Analysis of Factors Relevant to Revenue Enhancement in Hernia Interventions (SwissDRG G09)
Abstract
1. Introduction
2. Materials and Methods
2.1. Statistical Analysis
2.2. Data Collection
2.3. Variables and Definition
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| Abbreviation | Meaning |
| SwissDRG 8.0 | Schweizer Diagnose Related Groups Version 8.0 |
| DRG G09 | Diagnose Related Group G09 Hernia-Interventions |
| CM4 | Result of the contribution margin calculation at position 4 |
| CHF | Swiss francs |
| EBITDA | Earnings Before Interests, Taxes, Depreciation and Amortization |
| OKP | Compulsory health insurance (“Obligatorische Krankenpflegeversicherung”); General Health Insurance |
| VVG | Insurance Contract Act (“Versicherungsvertragsgesetz”) |
| KVG | Health Insurance Act (“Krankenversicherungsgesetz”) |
| Grouper | Grouping software |
| CHOP-Code | Swiss Operation Classification Code |
| BMI | Body Mass Index |
| ASA | American Society of Anesthesiologists |
| SD | Standard deviation |
| AUC | Area under the curve |
| RS | Resident Surgeon |
| AS | Attending Surgeon (Oberarzt) |
| CSe | Chief of Services (Leitender Arzt) |
| CSu | Chief of Surgery (Chefarzt) |
| SP | Semi-privately insured |
| P | Privately insured |
| Tarmed | Tariff for outpatient medical services in Switzerland |
| TEP | Total endoscopic extraperitoneal hernioplasty procedure |
References
- Miserez, M.; Alexandre, J.H.; Campanelli, G.; Corcione, F.; Cuccurullo, D.; Pascual, M.H.; Hoeferlin, A.; Kingsnorth, A.N.; Mandala, V.; Palot, J.P.; et al. The European hernia society groin hernia classication: Simple and easy to remember. Hernia 2007, 11, 113–116. [Google Scholar] [CrossRef] [PubMed]
- Ramshorst, G.H.; HS Group. International guidelines for groin hernia management. Hernia 2018, 22, 1–165. [Google Scholar] [CrossRef]
- Ielpo, B.; Alfonsel, J.N.; Duran, H.; Diaz, E.; Fabra, I.; Caruso, R.; Malavé, L.; Ferri, V.; Barzola, E.; Quijano, Y.; et al. Cost-effectiveness of Randomized Study of Laparoscopic Versus Open Bilateral Inguinal Hernia Repair. Ann. Surg. 2018, 268, 725–730. [Google Scholar] [CrossRef] [PubMed]
- Perez, A.J.; Strassle, P.D.; Sadava, E.E.; Gaber, C.; Schlottmann, F. Nationwide Analysis of Inpatient Laparoscopic Versus Open Inguinal Hernia Repair. J. Laparoendosc. Adv. Surg. Tech. 2020, 30, 292–298. [Google Scholar] [CrossRef] [PubMed]
- Aydin, M.; Fikatas, P.; Denecke, C.; Pratschke, J.; Raakow, J. Cost analysis of inguinal hernia repair: The influence of clinical and hernia-specific factors. Hernia 2021, 1–7. [Google Scholar] [CrossRef]
- Raakow, J.; Aydin, M.; Kilian, M.; Köhler, A.; Werner, S.; Pratschke, J.; Fikatas, P. Elektive Versorgung von Leistenhernien in der Universitären Chirurgie–eine Ökonomische Herausforderung. Der Chir. 2019, 90, 1011–1018. [Google Scholar] [CrossRef] [PubMed]
- SwissDRG AG. Fallpauschalen in Schweizer Spitälern/Seite 2. Was ist SwissDRG? 2015. Available online: https://www.swissdrg.org/application/files/5115/0234/7269/170810_SwissDRG_Broschuere.pdf (accessed on 28 March 2021).
