The Relationship between Scapular Upward Rotation and Shoulder Internal and External Rotation Isokinetic Strength in Professional Baseball Pitchers
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Measurement
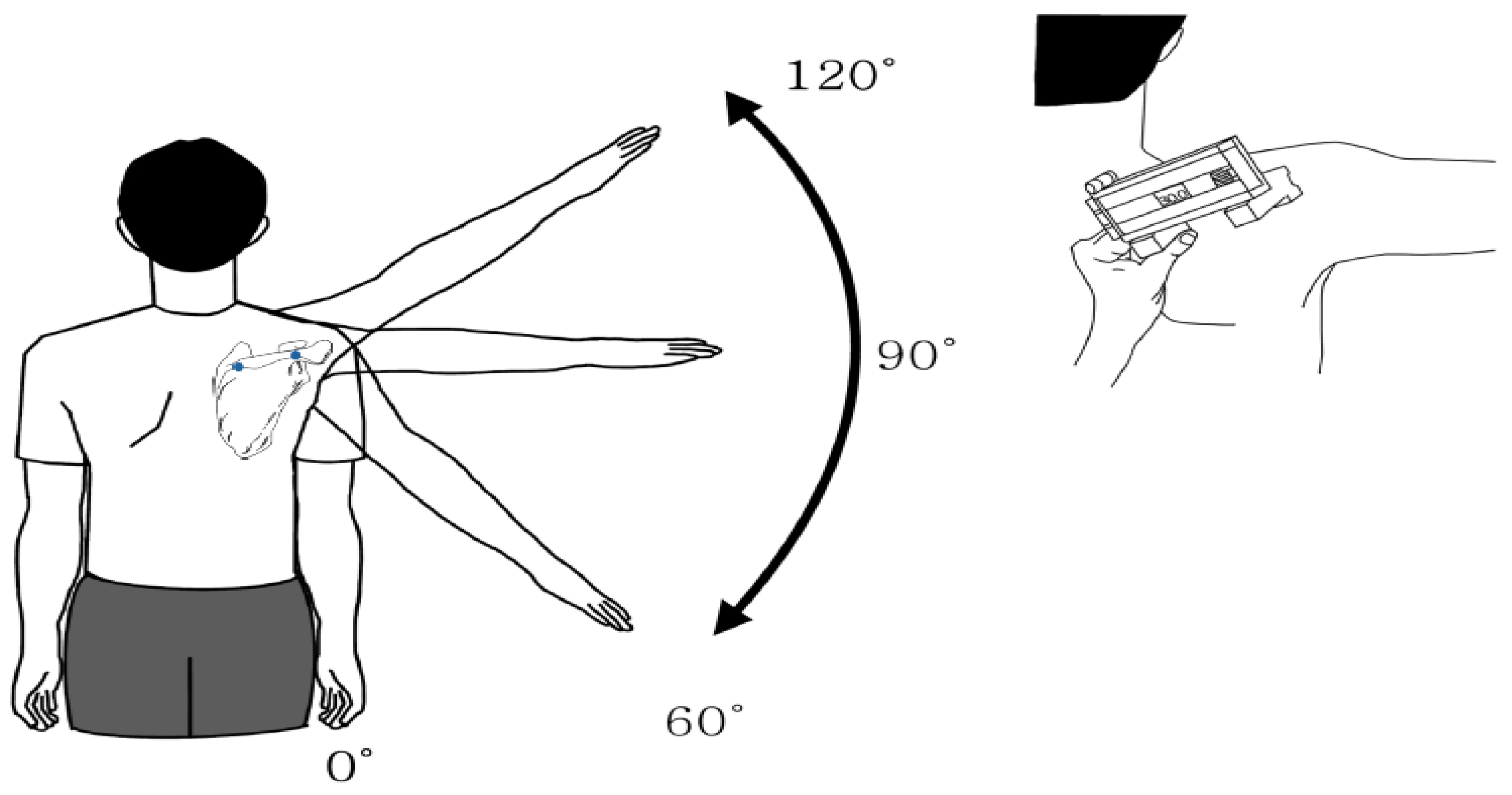
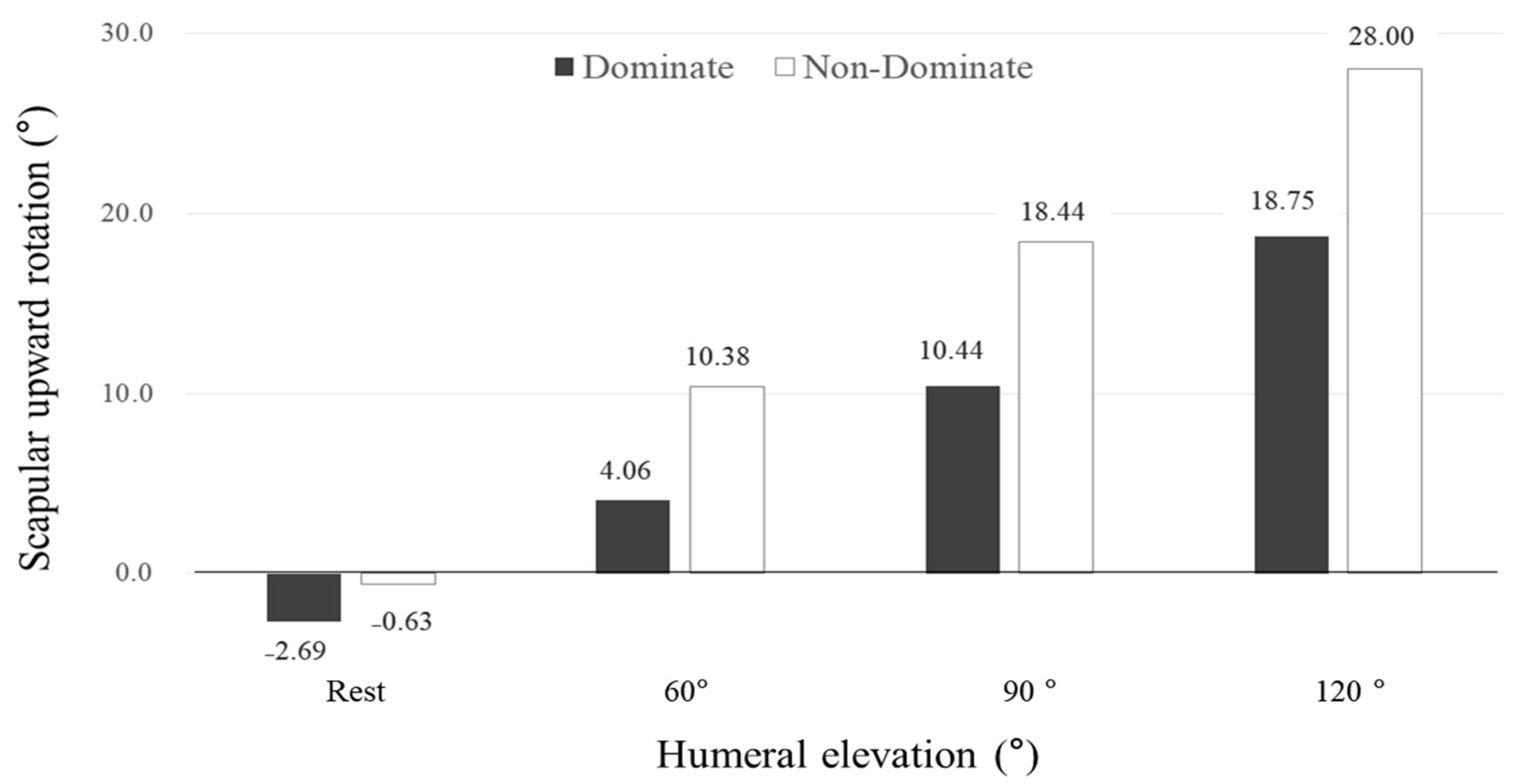
2.2.1. Scapular Upward Rotation
2.2.2. Shoulder Isokinetic Strength
2.3. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kibler, W.B. The role of the scapula in athletic shoulder function. Am. J. Sports Med. 1998, 26, 325–337. [Google Scholar] [CrossRef] [PubMed]
- Karduna, A.R.; McClure, P.W.; Michener, L.A. Scapular kinematics: Effects of altering the Euler angle sequence of rotations. J. Biomech. 2000, 33, 1063–1068. [Google Scholar] [CrossRef]
- Neumann, D.A. Kinesiology of the Musculoskeletal System-E-Book: Foundations For Rehabilitation; Elsevier Health Sciences: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Fayad, F.; Roby-Brami, A.; Yazbeck, C.; Hanneton, S.; Lefevre-Colau, M.M.; Gautheron, V.; Poiraudeau, S.; Revel, M. Three-dimensional scapular kinematics and scapulohumeral rhythm in patients with glenohumeral osteoarthritis or frozen shoulder. J. Biomech. 2008, 41, 326–332. [Google Scholar] [CrossRef]
- Rubin, B.D.; Kibler, W.B. Fundamental principles of shoulder rehabilitation: Conservative to postoperative management. Arthrosc. J. Arthrosc. Relat. Surg. 2002, 18, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Ludewig, P.M.; Reynolds, J.F. The association of scapular kinematics and glenohumeral joint pathologies. J. Orthop. Sports Phys. Ther. 2009, 39, 90–104. [Google Scholar] [CrossRef]
- Pellegrini, A.; Tonino, P.; Paladini, P.; Cutti, A.; Ceccarelli, F.; Porcellini, G. Motion analysis assessment of alterations in the scapulo-humeral rhythm after throwing in baseball pitchers. Musculoskelet. Surg. 2013, 97, 9–13. [Google Scholar] [CrossRef]
- Rich, R.L.; Struminger, A.H.; Tucker, W.S.; Munkasy, B.A.; Joyner, A.B.; Buckley, T.A. Scapular Upward-Rotation Deficits After Acute Fatigue in Tennis Players. J. Athl. Train. 2016, 51, 474–479. [Google Scholar] [CrossRef] [PubMed]
- Downar, J.M.; Sauers, E.L. Clinical Measures of Shoulder Mobility in the Professional Baseball Player. J. Athl. Train. 2005, 40, 23–29. [Google Scholar]
