Impact of Using the Intelligent Physical Health Measurement System on Active Aging: A Survey in Taiwan
Abstract
:1. Introduction
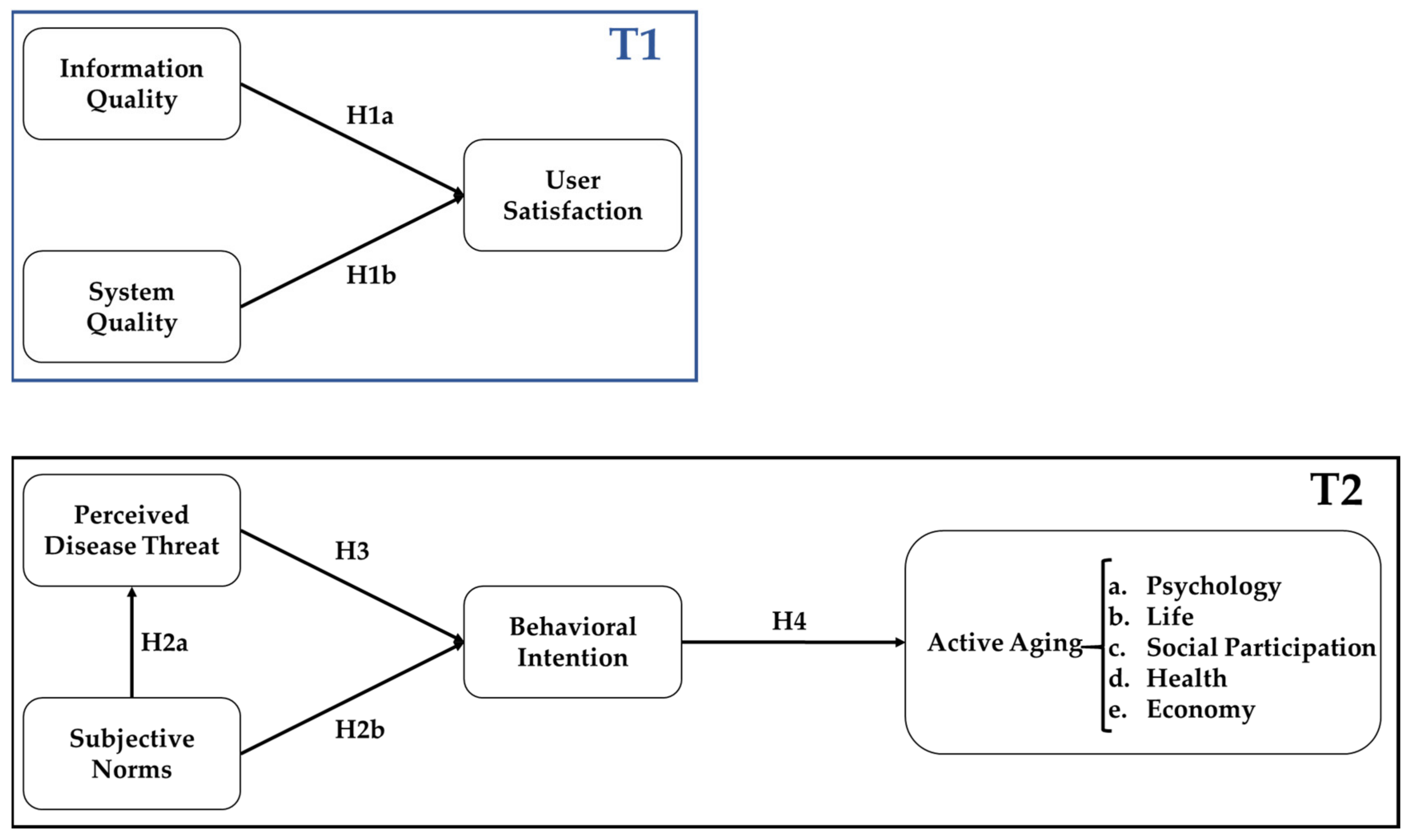
2. Theoretical Framework and Hypothesis Development
2.1. Information System Success Model (ISSM)
2.2. Health Belief Model (HBM) and Theory of Planned Behavior (TPB)
2.3. Active Aging
3. Research Methodology
3.1. Introduction of Case Studies
3.2. Subjects
3.3. Questionnaire Design
3.4. Data Collection and Analysis
4. Results
4.1. Descriptive Statistical
4.2. Reliability and Validity Analysis
- 1.
