Postural Control and Functional Ankle Stability in Professional and Amateur Skateboarders
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Subjects
2.2. Clinical History and Investigation
2.3. Range of Motion (ROM)
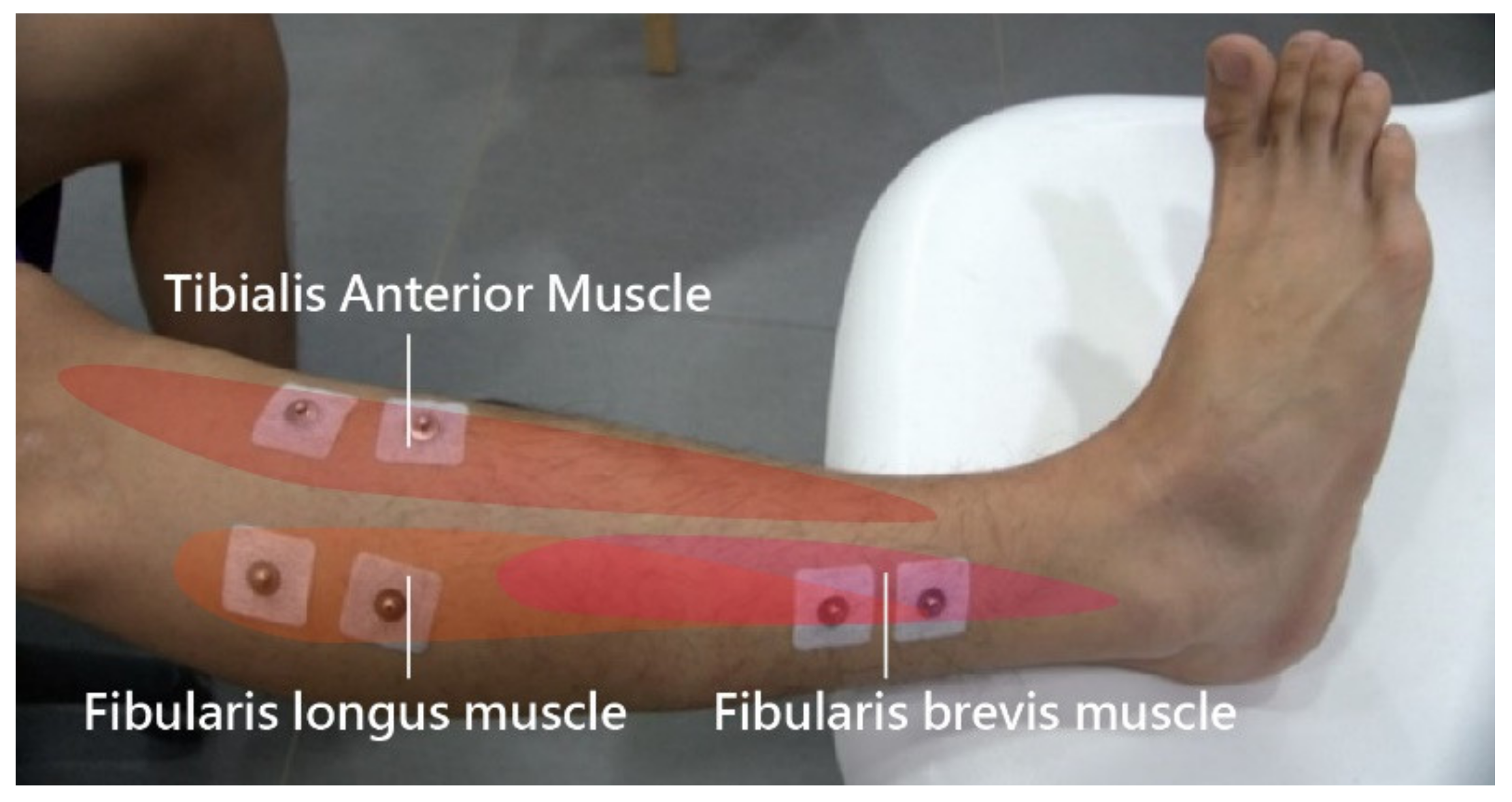
2.4. Muscle Reaction Time
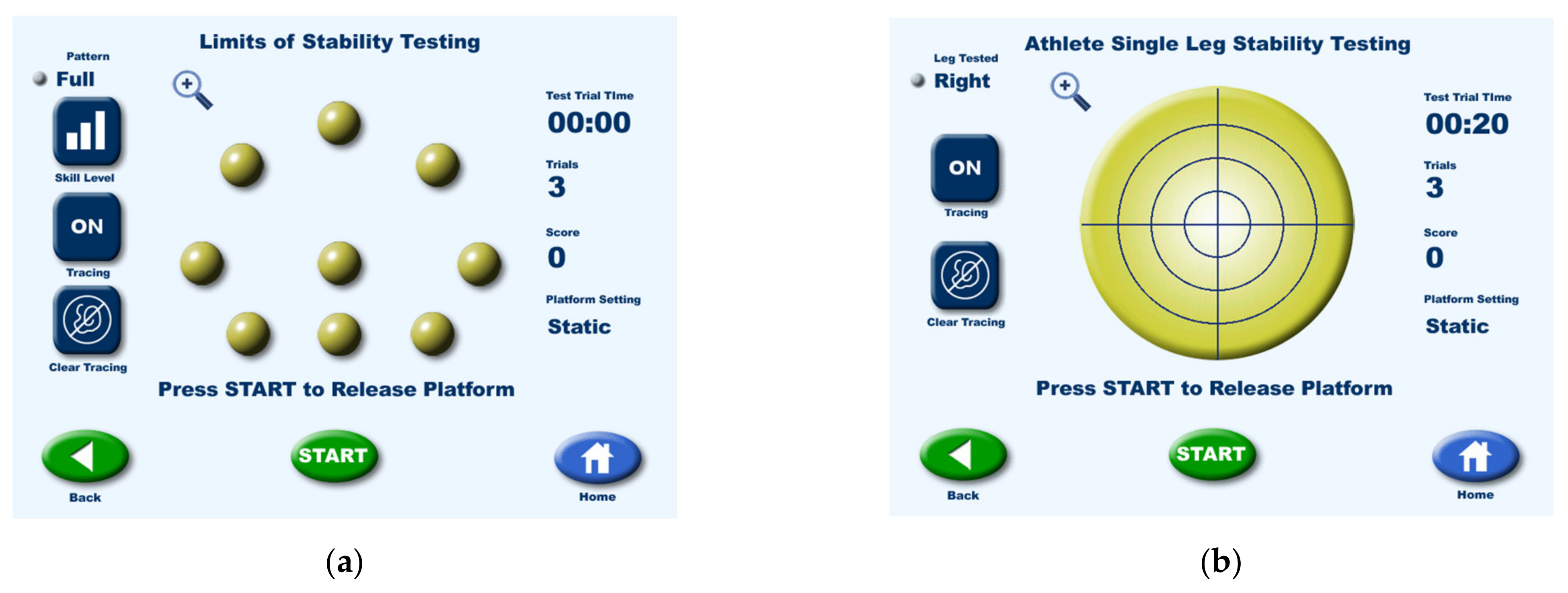
2.5. Postural Control
2.6. Tilting Platform
2.7. Research Procedure
2.8. Statistical Analysis
3. Results
3.1. Clinical History and Investigation
3.2. Ankle ROM
3.3. Muscle Reaction Time
3.3.1. Muscle Reaction Time in Professional versus Amateur Skateboarders
3.3.2. Muscle Reaction Time in Healthy versus Injured Skateboarders
3.4. Position Sense Test
3.4.1. Comparison of Stability Scores between Professional and Amateur Skateboarders at Levels 12 and 8
3.4.2. Comparing Stability Scores between Healthy and Injured Skateboarders at Levels 12 and 8
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- “Tokyo 2020 New Sport Support Kickoff Event” Held as Part of the Tokyo 2020 Official Programme. Available online: https://tokyo2020.jp/en/news/event/20161011-03.html (accessed on 3 May 2018).
