, L.; et al. From Child to Adulthood, a Multidisciplinary Approach of Multiple Microdontia Associated with Hypodontia: Case Report Relating a 15 Year-Long Management and Follow-Up. Healthcare 2021, 9, 1180. https://doi.org/10.3390/healthcare9091180
Thomas C, Vaysse F, Courset T, Nasr K, Courtois B, L’Homme A, Chassaing N, Vinel A, Bailleul-Forestier I, Raynaldy L, et al. From Child to Adulthood, a Multidisciplinary Approach of Multiple Microdontia Associated with Hypodontia: Case Report Relating a 15 Year-Long Management and Follow-Up. Healthcare. 2021; 9(9):1180. https://doi.org/10.3390/healthcare9091180
Chicago/Turabian StyleThomas, Charlotte, Frédéric Vaysse, Teva Courset, Karim Nasr, Bruno Courtois, Arnaud L’Homme, Nicolas Chassaing, Alexia Vinel, Isabelle Bailleul-Forestier, Luc Raynaldy, and et al. 2021. "From Child to Adulthood, a Multidisciplinary Approach of Multiple Microdontia Associated with Hypodontia: Case Report Relating a 15 Year-Long Management and Follow-Up" Healthcare 9, no. 9: 1180. https://doi.org/10.3390/healthcare9091180
APA StyleThomas, C., Vaysse, F., Courset, T., Nasr, K., Courtois, B., L’Homme, A., Chassaing, N., Vinel, A., Bailleul-Forestier, I., Raynaldy, L., & Laurencin-Dalicieux, S. (2021). From Child to Adulthood, a Multidisciplinary Approach of Multiple Microdontia Associated with Hypodontia: Case Report Relating a 15 Year-Long Management and Follow-Up. Healthcare, 9(9), 1180. https://doi.org/10.3390/healthcare9091180