- The diagonal line in bold is the square root of the average variance extracted (AVE) value of the facet [34].
- 2.
- The value under the diagonal is the correlation coefficient of the factor facet.
- 3.
- The comparison of each aspect and the code abbreviation is as follows: IQ: information products; SQ: system quality; US: user satisfaction; BI: behavioral intention; PDT: perceived disease threat; SN: subjective norms; AA-Phy: active aging psychology; AA-life: active aging life; AA-social: active aging-social participation; AA-Health: active aging health; AA-econ: active aging economy.
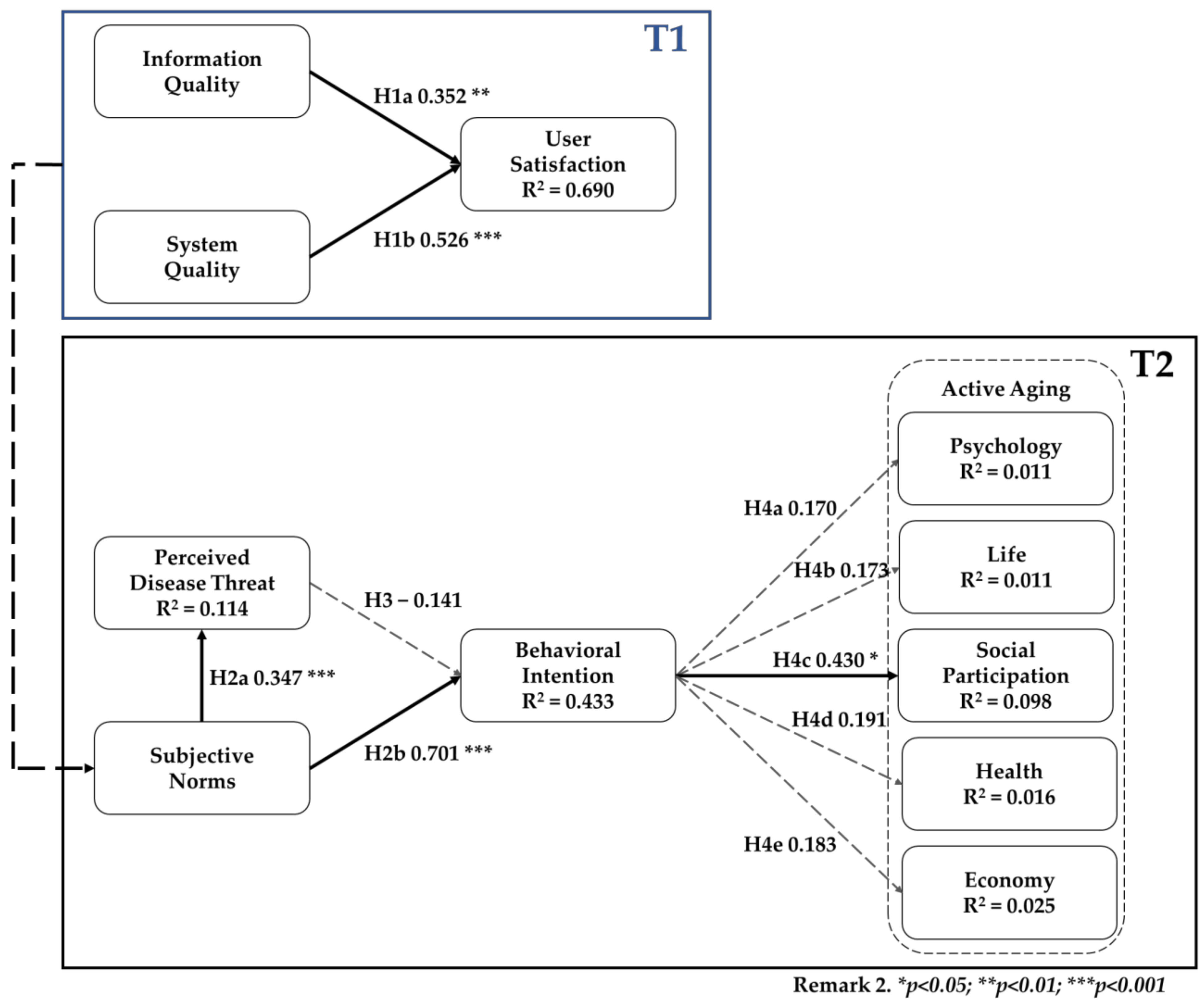
4.3. Structural Model Analysis
| Hypothesis | Path Coefficient | T-Value | p-Value | R Square | |
|---|---|---|---|---|---|
| H1a | IQ → US | 0.352 | 2.868 | 0.004 ** | 0.690 |
| H1b | SQ → US | 0.526 | 3.941 | 0.000 *** | |
| H2a | SN → PDT | 0.347 | 4.459 | 0.000 *** | 0.114 |
| H2b | SN → BI | 0.701 | 6.112 | 0.000 *** | 0.433 |
| H3 | PDT → BI | −0.141 | 1.247 | 0.212 | |
| H4a | BI → AA-Phy | 0.170 | 0.966 | 0.334 | 0.011 |
| H4b | BI → AA-Life | 0.173 | 0.963 | 0.335 | 0.011 |
| H4c | BI → AA-Social | 0.430 | 2.099 | 0.036 * | 0.098 |
| H4d | BI → AA-Health | 0.191 | 1.012 | 0.312 | 0.016 |
| H4e | BI → AA-Econ | 0.183 | 0.992 | 0.321 | 0.025 |
- 1.