- Smith, R.W.; Reischl, S.F. Treatment of ankle sprains in young athletes. Am. J. Sports Med. 1986, 14, 465–471. [Google Scholar] [CrossRef] [PubMed]
- Hertel, J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J. Athl. Train. 2002, 37, 364–375. [Google Scholar]
- Wikstrom, E.A.; Tillman, M.D.; Chmielewski, T.L.; Cauraugh, J.H. Dynamic postural stability deficits in subjects with self-reported ankle instability. Med. Sci. Sports Exerc. 2007, 39, 397–402. [Google Scholar] [CrossRef]
- Taylor, J.L. Proprioception. In Encyclopedia of Neuroscience; Squire, L.R., Ed.; Academic Press: Cambridge, UK, 2009; pp. 1143–1149. [Google Scholar]
- Lephart, S.M.; Fu, F.H. The role of proprioception in the treatment of sports injuries. Sports Exerc. Inj. 1995, 1, 96–102. [Google Scholar]
- Goldie, P.A.; Evans, O.M.; Bach, T.M. Postural control following inversion injuries of the ankle. Arch. Phys. Med. Rehabil. 1994, 75, 969–975. [Google Scholar] [CrossRef]
- Forkin, D.M.; Koczur, C.; Battle, R.; Newton, R.A. Evaluation of kinesthetic deficits indicative of balance control in gymnasts with unilateral chronic ankle sprains. J. Orthop. Sports Phys. Ther. 1996, 23, 245–250. [Google Scholar] [CrossRef] [Green Version]
- Switlick, T.; Kernozek, T.W.; Meardon, S. Differences in joint-position sense and vibratory threshold in runners with and without a history of overuse injury. J. Sport Rehabil. 2015, 24, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Hoch, M.C.; McKeon, P.O. Peroneal reaction time after ankle sprain: A systematic review and meta-analysis. Med. Sci. Sports Exerc. 2014, 46, 546–556. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bullock-Saxton, J.E. Local sensation changes and altered hip muscle function following severe ankle sprain. Phys. Ther. 1994, 74, 17–28. [Google Scholar] [CrossRef] [Green Version]
- Kleinrensink, G.J.; Stoeckart, R.; Meulstee, J.; Kaulesar, S.D.; Vleeming, A.; Snijders, C.J.; van Noort, A. Lowered motor conduction velocity of the peroneal nerve after inversion trauma. Med. Sci. Sports Exerc. 1994, 26, 877–883. [Google Scholar] [CrossRef] [PubMed]
- Wilkerson, G.B.; Pinerola, J.J.; Caturano, R.W. Invertor vs. evertor peak torque and power deficiencies associated with lateral ankle ligament injury. J. Orthop. Sports Phys. Ther. 1997, 26, 78–86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Docherty, C.L.; Valovich McLeod, T.C.; Shultz, S.J. Postural Control Deficits in Participants with Functional Ankle Instability as Measured by the Balance Error Scoring System. Clin. J. Sport Med. 2006, 16, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Lynch, S.A.; Renström, P.A. Treatment of acute lateral ankle ligament rupture in the athlete. Conservative versus surgical treatment. Sports Med. 1999, 27, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Halabchi, F.; Hassabi, M. Acute ankle sprain in athletes: Clinical aspects and algorithmic approach. World J. Orthop. 2020, 11, 534–558. [Google Scholar] [CrossRef]