- Pricewaterhouse Coopers. Schweizer Spitäler: So Gesund Waren Die Finanzen 2019/Seite 9. Ziel EBDITAR-Marge Entfernt Sich Weiter. 2020. Available online: https://www.pwc.ch/de/publications/2021/studie-schweizer-spitaeler-2019.pdf (accessed on 28 March 2021).
- Kutz, A.; Gut, L.; Ebrahimi, F.; Wagner, U.; Schuetz, P.; Mueller, B. Association of the Swiss Diagnosis-Related Group Reimbursement System With Length of Stay, Mortality, and Readmission Rates in Hospitalized Adult Patients. JAMA Netw. Open 2019, 2, e188332. [Google Scholar] [CrossRef] [PubMed]
- Holzer, B. SwissDRG: Das Wichtigste in Kürze. Schweiz. Ärztezeitung 2012, 93, 1079–1081. [Google Scholar]
- Simons, M.P.; Aufenacker, T.; Bay-Nielsen, M.; Bouillot, J.L.; Campanelli, G.; Conze, J.; De Lange, D.; Fortelny, R.; Heikkinen, T.; Kingsnorth, A.; et al. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 2009, 13, 343–403. [Google Scholar] [CrossRef] [PubMed]
- Templ, M.; Kowarik, A.; Alfons, A.; Prantner, B. VIM: Visualization and Imputation of Missing Values. 2019. Available online: https://CRAN.R-project.org/package=VIM (accessed on 5 January 2020).
- Bursac, Z.; Gauss, C.H.; Williams, D.K.; Hosmer, D.W. Purposeful selection of variables in logistic regression. Source Code Biol. Med. 2008, 3, 17. [Google Scholar] [CrossRef] [PubMed]
- Singh, M.M.; Choudhary, P.K.; Patnaik, S.K.; Kaushal, G. Break-Even Analysis in Healthcare Setup. Int. J. Res. Found. Hosp. Healthc. Adm. 2013, 1, 29–32. [Google Scholar] [CrossRef]
- Perkins Neil, J.; Schisterman Enrique, F. The Inconsistency of “Optimal” Cut-points Using Two ROC Based Criteria. Am. J. Epidemiol. 2006, 163, 670–675. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing, 2020. Available online: https://www.gbif.org/tool/81287/r-a-language-and-environment-for-statistical-computing (accessed on 4 May 2021).
- Welker, A.; Schleppers, A.; Saathoff, H.; Mende, H. DRG-based contribution margin accounting. A useful instrument for the evaluation of reorganization measures in anaesthesiology? An orienting monocentric study. Anasthesiol. Intensivmed. 2011, 52, S534–S537. [Google Scholar]
- Vettel, U.; Hoffmann, L. Leistungsmanagment im Krankenhaus: G-Drgs. In Schritt für Schritt Erfolgreich: Planen—Gestalten—Steuern; 1. Aufl.; Springer: Berlin, Germay, 2005. [Google Scholar]
- Peter Magunia und Matthias Bünte (16.11.2020): Patientenmangel Beschert Zwei von Drei Häusern im Laufenden Jahr ein Defizit; Rolandberger: Munich, Germany, 2020.
- Hanstein, T.; Kumpe, O.; Mittelmeier, W.; Skripitz, R. Teilzementierte und unzementierte Hüftendoprothetik: Deckungsbeitrag im deutschen Fallpauschalensystem Hybrid and uncemented hip arthroplasty: Contribution margin in the German lump sum reimbursement system. Orthopade 2015, 44, 617–622. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Richter, A.; Menger, M.; Pföhler, W. Anforderungen an den chirurgischen Chefarzt aus Sicht des Trägers Requirements for leading surgeons from the viewpoint of hospital administration authorities. Chirurg 2010, 81, 701–704. [Google Scholar] [CrossRef] [PubMed]
- Franz, D.; Roeder, N. Mengendynamik in den Krankenhäusern: Auch eine gesellschaftliche Frage. Dtsch. Arztebl. Int. 2012, 109, 2580–2584. [Google Scholar]
- BFS Service AG. Die EBITDA-Marge in Krankenhäusern. Welche Bedeutung Besitzt Sie und wie ist sie zu Interpretieren?/Seite1. 2021. Available online: https://www.bfs-service.de/Branchen-News/Die-EBITDA-Marge-in-Krankenhaeusern.html (accessed on 28 March 2021).
