The Socio-Demographic Characteristics Associated with Non-Communicable Diseases among the Adult Population of Dubai: Results from Dubai Household Survey 2019
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source, Study Design
2.2. Variables and Measures
2.3. Statistical Analysis
3. Results
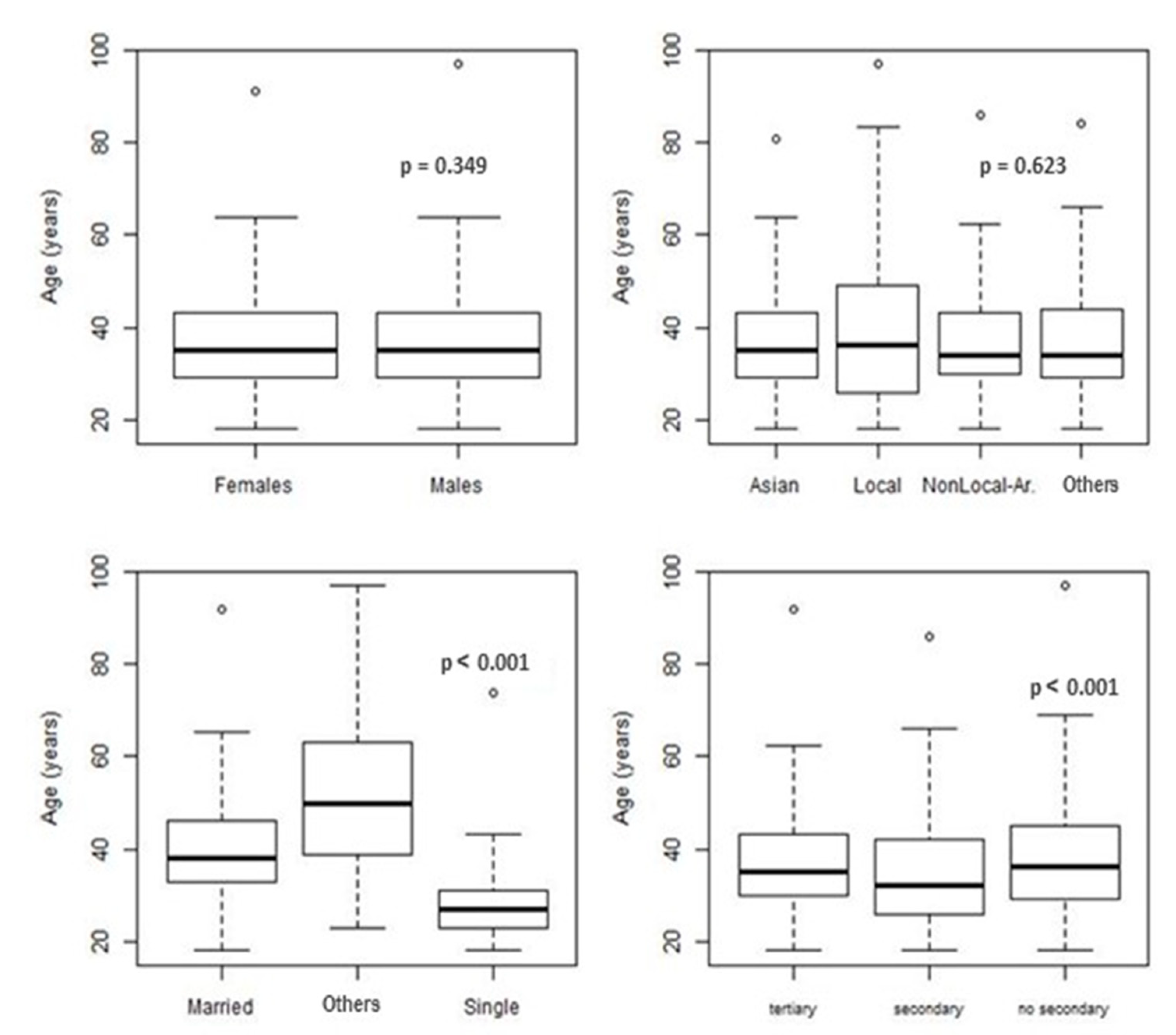
3.1. Sociodemographic Characteristics of the Population of Dubai
3.2. Associations with Non-Communicable Diseases
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- World Health Organization. Noncommunicable Diseases Country Profiles 2018. World Health Organization. 2018. Available online: https://apps.who.int/iris/handle/10665/274512 (accessed on 9 January 2021).
