Electronic Device Use before Bedtime and Sleep Quality among University Students
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
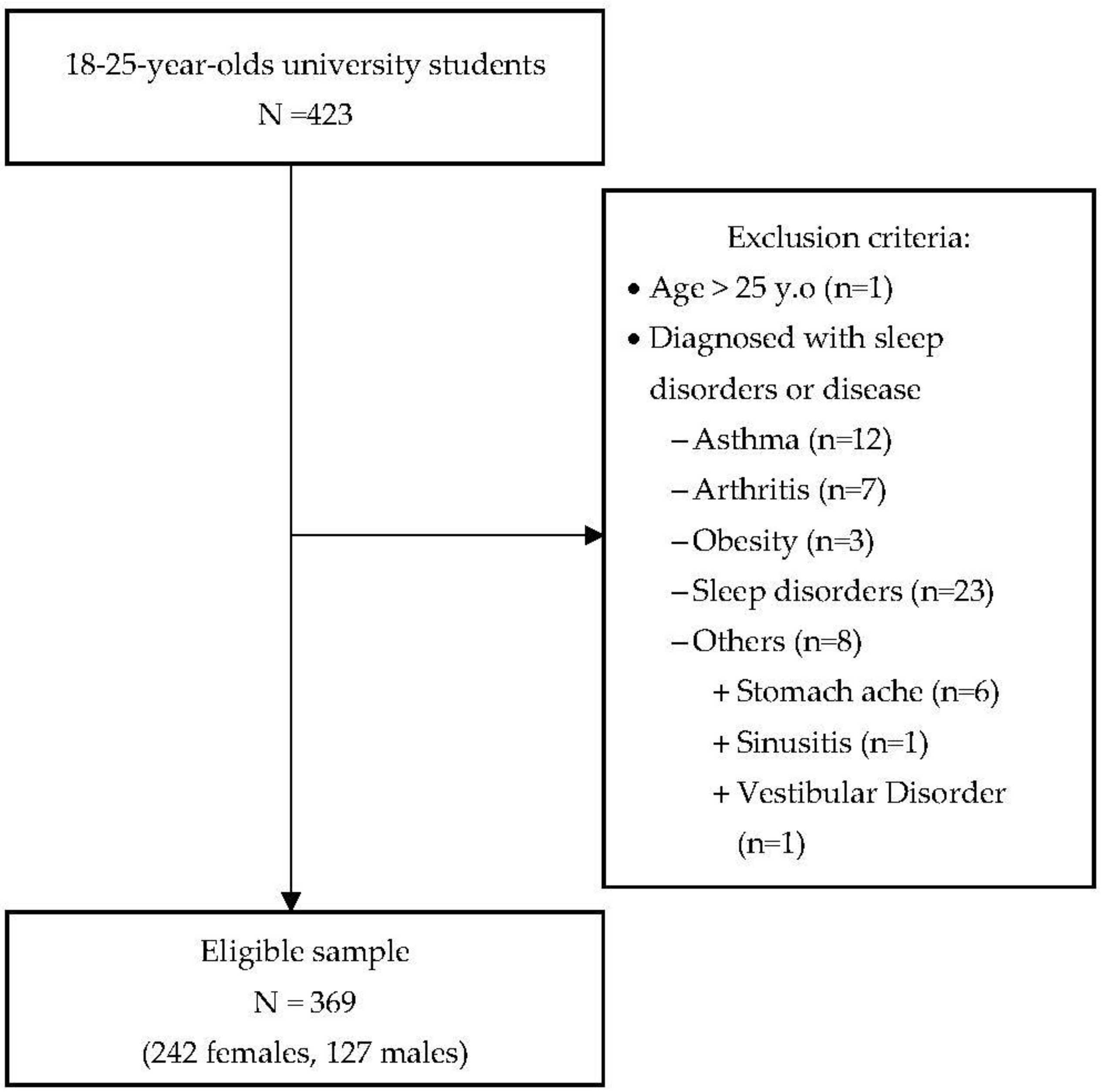
2.2. Participants
2.3. Measures
2.4. Data Analysis
3. Results
3.1. Sleep Quality
3.2. ED-Use Behavior and Sleep Quality
3.3. Factors Associated with Sleep Quality
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Acknowledgments
Conflicts of Interest
References
- Dinis, J.; Braganca, M. Quality of Sleep and Depression in College Students: A Systematic Review. Sleep Sci. 2018, 11, 290–301. [Google Scholar] [CrossRef]
- Hershner, S.D.; Chervin, R.D. Causes and consequences of sleepiness among college students. Nat. Sci. Sleep 2014, 6, 73–84. [Google Scholar] [CrossRef] [Green Version]
- Li, L.; Wang, Y.-Y.; Wang, S.-B.; Li, L.; Lu, L.; Ng, C.H.; Ungvari, G.S.; Chiu, H.F.K.; Hou, C.-L.; Jia, F.-J.; et al. Sleep Duration and Sleep Patterns in Chinese University Students: A Comprehensive Meta-Analysis. J. Clin. Sleep Med. JCSM Off. Publ. Am. Acad. Sleep Med. 2017, 13, 1153–1162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buboltz, W., Jr.; Jenkins, S.M.; Soper, B.; Woller, K.; Johnson, P.; Faes, T. Sleep habits and patterns of college students: An expanded study. J. Coll. Couns. 2009, 12, 113–124. [Google Scholar] [CrossRef]
- Yazdi, Z.; Loukzadeh, Z.; Moghaddam, P.; Jalilolghadr, S. Sleep Hygiene Practices and Their Relation to Sleep Quality in Medical Students of Qazvin University of Medical Sciences. J. Caring Sci. 2016, 5, 153–160. [Google Scholar] [CrossRef]
- Lemma, S.; Gelaye, B.; Berhane, Y.; Worku, A.; Williams, M.A. Sleep quality and its psychological correlates among university students in Ethiopia: A cross-sectional study. BMC Psychiatry 2012, 12, 237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lund, H.G.; Reider, B.D.; Whiting, A.B.; Prichard, J.R. Sleep Patterns and Predictors of Disturbed Sleep in a Large Population of College Students. J. Adolesc. Health 2010, 46, 124–132. [Google Scholar] [CrossRef]
- Nguyen, T.K.L.; Dang, H.N.; Pham, B.B.N.; Vo, V.T.; Nguyen, M.T. Sleep quality and its related factors among students at Hue University of Medicine and Pharmacy in 2015. Viet Nam Journal of Preventive Medicine 2015, 08, 109. [Google Scholar]
