Healthcare and Economic Impact of Lung Perfusion Scintigraphy in Patients Affected by Acute Pulmonary Embolism
Abstract
1. Introduction
Importance and Objectives
2. Materials and Methods
2.1. Patient Population—Organisation
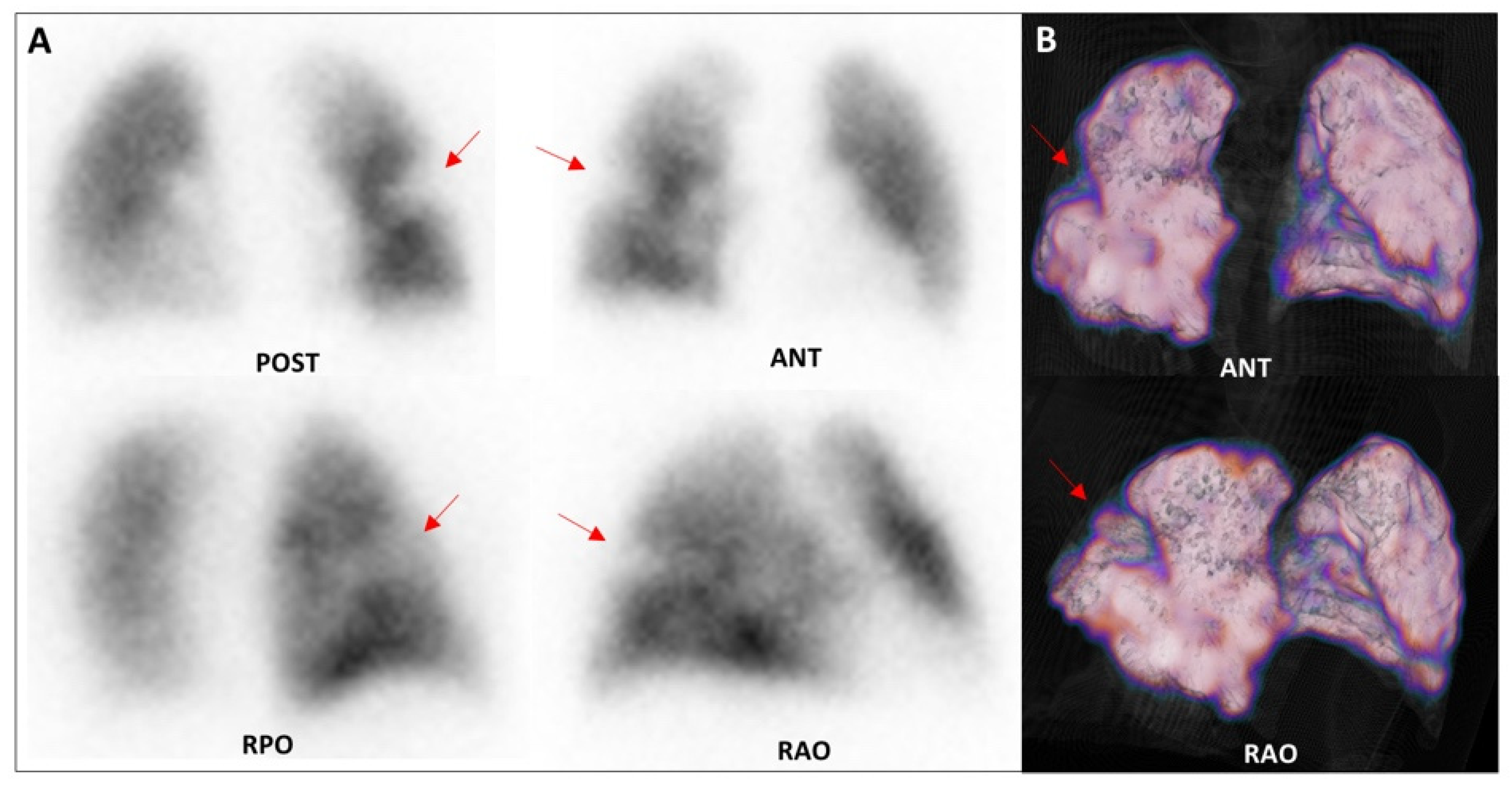
2.2. Lung Perfusion Scintigraphy (LPS): Acquisition and Interpretation Criteria
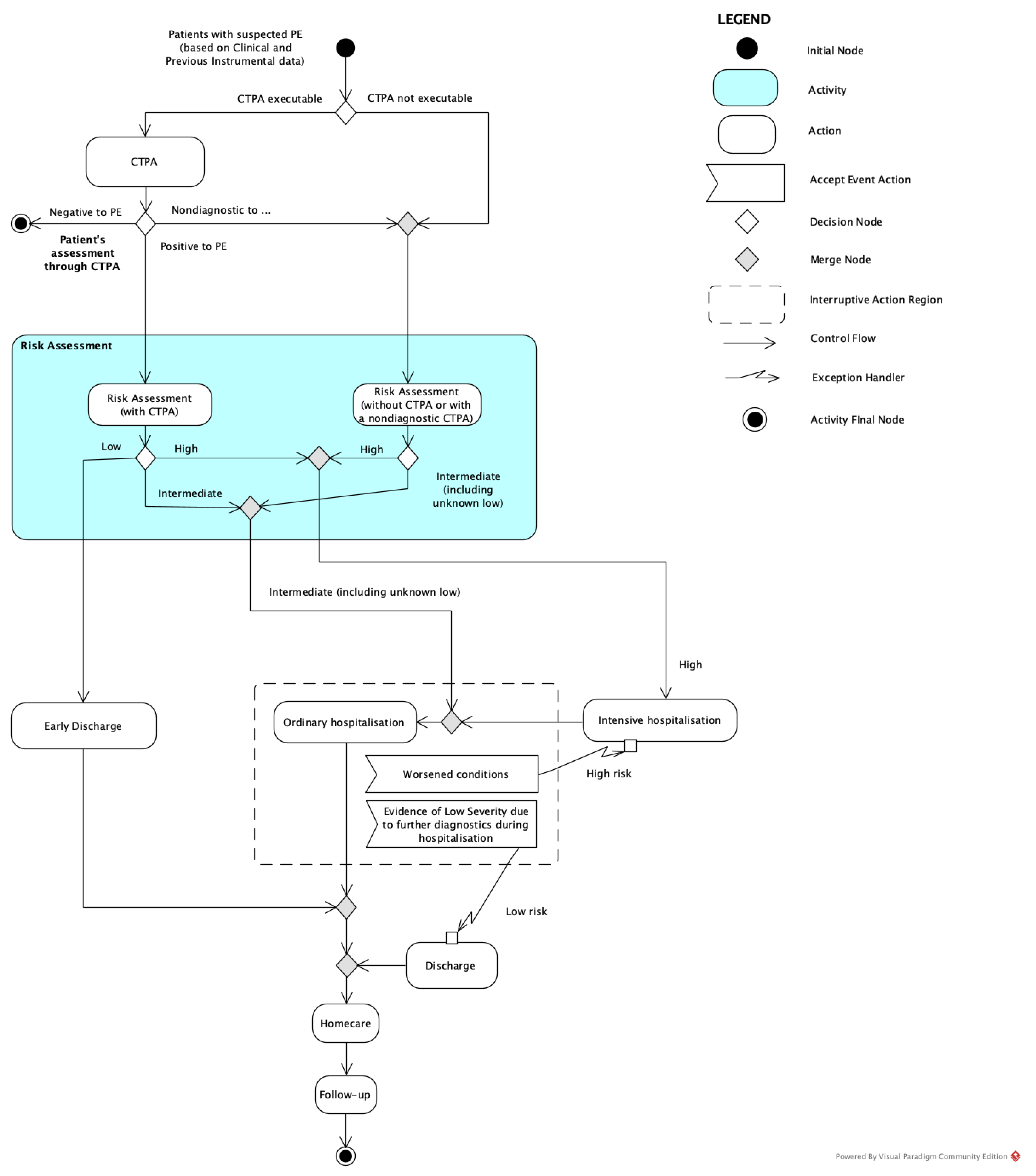
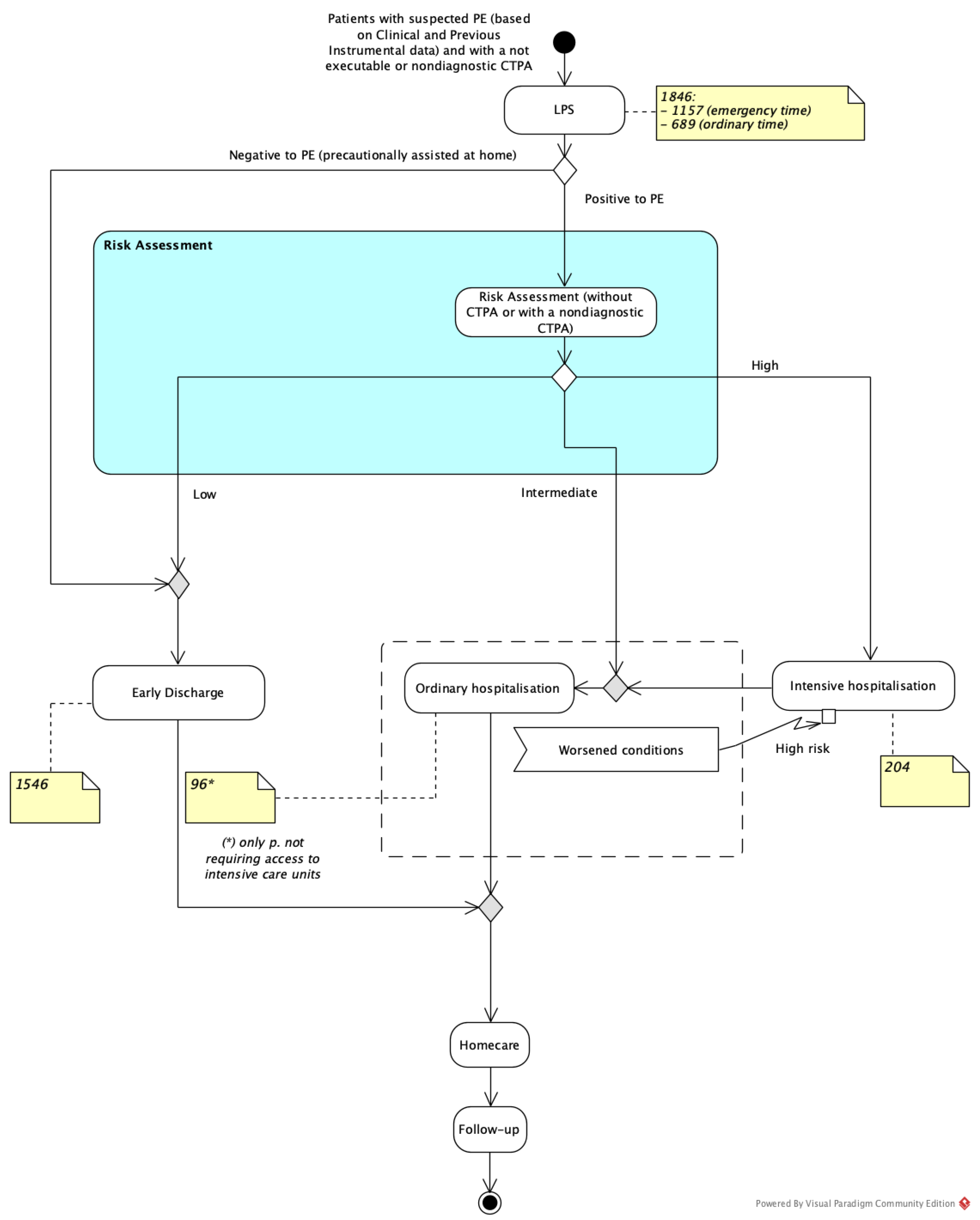
2.3. Risk Stratification and Homecare
- High risk, for those patients who present shock or hypotension. Due to the high rate of in-hospital mortality, especially in the first hours after hospitalisation, they must be addressed to thrombolytic therapy or, if contraindicated or not enough, to surgical embolectomy. These patients need hospitalisation with intensive care;
- Intermediate risk, for those patients in apparent hemodynamic stability on admission showing signs of right ventricular dysfunction and/or myocardial injury. The initial preferred anticoagulant therapy is unfractionated intravenous therapy. These patients need ordinary hospitalisation;
- Low risk, for those patients without any primary APE-related risk factors for whom early discharge can be planned with adequate outpatient care and anticoagulant therapy can be provided (subcutaneous low-molecular-weight heparin; new oral anticoagulants).
