Pharmacist Workforce at Primary Care Clinics: A Nationwide Survey in Taiwan
Abstract
1. Introduction
2. Materials and Methods
2.1. Background
2.2. Data Source
2.3. Study Design
2.4. Statistical Analysis
2.5. Ethical Approval
3. Results
3.1. Distribution of Pharmacies and Pharmacists Workforce in Urban, Suburban, and Rural Areas
3.2. Distribution of the Nationwide Pharmacist Workforce at Clinics, Stratified by Number of Physicians Per Clinic
3.3. Distribution of Pharmacist Workforce in Different Specialties Clinics
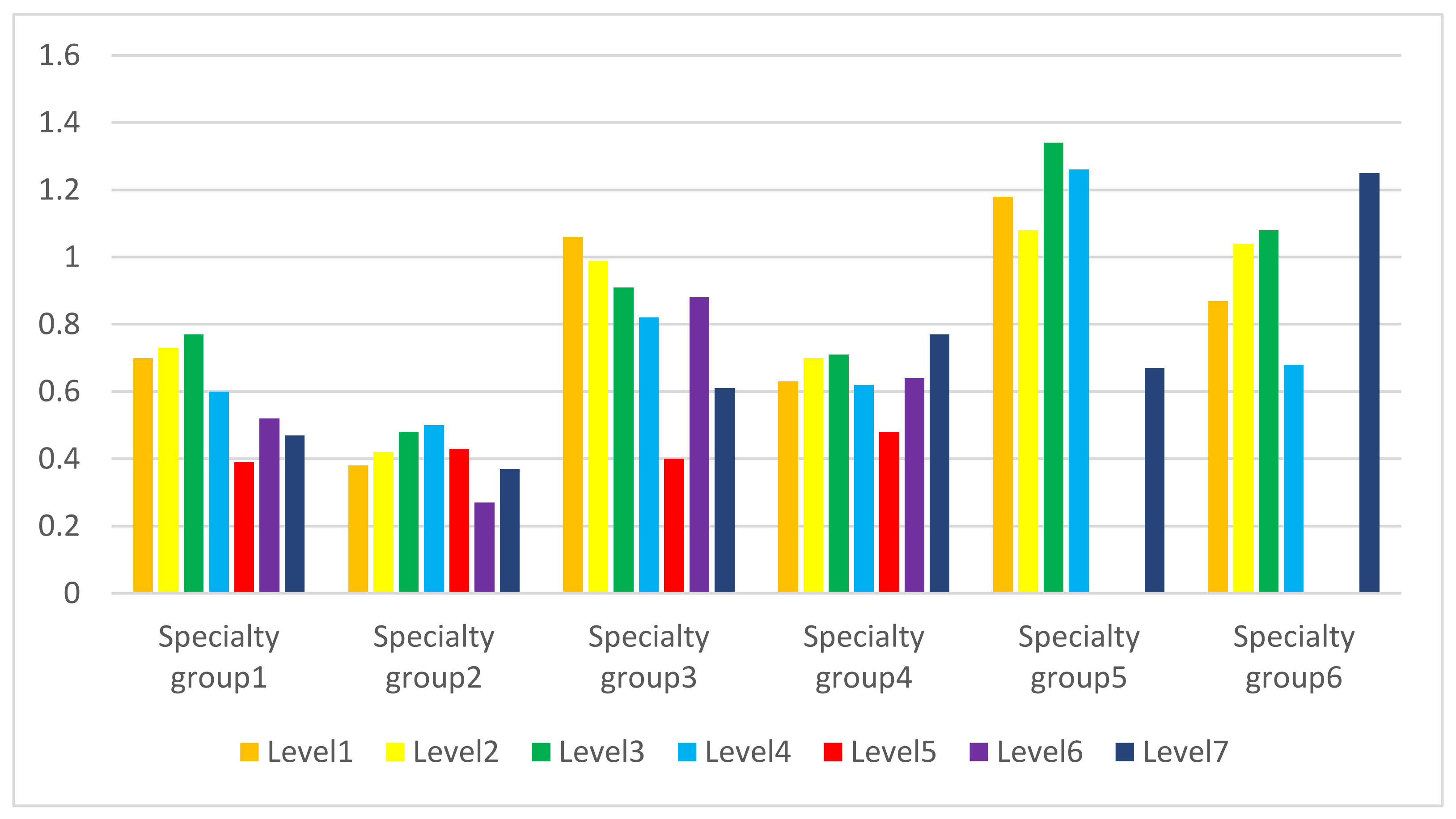
3.4. The Average Number of Pharmacists at Clinics by Urbanization Level and Specialty Group
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Urbanization Level | |||||||
|---|---|---|---|---|---|---|---|
| Level 1 | Level 2 | Level 3 | Level 4 | Level 5 | Level 6 | Level 7 | |
| * Specialty group 1 | 0.70 ± 0.04 | 0.73 ± 0.03 | 0.77 ± 0.04 | 0.60 ± 0.05 | 0.39 ± 0.12 | 0.52 ± 0.09 | 0.47 ± 0.08 |
| Specialty group 2 | 0.38 ± 0.03 | 0.42 ± 0.03 | 0.48 ± 0.06 | 0.50 ± 0.07 | 0.43 ± 0.31 | 0.27 ± 0.25 | 0.37 ± 0.19 |
| Specialty group 3 | 1.06 ± 0.03 | 0.99 ± 0.03 | 0.91 ± 0.04 | 0.82 ± 0.05 | 0.40 ± 0.37 | 0.88 ± 0.17 | 0.61 ± 0.14 |
| Specialty group 4 | 0.63 ± 0.02 | 0.70 ± 0.02 | 0.71 ± 0.03 | 0.62 ± 0.03 | 0.48 ± 0.09 | 0.64 ± 0.06 | 0.77 ± 0.06 |
| Specialty group 5 | 1.18 ± 0.06 | 1.08 ± 0.06 | 1.34 ± 0.12 | 1.26 ± 0.13 | N/A ** | N/A | 0.67 ± 0.48 |
| Specialty group 6 | 0.87 ± 0.08 | 1.04 ± 0.08 | 1.08 ± 0.14 | 0.68 ± 0.18 | N/A | N/A | 1.25 ± 0.41 |
References
- Yokoi, M.; Tashiro, T. Influence of the separation of prescription and dispensation of medicine on its cost in Japanese prefectures. Glob. J. Health Sci. 2014, 6, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Kwon, S. Pharmaceutical reform and physician strikes in Korea: Separation of drug prescribing and dispensing. Soc. Sci. Med. 2003, 57, 529–538. [Google Scholar] [CrossRef]