- Tarokh, L.; Raffray, T.; Van Reen, E.; Carskadon, M.A. Physiology of normal sleep in adolescents. Adolesc Med. State Art Rev. 2010, 21, 401–417, vii. [Google Scholar]
- Duffy, J.F.; Czeisler, C.A. Effect of Light on Human Circadian Physiology. Sleep Med. Clin. 2009, 4, 165–177. [Google Scholar] [CrossRef] [Green Version]
- Gabel, V.; Maire, M.; Reichert, C.F.; Chellappa, S.L.; Schmidt, C.; Hommes, V.; Viola, A.U.; Cajochen, C. Effects of artificial dawn and morning blue light on daytime cognitive performance, well-being, cortisol and melatonin levels. Chronobiol. Int. 2013, 30, 988–997. [Google Scholar] [CrossRef] [Green Version]
- Wallace-Guy, G.M.; Kripke, D.F.; Jean-Louis, G.; Langer, R.D.; Elliott, J.A.; Tuunainen, A. Evening light exposure: Implications for sleep and depression. J. Am. Geriatr Soc. 2002, 50, 738–739. [Google Scholar] [CrossRef] [PubMed]
- Chellappa, S.L.; Steiner, R.; Oelhafen, P.; Lang, D.; Gotz, T.; Krebs, J.; Cajochen, C. Acute exposure to evening blue-enriched light impacts on human sleep. J. Sleep Res. 2013, 22, 573–580. [Google Scholar] [CrossRef] [Green Version]
- Kozaki, T.; Kitamura, S.; Higashihara, Y.; Ishibashi, K.; Noguchi, H.; Yasukouchi, A. Effect of color temperature of light sources on slow-wave sleep. J. Physiol. Anthr. Appl. Hum. Sci. 2005, 24, 183–186. [Google Scholar] [CrossRef] [Green Version]
- Studer, P.; Brucker, J.M.; Haag, C.; Van Doren, J.; Moll, G.H.; Heinrich, H.; Kratz, O. Effects of blue- and red-enriched light on attention and sleep in typically developing adolescents. Physiol. Behav. 2019, 199, 11–19. [Google Scholar] [CrossRef]
- Cajochen, C.; Frey, S.; Anders, D.; Spati, J.; Bues, M.; Pross, A.; Mager, R.; Wirz-Justice, A.; Stefani, O. Evening exposure to a light-emitting diodes (LED)-backlit computer screen affects circadian physiology and cognitive performance. J. Appl. Physiol. (1985) 2011, 110, 1432–1438. [Google Scholar] [CrossRef] [Green Version]
- The Neisel Company. Southeast Asian Digital Consumer Habits. Available online: https://www.nielsen.com/us/en/insights/report/2011/south-east-asian-digital-consumer-habits/ (accessed on 17 August 2021).