- Hajat, C.; Stein, E. The global burden of multiple chronic conditions: A narrative review. Prev. Med. Rep. 2018, 12, 284–293. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Noncommunicable Diseases Country Profiles 2014. World Health Organization. 2014. Available online: https://apps.who.int/iris/handle/10665/128038, (accessed on 10 September 2020).
- The UAE National Health Survey Report 2017–2018. Dubai, UAE. 2019. Available online: https://www.mohap.gov.ae/Files/MOH_OpenData/1556/UAE_NHS_2018.pdf (accessed on 14 May 2021).
- Ministry of Health in Kuwait, Eastern Mediterranean Approach for Control of Non Communicable Diseases (EMAN). Survey for Risk Factors for Chronic Non-Communicable Diseases. WHO.int. 2015. Available online: http://www.who.int/chp/steps/Kuwait_2014_STEPS_Report.pdf?ua=1 (accessed on 10 December 2020).
- Al-Hanawi, M.K.; Keetile, M. Socio-Economic and Demographic Correlates of Non-communicable Disease Risk Factors among Adults in Saudi Arabia. Front. Med. 2021, 8, 8. [Google Scholar] [CrossRef] [PubMed]
- Al-Mawali, A.; Jayapal, S.K.; Morsi, M.; Al-Shekaili, W.; Pinto, A.D.; Al-Kharusi, H.; Al-Harrasi, A.; Al-Balushi, Z.; Idikula, J. Prevalence of Risk Factors of Non-Communicable Diseases in the Sultanate of Oman: STEPS Survey 2017. 2020. Available online: https://assets.researchsquare.com/files/rs-192942/v1/531ce0c1-b702-4d3b-a9d0-28efac6d836e.pdf?c=1616498059 (accessed on 19 January 2021).
- Dubai Statistics Center. Population by Gender—Emirate of Dubai. 2019. Available online: https://www.dsc.gov.ae/en-us/Themes/Pages/Population-and-Vital-Statistics.aspx?Theme=42 (accessed on 15 April 2020).
- Dubai Economic Report 2018. Available online: http://www.dubaided.ae/StudiesAndResearchDocument/Dubai-Economic-Report-2018-Full-Report.pdf (accessed on 15 April 2020).
- Loney, T.; Aw, T.C.; Handysides, D.G.; Ali, R.; Blair, I.; Grivna, M.; Shah, S.M.; Sheek-Hussein, M.; El-Sadig, M.; Sharif, A.A.; et al. An analysis of the health status of the United Arab Emirates: The ‘Big 4’ public health issues. Glob. Health Action 2013, 6, 20100. [Google Scholar] [CrossRef] [PubMed]
- Alnakhi, W.K.; Segal, J.B.; Frick, K.D.; Hussin, A.; Ahmed, S.; Morlock, L. Treatment destinations and visit frequencies for patients seeking medical treatment overseas from the United Arab Emirates: Results from Dubai Health Authority reporting during 2009–2016. Trop. Dis. Travel Med. Vaccines 2019, 5, 1–10. [Google Scholar] [CrossRef]
- Mayosi, B.M.; Flisher, A.J.; Lalloo, U.G.; Sitas, F.; Tollman, S.; Bradshaw, D. The burden of non-communicable diseases in South Africa. Lancet 2009, 374, 934–947. [Google Scholar] [CrossRef]
- Allen, L. Are we facing a noncommunicable disease pandemic? J. Epidemiol. Glob. Health 2016, 7, 5–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hosseinpoor, A.R.; Bergen, N.; Kunst, A.; Harper, S.; Guthold, R.; Rekve, D.; D’Espaignet, E.T.; Naidoo, N.; Chatterji, S. Socioeconomic inequalities in risk factors for non communicable diseases in low-income and middle-income countries: Results from the World Health Survey. BMC Public Health 2012, 12, 912. [Google Scholar] [CrossRef] [Green Version]
- van Zyl, S.; van der Merwe, L.J.; Walsh, C.M.; Groenewald, A.J.; van Rooyen, F.C. Risk-factor profiles for NCDs of lifestyle and metabolic syndrome in an urban and rural setting in South Africa. Afr. J. Prim. Health Care Fam. Med. 2012, 4, 346. [Google Scholar] [CrossRef] [Green Version]