- * p < 0.05; ** p < 0.01; *** p < 0.001
- 2.
- The comparison of each aspect and the code of abbreviations are as follows: user satisfaction (US); behavioral intention (BI); perceived disease threat (PDT); active aging psychology (AA-Phy); active aging life (AA-Life); active aging social participation (AA-Social); active aging health (AA-Health); active aging economy (AA-Econ).
4.4. Informal Follow-Up Interview for Subjects
5. Discussion and Conclusions
5.1. Discussion
5.2. Conclusions
6. Limitation and Direction of Future Studies
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| System Quality [11,35] |
| I think this system is very stable. |
| I think this system is easy to use. |
| I think the operation of this system is easy to learn. |
| I think this system responds very quickly. |
| Information Quality [11,36] |
| This system can provide correct information without repeating operations. |
| The system information can be clearly displayed on the screen, making it easy for users to read. |
| The user interface of this system is well designed. |
| User Satisfaction [11,35] |
| You have a positive attitude or comment on this system function. |
| The function of this system meets my work requirements. |
| You are satisfied with this system. |
| Perceived Disease Threat [37,38] | |
| I think I get sick easily. | |
| I think I may suffer from chronic diseases in the future. | |
| I feel that my health is worse than before. | |
| I may be forced to change my life due to chronic diseases in the future. | |
| Subjective Norms [39,40] | |
| People who influence my behavior would think that I should use the Baby machine. | |
| People who are important to me would think that I should use the Baby machine. | |
| Behavior Intention [41,42] | |
| I will use Baby machine on a regular basis in the future. | |
| I will frequently use Baby machine in the future. | |
| I will continue use Baby machine in the future. | |
| Active Aging [41,43,44] | |
| Psychological | Having satisfied one’s life goals. |
| I like myself very much. | |
| Having positive attitude. | |
| I can appreciate the meaning of life. | |
| Acceptance of own mortality. | |
| Life | Having pleasurable daily activities. |
| I feel dependent on life. | |
| Being socially active. | |
| Health | Pay attention to nutrition and health preservation. |
| Having good health. | |
| Being able to take care of personal needs. | |
| Remaining in control of one’s life. | |
| Economic | Having money to enjoy extras. |
| Being financially secure. | |
| Can afford emergency medical expenses. | |
| Social Participation | Interacting with others regularly. |
| Being able to do things for others. | |
| Participating in various community activities makes my life more colorful. | |
| Having good friends. | |
References
- Ministry of Health and Welfare. Long-Term Care Ten-Year Plan 2.0 Report. 2016. Available online: https://www.ttshb.gov.tw/ezfiles/0/1000/attach/67/pta_902_8072286_64551.pdf (accessed on 4 January 2021).
- Ministry of Health and Welfare. Long Care 2.0. 2021. Available online: https://www.mohw.gov.tw/dl-41398-de03f2b4-64b0-4d1a-9b01-18bf2f7cadb8.html (accessed on 5 January 2021).