- Moore Corporation. Vietnam Digital Landscape. Available online: https://www.slideshare.net/digitalknowledge/vietnam-digital-landscape-q32015-by-moore-corporation/16-ONLINEACTIVITIESBYTIMEOFDAY051015202530354045Before_9am_9am_Before12pm12pm_Before2pm2pm (accessed on 17 August 2021).
- Lavender, R.M. Electronic Media Use and Sleep Quality. Undergrad. J. Psychol. 2015, 28, 55–62. [Google Scholar]
- Hysing, M.; Pallesen, S.; Stormark, K.M.; Jakobsen, R.; Lundervold, A.J.; Sivertsen, B. Sleep and use of electronic devices in adolescence: Results from a large population-based study. BMJ Open 2015, 5, e006748. [Google Scholar] [CrossRef] [Green Version]
- Owens, J. Insufficient sleep in adolescents and young adults: An update on causes and consequences. Pediatrics 2014, 134, e921–e932. [Google Scholar] [CrossRef] [Green Version]
- Silver, L.; Smith, A.; Johnson, C.; Taylor, K.; Jiang, J.; Anderson, M.; Rainie, L. Mobile Connectivity in Emerging Economies; Pew Research Center: Washington, DC, USA, 2019. [Google Scholar]
- Zhang, M.W.; Tran, B.X.; Hinh, N.D.; Nguyen, H.L.T.; Tho, T.D.; Latkin, C.; Ho, R.C. Internet addiction and sleep quality among Vietnamese youths. Asian J. Psychiatry 2017, 28, 15–20. [Google Scholar] [CrossRef]
- Hale, L.; Guan, S. Screen time and sleep among school-aged children and adolescents: A systematic literature review. Sleep Med. Rev. 2015, 21, 50–58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bunyalug, M.; Kanchanakhan, N. Effect of Using Smartphone before Bed on Sleep Quality among Undergraduate Students at Chulalongkorn University, Thailand. J. Health Res. 2017, 31, S225–S231. [Google Scholar]
- Mohammadbeigi, A.; Valizadeh, F.; Saadati, M.; Sharifimoghadam, S.; Ahmadi, A.; Mokhtari, M.; Ansari, H. Sleep quality in medical students; the impact of over-use of mobile cell-phone and social networks. J. Res. Health Sci. 2016, 16, 46–50. [Google Scholar]
- Orzech, K.M.; Grandner, M.A.; Roane, B.M.; Carskadon, M.A. Digital media use in the 2 h before bedtime is associated with sleep variables in university students. Comput. Hum. Behav. 2016, 55, 43–50. [Google Scholar] [CrossRef] [Green Version]
- Dolezal, B.A.; Neufeld, E.V.; Boland, D.M.; Martin, J.L.; Cooper, C.B. Interrelationship between Sleep and Exercise: A Systematic Review. Adv. Prev. Med. 2017, 2017, 1364387. [Google Scholar] [CrossRef]
- Drake, C.; Roehrs, T.; Shambroom, J.; Roth, T. Caffeine effects on sleep taken 0, 3, or 6 hours before going to bed. J. Clin. Sleep Med. 2013, 9, 1195–1200. [Google Scholar] [CrossRef] [Green Version]
- Stein, M.D.; Friedmann, P.D. Disturbed sleep and its relationship to alcohol use. Subst. Abus. 2005, 26, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, J.K.M.; Trinder, J.; Andrewes, H.E.; Colrain, I.M.; Nicholas, C.L. The acute effects of alcohol on sleep architecture in late adolescence. Alcohol. Clin. Exp. Res. 2013, 37, 1720–1728. [Google Scholar] [CrossRef] [Green Version]