- Tiong, J.J.; Mai, C.W.; Gan, P.W.; Johnson, J.; Mak, V.S. Separation of prescribing and dispensing in Malaysia: The history and challenges. The International journal of pharmacy practice. Int. J. Pharm. Pract. 2016, 24, 302–305. [Google Scholar] [CrossRef] [PubMed]
- Rodwin, M.A.; Okamoto, A. Physicians’ conflicts of interest in Japan and the United States: Lessons for the United States. J. Health Polit. Policy Law 2000, 25, 343–375. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.-L. Discussion on the Restrictions and Possibilities of Social Practice of Separation Policy. Available online: https://www.rchss.sinica.edu.tw/app/ebook/journal/23-04-2011/4.pdf (accessed on 1 December 2020). (In Chinese)
- Law and Regulation Database of The Republic of China. Available online: https://law.moj.gov.tw/LawClass/LawSingleRela.aspx?PCODE=L0030002&FLNO=50&ty=L (accessed on 1 December 2020). (In Chinese)
- Chou, Y.J.; Yip, W.C.; Lee, C.H.; Huang, N.; Sun, Y.P.; Chang, H.J. Impact of separating drug prescribing and dispensing on provider behaviour: Taiwan’s experience. Health Policy Plan. 2003, 18, 316–329. [Google Scholar] [CrossRef]
- Yamamura, S.; Yamamoto, N.; Oide, S.; Kitazawa, S. Current state of community pharmacy in Japan: Practice, research, and future opportunities or challenges. Ann. Pharmacother. 2006, 40, 2008–2014. [Google Scholar] [CrossRef]
- National Health Insurance Administration; Ministry of Health and Welfare. The Coverage Rate of National Health Insurance. 2019. Available online: https://www.nhi.gov.tw/Content_List.aspx?n=4DAAA0A111B2378D&topn=23C660CAACAA159D (accessed on 1 December 2020).