2.4. Clinical Decision Models
2.5. Cost Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Pelletier-Galarneau, M.; Zannier, E.; Zuckier, L.S.; le Gal, G. Referral Patterns and Diagnostic Yield of Lung Scintigraphy in the Diagnosis of Acute Pulmonary Embolism. Thrombosis 2017, 2017, 1623868. [Google Scholar] [CrossRef] [PubMed]
- Raskob, G.E.; Angchaisuksiri, P.; Blanco, A.N.; Buller, H.; Gallus, A.; Hunt, B.J.; Hylek, E.M.; Kakkar, A.; Konstantinides, S.V.; McCumber, M.; et al. Thrombosis: A major contributor to global disease burden. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 2363–2371. [Google Scholar] [CrossRef] [PubMed]
- Rubini, G.; Asabella, A.N.; Ianora, A.S.; Rubini, D.; Gaudiano, A.; Angelelli, G.; Rotondo, A. Acute pulmonary embolism: Comparison and integration of perfusion lung scintigraphy with multislice spiral CT. Radiol. Med. 2007, 112, 174–184. [Google Scholar] [CrossRef] [PubMed]
- Torbicki, A.; Perrier, A.; Konstantinides, S.; Agnelli, G.; Galiè, N.; Pruszczyk, P.; Bengel, F.; Brady, A.J.; Ferreira, D.; Janssens, U.; et al. Linee guida per la diagnosi e il trattamento dell ’ embolia polmonare acuta Task Force per la Diagnosi e il Trattamento dell ’ Embolia Polmonare Acuta. G. Ital. Cardiol. 2009, 10, 303–345. [Google Scholar]
- Wood, K.E. Major pulmonary embolism: Review of a pathophysiologic approach to the golden hour of hemodynamically significant pulmonary embolism. Chest 2002, 121, 877–905. [Google Scholar] [CrossRef]
- Konstantinides, S.V.; Meyer, G.; Becattini, C.; Bueno, H.; Geersing, G.J.; Harjola, V.P.; Huisman, M.V.; Humbert, M.; Jennings, C.S.; Jiménez, D.; et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European respiratory society (ERS). Eur. Heart J. 2020, 41, 543–603. [Google Scholar] [CrossRef]
- Stein, P.D.; Fowler, S.E.; Goodman, L.R.; Gottschalk, A.; Hales, C.A.; Hull, R.D.; Leeper, K.V., Jr.; Popovich, J., Jr.; Quinn, D.A.; Sos, T.A.; et al. Multidetector Computed Tomography for Acute Pulmonary Embolism. N. Engl. J. Med. 2006, 354, 2317–2327. [Google Scholar] [CrossRef] [PubMed]
- Bajc, M.; Schümichen, C.; Grüning, T.; Lindqvist, A.; Le Roux, P.Y.; Alatri, A.; Bauer, R.W.; Dilic, M.; Neilly, B.; Verberne, H.J.; et al. EANM guideline for ventilation/perfusion single-photon emission computed tomography (SPECT) for diagnosis of pulmonary embolism and beyond. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 2429–2451. [Google Scholar] [CrossRef]
- Husereau, D.; Drummond, M.; Petrou, S.; Carswell, C.; Moher, D.; Greenberg, D.; Augustovski, F.; Briggs, A.H.; Mauskopf, J.; Loder, E. ISPOR Health Economic Evaluation Publication Guidelines-CHEERS Good Reporting Practices Task Force Consolidated health economic evaluation reporting standards (CHEERS)-explanation and elaboration: A report of the ISPOR health economic evaluation publication guidelines good reporting practices task force. Value Health 2013, 16, 231–250. [Google Scholar] [CrossRef]
- Ferrari, C.; Cimino, A.; Bianco, G.; Iuele, F.; Di Palo, A.; Fanelli, M.; Niccoli-Asabella, A.; Rubini, G. The impact of lung perfusion scintigraphy in the emergency management of patients with suspected pulmonary embolism. Hell. J. Nucl. Med. 2017, 20, 166. Available online: https://www.ncbi.nlm.nih.gov/pubmed/29324936 (accessed on 29 September 2020).
