Development and Effect of a Fall Prevention Program Based on King’s Theory of Goal Attainment in Long-Term Care Hospitals: An Experimental Study
Abstract
1. Introduction
2. Methods
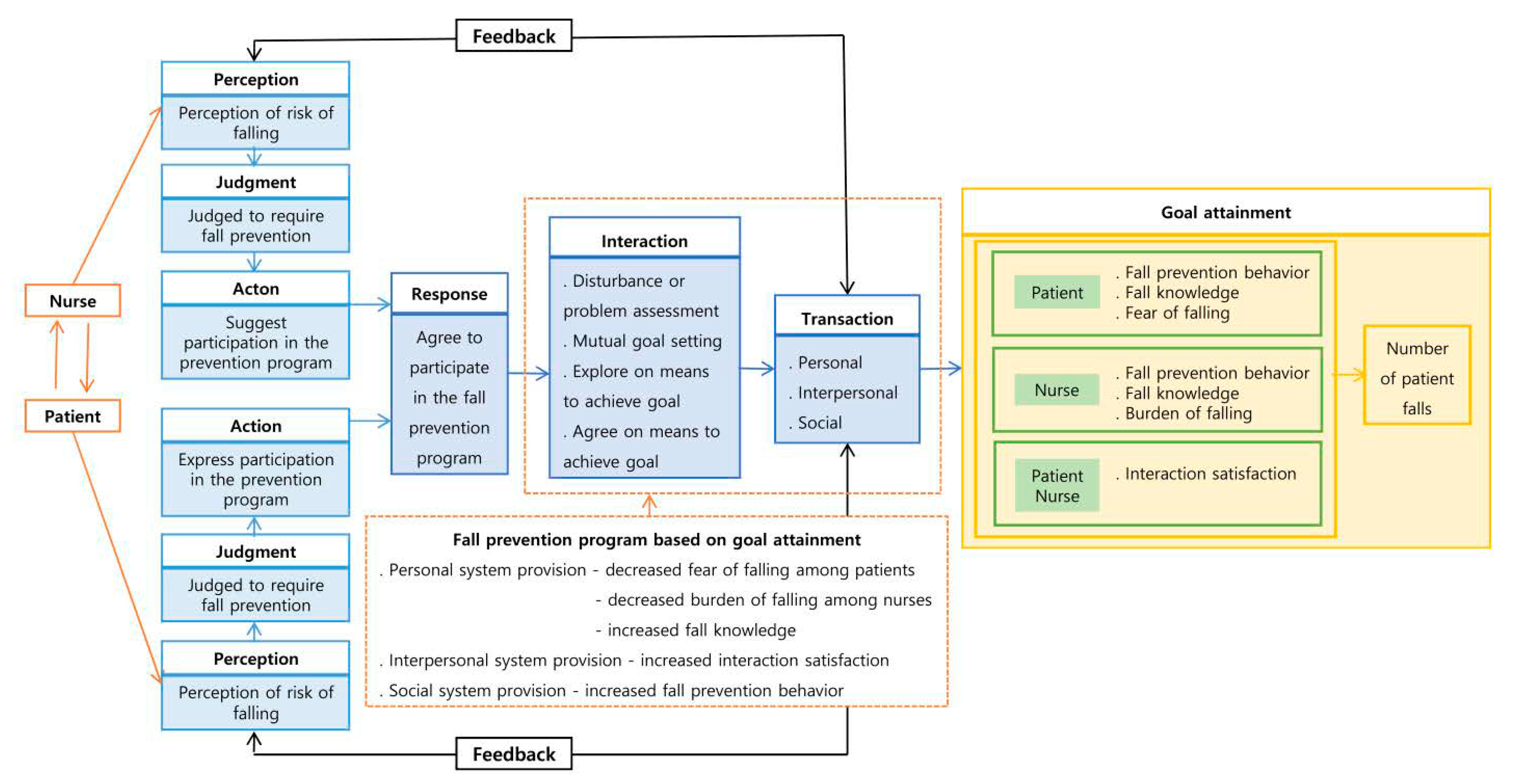
2.1. Fall Prevention Program Based on King’s Goal Achievement Theory
2.1.1. Fall Prevention Program Contents
- A.
- Individual education
- B.
- Group education
- C.
- Individual counseling
- D.