- Afshar, S.; Roderick, P.J.; Kowal, P.; Dimitrov, B.D.; Hill, A.G. Multimorbidity and the inequalities of global ageing: A cross-sectional study of 28 countries using the World Health Surveys. BMC Public Health 2015, 15, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Skinner, K.M.; Miller, D.R.; Lincoln, E.; Lee, A.; Kazis, L.E. Concordance between respondent self-reports and medical records for chronic conditions: Experience from the Veterans Health Study. J. Ambul. Care Manag. 2005, 28, 102–110. [Google Scholar] [CrossRef]
- Smith, T.C.; Smith, B.; Jacobson, I.G.; Corbeil, T.E.; Ryan, M.A. Reliability of Standard Health Assessment Instruments in a Large, Population-Based Cohort Study. Ann. Epidemiol. 2007, 17, 525–532. [Google Scholar] [CrossRef]
- Martin, L.M.; Leff, M.; Calonge, N.; Garrett, C.; Nelson, D.E. Validation of self-reported chronic conditions and health services in a managed care population. Am. J. Prev. Med. 2000, 18, 215–218. [Google Scholar] [CrossRef]
- Comino, E.J.; Tran, D.T.; Haas, M.; Flack, J.; Jalaludin, B.; Jorm, L.; Harris, M.F. Validating self-report of diabetes use by participants in the 45 and up study: A record linkage study. BMC Health Serv. Res. 2013, 13, 481. [Google Scholar] [CrossRef] [PubMed]
- Dunstan, D.W.; Zimmet, P.Z.; Welborn, T.A.; Cameron, A.J.; Shaw, J.; De Courten, M.; Jolley, D.; McCarty, D.J.; AusDiab Steering Committee. The Australian diabetes, obesity and life-style study (AusDiab)--methods and response rates. Diabetes Res. Clin. Pract. 2002, 57, 119–129. [Google Scholar] [CrossRef] [Green Version]
- Dubai Health Authority. Dubai Household Health Survey Full Report. 2019. Available online: https://www.dha.gov.ae/Documents/opendata/English_DDHS.pdf (accessed on 20 November 2020).
- World Health Organization. Noncommunicable Diseases Progress Monitor 2020; World Health Organization: Geneva, Switzerland, 2020; pp. 35–39. ISBN 978-92-4-000049-0. Available online: https://www.who.int/publications/i/item/ncd-progress-monitor-2020. (accessed on 20 February 2021).
- Rao, J.N.K.; Scott, A.J. On Chi-Squared Tests for Multiway Contingency Tables with Cell Proportions Estimated from Survey Data. Ann. Stat. 1984, 12, 46–60. [Google Scholar] [CrossRef]
- Koch, G.G.; Freeman, D.H.; Freeman, J.L. Strategies in the Multivariate Analysis of Data from Complex Surveys. Int. Stat. Rev. 1975, 43, 59. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria; Available online: https://www.R-project.org/9 (accessed on 19 January 2021).
- Badr, H.; Maktabi, M.A.; Al-Kandari, M.; Sibai, A.M. Review of Non-Communicable Disease Research Activity in Kuwait: Where is the Evidence for the Best Practice? Ann Glob Health. 2019, 85, 45. [Google Scholar] [CrossRef] [Green Version]
- Hamadeh, R.R. Noncommunicable diseases among the Bahraini population: A review. East. Mediterr. Health J. 2002, 6, 1091–1097. [Google Scholar]
- Radwan, H.; Ballout, R.A.; Hasan, H.; Lessan, N.; Karavetian, M.; Rizk, R. The Epidemiology and Economic Burden of Obesity and Related Cardiometabolic Disorders in the United Arab Emirates: A Systematic Review and Qualitative Synthesis. J. Obes. 2018, 2018, 1–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Najafi, F.; Moradinazar, M.; Hamzeh, B.; Rezaeian, S. The reliability of self-reporting NCDs: How reliable is the result of popula-tion-based cohort studies. J. Prev. Med. Hyg. 2019, 60, E349–E353. [Google Scholar]