- Panagiotakis, E.; Mok, K.-M.; Fong, D.T.-P.; Bull, A.M.J. Biochemical analysis of ankle ligamentous sprain injury cases from televised basketball games: Understanding when, how and why ligament failure occurs. J. Sci. Med. Sport 2017, 12, 1057–1061. [Google Scholar] [CrossRef] [Green Version]
- Gulbrandsen, M.; Hartigan, D.E.; Patel, K.A.; Makovicka, J.L.; Tummala, S.V.; Chhabra, A. Ten-Year Epidemiology of Ankle Injuries in Men’s and Women’s Collegiate Soccer Players. J. Athl. Train. 2019, 54, 881–888. [Google Scholar] [CrossRef] [Green Version]
- Khasnis, A.; Gokula, R.M. Romberg’s test. J. Postgrad. Med. 2003, 49, 169–172. [Google Scholar]
- Lustenberger, T.; Talving, P.; Barmparas, G.; Schnüriger, B.; Lam, L.; Inaba, K.; Demetriades, D. Skateboard-related injuries: Not to be taken lightly. A national trauma databank analysis. J. Trauma Acute Care Surg. 2010, 69, 924–927. [Google Scholar] [CrossRef] [PubMed]
- Keilani, M.; Krall, C.; Lipowec, L.; Posch, M.; Komanadj, T.S.; Crevenna, R. Skateboarding Injuries in Vienna: Location, Frequency, and Severity. PM R 2010, 2, 619–624. [Google Scholar] [CrossRef]
- Ma, N.; Mills, S.; McBride, C.; Kimble, R.; Redmond, M. Neurological injuries from skateboards in paediatric and adolescent poulations: Injury types and severity. ANZ J. Surg. 2018, 88, 337–340. [Google Scholar] [CrossRef]
- Rodríguez-Rivadulla, A.; Saavedra-García, M.A.; Arriaza-Loureda, F. Skateboarding Injuries in Spain: A Web-Based Survey Approach. Orthop. J. Sports Med. 2020, 8, 2325967119884907. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dumas, A.; Laforest, S. Skateparks as a health-resource: Are they as dangerous as they look? Leis. Stud. 2009, 28, 19–34. [Google Scholar] [CrossRef]
- Feletti, F.; Brymer, E. Pediatric and adolescent injury in skateboarding. Res. Sports Med. 2018, 26 (Suppl. 1), 129–149. [Google Scholar] [CrossRef]
- Determan, J.J.; Frederick, E.C.; Cox, J.S.; Nevitt, M.N. High impact forces in skateboarding landings affected by landing outcome. Footwear Sci. 2010, 2, 159–170. [Google Scholar] [CrossRef]
- Winter, T.; Beck, H.; Walther, A.; Zwipp, H.; Rein, S. Influence of a proprioceptive training on functional ankle stability in young speed skaters – a prospective randomised study. J. Sports Sci. 2014, 33, 831–840. [Google Scholar] [CrossRef] [PubMed]
- Rein, S.; Fabian, T.; Zwipp, H.; Rammelt, S.; Weindel, S. Postural control and functional ankle stability in professional and amateur dancers. Clin. Neurophysiol. 2011, 122, 1602–1610. [Google Scholar] [CrossRef] [PubMed]