- Wells, P.S.; Anderson, D.R.; Rodger, M.; Stiell, I.; Dreyer, J.F.; Barnes, D.; Forgie, M.; Kovacs, G.; Ward, J.; Kovacs, M.J. Excluding Pulmonary Embolism at the Bedside without Diagnostic Imaging: Management of Patients with Suspected Pulmonary Embolism Presenting to the Emergency Department by Using a Simple Clinical Model and d -dimer. Ann. Intern. Med. 2001, 135, 98. [Google Scholar] [CrossRef] [PubMed]
- Miniati, M.; Pistolesi, M.; Marini, C.; Di Ricco, G.; Formichi, B.; Prediletto, R.; Allescia, G.; Tonelli, L.; Sostman, H.D.; Giuntini, C. Value of perfusion lung scan in the diagnosis of pulmonary embolism: Results of the Prospective Investigative Study of Acute Pulmonary Embolism Diagnosis (PISA-PED). Am. J. Respir. Crit. Care Med. 1996, 154, 1387–1393. [Google Scholar] [CrossRef]
- Yamashita, Y.; Morimoto, T.; Amano, H.; Takase, T.; Hiramori, S.; Kim, K.; Oi, M.; Akao, M.; Kobayashi, Y.; Toyofuku, M.; et al. Validation of simplified PESI score for identification of low-risk patients with pulmonary embolism: From the COMMAND VTE Registry. Eur. Hear. J. Acute Cardiovasc. Care 2020, 9, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, Y.; Morimoto, T.; Amano, H.; Takase, T.; Hiramori, S.; Kim, K.; Oi, M.; Akao, M.; Kobayashi, Y.; Toyofuku, M.; et al. Usefulness of Simplified Pulmonary Embolism Severity Index Score for Identification of Patients With Low-Risk Pulmonary Embolism and Active Cancer: From the COMMAND VTE Registry. Chest 2020, 157, 636–644. [Google Scholar] [CrossRef] [PubMed]
- Mincarone, P.; Leo, C.G.; Trujillo-Martín, M.D.; Manson, J.; Guarino, R.; Ponzini, G.; Sabina, S. Standardized languages and notations for graphical modelling of patient care processes: A systematic review. Int. J. Qual. Health Care 2018, 30, 169–177. [Google Scholar] [CrossRef]
- Ideal Modeling & Diagramming Tool for Agile Team Collaboration. Available online: https://www.visual-paradigm.com/ (accessed on 16 April 2021).
- Stein, P.D.; Matta, F.; Hughes, P.G.; Hourmouzis, Z.N.; Hourmouzis, N.P.; White, R.M.; Ghiardi, M.M.; Schwartz, M.A.; Moore, H.L.; Bach, J.A.; et al. Home Treatment of Pulmonary Embolism in the Era of Novel Oral Anticoagulants. Am. J. Med. 2016, 129, 974–977. [Google Scholar] [CrossRef] [PubMed]
- Principali Caratteristiche Diagnosis Related Groups (DRG). Available online: http://www.salute.gov.it/portale/temi/p2_6.jsp?lingua=italiano&id=1349&area=ricoveriOspedalieri&menu=sistema (accessed on 6 April 2021).