- Taiwan Opening Data Government. Medical Institutions and Basic Information. Available online: https://data.gov.tw/ (accessed on 1 December 2020).
- Taiwan Ministry of the Interior. Monthly Bulletin of Interior Statistics.1.7—Population for Township and District and by Urban Area. Available online: https://www.moi.gov.tw/files/site_stuff/321/1/month/month_en.html (accessed on 1 December 2020).
- Taiwan Ministry of Health and Welfare. Annual Statistical Table. Available online: https://dep.mohw.gov.tw/DOS/lp-4934-113-1-20.html (accessed on 1 December 2020).
- Taiwan Ministry of Health and Welfare. Pharmaceutical Administration-Number of Pharmaceutical Merchants in Each County and City-By Township and City. Available online: https://dep.mohw.gov.tw/DOS/cp-1729-2940-113.html (accessed on 1 December 2020).
- Liu, C.Y.; Hung, Y.T.; Chuang, Y.L.; Chen, Y.J.; Weng, W.S.; Liu, J.S. Incorporating development stratification of Taiwan townships into sampling design of large scale health interview survey. J. Health Manag. 2006, 4, 1–22. [Google Scholar]
- Taylor, S.M.; Lindsay, D.; Glass, B.D. Rural pharmacy workforce: Influence of curriculum and clinical placement on pharmacists’ choice of rural practice. Aust. J. Rural Health 2019, 27, 132–138. [Google Scholar] [CrossRef]
- Martin, S.L.; Baker, R.P.; Piper, B.J. Evaluation of urban-rural differences in pharmacy practice needs in Maine with the MaPPNA. Pharm. Pract. 2015, 13, 669. [Google Scholar] [CrossRef]
- Soon, J.A.; Levine, M. Rural pharmacy in Canada: Pharmacist training, workforce capacity and research partnerships. Int. J. Circumpolar Health 2011, 70, 407–418. [Google Scholar] [CrossRef]
- Faraco, E.B.; Guimarães, L.; Anderson, C.; Leite, S.N. The pharmacy workforce in public primary healthcare centers: Promoting access and information on medicines. Pharm. Pract. 2020, 18, 2048. [Google Scholar] [CrossRef]
- Nattinger, M.; Ullrich, F.; Mueller, K.J. Characteristics of rural communities with a sole, independently owned pharmacy. Rural Policy Brief 2014, 7, 1–4. [Google Scholar]
- Bono, J.D.; Crawford, S.Y. Impact of Medicare Part D on independent and chain community pharmacies in rural Illinois--A qualitative study. Res. Soc. Adm. Pharm. 2010, 6, 110–120. [Google Scholar] [CrossRef]
- Stratton, T.P. The economic realities of rural pharmacy practice. J. Rural Health 2001, 17, 77–81. [Google Scholar] [CrossRef]
- Walton, S.M. The pharmacist shortage and medication errors: Issues and evidence. J. Med. Syst. 2004, 28, 63–69. [Google Scholar] [CrossRef]
- Young, D. Shortage of pharmacists may have contributed to patient’s death. Am. J. Health Syst. Pharm. 2002, 59, 2042–2045. [Google Scholar] [CrossRef]
- Health Care Resources: Pharmacists. Available online: https://stats.oecd.org/index.aspx?queryid=30178# (accessed on 26 January 2021).