- Individual activities
2.1.2. Weekly Themes and Goals of the Fall Prevention Program
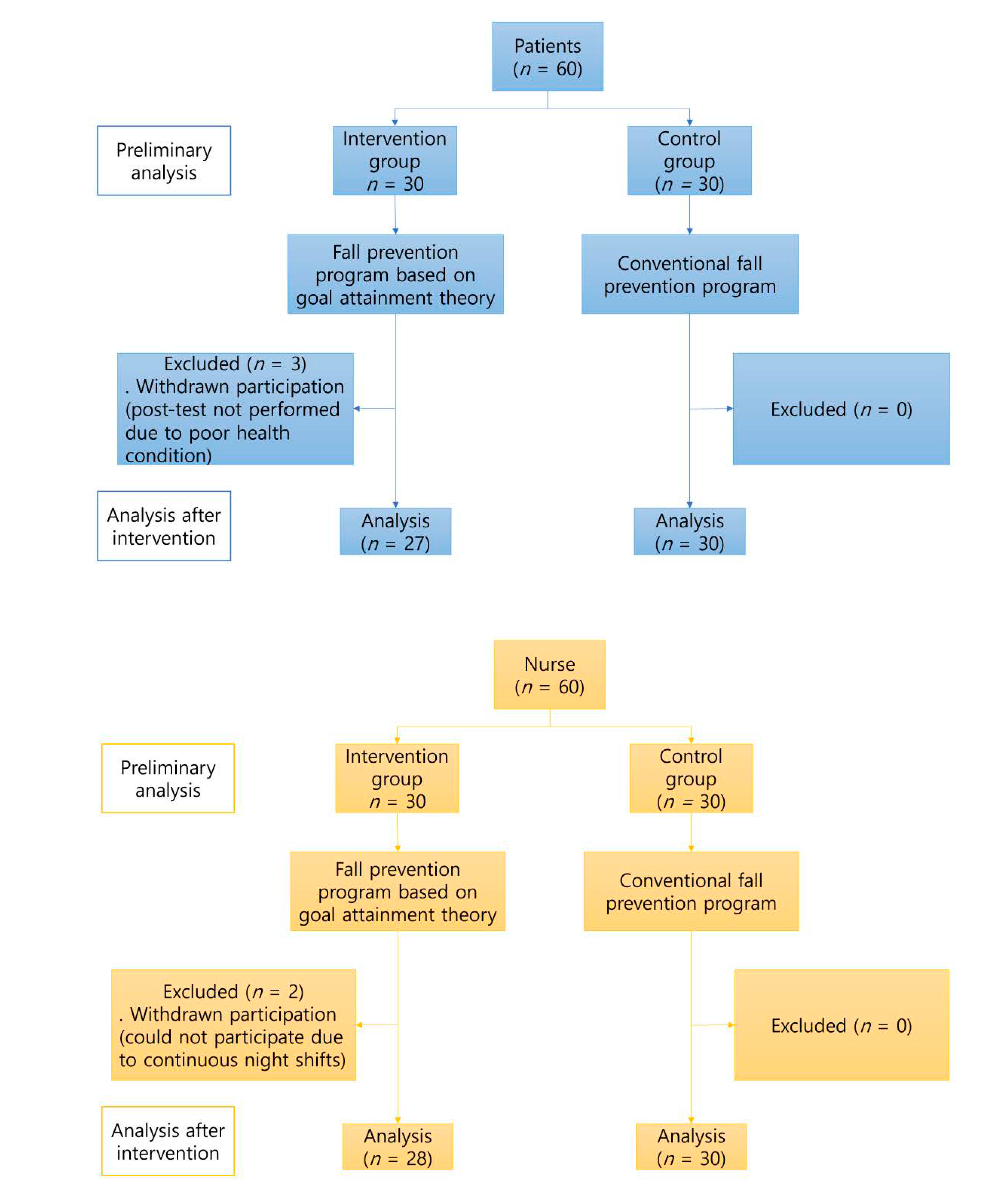
2.2. Verification of the Effects of the Fall Prevention Program Based on King’s Goal Attainment Theory
2.2.1. Design
2.2.2. Participants and Sampling Method
2.2.3. Research Tools
Patients
Nurses
2.2.4. Data Analysis
2.2.5. Ethical Considerations
3. Results
3.1. General and Disease-Related Characteristics
3.1.1. Patients
3.1.2. Nurses
3.2. Pre-Test Homogeneity Test for Study Variables
3.2.1. Patients
3.2.2. Nurses
3.3. Effects of the Fall Prevention Program
3.3.1. Patients’ Number of Falls, Fall Prevention Behavior, Fall Knowledge, and Fear of Falling
3.3.2. Nurses’ Fall Prevention Behavior, Fall Knowledge, and Burden of Falling
3.3.3. Interaction Satisfaction among Patients and Nurses
4. Discussion
4.1. Fall Prevention Program Based on King’s Goal Achievement Theory
4.2. Effects of the Fall Prevention Program
4.3. Limitations
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kostat. Elderly. Available online: https://kostat.go.kr/portal/korea/kor_nw/1/1/index.board?bmode=read&bSeq=&aSeq=377701&pgeNo=1&rowNum=10&navCount=10&currPg=&searchInfo=srch&sTarget=title&sTxt=%EA%B3%A0%EB%A0%B9%EC%9E%90+%ED%86%B5%EA%B3%84 (accessed on 27 September 2019).
- Kostat. Special Estimates for Future Furniture. Available online: https://kostat.go.kr/portal/korea/kor_nw/1/2/1/index.board?bmode=read&bSeq=&aSeq=377540&pageNo=2&rowNum=10&navCount=10&currPg=&searchInfo=&sTarget=title&sTxt= (accessed on 18 September 2019).
- National Health Insurance Service (NHIS). Health Insurance Statistical Yearbook. 2019. Available online: https://www.nhis.or.kr/nhis/together/wbhaea01600m01.do?mode=view&articleNo=10802558&article.offset=80&artcleLimit=10 (accessed on 13 November 2020).