- Yang, C.C.; Hsueh, J.Y.; Wei, C.Y. Current status of long-term care in Taiwan: Transition of long-term care plan from 1.0 to 2.0. Int. J. Health Policy Manag. 2020, 9, 363. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health and Welfare. Long-Term Care Ten-Year Plan 2.0—Construction of the Concept of ABC for the Overall Community Care Model. 2016. Available online: http://www.mohw.gov.tw/cht/LTC/DM1_P.aspx?f_list_no=976&fod_list_no=0&doc_no=56367 (accessed on 5 January 2021).
- Hsu, H.C.; Chen, C.F. LTC 2.0: The 2017 reform of home-and community-based long-term care in Taiwan. Health Policy 2019, 123, 912–916. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare. Long-Term Care Ten-Year Plan 2.0—Establish an Overall Care Model for Our Community and Build a Dense Care Network. 2020. Available online: https://1966.gov.tw/LTC/cp-3636-42415-201.html (accessed on 4 January 2021).
- Industrial Development Bureau, Ministry of Economic Affairs. Local Innovation Project of Smart City and Rural Application Development Project. 2018. Available online: https://www.twsmartcity.org.tw/news/46https://www.twsmartcity.org.tw/subsidy_list/18 (accessed on 3 December 2020).
- DeLone, W.H.; McLean, A. The DeLone and McLean model of information systems success: A ten-year update. J. Manag. Inf. Syst. 2003, 19, 9–30. [Google Scholar]
- Barteit, S.; Neuhann, F.; Bärnighausen, T.; Bowa, A.; Wolter, S.; Siabwanta, H.; Jahn, A. Technology Acceptance and Information System Success of a Mobile Electronic Platform for Nonphysician Clinical Students in Zambia: Prospective, Nonrandomized Intervention Study. J. Med Internet Res. 2019, 21, e14748. [Google Scholar] [CrossRef] [PubMed]
- Wixom, B.H.; Todd, P.A. A theoretical integration of user satisfaction and technology acceptance. Inf. Syst. Res. 2005, 16, 85–102. [Google Scholar] [CrossRef]
- DeLone, W.H.; McLean, E.R. Information systems success: The quest for the dependent variable. Inf. Syst. Res. 1992, 3, 60–95. [Google Scholar] [CrossRef] [Green Version]
- Hsieh, H.L.; Tsai, C.H.; Chih, W.H.; Lin, H.H. Factors affecting success of an integrated community-based telehealth system. Technol. Health Care 2015, 23, S189–S196. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurt, Ö.E. Examining an e-learning system through the lens of the information systems success model: Empirical evidence from Italy. Educ. Inf. Technol. 2019, 24, 1173–1184. [Google Scholar] [CrossRef]
- Yeh, K.J.; Wang TLee, C.H. Healthcare Information Technology Service Quality: From A Medical Staff Perspective. J. Inf. Manag. 2014, 21, 139–160. [Google Scholar]
- Lian, J.W. Establishing a cloud computing success model for hospitals in Taiwan. INQUIRY J. Health Care Organ. Provis. Financ. 2017, 54, 0046958016685836. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sussman, R.; Gifford, R. Causality in the theory of planned behavior. Personal. Soc. Psychol. Bull. 2019, 45, 920–933. [Google Scholar] [CrossRef] [Green Version]
- Santi Lozoya, C.J.; Giblin-Scanlon, L.; Boyd, L.D.; Nolen, S.; Vineyard, J. Influence of a Smartphone Application on the Oral Health Practices and Behaviors of Parents of Preschool Children. J. Dent. Hyg. 2019, 93, 31628171. [Google Scholar]
- Wang, X.; Chen, D.; Xie, T.; Zhang, W. Predicting women’s intentions to screen for breast cancer based on the health belief model and the theory of planned behavior. J. Obstet. Gynaecol. Res. 2019, 45, 2440–2451. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Lee, H.; Zo, H. User acceptance of smart home services: An extension of the theory of planned behavior. Ind. Manag. Data Syst. 2017, 117, 68–89. [Google Scholar] [CrossRef]
- Zhao, Y.; Ni, Q.; Zhou, R. What factors influence the mobile health service adoption? A meta-analysis and the moderating role of age. Int. J. Inf. Manag. 2018, 43, 342–343. [Google Scholar] [CrossRef]
- Marsillas, S.; de Donder, L.; Kardol, T.; van Regenmortel, S.; Dury, S.; Brosens, D.; Smetcoren, A.S.; Brana, T.; Varela, J. Does active ageing contribute to life satisfaction for older people? Testing a new model of active ageing. Eur. J. Ageing 2017, 14, 295–310. [Google Scholar] [CrossRef]
- World Health Organization. Active Ageing: A Policy Framework. 2002. Available online: https://apps.who.int/iris/handle/10665/67215 (accessed on 9 December 2020).