- Zapp, W.; Oswald, J. Controlling-Instrumente für Krankenhäuser; W. Kohlhammer Verlag: Stuttgart, Germany, 2009. [Google Scholar]
- Gerginov, D. Betriebswirtschaft: Deckungsbeitrag—Definition, Unterscheidung & Berechnung. 2021. Available online: https://www.gevestor.de/details/deckungsbeitrag-668940.html (accessed on 14 April 2021).
- Geldner, G.; Eberhart, L.H.J.; Trunk, S.; Dahmen, K.G.; Reissmann, T.; Weiler, T.; Bach, A. Effizientes OP-Management Vorschläge zur Optimierung von Prozessabläufen als Grundlage für die Erstellung eines OP-Statuts. Anaesthesist 2002, 51, 760–767. [Google Scholar] [CrossRef] [PubMed]
- Handbuch zur Kalkulation von Behandlungskosten Version 4.0–10: Kapitel 4.2 Personalkostenverrechnung; Deutsche Krankenhaus Verlagsgesellschaft mbH Düsseldorf: Düsseldorf, Germany, 2016; pp. 32–41.
- PricewaterhouseCoopers. Ambulant vor Stationär. Oder Wie Sich eine Milliarde Franken jährlich einsparen lassen/Seite13. 2016. Available online: https://www.pwc.ch/de/publications/2016/ambulant_vor_stationaer_de_16_web_final.pdf (accessed on 7 April 2021).
- Wirth, U.; Saller, M.L.; von Ahnen, T.; Köckerling, F.; Schardey, H.M.; Schopf, S. Ambulanter transabdomineller präperitonealer Leistenhernienverschluss (TAPP)—Um welchen Preis? Inguinal hernia repair in TAPP technique in a day-case surgery setting—At what price? Chirurg 2017, 88, 792–798. [Google Scholar] [CrossRef] [PubMed]


| Variable | Definition | Formula/Categories |
|---|---|---|
| Age | Patient’s age | Date of operation–patient’s date of birth |
| Sex | Male/female/divers | |
| BMI | Body Mass Index | Patient weight (kg)/(Patient height (cm))2 |
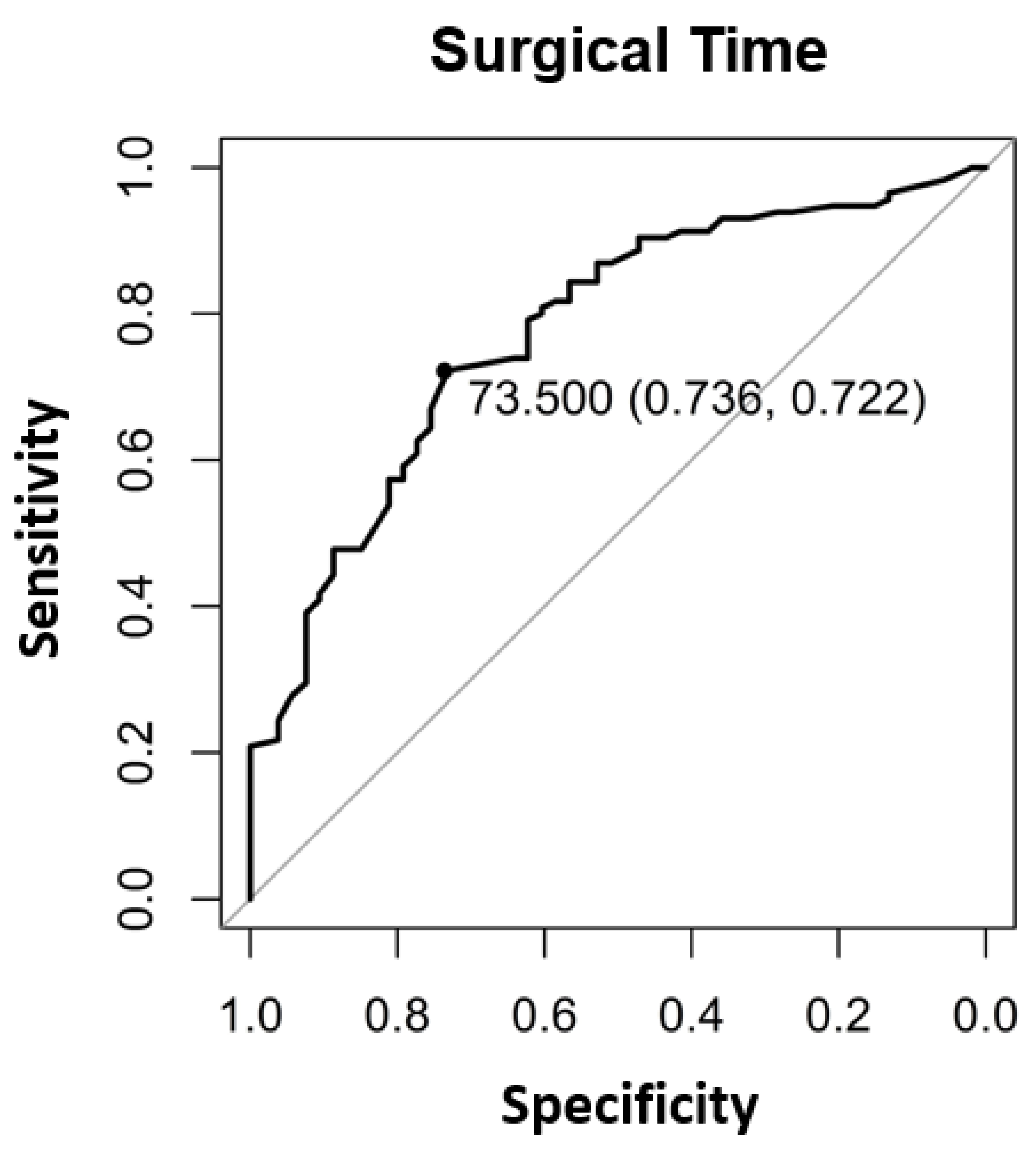
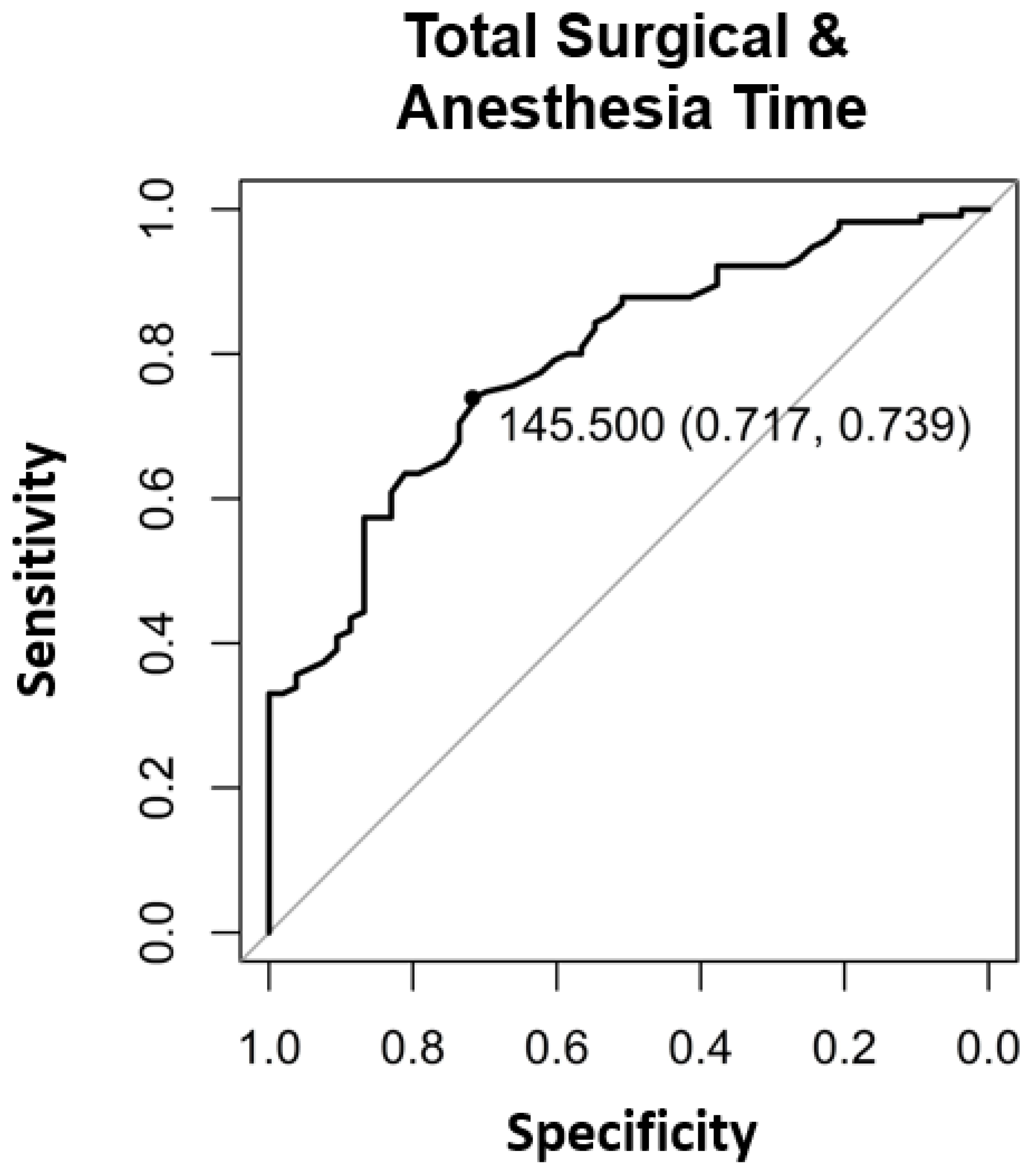
| Surgical Time | Period from first surgical cut to final surgical suture | Timepoint (final suture)–timepoint (first surgical cut) |
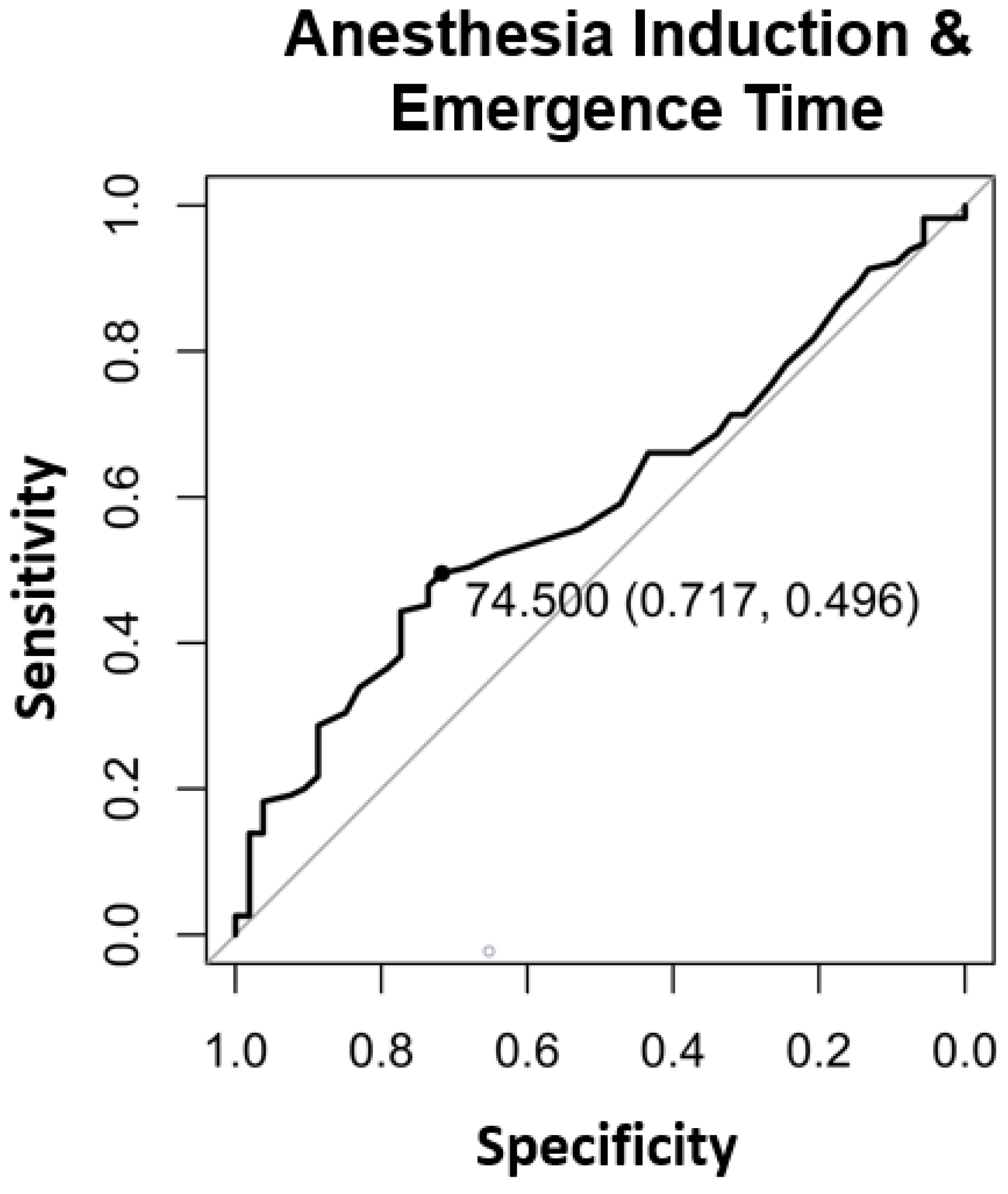