- Miake-Lye, I.M.; Hempel, S.; Ganz, D.A.; Shekelle, P.G. Inpatient fall prevention programs as a patient safety strategy: A systematic review. Ann. Intern. Med. 2013, 158, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Yoo, K.S. Knowledge, attitude and prevention activities related to fall among of geriatric hospital nurse. J. Korean Public Health Nurs. 2017, 31, 436–450. [Google Scholar] [CrossRef]
- Heung, M.; Adamowski, T.; Segal, J.H.; Malani, P.N. A successful approach to fall prevention in an outpatient hemodialysis center. Clin. J. Am. Soc. Nephrol. 2010, 5, 1775–1779. [Google Scholar] [CrossRef] [PubMed]
- Carroll, D.L.; Dykes, P.C.; Hurley, A.C. Patients’ perspectives of falling while in an acute care hospital and suggestions for prevention. Appl. Nurs. Res. 2010, 23, 238–241. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Falls. Available online: http://www.who.int/mediacentre/factsheets/fs344/en/ (accessed on 16 January 2018).
- Chung, M.S. The effects of fall prevention education on the fall-related knowledge and prevention activity of the elderly hospitalized in internal medicine department. J. Muscle Jt. Health 2013, 20, 102–111. [Google Scholar] [CrossRef][Green Version]
- Bae, J.; Cho, S.I. Effects of community-based comprehensive call prevention program on muscle strength, postural balance and fall efficacy in elderly people. J Korean Acad. Nurs. 2014, 44, 697–707. [Google Scholar] [CrossRef]
- World Health Organization. Global Report on Falls Prevention in Older Age. Available online: https://extranet.who.int/agefriendlyworld/global-report-on-falls-prevention-in-older-age/ (accessed on 26 June 2014).
- Glogovsky, D. How can policy change guide nursing practice to reduce in-patient falls? Nursing2020 2017, 47, 63–67. [Google Scholar] [CrossRef]
- Lopez, K.D.; Gerling, G.J.; Cary, M.P.; Kanak, M.F. Cognitive work analysis to evaluate the problem of patient falls in an inpatient setting. J. Am. Med. Inform. Assoc. 2010, 17, 313–321. [Google Scholar] [CrossRef][Green Version]
- Gu, Y.Y.; Balcaen, K.; Ni, Y.; Ampe, J.; Goffin, J. Review on prevention of falls in hospital settings. Chin. Nurs. Res. 2016, 3, 7–10. [Google Scholar] [CrossRef]
- Park, Y.H. Characteristics and ADL (Activities of Daily Living) associated factors of elderly inpatients in long-term care hospitals: A survey of patients (2013–2014). Korean J. Health Serv. Manag. 2016, 10, 159–171. [Google Scholar] [CrossRef]
- Lee, Y.J.; Gu, M.O. The fall related circumstance, fall risk factor, and fall predictors of inpatients of small and medium sized hospitals. Clin. Nurs. Res. 2015, 21, 252–265. [Google Scholar]
- King, B.; Pecanac, K.; Krupp, A.; Liebzeit, D.; Mahoney, J. Impact of fall prevention on nurses and care of fall risk patients. Gerontologist 2018, 58, 331–340. [Google Scholar] [CrossRef] [PubMed]
- Njine, D.; Soroka, B. Good Quality Interaction between the Registered Nurse and the Patient: A Systematic Review. Degree Programme in Nursing; Seinajoki University of Applied Sciences: Seinajoki, Finland, 2016. [Google Scholar]
- Jang, H.K.; Lee, J.Y.; Kim, M.K.; Yang, E.O.; Gil, C.R. Reliability and validity of Korean version of the nurse-patient interaction scale. J. Korea Acad. Industr. Coop. Soc. 2019, 20, 747–757. [Google Scholar] [CrossRef]
- King, I.M. A Theory for Nursing Systems, Concepts, Process; Wiley: New York, NY, USA, 1981. [Google Scholar]
- de Leon-Demare, K.; MacDonald, J.; Gregory, D.M.; Katz, A.; Halas, G. Articulating nurse practitioner practice using King’s theory of goal attainment. J. Am. Assoc. Nurs. Pract. 2015, 27, 631–636. [Google Scholar] [CrossRef]
- Araújo, E.S.S.; Silva, L.F.D.; Moreira, T.M.M.; Almeida, P.C.D.; Freitas, M.C.D.; Guedes, M.V.C. Nursing care to patients with diabetes based on King’s theory. Rev. Bras. Enferm. 2018, 71, 1092–1098. [Google Scholar] [CrossRef] [PubMed]