- Wu, S.T.; Chen, C.Y. Relationships between Social Support, Social Participation, and Active Aging for and in Aged People. J. Gerontechnology Serv. Manag. 2017, 5, 331–352. [Google Scholar]
- Petretto, D.R.; Pili, L.; Gaviano, L.; Pili, R. On the semantic of ageing: From successful ageing to dynamic and developmental model of ageing. 2017. Available online: https://iris.unica.it/handle/11584/219679#.YSYcAt8RXIw (accessed on 11 January 2021).
- Chuang, T.Y.; Chen, J.L. A Study of the Relations among Family Support, Self-Value and Active Aging for the Elders. Fu Jen J. Hum. Ecol. 2017, 23, 65–82. [Google Scholar]
- Bousquet, J.; Barbara, C.; Bateman, E.; Bel, E.; Bewick, M.; Chavannes, N.H.; Cruz, A.A.; Haahtela, T.; Hellings, P.W.; Khaltaev, N.; et al. AIRWAYS-ICPs (European Innovation Partnership on Active and Healthy Ageing) from concept to implementation. Eur. Respir. J. 2016, 47, 1028–1033. [Google Scholar] [CrossRef] [Green Version]
- Zaidi, A.; Howse, K. The policy discourse of active ageing: Some reflections. J. Popul. Ageing 2017, 10, 1–10. [Google Scholar] [CrossRef]
- Zaidi, A.; Gasior, K.; Hofmarcher, M.M.; Lelkes, O.; Marin, B.; Rodrigues, R.; Schmidt, A.; Vanhuysse, P.; Zolyomi, E. Active Ageing Index 2012 Concept, Methodology and Final Results; Citeseer: University Park, PA, USA, 2013. [Google Scholar]
- Gjevjon, E.R.; Øderud, T.; Wensaas, G.H.; Moen, A. Toward a typology of technology users: How older people experience technology’s potential for active aging. In Nursing Informatics; IOS Press: Amsterdam, The Netherlands, 2014; pp. 25–31. [Google Scholar]
- Chen, Y.L.; Tang, H.F. Developing a Leisure and Health Mobile App for the Active Aging; Departmant of Leisure Industry and Health Promotion: Yilan City, Taiwan, 2015; pp. 83–101. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows; Version 22.0.; IBM Corp: Armonk, NY, USA, 2013. [Google Scholar]
- Ringle, C.M.; Wende, S.; Becker, J.-M. SmartPLS 3. Bönningstedt: SmartPLS. 2015. Available online: http://www.smartpls.com (accessed on 20 January 2021).
- Hair, J.F., Jr.; Hult, G.T.; Ringle, C.M.; Sarstedt, M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM); Sage Publications: Thousand Oaks, CA, USA, 2016. [Google Scholar]
- Fornell, C.; Larcker, D.F. Structural equation models with unobservable variables and measurement error: Algebra and statistics. J. Mark. Res. 1981, 18, 382–388. [Google Scholar] [CrossRef]
- Parker, M.A.; Martin, F. Synchronous virtual classrooms: Student perceptions from an online and blended education course. In Proceedings of the 2010 International Conference on Technology for Education, Mumbai, India, 1–3 July 2010; pp. 93–100. [Google Scholar]
- Rai, V.N.; Rai, A.K.; Yueh, F.Y.; Singh, J.P. Optical emission from laser-induced breakdown plasma of solid and liquid samples in the presence of a magnetic field. Appl. Opt. 2003, 42, 2085–2093. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, I.M. Why people use health services. Milbank Q. 2005, 83. [Google Scholar] [CrossRef]
- Lin, S.P.; Chen, S.X.; Yang, H.Y. Exploring Factors of Influencing People’s to Use Institutional Respite Service: Application of Health Belief Model. J. Account. Financ. Dev. 2016, 9, 127–142. [Google Scholar] [CrossRef]