- Manning, K.; Senekal, M.; Harbron, J. Non-communicable disease risk factors and treatment preference of obese patients in Cape Town. Afr. J. Prim. Health Care Fam. Med. 2016, 8, e1–e12. [Google Scholar] [CrossRef]
- El-Shahat, I.Y.; Bakir, S.Z.; Farjou, N.; Hashim, T.; Bohaliga, A.; Al-Hossani, H.; Jaffar, A.R. Hypertension in UAE Citizens—Preliminary Results of a Prospective Study. Saudi J. Kidney Dis. Transpl. 2008, 10, 376–381. [Google Scholar]
- Shah, S.M.; Loney, T.; Sheek-Hussein, M.; El Sadig, M.; Al Dhaheri, S.; El Barazi, I.; Al Marzouqi, L.; Aw, T.-C.; Ali, R. Hypertension prevalence, awareness, treatment, and control, in male South Asian immigrants in the United Arab Emirates: A cross-sectional study. BMC Cardiovasc. Disord. 2015, 15, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alawadi, F.; Hassanein, M.; Suliman, E.; Hussain, H.Y.; Mamdouh, H.; Ibrahim, G.; Al Faisal, W.; Monsef, N.; Farghaly, M. The Prevalence of Diabetes and Pre-Diabetes among the Dubai Population: Findings from Dubai Household Health Surveys, 2014 and 2017. Dubai Diabetes Endocrinol. J. 2020, 26, 78–84. [Google Scholar] [CrossRef]
- Sulaiman, N.; Albadawi, S.; Abusnana, S.; Mairghani, M.; Hussein, A.; Al Awadi, F.; Madani, A.; Zimmet, P.; Shaw, J. High prevalence of diabetes among migrants in the United Arab Emirates using a cross-sectional survey. Sci. Rep. 2018, 8, 6862. [Google Scholar] [CrossRef] [PubMed]
- Mahmood, F.M. Prevalence and prevention of lifestyle-related diseases in Saudi Arabia. Int. J. Health Sci. 2018, 12, 1–2. [Google Scholar]
- Ong, M.E.H.; Shin, S.D.; De Souza, N.N.A.; Tanaka, H.; Nishiuchi, T.; Song, K.J.; Ko, P.C.-I.; Leong, B.S.-H.; Khunkhlai, N.; Naroo, G.Y.; et al. Outcomes for out-of-hospital cardiac arrests across 7 countries in Asia: The Pan Asian Resuscitation Outcomes Study (PAROS). Resuscitation 2015, 96, 100–108. [Google Scholar] [CrossRef]
- Malik, M.; Bakir, A.; Saab, B.A.; Roglic, G.; King, H. Glucose intolerance and associated factors in the multi-ethnic population of the United Arab Emirates: Results of a national survey. Diabetes Res. Clin. Pr. 2005, 69, 188–195. [Google Scholar] [CrossRef]
- Balfour, P.C.; Rodriguez, C.J.; Ferdinand, K.C. The Role of Hypertension in Race-Ethnic Disparities in Cardiovascular Disease. Curr. Cardiovasc. Risk Rep. 2015, 9, 1–8. [Google Scholar] [CrossRef] [Green Version]
- O’Loughlin, J. Understanding the role of ethnicity in NCD: A challenge for the new millennium. CMAJ 1999, 161, 152–153. [Google Scholar]
- Strauss, J.; Gertler, P.J.; Rahman, O.; Fox, K. Gender and Life-Cycle Differentials in the Patterns and Determinants of Adult Health. J. Hum. Resour. 1993, 28, 791. [Google Scholar] [CrossRef]
- Charmaz, K. Identity dilemmas of chronically ill men. Sociol. Q 1994, 35, 269–288. [Google Scholar] [CrossRef]
- Traynor, V. One world, one future. Elder. Care 1998, 10, 12. [Google Scholar] [CrossRef] [PubMed]
- Babwah, F.; Baksh, S.; Blake, L.; Cupid-Thuesday, J.; Hosein, I.; Sookhai, A.; Poon-King, C.; Hutchinson, G. The role of gender in compliance and attendance at an outpatient clinic for type 2 diabetes mellitus in Trinidad. Rev. Panam. Salud Pública 2006, 19, 79–84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bird, C.E.; Rieker, P.P. Gender matters: An integrated model for understanding men’s and women’s health. Soc. Sci. Med. 1999, 48, 745–755. [Google Scholar] [CrossRef]