- Shim, S.M.; Kim, E.H. Effect of fall prevention education for older patients in comprehensive nursing care service ward. J. Korean Public Health Nurs. 2019, 33, 200–213. [Google Scholar] [CrossRef]
- Kang, Y.O.; Song, R.Y. Effects of fall prevention education program on attitu.des, prevention behaviors, and satisfaction among elderly inpatients. Korean J. Adult Nurs. 2018, 30, 49–59. [Google Scholar] [CrossRef]
- Lee, H.O.; Lee, B.H.; Lee, C.H. Effect of strength exercise on patient fall prevention program: Focusing on the fall high risk group elderly patients. J. Health Inform. Stat. 2017, 42, 338–345. [Google Scholar] [CrossRef]
- Cho, E.K.; Sung, M.H.; Lee, Y.S.; Seok, S.H. Effects of fall prevention educational program for nurses in comprehensive nursing care units. J. Korea Contents Assoc. 2019, 19, 190–200. [Google Scholar] [CrossRef]
- Park, B.M.; Ryu, H.S.; Kwon, K.E.; Lee, C.Y. Development and effects of a fall prevention program based on King’s goal attainment theory for fall high-risk elderly patients in long-term care hospital. J. Korean Acad. Nurs. 2019, 49. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, H.A.; Park, S.W. Prevention of fall in the hospital. J. Korean Med. Assoc. 2015, 58, 123–130. [Google Scholar] [CrossRef]
- Kim, E.K.; Lee, J.C.; Eom, M.R. Fall risk factors of inpatients. J. Korean Acad. Nurs. 2008, 38, 676–684. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J. Identifying Characteristics of Fall Episodes and Fall-Related Risk Predictors. Master’s Thesis, Graduate School of Hanyang University, Seoul, Korea, 2018. [Google Scholar]
- Baek, Y.J.; Jung, I.S. Fall risk of patients admitted to emergency room. Global Health Nur. 2012, 2, 34–42. [Google Scholar]
- Pohl, P.; Sandlund, M.; Ahlgren, C.; Bergvall-Kåreborn, B.; Lundin-Olsson, L.; Wikman, A.M. Fall risk awareness and safety precautions taken by older community-dwelling women and men—A qualitative study using focus group discussions. PLoS ONE 2015, 10, e0119630. [Google Scholar] [CrossRef]
- Adib-Hajbaghery, M.; Tahmouresi, M. Nurse–patient relationship based on the Imogene King’s theory of goal attainment. Nurs. Midwifery Stud. 2018, 7, 141–144. [Google Scholar] [CrossRef]
- Ladee, C.; Lagampan, S.; Pichayapinyo, P.; Mayurasakorn, K.; Lagampan, C. Effect of a goal attainment nursing program on self-management and blood pressure control in high-risk hypertensive patients in a primary care unit. Siriraj Med. J. 2020, 72, 140–150. [Google Scholar] [CrossRef]
- Killeen, M.B.; King, I.M. Use of King’s conceptual system, nursing informatics, and nursing classification systems for global communication. Int. J. Nurs. Terminol. Classif. 2007, 18, 51–57. [Google Scholar] [CrossRef]
- Lee, C.H. Development and Evaluation of Fall Prevention Program Based on King’s Goal Attainment Theory for the Elderly with Lower Extremity Osteoarthritis in the Community. Ph.D. Thesis, Graduate School of Keimyung University, Seoul, Korea, 2019. [Google Scholar]
- How-to Guide: Reducing Patient Injuries from Falls. Available online: https://www.ihi.org/resources/Pages/Tools/TCABHowToGuideReducingPatientInjuriesfromFalls.aspx (accessed on 1 December 2012).
- Korea Institute for Healthcare Accreditation (KOIHA). 3rd Period Long Term Care Hospital Certification Standards Promulgated. Available online: https://www.koiha.or.kr/member/kr/board/establish/establish_BoardList.do (accessed on 26 December 2019).
- Ministry of Health and Welfare (MOHW). The First Comprehensive Patient Safety Plan. Available online: https://www.mohw.go.kr/react/jb/sjb030301vw.jsp?PAR_MENU_ID=03&MENU_ID=0319&CONT_SEQ=344873&page=1 (accessed on 11 July 2018).