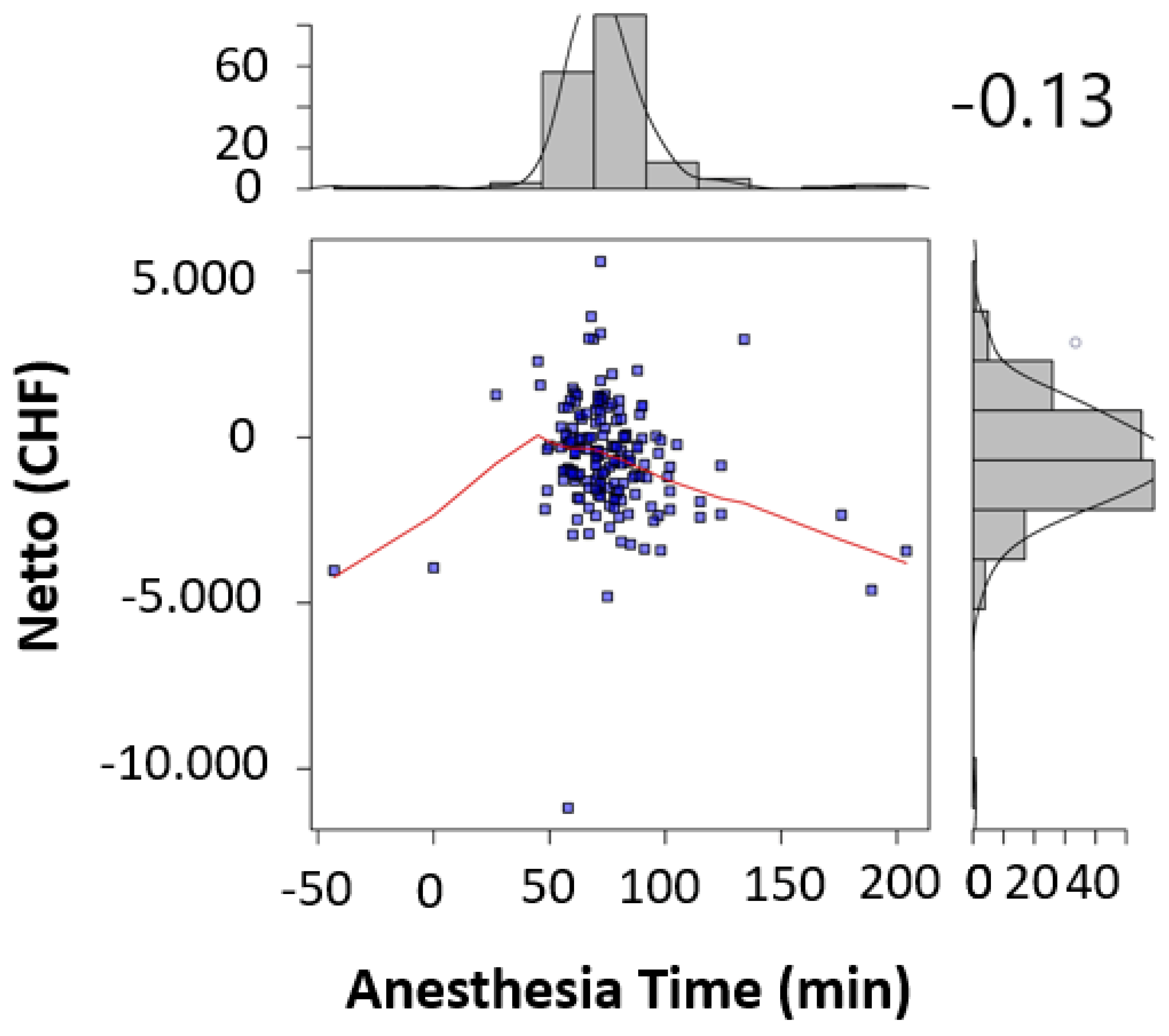
| Total Anesthesia Time | Sum of induction time and emergence time as reported by the anesthesiologist | Induction time + Emergence time |
| ASA-Classification | as defined by the American society of Anesthesiologists | I, II, III, IV, V, VI |
| Teaching operation | Procedures conducted by or under assistance of residents are considered a teaching operation |
|
| Insurance status | Coverage status of patient’s procedure by one of the health care providers shown in the following box |
|
| Number of surgeons | Number of surgeons present during the procedure | Numerical value |
| Unilateral or bilateral operations |
| |
| Experience level of the attending operators | Operator’s experience defined by his/her position within the department |
|
| Additional procedures | Any additional procedures performed during hernia repair surgery |
| Parameter | Overall | No Loss | Loss | p |