- Maleki, B.; Mantashloo, Z.; Salehi, S.; Abedi Yekta, A. Effect of Ankle Sprain on Postural Control and Electrical Activity of Selected Muscles after Single-Leg Jump Landing Task. Nov. Biomed. 2019, 4, 218–224. [Google Scholar]
- Shuman, K.M.; Meyers, M.C. Skateboarding injuries: An updated review. Phys. Sportsmed. 2015, 43, 317–323. [Google Scholar] [CrossRef] [PubMed]
- Graham, L.B. Skate parks as a context for adolescent development. J. Adolesc. Res. 2010, 25, 288–323. [Google Scholar]

| Professional Skateboarding Players | Amateur Skateboarding Players | |
|---|---|---|
| Age (y) Mean (SD) Range | 25.5 (±5.5) 19–36 | 20.1 (±1.6) 18–23 |
| Sex (n (%)) Male Female | 15 (93.75) 1 (6.25) | 15 (93.75) 1 (6.25) |
| Body weight (kg) Mean (SD) Range | 63.1 (±10) 48–85 | 61.4 (±8.3) 50–80 |
| Body height (cm) Mean (SD) Range | 170.8 (±7) 159–181 | 171.8 (±5.6) 157–179 |
| BMI (body mass index) Mean (SD) Range | 21.6 (±3.17) 17.6–30.12 | 20.8 (±2.31) 17–24.97 |
| Dominant foot (n (%)) Left foot Right foot | 6 (37.5) 10 (62.5) | 9 (56.25) 7 (43.75) |
| Leisure Activities involving (n (%)) | 2 (12.5) | 3 (18.75) |
| Ankle sprain (n (%)) | 9 (56.25) | 4 (25) |
| Treatment (n (%)) | 9 (100) | 1 (25) |
| Professional Skateboarding Players | Amateur Skateboarding Players | ||
|---|---|---|---|
| Supination | Dominant Foot * | 32.50° (±4.00°) | 37.25° (±7.08°) |
| Non-Dominant Foot | 35.25° (±6.14°) | 35.31° (±8.19°) | |
| Pronation | Dominant Foot | 23.56° (±6.32°) | 24.19° (±10.08°) |
| Non-Dominant Foot | 26.69° (±9.30°) | 21.44° (±7.32°) | |
| Dorsiflexion | Dominant Foot | 43.50° (±7.47°) | 43.44° (±7.52°) |
| Non-Dominant Foot | 42.00° (±7.75°) | 43.13° (±8.99°) | |
| Plantarflexion | Dominant Foot | 27.44° (±7.13°) | 31.50° (±7.70°) |
| Non-Dominant Foot | 28.00° (±6.94°) | 27.31° (±5.49°) |
| Professional Skateboarding Players | Amateur Skateboarding Players | ||
|---|---|---|---|
| Tibialis Anterior Muslce | Dominant Foot | 0.3045 s (±0.04 s) | 0.3078 s (±0.10 s) |
| Non-Dominant Foot | 0.2864 s (±0.04 s) | 0.2799 s (±0.04 s) | |
| Fibularis Longus Muscle | Dominant Foot | 0.2962 s (±0.04 s) | 0.2899 s (±0.03 s) |
| Non-Dominant Foot | 0.2793 s (±0.04 s) | 0.2810 s (±0.03 s) | |
| Fibularis Brevis Muscle | Dominant Foot | 0.2786 s (±0.03 s) | 0.2934 s (±0.04 s) |
| Non-Dominant Foot | 0.2747 s (±0.04 s) | 0.2737 s (±0.03 s) |
| Healthy Skateboarding Players | Injured Skateboarding Players | ||
|---|---|---|---|
| Tibialis Anterior Muslce | Dominant Foot | 0.2927 s (±0.03 s) | 0.3137 s (±0.05 s) |
| Non-Dominant Foot | 0.2727 s (±0.04 s) | 0.2894 s (±0.03 s) | |
| Fibularis Longus Muscle | Dominant Foot | 0.2858 s (±0.02 s) | 0.3043 s (±0.05 s) |
| Non-Dominant Foot | 0.2645 s (±0.04 s) | 0.2832 s (±0.03 s) | |
| Fibularis Brevis Muscle | Dominant Foot | 0.2749 s (±0.04 s) | 0.2814 s (±0.02 s) |
| Non-Dominant Foot | 0.2555 s (±0.04 s) | 0.2828 s (±0.03 s) |