- The Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel, Liaisons, and Staff. A clinical practice guideline for treating tobacco use and dependence: 2008 update: A U.S. public health service report. Am. J. Prev. Med. 2008, 35, 158–176. [Google Scholar] [CrossRef]
- Krauss, M.J.; Tutlam, N.; Costantinou, E.; Johnson, S.; Jackson, D.; Fraser, V.J. Intervention to prevent falls on the medical service in a teaching hospital. Infect. Control Hosp. Epidemiol. 2008, 29, 539–545. [Google Scholar] [CrossRef][Green Version]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Jung, I.J.; Kim, S.J. Effects of group counseling program based on King’s goal attainment theory for middle school students with emotional and behavioral problems. J. Korean Acad. Nurs. 2017, 47, 199–210. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Richman, D.; Powell, L. Falls efficacy as a measure of fear of falling. J. Gerontol. 1990, 45, P239–P243. [Google Scholar] [CrossRef]
- Jang, J.M. A Structural Model for Falls and Quality of Life in Elderly People Living at Home. Ph.D. Thesis, Graduate School of Kyunghee University, Seoul, Korea, 2005. [Google Scholar]
- Kim, M.Y. A Study of Fall Risk, Fear of Falling, and Depression in Patients after Brain Tumor Surgery. Master’s Thesis, Graduate School of Ewha Womans University, Seoul, Korea, 2014. [Google Scholar]
- Kim, C.K. An Analysis of Fall Incidence Rate and Its Related Factors of Fall in in Patients. Ph.D. Thesis, Graduate School of Seoul National University, Seoul, Korea, 2002. [Google Scholar]
- Kim, M.Y. Fall-Related Knowledge and Prevention Behavior among Hospitalized Elderly Inpatients. Master’s Thesis, Graduate School of Keimyung University, Seoul, Korea, 2008. [Google Scholar]
- Lim, S.R.; Kwon, J.H. Marital communication behavior and marital satisfaction. Korean J. Clin. Psychol. 1998, 1998, 109–123. [Google Scholar]
- Kim, Y.J. Nurse-patient interaction patterns and patient satisfaction in the emergency department. J. Korean Acad. Nurs. 2010, 40, 99–109. [Google Scholar] [CrossRef]
- Kim, M.S.; Kim, J.S. Effects of the fall prevention education program (FPEP) for caregivers in elderly care facilities on fall-related knowledge, fall-related burden, and caring behaviors for fall prevention. J. Korea Contents Assoc. 2013, 13, 778–790. [Google Scholar] [CrossRef][Green Version]
- Kim, S.H.; Seo, J.M. Geriatric hospital nurses’ knowledge, attitude toward falls, and fall prevention activities. J. Korean Gerontol. Nurs. 2017, 19, 81–91. [Google Scholar] [CrossRef]
- Vahdat, S.; Hamzehgardeshi, L.; Hessam, S.; Hamzehgardeshi, Z. Patient involvement in health care decision making: A review. Iran Red. Crescent Med. J. 2014, 16, e12454. [Google Scholar] [CrossRef] [PubMed]
- Lim, M.L.; Ang, S.G.M.; Teo, K.Y.; Wee, Y.H.C.; Yee, S.P.; Lim, S.H.; Ang, S.Y. Patients’ experience after a fall and their perceptions of fall prevention: A qualitative study. J. Nurs. Care Qual. 2018, 33, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Herbst, A.M.; Friesen, M.A.; Speroni, K.G. Caring, connecting, and communicating: Reflections on developing a patient-centered bedside handoff. Int. J. Hum. Caring 2013, 17, 16–22. [Google Scholar] [CrossRef]
- Doane, G.H.; Varcoe, C. Relational practice and nursing obligations. Adv. Nurs. Sci. 2007, 30, 192–205. [Google Scholar] [CrossRef]
- Zhao, Y.L.; Bott, M.; He, J.; Kim, H.; Park, S.H.; Dunton, N. Evidence on fall and injurious fall prevention interventions in acute care hospitals. J. Nurs. Adm. 2019, 49, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Yardley, L.; Donovan-Hall, M.; Francis, K.; Todd, C. Attitudes and beliefs that predict older people’s intention to undertake strength and balance training. J. Gerontol. B Psychol. Sci. Soc. Sci. 2007, 62, 119–125. [Google Scholar] [CrossRef]
- Tzeng, H.M.; Yin, C.Y. Patient engagement in hospital fall prevention. Nurs. Econ. 2015, 33, 326–334. [Google Scholar] [PubMed]
- Dykes, P.C.; Carroll, D.L.; Hurley, A.; Lipsitz, S.; Benoit, A.; Chang, F.; Middleton, B. Fall prevention in acute care hospitals: A randomized trial. J. Am. Med. Assoc. 2010, 304, 1912–1918. [Google Scholar] [CrossRef] [PubMed]
- Fonda, D.; Cook, J.; Sandler, V.; Bailey, M. Sustained reduction in serious fall-related injuries in older people in hospital. Med. J. Aust. 2006, 184, 379–382. [Google Scholar] [CrossRef]
- Healey, F.; Monro, A.; Cockram, A.; Adams, V.; Heseltine, D. Using targeted risk factor reduction to prevent falls in older in-patients: A randomised controlled trial. Age Ageing 2004, 33, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Barry, E.; Laffoy, M.; Matthews, E.; Carey, D. Preventing accidental falls among older people in long stay units. Ir. Med. J. 2001, 94, 172–175. [Google Scholar]
- Kiyoshi-Teo, H.; Northrup-Snyder, K.; Cohen, D.J.; Dieckmann, N.; Stoyles, S.; Winters-Stone, K.; Eckstrom, E. Older hospital inpatients’ fall risk factors, perceptions, and daily activities to prevent falling. Geriatr. Nurs. 2019, 40, 290–295. [Google Scholar] [CrossRef]
- McMahon, S.; Talley, K.M.; Wyman, J.F. Older people’s perspectives on fall risk and fall prevention programs: A literature review. Int. J. Older People Nurs. 2011, 6, 289–298. [Google Scholar] [CrossRef]
- Spoelstra, S.L.; Given, B.A.; Given, C.W. Fall prevention in hospitals: An integrative review. Clin. Nurs. Res. 2012, 21, 92–112. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.G. Nurses’ knowledge and attitude toward fall in hospitalized patients. J. Ind. Sci. Res. 2011, 28, 275–281. [Google Scholar]
- Kim, H.J.; Kim, H.Y. Experience of job stress among nurses working in long-term care hospital: A phenomenological approach. J. Korean Acad. Adult Nurs. 2016, 28, 572–584. [Google Scholar] [CrossRef]
- Ryu, J.M.; Kim, M.S. Influence of professional self-concept, self-leadership on elderly care performance of geriatric hospital nurses. J. Health Inform. Stat. 2016, 41, 392–402. [Google Scholar] [CrossRef]
- Kim, Y.J. Nurses’ experience of inpatients’ falls. J. Korean Acad. Fundam. Nurs. 2017, 24, 106–117. [Google Scholar] [CrossRef]
- Korea Ministry of Government Legislation (KMGL). Patient Safety Act. Available online: https://www.law.go.kr/LSW/lsLinkProc.do?&lsNm=%ED%99%98%EC%9E%90%EC%95%88%EC%A0%84%EB%B2%95&chrClsCd=010202&mode=20&ancYnChk=0# (accessed on 29 July 2016).