- Nomenclatore Dell’assistenza Specialistica Ambulatoriale. Available online: http://www.salute.gov.it/portale/temi/p2_6.jsp?lingua=italiano&id=1767&area=programmazioneSanitariaLea&menu=lea (accessed on 6 April 2021).
- Yoo, H.H.B.; Nunes-Nogueira, V.S.; Boas, P.J.F.V.; Broderick, C. Outpatient versus inpatient treatment for acute pulmonary embolism. Cochrane Database Syst. Rev. 2019, 2019. [Google Scholar] [CrossRef]
- Moore, A.J.E.; Wachsmann, J.; Chamarthy, M.R.; Panjikaran, L.; Tanabe, Y.; Rajiah, P. Imaging of acute pulmonary embolism: An update. Cardiovasc. Diagn. Ther. 2018, 8, 225–243. [Google Scholar] [CrossRef] [PubMed]
- Schembri, G.P.; Miller, A.E.; Smart, R. Radiation dosimetry and safety issues in the investigation of pulmonary embolism. Semin. Nucl. Med. 2010, 40, 442–454. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Bodalia, P.N.; Bryden, P.A.; Davies, P.A.; López-López, J.A.; Okoli, G.N.; Thom, H.H.; Caldwell, D.M.; Dias, S.; Eaton, D.; et al. Oral anticoagulants for primary prevention, treatment and secondary prevention of venous thromboembolic disease, and for prevention of stroke in atrial fibrillation: Systematic review, network meta-analysis and cost-effectiveness analysis. Health Technol. Assess. 2017, 21, 1–385. [Google Scholar] [CrossRef]
- Dasta, J.F.; Pilon, D.; Mody, S.H.; Lopatto, J.; Laliberté, F.; Germain, G.; Bookhart, B.K.; Lefebvre, P.; Nutescu, E.A. Daily hospitalization costs in patients with deep vein thrombosis or pulmonary embolism treated with anticoagulant therapy. Thromb. Res. 2015, 135, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Zondag, W.; Kooiman, J.; Klok, F.A.; Dekkers, O.M.; Huisman, M.V. Outpatient versus inpatient treatment in patients with pulmonary embolism: A meta-analysis. Eur. Respir. J. 2013, 2, 134–144. [Google Scholar] [CrossRef] [PubMed]
- Piran, S.; Le Gal, G.; Wells, P.S.; Gandara, E.; Righini, M.; Rodger, M.A.; Carrier, M. Outpatient treatment of symptomatic pulmonary embolism: A systematic review and meta-analysis. Thromb. Res. 2013, 132, 515–519. [Google Scholar] [CrossRef]