- McNamara, J.P.; Wang, J.; Holiday, D.B.; Warren, J.Y.; Paradoa, M.; Balkhi, A.M.; Fernandez-Baca, J.; McCrae, C.S. Sleep disturbances associated with cigarette smoking. Psychol. Health Med. 2014, 19, 410–419. [Google Scholar] [CrossRef]
- To, N.; Nguyen, N. Validity of the Vietnamese version of the Pittsburgh sleep quality index. Sleep Med. 2015, 16, S52. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F., 3rd; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Thanh, N.D.; Quyen, B.T.; Tien, T.Q. Validation of a brief CES-D scale for measuring depression and its associated predictors among adolescents in Chi Linh, Hai Duong, Vietnam. AIMS Public Health 2016, 3, 448. [Google Scholar] [CrossRef]
- Ayala, E.E.; Berry, R.; Winseman, J.S.; Mason, H.R. A cross-sectional snapshot of sleep quality and quantity among US medical students. Acad. Psychiatry 2017, 41, 664–668. [Google Scholar] [CrossRef]
- Pensuksan, W.C.; Lertmaharit, S.; Lohsoonthorn, V.; Rattananupong, T.; Sonkprasert, T.; Gelaye, B.; Williams, M.A. Relationship between Poor Sleep Quality and Psychological Problems among Undergraduate Students in the Southern Thailand. Walailak J. Sci. Technol. 2016, 13, 235–242. [Google Scholar]
- Cheng, S.H.; Shih, C.-C.; Lee, I.H.; Hou, Y.-W.; Chen, K.C.; Chen, K.-T.; Yang, Y.K.; Yang, Y.C. A study on the sleep quality of incoming university students. Psychiatry Res. 2012, 197, 270–274. [Google Scholar] [CrossRef] [PubMed]
- Suen, L.K.P.; Ellis Hon, K.L.; Tam, W.W.S. Association between Sleep Behavior and Sleep-Related Factors among University Students in Hong Kong. Chronobiol. Int. 2008, 25, 760–775. [Google Scholar] [CrossRef]
- Hirshkowitz, M.; W, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L. National Sleep Foundation’s sleep time duration recommendations: Methodology and results summary. Sleep Health 2015, 1, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Peltzer, K.; Pengpid, S. Sleep duration and health correlates among university students in 26 countries. Psychol. Health Med. 2016, 21, 208–220. [Google Scholar] [CrossRef]
- Alshobaili, F.A.; AlYousefi, N.A. The effect of smartphone usage at bedtime on sleep quality among Saudi non-medical staff at King Saud University Medical City. J. Fam. Med. Prim. Care 2019, 8, 1953. [Google Scholar] [CrossRef]
- Levenson, J.C.; Shensa, A.; Sidani, J.E.; Colditz, J.B.; Primack, B.A. Social media use before bed and sleep disturbance among young adults in the United States: A nationally representative study. Sleep 2017, 40, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Algorta, G.P.; Van Meter, A.; Dubicka, B.; Jones, S.; Youngstrom, E.; Lobban, F. Blue blocking glasses worn at night in first year higher education students with sleep complaints: A feasibility study. Pilot Feasibility Stud. 2018, 4, 1–7. [Google Scholar]
| Factors | n | % | Mean | SD | F | p |
|---|---|---|---|---|---|---|
| Gender | ||||||
| Female | 242 | 65.6 | 5.87 | 2.64 | 2.536 | 0.112 |
| Male | 127 | 34.4 | 5.38 | 3.11 | ||
| Year of study | ||||||
| Freshmen | 75 | 20.3 | 5.65 | 2.78 | 1.166 | 0.322 |
| Sophomore | 155 | 42.0 | 5.45 | 2.73 | ||