- Laudner, K.G.; Stanek, J.M.; Meister, K. Differences in scapular upward rotation between baseball pitchers and position players. Am. J. Sports Med. 2007, 35, 2091–2095. [Google Scholar] [CrossRef]
- Timmons, M.K.; Thigpen, C.A.; Seitz, A.L.; Karduna, A.R.; Arnold, B.L.; Michener, L.A. Scapular kinematics and subacromial-impingement syndrome: A meta-analysis. J. Sport Rehabil. 2012, 21, 354–370. [Google Scholar] [CrossRef]
- Struyf, F.; Nijs, J.; Baeyens, J.P.; Mottram, S.; Meeusen, R. Scapular positioning and movement in unimpaired shoulders, shoulder impingement syndrome, and glenohumeral instability. Scand. J. Med. Sci. Sports 2011, 21, 352–358. [Google Scholar] [CrossRef]
- Contemori, S.; Panichi, R.; Biscarini, A. Effects of scapular retraction/protraction position and scapular elevation on shoulder girdle muscle activity during glenohumeral abduction. Hum. Mov. Sci. 2019, 64, 55–66. [Google Scholar] [CrossRef]
- Ekstrom, R.A.; Bifulco, K.M.; Lopau, C.J.; Andersen, C.F.; Gough, J.R. Comparing the function of the upper and lower parts of the serratus anterior muscle using surface electromyography. J. Orthop. Sports Phys. Ther. 2004, 34, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Ludewig, P.M.; Cook, T.M. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys. Ther. 2000, 80, 276–291. [Google Scholar] [CrossRef] [PubMed]
- Johnson, G.; Bogduk, N.; Nowitzke, A.; House, D. Anatomy and actions of the trapezius muscle. Clin. Biomech. 1994, 9, 44–50. [Google Scholar] [CrossRef]
- Phadke, V.; Camargo, P.; Ludewig, P. Scapular and rotator cuff muscle activity during arm elevation: A review of normal function and alterations with shoulder impingement. Rev. Bras. Fisioter. 2009, 13, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Ellenbecker, T.S.; Davies, G.J. The application of isokinetics in testing and rehabilitation of the shoulder complex. J. Athl. Train. 2000, 35, 338–350. [Google Scholar]
- Huang, T.-S.; Lin, J.-J.; Ou, H.-L.; Chen, Y.-T. Movement Pattern of Scapular Dyskinesis in Symptomatic Overhead Athletes. Sci. Rep. 2017, 7, 6621. [Google Scholar] [CrossRef]
- Barcia, A.M.; Makovicka, J.L. Scapular Motion in the Presence of Rotator Cuff Tears: A Systematic Review. J. Shoulder Elb. Surg. 2021. [Google Scholar] [CrossRef]
- Kim, B.-G.; Yoon, W.-Y.; Oh, J.-K. The effect of game participation of a professional baseball pitcher on GIRD, scapulohumeral rhythm. Int. Conf. Converg. Technol. 2014, 4, 662–663. [Google Scholar]