|---|---|---|---|---|
| Patients (n) | 168 | 53 | 115 | |
| Age (mean/SD) | 61.73 (15.82) | 63.02 (16.91) | 61.13 (15.33) | 0.474 |
| Sex = Male | 147 (87.5) | 45 (84.9) | 102 (88.7) | 0.660 |
| BMI (mean/SD) | 25.09 (3.48) | 25.06 (3.69) | 25.11 (3.40) | 0.939 |
| ASA (mean/SD) | 2.12 (0.70) | 2.00 (0.71) | 2.18 (0.70) | 0.118 |
| Prior Surgery | 16 (9.5) | 4 (7.5) | 12 (10.4) | 0.757 |
| Insurance-Status | <0.001 * | |||
| General—(OKP) | 150 (89.3) | 40 (75.5) | 110 (95.7) | |
| Supplementary —Semi-private (SP) | 14 (8.3) | 9 (17.0) | 5 (4.3) | |
| Supplementary —Private (P) | 4 (2.4) | 4 (7.5) | 0 (0.0) | |
| Bilateral TEP Procedure | 115 (68.5) | 37 (69.8) | 78 (67.8) | 0.937 |
| Lichtenstein Procedure | 35 (20.2) | 4 (7.5) | 31 (26.1) | 0.010 * |
| Additional Procedures | 18 (10.7) | 4 (7.5) | 14 (12.2) | 0.527 |
| Teaching-Operation | 32 (19.0) | 3 (5.7) | 29 (25.2) | 0.005 * |
| Qualification of Surgeon | 0.214 | |||