| Junior | 111 | 30.1 | 6.10 | 2.79 | ||
| Senior | 28 | 7.6 | 5.61 | 3.39 | ||
| Department | ||||||
| Nursing | 222 | 60.2 | 5.70 | 2.62 | 0.108 | 0.898 |
| Law | 84 | 22.8 | 5.61 | 3.00 | ||
| Electronics | 63 | 17.0 | 5.83 | 3.22 | ||
| Living status | ||||||
| Family | 168 | 45.5 | 5.31 | 2.80 | 2.395 | 0.093 |
| Alone | 138 | 37.4 | 6.16 | 3.06 | ||
| Friend(s) | 63 | 17.1 | 5.85 | 2.70 | ||
| Caffeinated drink consumption a | ||||||
| No | 177 | 48.0 | 5.42 | 2.86 | 3.420 | 0.065 |
| Yes | 192 | 52.0 | 5.96 | 2.75 | ||
| Coffee | ||||||
| No | 312 | 15.4 | 5.55 | 2.74 | 5.655 | 0.018 |
| Yes | 57 | 84.6 | 6.51 | 3.09 | ||
| Tea | ||||||
| No | 339 | 8.1 | 5.68 | 2.79 | 0.226 | 0.635 |
| Yes | 30 | 91.9 | 5.93 | 3.11 | ||
| Milk tea | ||||||
| No | 253 | 31.4 | 5.56 | 2.810 | 2.053 | 0.153 |
| Yes | 116 | 68.6 | 6.01 | 2.805 | ||
| Energy drinks | ||||||
| No | 331 | 10.3 | 5.66 | 2.81 | 0.484 | 0.487 |
| Yes | 38 | 89.7 | 6.00 | 2.85 | ||
| Soft drinks | ||||||
| No | 303 | 17.9 | 5.62 | 2.76 | 1.442 | 0.231 |
| Yes | 66 | 83.1 | 6.08 | 3.03 | ||
| Alcohol consumption b | ||||||
| No | 236 | 64.0 | 5.45 | 2.60 | 5.055 | 0.025 |
| Yes | 133 | 36.0 | 6.14 | 3.11 | ||
| Smoking | ||||||
| No | 353 | 95.7 | 5.68 | 2.76 | 0.503 | 0.478 |
| Yes | 16 | 4.3 | 6.19 | 3.90 | ||
| Exercise c | ||||||
| No | 231 | 62.6 | 6.01 | 2.61 | 7.611 | 0.006 |
| Yes | 138 | 37.4 | 5.18 | 3.07 | ||
| n | % | |
|---|---|---|
| Sleep quality (PSQI-V) | 5.7 ± 2.8 (0–16) | |
| Good sleep (PSQI-V ≤ 5) | 189 | 51.2 |
| Poor sleep (PSQI-V > 5) | 180 | 48.8 |
| Subjective sleep quality | ||
| Very good | 61 | 16.5 |
| Fairly good | 239 | 64.8 |
| Fairly bad | 67 | 18.2 |
| Very bad | 2 | 0.5 |
| Sleep latency | ||
| <15 min | 215 | 58.3 |
| 16–30 min | 95 | 25.7 |
| 31–60 min | 36 | 9.8 |
| >60 min | 23 | 6.2 |
| Sleep disturbance a | ||
| Unable to fall asleep within 30 min | 65 | 17.6 |
| Waking up in the middle of the night or early in the morning | 35 | 9.5 |
| Having to get up to use the bathroom | 27 | 7.3 |
| Unable to breath comfortably | 10 | 2.7 |
| Coughing or snore loudly | 14 | 3.8 |
| Feeling too cold | 28 | 7.6 |
| Feeling too hot | 18 | 4.9 |
| Having bad dreams | 17 | 4.6 |
| Experiencing pain | 13 | 3.5 |
| Other reasons | 19 | 5.1 |
| Sleep duration | 6.4 ± 1.1 (311) hrs | |
| >= 7 h | 161 | 43.6 |
| 6–6.9 h | 137 | 37.1 |
| 5–5.9 h | 56 | 15.2 |
| 4–4.9 h | 15 | 4.1 |
| Habitual sleep efficiency (SE) b | ||
| >85% | 241 | 65.3 |
| 75~84% | 77 | 20.9 |
| 65~74% | 43 | 11.7 |
| <65% | 8 | 2.2 |
| Use of sleeping aid medication | ||
| None during the past month | 363 | 98.4 |
| <once/week | 4 | 1.1 |
| 1–2 times/week | 2 | 0.5 |
| >= 3 times/week | 0 | 0 |
| Daytime dysfunction | ||
| Trouble staying awake while driving, eating meals, and/or engaging in social activity | ||
| Not during the past month | 209 | 56.6 |
| <once/week | 86 | 23.3 |
| 1–2 times/week | 58 | 15.7 |
| >= 3 times/week | 16 | 4.3 |
| Trouble with enthusiasm to get things done | ||
| No problem | 76 | 20.6 |