- Senanayake, P. Women and reproductive health in a graying world. Int. J. Gynecol. Obstet. 2000, 70, 59–67. [Google Scholar] [CrossRef]
- Joung, I.M.; Van De Mheen, H.; Stronks, K.; Van Poppel, F.W.; MacKenbach, J.P. Differences in self-reported morbidity by marital status and by living arrangement. Int. J. Epidemiol. 1994, 23, 91–97. [Google Scholar] [CrossRef]
- Verbrugge, L.M. Marital Status and Health. J. Marriage Fam. 1979, 41, 267. [Google Scholar] [CrossRef]
- Franke, S.; Kulu, H. Mortality Differences by Partnership Status in England and Wales: The Effect of Living Arrangements or Health Selection? Eur. J. Popul. 2017, 34, 87–118. [Google Scholar] [CrossRef] [Green Version]
- Goldman, N.; Korenman, S.; Weinstein, R. Marital status and health among the elderly. Soc. Sci. Med. 1995, 40, 1717–1730. [Google Scholar] [CrossRef]
- Rendall, M.S.; Weden, M.M.; Favreault, M.M.; Waldron, H. The Protective Effect of Marriage for Survival: A Review and Update. Demography 2011, 48, 481–506. [Google Scholar] [CrossRef] [PubMed]
- Zueras, P.; Rutigliano, R.; Trias-Llimós, S. Marital status, living arrangements, and mortality in middle and older age in Europe. Int. J. Public Health 2020, 65, 627–636. [Google Scholar] [CrossRef] [PubMed]
- Bauer, U.E.; Briss, P.A.; Goodman, R.A.; Bowman, B.A. Prevention of NCD in the 21st century: Elimination of the leading preventable causes of premature death and disability in the USA. Lancet 2014, 384, 45–52. [Google Scholar] [CrossRef]
- Who.int. Non Communicable Diseases. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 21 April 2021).
- Al-Houqani, M.; Leinberger-Jabari, A.; Al Naeemi, A.; Al Junaibi, A.; Al Zaabi, E.; Oumeziane, N.; Kazim, M.; Al-Maskari, F.; Al Dhaheri, A.; Wareth, L.A.; et al. Patterns of tobacco use in the United Arab Emirates Healthy Future (UAEHFS) pilot study. PLoS ONE 2018, 13, e0198119. [Google Scholar] [CrossRef] [Green Version]
- Jarallah, J.S.; Al-Rubeaan, K.A.; Al-Nuaim, A.R.A.; Al-Ruhaily, A.A.; Kalantan, K.A. Prevalence and determinants of smoking in three regions of Saudi Arabia. Tob. Control. 1999, 8, 53–56. [Google Scholar] [CrossRef] [PubMed]
- Alhashimi, F.H.; Khabour, O.F.; Alzoubi, K.H.; Al-Shatnawi, S.F. Attitudes and beliefs related to reporting alcohol consumption in research studies: A case from Jordan. Pragmat Obs Res. 2018, 9, 55–61. [Google Scholar] [CrossRef] [Green Version]
- Ghandour, L.; Chalak, A.; El-Aily, A.; Yassin, N.; Nakkash, R.; Tauk, M.; El Salibi, N.; Heffron, M.; Afifi, R. Alcohol consumption in the Arab region: What do we know, why does it matter, and what are the policy implications for youth harm reduction? Int. J. Drug Policy 2016, 28, 10–33. [Google Scholar] [CrossRef]
| Variable | Category | Having NCDs | Wald’s χ12 Test (ndf) | p Value | |
|---|---|---|---|---|---|
| No | Yes | ||||
| Age groups (years) | 18–24 | 298,774 (95.86%) | 12,893 (4.14%) | 39.03 (3) | <0.0001 |
| 25–44 | 1,644,723 (92.57%) | 132,052 (7.43%) | |||
| 45–59 | 344,062 (71.86%) | 134,735 (28.14%) | |||
| 60+ | 54,435 (51.97%) | 50,300 (48.03%) | |||
| Gender | Female | 697,618 (89.29%) | 83,644 (10.71%) | 3.39 (1) | 0.067 |
| Male | 1,644,376 (86.97%) | 246,336 (13.03%) | |||
| Nationality | Asians | 1,629,905 (87.85%) | 225,415 (12.15%) | 37.17 (3) | <0.0001 |
| Local-Arabs (Emirati) | 117,901(74.68%) | 39,604 (25.14%) | |||