| Resident Surgeon (RS) | 6 (3.6) | 1 (1.9) | 5 (4.3) | |
| Attending Surgeon (AS) | 66 (39.3) | 16 (30.2) | 50 (43.5) | |
| Chief of Service (CSe) | 95 (56.5) | 36 (67.9) | 59 (51.3) | |
| Chief of Surgery (CSu) | 1 (0.6) | 0 (0.0) | 1 (0.9) | |
| Number of Surgeons | 2.10 (0.39) | 2.00 (0.28) | 2.15 (0.42) | 0.022 * |
| Length of Hospital Stay | 2.13 (1.05) | 2.11 (0.58) | 2.14 (1.21) | 0.883 |
| Complication | 7 (4.2) | 0 (0.0) | 7 (6.1) | 0.156 |
| Surgical time | 80.47 (32.14) | 60.49 (22.82) | 89.68 (31.69) | <0.001 * |
| Total Anesthesia Time | 75.01 (24.39) | 70.55 (15.09) | 77.06 (27.46) | 0.108 |
| Surgical and Anesthesia Time | 155.48 (36.98) | 131.04 (26.96) | 166.74 (35.59) | <0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Enodien, B.; Taha-Mehlitz, S.; Bachmann, M.; Staartjes, V.E.; Gripp, M.; Staudner, T.; Taha, A.; Frey, D. Analysis of Factors Relevant to Revenue Enhancement in Hernia Interventions (SwissDRG G09). Healthcare 2021, 9, 862. https://doi.org/10.3390/healthcare9070862
Enodien B, Taha-Mehlitz S, Bachmann M, Staartjes VE, Gripp M, Staudner T, Taha A, Frey D. Analysis of Factors Relevant to Revenue Enhancement in Hernia Interventions (SwissDRG G09). Healthcare. 2021; 9(7):862. https://doi.org/10.3390/healthcare9070862
Chicago/Turabian StyleEnodien, Bassey, Stephanie Taha-Mehlitz, Marta Bachmann, Victor E. Staartjes, Maike Gripp, Tobias Staudner, Anas Taha, and Daniel Frey. 2021. "Analysis of Factors Relevant to Revenue Enhancement in Hernia Interventions (SwissDRG G09)" Healthcare 9, no. 7: 862. https://doi.org/10.3390/healthcare9070862
APA StyleEnodien, B., Taha-Mehlitz, S., Bachmann, M., Staartjes, V. E., Gripp, M., Staudner, T., Taha, A., & Frey, D. (2021). Analysis of Factors Relevant to Revenue Enhancement in Hernia Interventions (SwissDRG G09). Healthcare, 9(7), 862. https://doi.org/10.3390/healthcare9070862