- Taiwan Ministry of Health and Welfare. Available online: https://dep.mohw.gov.tw/dos/cp-1735-3245-113.html (accessed on 26 January 2021). (In Chinese)
- Rollins, B.L.; Gunturi, R.; Sullivan, D. A pharmacy business management simulation exercise as a practical application of business management material and principles. Am. J. Pharm. Educ. 2014, 78, 62. [Google Scholar] [CrossRef]
- Davies, M.J.; Fleming, H.; Jones, R.; Menzie, K.; Smallwood, C.; Surendar, S. The inclusion of a business management module within the master of pharmacy degree: A route to asset enrichment? Pharm. Pract. 2013, 11, 109–117. [Google Scholar] [CrossRef]
- Mattingly, T.J.; Mullins, C.D.; Melendez, D.R.; Boyden, K.; Eddington, N.D. A systematic review of entrepreneurship in pharmacy practice and education. Am. J. Pharm. Educ. 2019, 83, 7233. [Google Scholar] [CrossRef]
- Lin, H.C.; Chen, C.S.; Liu, T.C.; Lee, H.C. Differences in practice income between solo and group practice physicians. Health Policy 2006, 79, 296–305. [Google Scholar] [CrossRef]
- Bureau of National Health Insurance. Available online: https://www.nhi.gov.tw/Content_List.aspx?n=58ED9C8D8417D00B (accessed on 1 December 2020).
- Investigation Bureau, Ministry of Justice in Taiwan. Available online: https://www.moj.gov.tw/2204/2795/2796/54190/ (accessed on 26 January 2021).
- Chen, T.H.; Hsu, M.M. Disputes about the program of handling next-door pharmacies. Taiwan Med. J. 2005, 48, 549–550. (In Chinese) [Google Scholar]
- Explanation of Law of Dispensing Medicine, Judicial Yuan in Taiwan. Available online: https://www.president.gov.tw/File/Doc/7b219027-bd5a-448c-9294-1de3c0036265 (accessed on 26 January 2021). (In Chinese)
- Willing of Clinic Physicians to Approve Prescription Refills for Chronic Disease. Available online: https://www.asia.edu.tw/Main_pages/academics/teacher_research/pk_kung/10.pdf (accessed on 26 January 2021). (In Chinese).
- Practicing Physicians’ Views on the Implementation of Separation Policy in the Future. Available online: https://www.chimei.org.tw/main/cmh_department/57726/08/data/II-11.pdf (accessed on 26 January 2021). (In Chinese).
- Brathwaite, D.; Aziz, F.; Eakins, C.; Charles, A.J.; Cristian, A. Safety precautions in the rehabilitation medicine prescription. Phys. Med. Rehabil. Clin. N. Am. 2012, 23, 231–239. [Google Scholar] [CrossRef] [PubMed]
- What is Rehabilitation? Available online: https://www.who.int/news-room/fact-sheets/detail/rehabilitation (accessed on 26 January 2021).
- Bicket, M.C.; Brat, G.A.; Hutfless, S.; Wu, C.L.; Nesbit, S.A.; Alexander, G.C. Optimizing opioid prescribing and pain treatment for surgery: Review and conceptual framework. Am. J. Health Syst. Pharm. 2019, 76, 1403–1412. [Google Scholar] [CrossRef] [PubMed]
- Kukreja, S.; Kalra, G.; Shah, N.; Shrivastava, A. Polypharmacy in psychiatry: A review. Mens Sana Monogr. 2013, 11, 82–99. [Google Scholar] [CrossRef]
- Tarn, D.M.; Schwartz, J.B. Polypharmacy: A five-step call to action for family physicians. Fam. Med. 2020, 52, 699–701. [Google Scholar] [CrossRef]
- Masnoon, N.; Shakib, S.; Kalisch-Ellett, L.; Caughey, G.E. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017, 17, 230. [Google Scholar] [CrossRef]
- Mojtabai, R.; Olfson, M. National trends in psychotropic medication polypharmacy in office-based psychiatry. Arch. Gen. Psychiatry 2010, 67, 26–36. [Google Scholar] [CrossRef]