| Professional Skateboarding Players | Amateur Skateboarding Players | ||
|---|---|---|---|
| Level 12 | Overall | 25.25 (±4.30) | 21.88 (±4.29) |
| Anterior | 29.94 (±5.92) | 29.25 (±11.96) | |
| Posterior | 29.31 (±6.72) | 28.00 (±13.65) | |
| Left | 32.50 (±9.19) | 27.31 (±9.80) | |
| Right | 30.75 (±7.00) | 26.25 (±6.70) | |
| Left Anterior | 28.13 (±7.77) | 28.31 (±8.63) | |
| Right Anterior | 30.38 (±8.04) | 24.44 (±8.25) | |
| Left Posterior | 24.88 (±7.21) | 25.63 (±11.00) | |
| Right Posterior | 26.19 (±5.72) | 21.38 (±6.42) | |
| Level 8 | Overall | 26.44 (±4.79) | 24.19 (±4.45) |
| Anterior | 32.19 (±9.47) | 29.19 (±7.51) | |
| Posterior | 32.31 (±12.76) | 32.81 (±15.65) | |
| Left | 28.13 (±8.05) | 25.81 (±8.08) | |
| Right | 29.56 (±8.49) | 26.38 (±6.11) | |
| Left Anterior | 33.88 (±9.75) | 32.25 (±8.08) | |
| Right Anterior | 33.31 (±8.77) | 30.75 (±9.01) | |
| Left Posterior | 33.31 (±8.61) | 27.88 (±7.59) | |
| Right Posterior | 27.75 (±7.13) | 26.31 (±5.65) |
| Healthy Skateboarding Players | Injured Skateboarding Players | ||
|---|---|---|---|
| Level 12 | Overall | 23.33 (±3.63) | 24.67 (±3.52) |
| Anterior | 31.00 (±13.01) | 30.50 (±7.06) | |
| Posterior | 29.17 (±14.86) | 32.83 (±15.87) | |
| Left | 27.58 (±10.06) | 28.08 (±6.99) | |
| Right | 28.17 (±6.41) | 26.83 (±4.82) | |
| Left Anterior | 31.17 (±7.69) | 33.75 (±8.13) | |
| Right Anterior | 26.92 (±7.74) | 30.92 (±7.97) | |
| Left Posterior | 28.17 (±11.09) | 28.08 (±6.46) | |
| Right Posterior | 23.58 (±5.25) | 26.00 (±5.70) | |
| Level 8 | Overall | 17.50 (±3.11) | 22.75 (±7.04) |
| Anterior | 24.00 (±6.78) | 25.25 (±8.46) | |
| Posterior | 24.50 (±9.98) | 32.75 (±17.35) | |
| Left | 26.50 (±10.41) | 19.00 (±8.04) | |
| Right | 20.50 (±3.87) | 25.00 (±9.90) | |
| Left Anterior | 19.75 (±5.06) | 27.75 (±6.95) | |
| Right Anterior | 17.00 (±4.69) | 30.25 (±13.15) | |
| Left Posterior | 18.00 (±7.07) | 27.24 (±11.59) | |
| Right Posterior | 14.75 (±5.19) | 27.25 (±6.24) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ou, Y.-K.; Chen, Z.-W.; Yeh, C.-N. Postural Control and Functional Ankle Stability in Professional and Amateur Skateboarders. Healthcare 2021, 9, 1009. https://doi.org/10.3390/healthcare9081009
Ou Y-K, Chen Z-W, Yeh C-N. Postural Control and Functional Ankle Stability in Professional and Amateur Skateboarders. Healthcare. 2021; 9(8):1009. https://doi.org/10.3390/healthcare9081009
Chicago/Turabian StyleOu, Yang-Kun, Zhi-Wei Chen, and Chien-Nan Yeh. 2021. "Postural Control and Functional Ankle Stability in Professional and Amateur Skateboarders" Healthcare 9, no. 8: 1009. https://doi.org/10.3390/healthcare9081009
APA StyleOu, Y.-K., Chen, Z.-W., & Yeh, C.-N. (2021). Postural Control and Functional Ankle Stability in Professional and Amateur Skateboarders. Healthcare, 9(8), 1009. https://doi.org/10.3390/healthcare9081009