- Konstantinides, S.V.; Torbicki, A.; Agnelli, G.; Danchin, N.; Fitzmaurice, D.; Galiè, N.; Gibbs, J.S.R.; Huisman, M.V.; Humbert, M.; Kucher, N.; et al. ESC GUIDELINES 2014 ESC Guidelines on the diagnosis and management of acute pulmonary embolism. Eur. Heart J. 2014, 35, 3033–3069; 3069a–3069k. [Google Scholar] [CrossRef]
- Sostman, H.D.; Miniati, M.; Gottschalk, A.; Matta, F.; Stein, P.D.; Pistolesi, M. Sensitivity and specificity of perfusion scintigraphy combined with chest radiography for acute pulmonary embolism in PIOPED II. J. Nucl. Med. 2008, 49, 1741–1748. [Google Scholar] [CrossRef]
- Mazurek, A.; Dziuk, M.; Witkowska-Patena, E.; Piszczek, S.; Gizewska, A. The Utility of Hybrid SPECT/CT Lung Perfusion Scintigraphy in Pulmonary Embolism Diagnosis. Respiration 2015, 90, 393–401. [Google Scholar] [CrossRef] [PubMed]

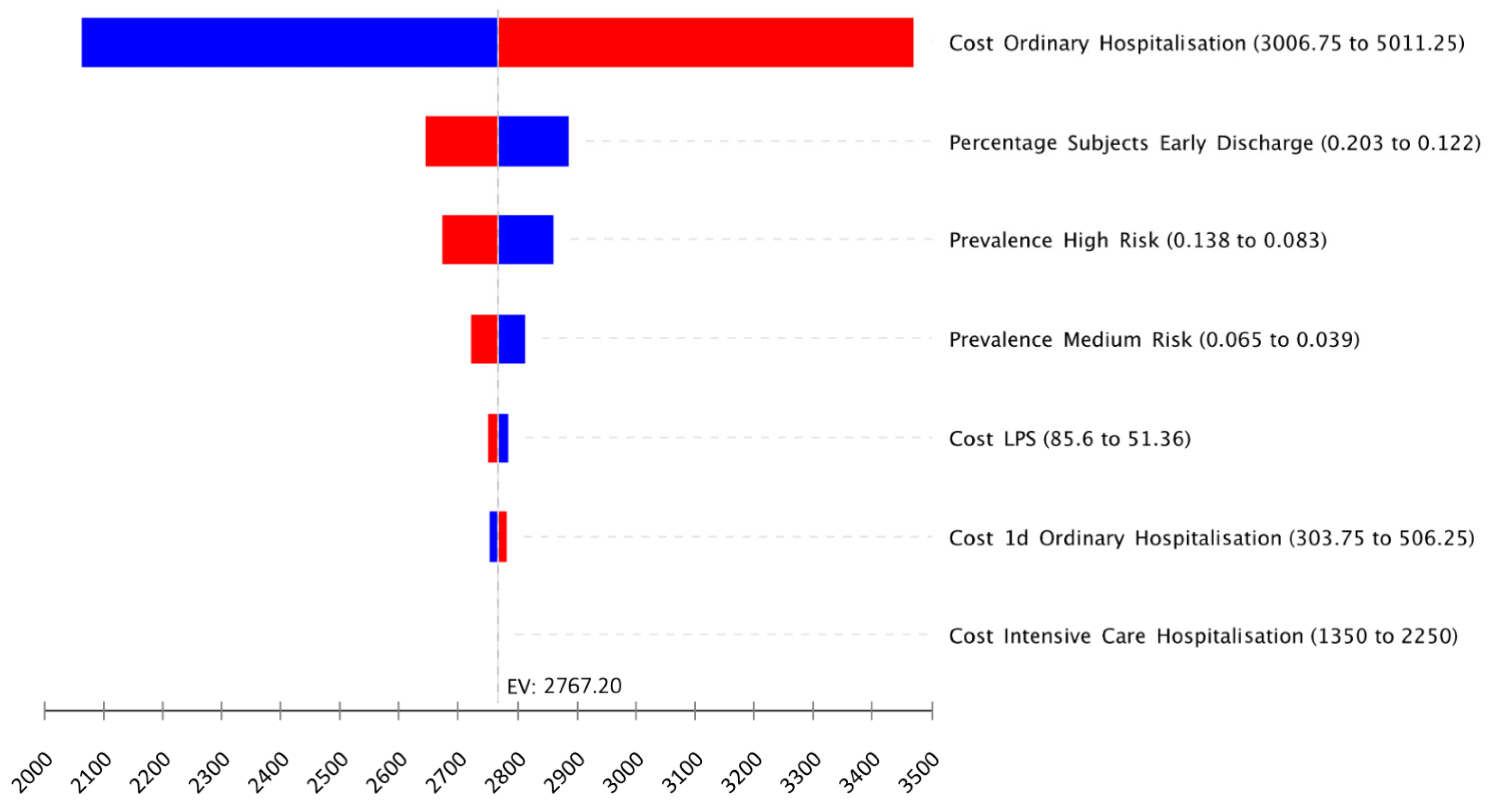

| Name | Description | Basal Value | Sensitivity Range Values (±25%) | Source |
|---|---|---|---|---|
| Prevalence high risk | Prevalence of PE subjects needing hospitalisation in ICU | 204/1846 (11.1%) | 8.3%, 13.8% | Internal retrospective data |
| Prevalence medium risk | Prevalence of PE subjects needing ordinary hospitalisation | 96/1846 (5.2%) | 3.9%, 6.5% | Internal retrospective data |
| Percentage of subjects with early discharge | Percentage of subjects in ordinary hospitalisation who are discharged early, which determines a low fare | 16.2% | 12.2%, 20.3% | Stein et al. [17] |
| Daily cost of intensive care hospitalisation | Daily cost of hospitalisation for pulmonary embolism for patients requiring intensive care | EUR 1800 | EUR 1350.00, EUR 2250.00 | Expert opinion |
| Duration of intensive care hospitalisation | Number of days of hospitalisation for pulmonary embolism for patients requiring intensive care (average number) | 7 days | / | Expert opinion |
| Cost of 1-day ordinary hospitalisation | Cost of the DRG 78 (pulmonary embolism) for patients discharged after 1 day | EUR 405 | 303.75 €, 506.25 € | Italian National Fares [18] |
| Cost of ordinary hospitalisation | Cost of the DRG 78 (pulmonary embolism) in ordinary hospitalisation | EUR 4009 | EUR 3006.75, EUR 5011.25 | Italian National Fares [18] |