- Taylor, S.; Todd, P.A. Understanding information technology usage: A test of competing models. Inf. Syst. Res. 1995, 6, 144–176. [Google Scholar] [CrossRef]
- Bhattarcherjee, A.; Premkumar, G. Understanding changes in belief and attitude toward information technology usage: A theoretical model and longitudinal test. Manag. Inf. Syst. Q. 2004, 28, 229–254. [Google Scholar] [CrossRef] [Green Version]
- Mathieson, K. Predicting user intentions: Comparing the technology acceptance model with the theory of planned behavior. Inf. Syst. Res. 1991, 2, 173–191. [Google Scholar] [CrossRef]
- Roca, J.C.; Chiu, C.M.; Martínez, F.J. Understanding e-learning continuance intention: An extension of the Technology Acceptance Model. Int. J. Hum.–Comput. Stud. 2006, 64, 683–696. [Google Scholar] [CrossRef] [Green Version]
- Rowe, J.W.; Kahn, R.L. Successful aging. Gerontologist 1997, 37, 433–440. [Google Scholar] [CrossRef]
- Zhan, M.-J. A Study on the Relationship between Middle-Aged Learners’ Leisure Attitudes and Active Ageing. Master’s Thesis, National Chi Nan University Department of Institute of Lifelong Learning and Human Resource Development of Dissertation, Puli, Nantou County, Taiwan, 2009; pp. 1–151. [Google Scholar] [CrossRef]

| Long-Term Care Unit | Setting | Service |
|---|---|---|
| A-level |
|
|
| B-level |
|
|
| C-level |
|
|
| Volunteers (N = 55) | Participants of Measurement Service (N = 125) | |||
|---|---|---|---|---|
| n | % | n | % | |
| Age | ||||
| Under 30 years old (inclusive) | 1 | 1.8% | 0 | 0.0% |
| 31–40 years old | 5 | 9.1% | 1 | 0.8% |
| 41–50 years old | 8 | 14.5% | 1 | 0.8% |
| 51–60 years old | 9 | 16.4% | 16 | 12.8% |
| Over 61 years old | 32 | 58.2% | 107 | 85.6% |
| Gender | ||||
| Male | 16 | 29.1% | 37 | 29.6% |
| Female | 39 | 70.9% | 88 | 70.4% |
| Education level | ||||
| Below middle school | 6 | 10.9% | 78 | 62.4% |
| High school | 7 | 12.7% | 31 | 24.8% |
| Specialist | 22 | 40.0% | 11 | 8.8% |
| the University | 13 | 23.6% | 3 | 2.4% |
| master’s degree | 5 | 9.1% | 1 | 0.8% |
| PhD | 2 | 3.6% | 1 | 0.8% |
| Community service (participation) years | ||||
| Less than 1 year | 6 | 10.9% | 17 | 13.6% |
| Less than 1–3 years | 13 | 23.6% | 49 | 39.2% |
| Less than 3–6 years | 23 | 41.8% | 26 | 20.8% |
| Under 6–9 years | 2 | 3.6% | 8 | 6.4% |
| >9 years | 11 | 20.0% | 25 | 20.0% |
| Average number of days in the community a week | ||||
| 1 day a week | 8 | 6.4% | ||
| 2 days a week | 27 | 21.6% | ||
| 3 days a week | 11 | 8.8% | ||
| 4 days a week | 17 | 13.6% | ||
| More than 5 days a week | 62 | 49.6% | ||
| Use body measurement equipment frequency | ||||
| Daily use | 18 | 14.4% | ||
| Use 3 times a week | 16 | 12.8% | ||
| Use once a week | 81 | 64.8% | ||
| Use once a week | 10 | 8.0% | ||
| Measured service experience | ||||
| Less than 6 months | 4 | 7.3% | ||
| 6 months–1 year | 27 | 49.1% | ||
| 1–3 years | 20 | 36.4% | ||
| 3–5 years | 3 | 5.5% | ||
| 5 years | 1 | 1.8% | ||
| Research Participants | Dimensions | Items | Factor Loading | Cronbach’s α | Composite Reliability (CR) | Average Variance Extracted (AVE) | ||
|---|---|---|---|---|---|---|---|---|
| Volunteers | Information Quality | IQ1 | 0.879 | 0.840 | 0.904 | 0.758 | ||