| Slight problem | 208 | 56.4 |
| Somewhat problematic | 79 | 21.4 |
| Very problematic | 6 | 1.6 |
| Going to sleep after midnight | 247 | 66.9 |
| Factors | N | % | Mean | SD | F | p |
|---|---|---|---|---|---|---|
| ED use | ||||||
| No | 7 | 1.9 | 3.43 | 1.40 | 4.696 | 0.031 |
| Yes | 362 | 98.1 | 5.74 | 2.82 | ||
| ED use frequency | ||||||
| Daily | 320 | 88.4 | 5.85 | 2.88 | 1.847 | 0.138 |
| Sometimes/week | 38 | 10.5 | 4.97 | 2.19 | ||
| Once/week | 2 | 0.6 | 3.50 | 0.71 | ||
| 1–3 times/month | 2 | 0.6 | 6.00 | 2.83 | ||
| ED use duration | ||||||
| No use (0) | 7 | 1.9 | 3.43 | 1.397 | 9.842 | 0.000 a |
| 15–30 min (1) | 63 | 17.1 | 4.38 | 2.03 | (4) > (2) > (1) b; | |
| 30–60 min (2) | 103 | 27.9 | 5.40 | 2.42 | (4) > (0) | |
| 1–2 h (3) | 107 | 29.0 | 5.93 | 2.98 | (3) > (1) b; (3) > (0) | |
| >2 h (4) | 89 | 24.1 | 6.88 | 3.06 | ||
| ED location while sleeping | ||||||
| Under a pillow (1) | 24 | 6.5 | 6.71 | 3.41 | 3.722 | 0.012 |
| In bed (2) | 232 | 62.9 | 5.91 | 2.80 | (1) > (3) c | |
| In the bedroom but 5 m or more from the bed (3) | 106 | 28.7 | 5.08 | 2.61 | (2) > (3) c | |
| Outside the bedroom (4) | 7 | 1.9 | 4.43 | 2.22 | ||
| Adjust ED’s screen display light | ||||||
| No | 110 | 30.4 | 5.91 | 2.72 | 2.884 | 0.090 |
| Yes | 252 | 69.6 | 5.36 | 3.01 | ||
| ED mode while sleeping | ||||||
| Normal | 185 | 50.1 | 5.55 | 2.64 | 0.164 | 0.921 |
| Airplane | 92 | 24.9 | 5.68 | 2.69 | ||
| Silent | 49 | 13.3 | 5.95 | 3.24 | ||
| Vibrate | 43 | 11.7 | 5.70 | 2.99 | ||
| Variables | B | 95% CI | T | p |
|---|---|---|---|---|
| Coffee a | 0.726 | [−0.016, 1.467] | 1.923 | 0.055 |
| Alcohol b | 0.058 | [−0.529, 0.646] | 0.196 | 0.845 |
| Exercise c | −0.311 | [−0.879, 0.256] | −1.079 | 0.281 |
| EDs_place d | −0.381 | [−0.963, 0.201] | −1.289 | 0.198 |
| Depression e | 0.095 | [0.064, 0.127] | 6.025 | 0.000 |
| EDs_duration f | ||||
| EDs_duration_less than 30 min | 1.575 | [−0.422, 3.573] | 1.551 | 0.122 |
| EDs_duration_30 min_2 h | 2.588 | [0.667, 4.510] | 2.649 | 0.008 |
| EDs_duration_more 2 h | 3.343 | [1.383, 5.304] | 3.353 | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pham, H.T.; Chuang, H.-L.; Kuo, C.-P.; Yeh, T.-P.; Liao, W.-C. Electronic Device Use before Bedtime and Sleep Quality among University Students. Healthcare 2021, 9, 1091. https://doi.org/10.3390/healthcare9091091
Pham HT, Chuang H-L, Kuo C-P, Yeh T-P, Liao W-C. Electronic Device Use before Bedtime and Sleep Quality among University Students. Healthcare. 2021; 9(9):1091. https://doi.org/10.3390/healthcare9091091
Chicago/Turabian StylePham, Hue Thi, Hsiao-Ling Chuang, Ching-Pyng Kuo, Tzu-Pei Yeh, and Wen-Chun Liao. 2021. "Electronic Device Use before Bedtime and Sleep Quality among University Students" Healthcare 9, no. 9: 1091. https://doi.org/10.3390/healthcare9091091
APA StylePham, H. T., Chuang, H.-L., Kuo, C.-P., Yeh, T.-P., & Liao, W.-C. (2021). Electronic Device Use before Bedtime and Sleep Quality among University Students. Healthcare, 9(9), 1091. https://doi.org/10.3390/healthcare9091091