- Abou El Enein, N.Y.; Abd El Ghany, A.S.; Zaghloul, A.A. Knowledge and performance among nurses before and after a training programme on patient falls. Open J. Nurs. 2012, 2, 358–364. [Google Scholar] [CrossRef]
- Jung, J.Y.; Jung, K.H. The affect factors of geriatric hospital nurse’s falls prevention activities. J. Health Inform. Stat. 2016, 41, 203–211. [Google Scholar] [CrossRef]
| King’s Conceptual System | King’s Concept | Configuration Element | Main Strategy | Goal | Intervention Content | Intervention Methods | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Individual Education | Group Education | Individual Counseling | Individual Activities | ||||||||
| Personal system | Perception | Fear of falling | Problem assessment Knowledge and information provision | Decreased fear of falling among patients | (1) Assessment of problems related to falling among patients (2) Understanding the fear of falling | ● | ● | ||||
| Burden of falling | Problem assessment Knowledge and information provision | Reduced burden of falling among nurses | (1) Assessment of problems related to falling regarding nurses (2) Understanding the burden of falling | ● | ● | ||||||
| Growth and development | Fall knowledge | Knowledge and information provision | Improved fall knowledge | (1) Understanding fall knowledge using guidelines and prints | ● | ● | |||||
| Interpersonal system | Communication | Interaction satisfaction | Goal setting and motivation Knowledge and information provision | Increased fall prevention behavior through communication Increased interaction satisfaction | (1) Mutual goal setting to reduce the number of falls (2) Assessment of disturbance factors for fall prevention (3) Education on fall prevention guidelines and demonstrations (4) Feedback on understanding after education (5) Mutual assessment of fall prevention checklist (6) Fall prevention education using the 5A method by the assigned nurse 7) Medication education | ● | ● | ● | |||
| Interaction | |||||||||||
| Social System | Education system | Fall prevention behavior | Improved function and behavior | Improved fall prevention behavior | (1) Fall prevention education for patients and nurses (2) Fall prevention education with therapists and a nurse in charge of patient safety | ● | ● | ||||
| Social support | Motivation and emotional support | Enhanced motivation through improved social support | (1) Consultation and support for difficulties and concerns related to falls among patients (2) Consultation and support for difficulties and concerns related to falls regarding nurses (3) Supporting continued participation for fall prevention | ● | |||||||
| Group | Intervention Method | Program Schedule (Weeks) | |||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | ||||
| Intervention group | Individual education | ● | ● | ● | ● | ● | ● | ● | ● | ||
| Group education | ● | ||||||||||
| Individual counseling | ● | ● | ● | ● | ● | ● | ● | ● | |||
| Individual activities | ● | ● | |||||||||
| Variable | Classification | Patient Intervention Group (n = 27) Mean ± SD or Number (%) or Cases | Patient Control Group (n = 30) Mean ± SD or Number (%) or Cases | Total | χ2/ Z/ t | p |
|---|---|---|---|---|---|---|
| Age | 78.78 ± 9.50 | 78.77 ± 10.58 | 78.77 ± 9.99 | 0.00 | 0.997 | |
| Number of days in the hospital | 583.52 ± 444.28 | 376.60 ± 349.08 | 474.61 ± 406.95 | 1.97 | 0.054 | |
| Sex | Female | 18 (66.7) | 19 (63.3) | 37 (64.9) | 0.07 | 0.792 |