| IQ2 | 0.888 | |||||||
| IQ3 | 0.843 | |||||||
| System Quality | SQ1 | 0.818 | 0.850 | 0.899 | 0.689 | |||
| SQ2 | 0.897 | |||||||
| SQ3 | 0.812 | |||||||
| SQ4 | 0.810 | |||||||
| Use Satisfaction | US1 | 0.867 | 0.841 | 0.904 | 0.759 | |||
| US2 | 0.848 | |||||||
| US3 | 0.898 | |||||||
| Participants of measurement service | Perceived Disease Threat | PDT1 | 0.854 | 0.891 | 0.924 | 0.753 | ||
| PDT2 | 0.879 | |||||||
| PDT3 | 0.875 | |||||||
| PDT4 | 0.864 | |||||||
| Subjective Norms | SN1 | 0.796 | 0.634 | 0.841 | 0.727 | |||
| SN2 | 0.905 | |||||||
| Behavioral Intention | BI1 | 0.935 | 0.947 | 0.966 | 0.904 | |||
| BI2 | 0.967 | |||||||
| BI3 | 0.950 | |||||||
| Active Aging | Psychology | AA1 | 0.947 | 0.932 | 0.949 | 0.825 | ||
| AA2 | 0929 | |||||||
| AA3 | 0.857 | |||||||
| AA4 | 0.897 | |||||||
| Life | AA6 | 0.909 | 0.878 | 0.922 | 0.798 | |||
| AA7 | 0927 | |||||||
| AA8 | 0.841 | |||||||
| Social Participation | AA16 | 0.921 | 0.932 | 0.949 | 0.825 | |||
| AA17 | 0.825 | |||||||
| AA18 | 0.930 | |||||||
| AA19 | 0.793 | |||||||
| Health | AA9 | 0.859 | 0.878 | 0.915 | 0.728 | |||
| AA10 | 0.855 | |||||||
| AA11 | 0.866 | |||||||
| AA12 | 0.834 | |||||||
| Economy | AA13 | 0.881 | 0.790 | 0.875 | 0.701 | |||
| AA14 | 0.899 | |||||||
| AA15 | 0.720 | |||||||
| Volunteers | ||||||||
| Dimensions | IQ | SQ | US | |||||
| IQ | 0.870 | |||||||
| SQ | 0.812 | 0.830 | ||||||
| US | 0.779 | 0.812 | 0.871 | |||||
| Participants of Measurement Service | ||||||||
| Dimensions | AA Econ | AA Health | AA Phy | AA Social | AA life | BI | PDT | SN |
| AA_Econ | 0.837 | |||||||
| AA_Health | 0.765 | 0.853 | ||||||
| AA_Phy | 0.767 | 0.814 | 0.908 | |||||
| AA_Social | 0.684 | 0.803 | 0.728 | 0.869 | ||||
| AA_life | 0.710 | 0.807 | 0.777 | 0.785 | 0.893 | |||
| BI | 0.011 | 0.042 | 0.032 | 0.196 | 0.036 | 0.951 | ||
| PDT | −0.260 | −0.295 | −0.292 | −0.232 | −0.310 | 0.103 | 0.868 | |
| SN | −0.146 | −0.104 | −0.100 | −0.078 | −0.097 | 0.652 | 0.347 | 0.853 |
| Encoding | Interview Code | Age | Education Level | Profession |
|---|---|---|---|---|
| Volunteer | A | 42 | University | Director General |
| B | 61 | University | Volunteer | |
| C | 67 | University | Chairman |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chi, W.-C.; Cheng, W.-C.; Chen, T.-H.; Lin, P.-J. Impact of Using the Intelligent Physical Health Measurement System on Active Aging: A Survey in Taiwan. Healthcare 2021, 9, 1142. https://doi.org/10.3390/healthcare9091142
Chi W-C, Cheng W-C, Chen T-H, Lin P-J. Impact of Using the Intelligent Physical Health Measurement System on Active Aging: A Survey in Taiwan. Healthcare. 2021; 9(9):1142. https://doi.org/10.3390/healthcare9091142
Chicago/Turabian StyleChi, Wen-Chou, Wei-Chen Cheng, Ting-Hung Chen, and Po-Jin Lin. 2021. "Impact of Using the Intelligent Physical Health Measurement System on Active Aging: A Survey in Taiwan" Healthcare 9, no. 9: 1142. https://doi.org/10.3390/healthcare9091142
APA StyleChi, W.-C., Cheng, W.-C., Chen, T.-H., & Lin, P.-J. (2021). Impact of Using the Intelligent Physical Health Measurement System on Active Aging: A Survey in Taiwan. Healthcare, 9(9), 1142. https://doi.org/10.3390/healthcare9091142