| Cost of lung perfusion scintigraphy | Cost for executing an ordinary scintigraphy (i.e., during the morning regimen) | EUR 68.48 | EUR 51.36, EUR 85.60 | Italian National Fares [19] |
| Additional cost of pulmonary scintigraphy in emergency | Additional cost for executing an ordinary scintigraphy (i.e., during the evening/night regimen) | EUR 41.32 | EUR 30.99, EUR 51.65 | Internal retrospective data |
| Cost of SPET/CT supplemented LPS | The additional cost of an LPS when executed with SPET or SPET/CT | EUR 34.71 | EUR 26.03, EUR 43.39 | Italian National Fares [19] |
| Percentage of subjects with nondiagnostic LPS | Percentage of subjects with a nondiagnostic LPS that requires LPS complemented with SPET or SPET/CT | 20% | 15.0%, 25.0% | Internal retrospective data |
| Percentage of LPS in emergency | Percentage of LPS instances executed during the emergency timeframe | 1157/1846 (62.7%) | 47.0%, 78.3% | Internal retrospective data |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rubini, G.; Ferrari, C.; Mammucci, P.; Pisani, A.R.; Mincarone, P.; Leo, C.G. Healthcare and Economic Impact of Lung Perfusion Scintigraphy in Patients Affected by Acute Pulmonary Embolism. Healthcare 2021, 9, 716. https://doi.org/10.3390/healthcare9060716
Rubini G, Ferrari C, Mammucci P, Pisani AR, Mincarone P, Leo CG. Healthcare and Economic Impact of Lung Perfusion Scintigraphy in Patients Affected by Acute Pulmonary Embolism. Healthcare. 2021; 9(6):716. https://doi.org/10.3390/healthcare9060716
Chicago/Turabian StyleRubini, Giuseppe, Cristina Ferrari, Paolo Mammucci, Antonio Rosario Pisani, Pierpaolo Mincarone, and Carlo Giacomo Leo. 2021. "Healthcare and Economic Impact of Lung Perfusion Scintigraphy in Patients Affected by Acute Pulmonary Embolism" Healthcare 9, no. 6: 716. https://doi.org/10.3390/healthcare9060716
APA StyleRubini, G., Ferrari, C., Mammucci, P., Pisani, A. R., Mincarone, P., & Leo, C. G. (2021). Healthcare and Economic Impact of Lung Perfusion Scintigraphy in Patients Affected by Acute Pulmonary Embolism. Healthcare, 9(6), 716. https://doi.org/10.3390/healthcare9060716