| Male | 9 (33.3) | 11 (36.7) | 20 (35.1) | |||
| Educational level | Elementary school | 6 (22.2) | 8 (26.7) | 14 (24.6) | 0.62 | 0.961 |
| Middle school | 5 (18.5) | 4 (13.3) | 9 (15.8) | |||
| High school | 5 (18.5) | 5 (16.7) | 10 (17.5) | |||
| Professional school | 1 (3.7) | 2 (6.7) | 3 (5.3) | |||
| College and above | 10 (37.0) | 11 (36.7) | 21 (36.8) | |||
| Fall experience in the past year | Yes | 5 (18.5%) | 8 (26.7%) | 13 (22.8%) | 0.66 | 0.513 |
| No | 22 (81.5%) | 22 (73.3%) | 44 (71.2%) | |||
| Experience of fall prevention education in the past year | Yes | 5 (18.5) | 6 (20.0) | 11 (19.3) | 0.02 | 0.887 |
| No | 22 (81.5) | 24 (80.0) | 46 (80.7) | |||
| How informative was the education session | Very helpful | 0 (0.0) | 5 (83.3) | 5 (45.5) | 7.77 | 0.026 |
| Helpful | 4 (80.0) | 1 (16.7) | 5 (45.5) | |||
| Not helpful | 1 (20.0) | 0 (0.0) | 1(9.1) | |||
| Diagnosis | Cerebrovascular disease | 22 (81.5) | 26 (86.7) | 48 (84.2) | 0.29 | 0.592 |
| Parkinson’s disease | 3 (11.1) | 3 (10.0) | 6 (10.5) | 0.02 | 0.891 | |
| Dementia | 15 (55.6) | 23 (76.7) | 38 (66.7) | 2.85 | 0.091 | |
| Femur fracture | 0 (0.0) | 1 (3.3) | 1 (1.8) | 0.92 | 0.339 | |
| Others | 3 (11.1) | 0 (0.0) | 3 (5.3) | 3.52 | 0.061 | |
| Comorbidity | Hypertension | 22 (81.5) | 23 (76.7) | 45 (78.9) | 0.20 | 0.656 |
| Diabetes | 5 (18.5) | 6 (20.0) | 11 (19.3) | 0.02 | 0.887 | |
| Cerebrovascular disease | 24 (88.9) | 27 (90.0) | 51 (89.5) | 0.02 | 0.891 | |
| Parkinson’s disease | 4 (14.8) | 4 (13.3) | 8 (14.0) | 0.02 | 0.872 | |
| Hemiparalysis | 22 (81.5) | 24 (80.0) | 46 (80.7) | 0.02 | 0.887 | |
| Paraplegia | 3 (11.1) | 0 (0.0) | 3 (5.3) | 3.52 | 0.061 | |
| Anti-psychotic medication | Yes | 9 (33.3) | 14 (46.7) | 23 (40.4) | 1.05 | 0.306 |
| No | 18 (66.7) | 16 (53.3) | 34 (59.6) | |||
| MMSE | 24.44 ± 4.10 | 23.97 ± 3.84 | 24.19 ± 3.93 | 0.46 | 0.651 | |
| MFS | 50.19 ± 23.88 | 56.33 ± 21.49 | 53.42 ± 22.66 | 1.02 | 0.331 | |
| Variable | Classification | Nurse intervention group (n = 28) Mean ± SD or number (%) | Nurse control group (n = 30) Mean ± SD or number (%) | Total | χ2/t | p |
| Age | 42.25 ± 7.53 | 35.97 ± 9.83 | 39.00 ± 9.28 | 2.72 | 0.008 | |
| Sex | Female | 28 (100.0) | 27 (90.0) | 55 (94.8) | 2.95 | 0.086 |
| Male | 0 (0.0) | 3 (10.0) | 3 (5.2) | |||
| Educational level | Professional school | 11 (39.3) | 9 (30.0) | 20 (34.5) | 0.55 | 0.457 |
| College | 17 (60.7) | 21 (70.0) | 38 (65.5) | |||
| Working experience | 11.80 ± 8.07 | 8.01 ± 6.22 | 9.84 ± 7.36 | 2.01 | 0.052 | |
| Fall experience of assigned patients in the past year | Yes | 18 (64.3) | 26 (86.7) | 44 (75.9) | 3.96 | 0.047 |
| No | 10 (35.7) | 4 (13.3) | 14 (24.1) | |||
| Fall prevention education in the past year | Yes | 28 (100.0) | 29 (96.7) | 57 (98.3) | 0.95 | 0.330 |
| No | 0 (0.0) | 1 (3.3) | 1 (1.7) | |||
| How informative was the education session | Very helpful | 11 (39.3) | 5 (17.2) | 16 (28.1) | 4.25 | 0.119 |
| Helpful | 15 (53.6) | 23 (79.3) | 38 (66.7) | |||
| Not helpful | 2 (7.1) | 1 (3.4) | 3 (5.3) | |||
| Nursing performance for fall prevention | Strongly agree | 7 (25.0) | 3 (10.0) | 10 (17.2) | 3.12 | 0.374 |
| Agree | 19 (67.9) | 24 (80.0) | 43 (74.1) | |||
| Disagree | 2 (7.1) | 2 (6.7) | 4 (6.9) | |||
| Strongly disagree | 0 (0.0) | 1 (3.3) | 1 (1.7) | |||
| Necessity of fall prevention education | Strongly agree | 12 (42.9) | 12 (40.0) | 24 (41.4) | 0.05 | 0.825 |
| Agree | 16 (57.1) | 18 (60.0) | 34 (58.6) |