- Laudner, K.G.; Stanek, J.M.; Meister, K. Assessing posterior shoulder contracture: The reliability and validity of measuring glenohumeral joint horizontal adduction. J. Athl. Train. 2006, 41, 375. [Google Scholar] [PubMed]
- Johnson, M.P.; McClure, P.W.; Karduna, A.R. New method to assess scapular upward rotation in subjects with shoulder pathology. J. Orthop. Sports Phys. Ther. 2001, 31, 81–89. [Google Scholar] [CrossRef]
- Tucker, W.S.; Ingram, R.L. Reliability and validity of measuring scapular upward rotation using an electrical inclinometer. J. Electromyogr. Kinesiol. 2012, 22, 419–423. [Google Scholar] [CrossRef] [PubMed]
- Wilkin, L.D.; Haddock, B.L. Isokinetic strength of collegiate baseball pitchers during a season. J. Strength Cond. Res. 2006, 20, 829–832. [Google Scholar] [PubMed]
- Ellenbecker, T.S.; Mattalino, A.J. Concentric Isokinetic Shoulder Internal and External Rotation Strength in Professional Baseball Pitchers. J. Orthop. Sports Phys. Ther. 1997, 25, 323–328. [Google Scholar] [CrossRef]
- Van Meeteren, J.; Roebroeck, M.; Stam, H. Test-retest reliability in isokinetic muscle strength measurements of the shoulder. J. Rehabil. Med. 2002, 34, 91–95. [Google Scholar] [CrossRef]
- Baltzopoulos, V.; Williams, J.G.; Brodie, D.A. Sources of error in isokinetic dynamometry: Effects of visual feedback on maximum torque. J. Orthop. Sports Phys. Ther. 1991, 13, 138–142. [Google Scholar] [CrossRef]
- Keshavarz, R.; Bashardoust Tajali, S.; Mir, S.M.; Ashrafi, H. The role of scapular kinematics in patients with different shoulder musculoskeletal disorders: A systematic review approach. J. Bodyw. Mov. Ther. 2017, 21, 386–400. [Google Scholar] [CrossRef]
- Karduna, A.R.; McClure, P.W.; Michener, L.A.; Sennett, B. Dynamic measurements of three-dimensional scapular kinematics: A validation study. J. Biomech. Eng. 2001, 123, 184–190. [Google Scholar] [CrossRef]
- Scibek, J.S.; Carcia, C.R. Assessment of scapulohumeral rhythm for scapular plane shoulder elevation using a modified digital inclinometer. World J. Orthop. 2012, 3, 87–94. [Google Scholar] [CrossRef]
- Ebaugh, D.D.; McClure, P.W.; Karduna, A.R. Three-dimensional scapulothoracic motion during active and passive arm elevation. Clin. Biomech. 2005, 20, 700–709. [Google Scholar] [CrossRef]