| Non-Local-Arabs | 253,466 (90.25%) | 27,373 (9.75%) | |||
| Other nationalities | 340,722 (90.16%) | 37,589 (9.94%) | |||
| Marital Status | Married | 1,551,962 (85.25%) | 268,558 (14.75%) | 32.42 (2) | <0.0001 |
| Single | 751,578 (94.78%) | 41,425 (5.22%) | |||
| Others * | 38,454 (65.79%) | 19,997 (34.21%) | |||
| Work Status | Currently working | 2,008,951 (88.61%) | 258,271 (11.39%) | 18.33 (1) | <0.0001 |
| Currently not working | 333,043 (82.28%) | 71,709 (17.72%) | |||
| Educational Attainment | Less than secondary education | 570,458 (85.13%) | 99,666 (14.87%) | 1.31 (2) | 0.271 |
| Completed secondary school | 525,871 (88.27%) | 69,888 (11.73%) | |||
| Tertiary education | 1,245,666 (88.59%) | 160,427 (11.41%) | |||
| Income Categories | Low Income | 344,101(88.78%) | 43,509 (11.22%) | 1.74 (3) | 0.161 |
| Middle income | 188,026 (85.96%) | 30,714 (14.04%) | |||
| High income | 209,398 (83.76%) | 40,611 (16.24%) | |||
| Total | 84.99% | 15.01% | |||
| Variable | Category | Odds Ratio (95% CI) | Wald’s χ12 Test | p Value |
|---|---|---|---|---|
| Age (years) | 18–60+ | 3.6 (2.8, 4.7) | 90.32 | <0.001 |
| Marital Status | Married | (Reference) | ||
| Unmarried | 0.11 (0.02, 0.70) | 5.43 | 0.020 | |
| Others | 0.32 (0.04, 2.32) | 1.28 | 0.258 | |
| Nationality | Asians | (Reference) | ||
| Local-Arab (Emirati) | 2.08 (1.62, 2.67) | 32.49 | <0.001 | |
| Non-Local (other Arabs) | 0.72 (0.45, 1.15) | 1.94 | 0.163 | |
| Other Nationalities | 0.81 (0.56, 1.18) | 1.19 | 0.275 | |
| Gender | Female | (Reference) | ||
| Male | 1.61 (1.28, 2.04) | 16.107 | <0.001 | |
| Educational Attainment | Education tertiary education | (Reference) | ||
| Education less than secondary school | 1.09 (0.73, 1.64) | 0.181 | 0.671 | |
| Completed secondary school | 1.18 (0.80, 1.74) | 0.69 | 0.407 | |
| Age and marital Status | Age & married marital status | (Reference) | ||
| Age & unmarried marital status | 2.75 (1.24, 6.09) | 6.17 | 0.013 | |
| Age & other marital status | 1.56 (0.86, 2.85) | 2.12 | 0.146 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alnakhi, W.K.; Mamdouh, H.; Hussain, H.Y.; Ibrahim, G.M.; Ahmad, A.S.; Ali, R.; Abdulle, A. The Socio-Demographic Characteristics Associated with Non-Communicable Diseases among the Adult Population of Dubai: Results from Dubai Household Survey 2019. Healthcare 2021, 9, 1139. https://doi.org/10.3390/healthcare9091139
Alnakhi WK, Mamdouh H, Hussain HY, Ibrahim GM, Ahmad AS, Ali R, Abdulle A. The Socio-Demographic Characteristics Associated with Non-Communicable Diseases among the Adult Population of Dubai: Results from Dubai Household Survey 2019. Healthcare. 2021; 9(9):1139. https://doi.org/10.3390/healthcare9091139
Chicago/Turabian StyleAlnakhi, Wafa K., Heba Mamdouh, Hamid Y. Hussain, Gamal M. Ibrahim, Amar Sabri Ahmad, Raghib Ali, and Abdishakur Abdulle. 2021. "The Socio-Demographic Characteristics Associated with Non-Communicable Diseases among the Adult Population of Dubai: Results from Dubai Household Survey 2019" Healthcare 9, no. 9: 1139. https://doi.org/10.3390/healthcare9091139
APA StyleAlnakhi, W. K., Mamdouh, H., Hussain, H. Y., Ibrahim, G. M., Ahmad, A. S., Ali, R., & Abdulle, A. (2021). The Socio-Demographic Characteristics Associated with Non-Communicable Diseases among the Adult Population of Dubai: Results from Dubai Household Survey 2019. Healthcare, 9(9), 1139. https://doi.org/10.3390/healthcare9091139