- Chou, Y.C.; Lin, S.Y.; Chen, T.J.; Chiang, S.C.; Jeng, M.J.; Chou, L.F. Dosing variability in prescriptions of acetaminophen to children: Comparisons between pediatricians, family physicians and otolaryngologists. BMC Pediatr. 2013, 13, 64. [Google Scholar] [CrossRef][Green Version]

| Urbanization Level | No. of Townships | No. of Pharmacists * | No. of Pharmacies | No. of Clinics | % of Clinics with Pharmacists | No. of Pharmacists in Clinics |
|---|---|---|---|---|---|---|
| Urban | ||||||
| Level 1 | 27 | 10,872 | 1988 | 3526 | 50.5 | 2660 |
| Level 2 | 43 | 12,659 | 2599 | 3998 | 53.4 | 3147 |
| Suburban | ||||||
| Level 3 | 56 | 5451 | 1696 | 1780 | 54.2 | 1424 |
| Level 4 | 88 | 4561 | 1248 | 1478 | 51.0 | 1011 |
| Rural | ||||||
| Level 5 | 35 | 236 | 104 | 135 | 43.0 | 62 |
| Level 6 | 61 | 661 | 266 | 295 | 51.9 | 162 |
| Level 7 | 49 | 818 | 318 | 334 | 53.0 | 222 |
| Total | 359 | 35258 | 8219 | 11546 | 52.1 | 8688 |
| Specialty | Number of Clinics | % of Clinics with Pharmacists | |||||
|---|---|---|---|---|---|---|---|
| 0 Pharmacist/Clinic | 1 Pharmacists/Clinic | 2 Pharmacists/Clinic | 3 Pharmacists/Clinic | ≥4 Pharmacists/Clinic | Total | ||
| Single-specialty clinics | 4857 | 3445 | 1504 | 212 | 35 | 10,053 | 51.7 |
| Practices without specialist title | 1558 | 1057 | 282 | 32 | 3 | 2932 | 46.9 |
| General medicine | 566 | 371 | 133 | 11 | 0 | 1081 | 47.6 |
| Family medicine | 493 | 391 | 158 | 27 | 3 | 1072 | 54.0 |
| Otolaryngology | 388 | 298 | 263 | 42 | 5 | 996 | 61.0 |
| Pediatrics | 317 | 344 | 211 | 31 | 5 | 908 | 65.1 |
| Ophthalmology | 232 | 286 | 164 | 20 | 3 | 705 | 67.1 |
| Obstetrics and gynecology | 251 | 218 | 62 | 2 | 2 | 535 | 53.1 |
| Dermatology | 150 | 133 | 126 | 26 | 12 | 447 | 66.4 |
| Rehabilitation | 278 | 31 | 3 | 0 | 0 | 312 | 10.9 |
| Psychiatry | 88 | 132 | 50 | 11 | 1 | 282 | 68.8 |
| General surgery | 160 | 74 | 13 | 0 | 1 | 248 | 35.5 |
| Plastic surgery | 209 | 11 | 0 | 0 | 0 | 220 | 5.0 |
| Orthopedics | 114 | 55 | 25 | 7 | 0 | 201 | 43.3 |
| Others | 53 | 44 | 14 | 3 | 0 | 114 | 53.5 |
| Multi-specialty clinics | 668 | 545 | 217 | 50 | 13 | 1493 | 55.3 |
| All clinics | 5525 | 3990 | 1721 | 262 | 48 | 11,546 | 52.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, W.-H.; Lee, P.-C.; Chiang, S.-C.; Chang, Y.-L.; Chen, T.-J.; Chou, L.-F.; Hwang, S.-J. Pharmacist Workforce at Primary Care Clinics: A Nationwide Survey in Taiwan. Healthcare 2021, 9, 863. https://doi.org/10.3390/healthcare9070863
Chen W-H, Lee P-C, Chiang S-C, Chang Y-L, Chen T-J, Chou L-F, Hwang S-J. Pharmacist Workforce at Primary Care Clinics: A Nationwide Survey in Taiwan. Healthcare. 2021; 9(7):863. https://doi.org/10.3390/healthcare9070863
Chicago/Turabian StyleChen, Wei-Ho, Pei-Chen Lee, Shu-Chiung Chiang, Yuh-Lih Chang, Tzeng-Ji Chen, Li-Fang Chou, and Shinn-Jang Hwang. 2021. "Pharmacist Workforce at Primary Care Clinics: A Nationwide Survey in Taiwan" Healthcare 9, no. 7: 863. https://doi.org/10.3390/healthcare9070863
APA StyleChen, W.-H., Lee, P.-C., Chiang, S.-C., Chang, Y.-L., Chen, T.-J., Chou, L.-F., & Hwang, S.-J. (2021). Pharmacist Workforce at Primary Care Clinics: A Nationwide Survey in Taiwan. Healthcare, 9(7), 863. https://doi.org/10.3390/healthcare9070863