- Ishikawa, H.; Muraki, T.; Morise, S.; Yamamoto, N.; Itoi, E.; Izumi, S.-I. Differences in scapular motion and parascapular muscle activities among patients with symptomatic and asymptomatic rotator cuff tears, and healthy individuals. JSES Int. 2020, 5, 238–246. [Google Scholar] [CrossRef]
- Lawrence, R.L.; Braman, J.P.; Ludewig, P.M. Shoulder kinematics impact subacromial proximities: A review of the literature. Braz. J. Phys. 2020, 24, 219–230. [Google Scholar] [CrossRef]
- Soslowsky, L.J.; Malicky, D.M.; Blasier, R.B. Active and passive factors in inferior glenohumeral stabilization: A biomechanical model. J. Shoulder Elb. Surg. 1997, 6, 371–379. [Google Scholar] [CrossRef]
- Thomas, S.J.; Swanik, K.A.; Swanik, C.B.; Kelly, J.D.T. Internal rotation deficits affect scapular positioning in baseball players. Clin. Orthop. Relat. Res. 2010, 468, 1551–1557. [Google Scholar] [CrossRef]
- Zago, M.; Kawczyński, A.; Klich, S.; Pietraszewski, B.; Galli, M.; Lovecchio, N. Fatigue-Induced Scapular Dyskinesis in Healthy Overhead Athletes. Front. Bioeng. Biotechnol. 2020, 8, 302. [Google Scholar] [CrossRef]
- Sehgal, S.; Sen, S.; Dhawan, A. Effects of muscle energy technique in increasing range of motion and strength of glenohumeral internal rotator, in athletes with glenohumeral internal rotation deficit. Am. J. Sports Sci. 2016, 4, 43–48. [Google Scholar] [CrossRef][Green Version]
- Chopp-Hurley, J.N.; O’Neill, J.M.; McDonald, A.C.; Maciukiewicz, J.M.; Dickerson, C.R. Fatigue-induced glenohumeral and scapulothoracic kinematic variability: Implications for subacromial space reduction. J. Electromyogr. Kinesiol. 2016, 29, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Maenhout, A.; Dhooge, F.; Van Herzeele, M.; Palmans, T.; Cools, A. Acromiohumeral distance and 3-dimensional scapular position change after overhead muscle fatigue. J. Athl. Train. 2015, 50, 281–288. [Google Scholar] [CrossRef]
- Bach, G.H.; Goldberg, B.A. Posterior Capsular Contracture of the Shoulder. J. Am. Acad. Orthop. Surg. 2006, 14, 265–277. [Google Scholar] [CrossRef][Green Version]
- Grossman, M.G.; Tibone, J.E.; McGarry, M.H.; Schneider, D.J.; Veneziani, S.; Lee, T.Q. A cadaveric model of the throwing shoulder: A possible etiology of superior labrum anterior-to-posterior lesions. J Bone Jt. Surg. Am. 2005, 87, 824–831. [Google Scholar]