| Variable | Time | Patient Intervention Group (n = 27) | Patient Control Group (n = 30) | Z/t | p |
|---|---|---|---|---|---|
| N (%) or Cases | N (%) or Cases | ||||
| Number of falls | Pre-test | 3 | 3 | −0.14 | 0.892 |
| Post-test | 2 | 5 | −1.22 | 0.222 | |
| Pre-post difference | −1 | 2 | −0.98 | 0.326 | |
| Z(p) | −0.71 (0.480) | −0.38 (0.705) | |||
| Fall prevention behavior | Pre-test | 2.38 ± 0.42 | 2.60 ± 0.60 | 1.57 | 0.121 |
| Post-test | 3.83 ± 0.22 | 2.38 ± 0.55 | −13.25 | <0.001 | |
| Pre-post difference | 1.44 ± 0.49 | −0.22 ± 0.58 | −11.66 | <0.001 | |
| t(p) | −15.26 (<0.001) | 2.12 (0.043) | |||
| Fall knowledge | Pre-test | 6.89 ± 3.19 | 8.13 ± 3.41 | 1.42 | 0.162 |
| Post-test | 13.41 ± 1.72 | 8.27 ± 4.39 | −5.93 | <0.001 | |
| Pre-post difference | 6.52 ± 3.57 | 0.13 ± 3.79 | −6.57 | <0.001 | |
| t(p) | −9.50 (<0.001) | −0.20 (0.847) | |||
| Fear of falling | Pre-test | 6.34 ± 1.87 | 6.34 ± 2.17 | −0.01 | 0.994 |
| Post-test | 1.91 ± 1.23 | 5.91 ± 2.95 | 6.79 | <0.001 | |
| Pre-post difference | −4.43 ± 2.27 | −0.43 ± 3.04 | 5.58 | <0.001 | |
| t(p) | 10.15 (<0.001) | 0.78 (0.444) | |||
| Interaction satisfaction | Pre-test | 3.35 ± 0.54 | 3.43 ± 0.49 | 0.59 | 0.558 |
| Post-test | 4.87 ± 0.42 | 3.32 ± 0.61 | −11.33 | <0.001 | |
| Pre-post difference | 1.52 ± 0.69 | −0.11 ± 0.82 | −8.06 | <0.001 | |
| t(p) | −11.39 (<0.001) | 0.74 (0.465) | |||
| Variable | Time | Nurse intervention group (n = 28) | Nurse control group (n = 30) | t | p |
| Mean ± SD | Mean ± SD | ||||
| Fall prevention behavior | Pre-test | 3.96 ± 0.48 | 3.78 ± 0.74 | −1.12 | 0.269 |
| Post-test | 4.69 ± 0.35 | 3.76 ± 0.71 | −6.40 | <0.001 | |
| Pre-post difference | 0.73 ± 0.68 | −0.02 ± 0.88 | −3.60 | <0.001 | |
| t(p) | −5.67 (<0.001) | 0.11 (0.912) | |||
| Fall knowledge | Pre-test | 13.50 ± 2.43 | 13.43 ± 2.11 | −0.11 | 0.911 |
| Post-test | 15.79 ± 0.63 | 14.00 ± 1.64 | −5.54 | <0.001 | |
| Pre-post difference | 2.29 ± 2.46 | 0.57 ± 2.43 | −2.67 | 0.010 | |
| t(p) | −4.91 (<0.001) | −1.28 (0.212) | |||
| Burden of falling | Pre-test | 2.76 ± 0.26 | 2.69 ± 0.26 | −0.92 | 0.362 |
| Post-test | 2.70 ± 0.51 | 2.84 ± 0.48 | 1.03 | 0.306 | |
| Pre-post difference | −0.05 ± 0.49 | 0.14 ± 0.43 | 1.65 | 0.105 | |
| t(p) | 0.58 (0.565) | −1.85 (0.074) | |||
| Interaction satisfaction | Pre-test | 3.37 ± 0.70 | 3.19 ± 0.54 | −1.10 | 0.278 |
| Post-test | 4.28 ± 0.67 | 3.22 ± 0.67 | −6.45 | <0.001 | |
| Pre-post difference | 0.92 ± 0.84 | 0.04 ± 0.77 | −4.16 | <0.001 | |
| t(p) | −5.78 (<0.001) | −0.26 (0.795) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, B.-M. Development and Effect of a Fall Prevention Program Based on King’s Theory of Goal Attainment in Long-Term Care Hospitals: An Experimental Study. Healthcare 2021, 9, 715. https://doi.org/10.3390/healthcare9060715
Park B-M. Development and Effect of a Fall Prevention Program Based on King’s Theory of Goal Attainment in Long-Term Care Hospitals: An Experimental Study. Healthcare. 2021; 9(6):715. https://doi.org/10.3390/healthcare9060715
Chicago/Turabian StylePark, Bom-Mi. 2021. "Development and Effect of a Fall Prevention Program Based on King’s Theory of Goal Attainment in Long-Term Care Hospitals: An Experimental Study" Healthcare 9, no. 6: 715. https://doi.org/10.3390/healthcare9060715
APA StylePark, B.-M. (2021). Development and Effect of a Fall Prevention Program Based on King’s Theory of Goal Attainment in Long-Term Care Hospitals: An Experimental Study. Healthcare, 9(6), 715. https://doi.org/10.3390/healthcare9060715