- Wilk, K.E.; Arrigo, C.A.; Andrews, J.R. Current concepts: The stabilizing structures of the glenohumeral joint. J. Orthop. Sports Phys. Ther. 1997, 25, 364–379. [Google Scholar] [CrossRef] [PubMed]
- Edouard, P.; Frize, N.; Calmels, P.; Samozino, P.; Garet, M.; Degache, F. Influence of rugby practice on shoulder internal and external rotators strength. Int. J. Sports Med. 2009, 30, 863–867. [Google Scholar] [CrossRef] [PubMed]
- Van Dyk, N.; Bahr, R.; Whiteley, R.; Tol, J.L.; Kumar, B.D.; Hamilton, B.; Farooq, A.; Witvrouw, E. Hamstring and Quadriceps Isokinetic Strength Deficits Are Weak Risk Factors for Hamstring Strain Injuries: A 4-Year Cohort Study. Am. J. Sports Med. 2016, 44, 1789–1795. [Google Scholar] [CrossRef]
- Pinto, M.D.; Blazevich, A.J.; Andersen, L.L.; Mil-Homens, P.; Pinto, R.S. Hamstring-to-quadriceps fatigue ratio offers new and different muscle function information than the conventional non-fatigued ratio. Scand. J. Med. Sci. Sports 2018, 28, 282–293. [Google Scholar] [CrossRef]
- Delextrat, A.; Baker, J.; Cohen, D.D.; Clarke, N.D. Effect of a simulated soccer match on the functional hamstrings-to-quadriceps ratio in amateur female players. Scand. J. Med. Sci. Sports 2013, 23, 478–486. [Google Scholar] [CrossRef]
- Stickley, C.D.; Hetzler, R.K.; Freemyer, B.G.; Kimura, I.F. Isokinetic peak torque ratios and shoulder injury history in adolescent female volleyball athletes. J. Athl. Train. 2008, 43, 571–577. [Google Scholar] [CrossRef]
- Greig, M. The Influence of Soccer-Specific Fatigue on Peak Isokinetic Torque Production of the Knee Flexors and Extensors. Am. J. Sports Med. 2008, 36, 1403–1409. [Google Scholar] [CrossRef]
- Hsu, J.E.; Hulet, D.A.; McDonald, C.; Whitson, A.; Russ, S.M.; Matsen, F.A., III. The contribution of the scapula to active shoulder motion and self-assessed function in three hundred and fifty two patients prior to elective shoulder surgery. Int. Orthop. 2018, 42, 2645–2651. [Google Scholar] [CrossRef]
- Birfer, R.; Sonne, M.W.; Holmes, M.W. Manifestations of muscle fatigue in baseball pitchers: A systematic review. PeerJ 2019, 7, e7390. [Google Scholar] [CrossRef]
- Sauers, E. Theories on throwing injuries diverge from book of Jobe. Biomechanics 2001, 8, 61–66. [Google Scholar]
- Brown, L.P.; Niehues, S.L.; Harrah, A.; Yavorsky, P.; Hirshman, H.P. Upper extremity range of motion and isokinetic strength of the internal and external shoulder rotators in major league baseball players. Am. J. Sports Med. 1988, 16, 577–585. [Google Scholar] [CrossRef]
- Konda, S.; Yanai, T.; Sakurai, S. Configuration of the Shoulder Complex During the Arm-Cocking Phase in Baseball Pitching. Am. J. Sports Med. 2015, 43, 2445–2451. [Google Scholar] [CrossRef]
- Giphart, J.E.; van der Meijden, O.A.; Millett, P.J. The effects of arm elevation on the 3-dimensional acromiohumeral distance: A biplane fluoroscopy study with normative data. J. Shoulder Elb. Surg. 2012, 21, 1593–1600. [Google Scholar] [CrossRef]
- Bagordo, A.; Ciletti, K.; Kemp-Smith, K.; Simas, V.; Climstein, M.; Furness, J. Isokinetic Dynamometry as a Tool to Predict Shoulder Injury in an Overhead Athlete Population: A Systematic Review. Sports 2020, 8, 124. [Google Scholar] [CrossRef]
- Croisier, J.L.; Ganteaume, S.; Binet, J.; Genty, M.; Ferret, J.M. Strength imbalances and prevention of hamstring injury in professional soccer players: A prospective study. Am. J. Sports Med. 2008, 36, 1469–1475. [Google Scholar] [CrossRef]
- Asker, M.; Brooke, H.L.; Waldén, M.; Tranaeus, U.; Johansson, F.; Skillgate, E.; Holm, L.W. Risk factors for, and prevention of, shoulder injuries in overhead sports: A systematic review with best-evidence synthesis. Br. J. Sports Med. 2018, 52, 1312–1319. [Google Scholar] [CrossRef]

| Variables | Mean ± SD | Range | |
|---|---|---|---|
| Age (year) | 23.94 ± 4.71 | 18–33 | |
| Height (cm) | 183.31 ± 4.47 | 174–192 | |
| Weight (kg) | 87.69 ± 8.17 | 76–108 | |
| Body Mass Index, (kg/m2) | 26.08 ± 1.98 | 23.4–29.3 | |
| Career (years) | 13.33 ± 3.50 | 8–20 | |
| 60°/s PT%BW (%) | IR | 31.63 ± 5.78 | 23–40 |
| ER | 29.5 ± 3.44 | 23–36 | |
| ER/IR | 96.30 ± 20.98 | 69.2–134.6 | |
| 120°/s PT%BW (%) | IR | 29.75 ± 6.76 | 21–40 |
| ER | 28.88 ± 3.90 | 21–39 | |
| ER/IR | 101.53 ± 25.39 | 71–145 | |
| 180°/s PT%BW (%) | IR | 33.63 ± 6.02 | 23–44 |
| ER | 28.81 ± 3.53 | 24–36 | |
| ER/IR | 88.19 ± 18.95 | 66–128 | |
| Scapular upward Rotation Angle IR and ER Isokinetic Strength and Ratio | Humeral Elevation | ||||
|---|---|---|---|---|---|
| Rest, r (p) | 60°, r (p) | 90°, r (p) | 120°, r (p) | ||
| 60°/s PT%BW (%) | IR | 0.460 (0.073) | 0.424 (0.102) | 0.422 (0.104) | 0.279 (0.296) |
| ER | 0.064 (0.814) | −0.392 (−0.133) | −0.418 (0.107) | −0.558 (0.023) * | |
| Ratio | −0.378 (0.149) | −0.505 (0.046) * | −0.574 (0.020) * | −0.517 (0.040) * | |
| 60°/s TW%BW (%) | IR | 0.443 (0.086) | 0.297 (0.265) | 0.336 (0.203) | 0.091 (0.738) |
| ER | −0.012 (0.966) | −0.402 (0.123) | −0.457 (0.075) | −0.393 (0.132) | |
| Ratio | −0.399 (0.126) | −0.473 (0.064) | −0.554 (0.026) * | −0.318 (0.230) | |
| 120°/s PT%BW (%) | IR | 0.535 (0.033)* | 0.367 (0.163) | 0.272 (0.308) | 0.184 (0.495) |
| ER | −0.045 (0.868) | −0.385 (0.141) | −0.435 (0.092) | −0.504 (0.047) * | |
| Ratio | −0.500 (0.051) | −0.500 (0.049) * | −0.521 (0.039) * | −0.448 (0.082) | |
| 120°/s TW%BW (%) | IR | 0.311 (0.241) | 0.243 (0.365) | 0.309 (0.244) | −0.139 (0.607) |
| ER | −0.027 (0.921) | −0.294 (0.269) | −0.277 (0.299) | −0.524 (0.037)* | |
| Ratio | −0.341 (0.197) | −0.470 (0.066) | −0.589 (0.016) * | −0.282 (0.290) | |
| 180°/s PT%BW (%) | IR | 0.522 (0.038) * | 0.005 (0.985) | −0.105 (0.698) | −0.088 (0.747) |
| ER | 0.071 (0.794) | −0.426 (0.100) | −0.591 (0.016) * | −0.543 (0.030) * | |
| Ratio | −0.368 (0.160) | −0.192 (0.476) | −0.256 (0.339) | −0.188 (0.485) | |
| 180°/s TW%BW (%) | IR | 0.377 (0.150) | 0.185 (0.493) | −0.132 (0.627) | −0.026 (0.923) |
| ER | 0.033 (0.903) | −0.333 (0.208) | −0.556 (0.025) * | −0.495 (0.051) | |
| Ratio | −0.418 (0.107) | −0.360 (0.171) | −0.264 (0.322) | −0.297 (0.264) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, B.G.; Lim, S.K.; Kong, S. The Relationship between Scapular Upward Rotation and Shoulder Internal and External Rotation Isokinetic Strength in Professional Baseball Pitchers. Healthcare 2021, 9, 759. https://doi.org/10.3390/healthcare9060759
Kim BG, Lim SK, Kong S. The Relationship between Scapular Upward Rotation and Shoulder Internal and External Rotation Isokinetic Strength in Professional Baseball Pitchers. Healthcare. 2021; 9(6):759. https://doi.org/10.3390/healthcare9060759
Chicago/Turabian StyleKim, Byung Gon, Seung Kil Lim, and Sunga Kong. 2021. "The Relationship between Scapular Upward Rotation and Shoulder Internal and External Rotation Isokinetic Strength in Professional Baseball Pitchers" Healthcare 9, no. 6: 759. https://doi.org/10.3390/healthcare9060759
APA StyleKim, B. G., Lim, S. K., & Kong, S. (2021). The Relationship between Scapular Upward Rotation and Shoulder Internal and External Rotation Isokinetic Strength in Professional Baseball Pitchers. Healthcare, 9(6), 759. https://doi.org/10.3390/healthcare9060759







