Relationship of Physical Activity and Sedentary Time with Metabolic Health in Children and Adolescents Measured by Accelerometer: A Narrative Review
Abstract
1. Introduction
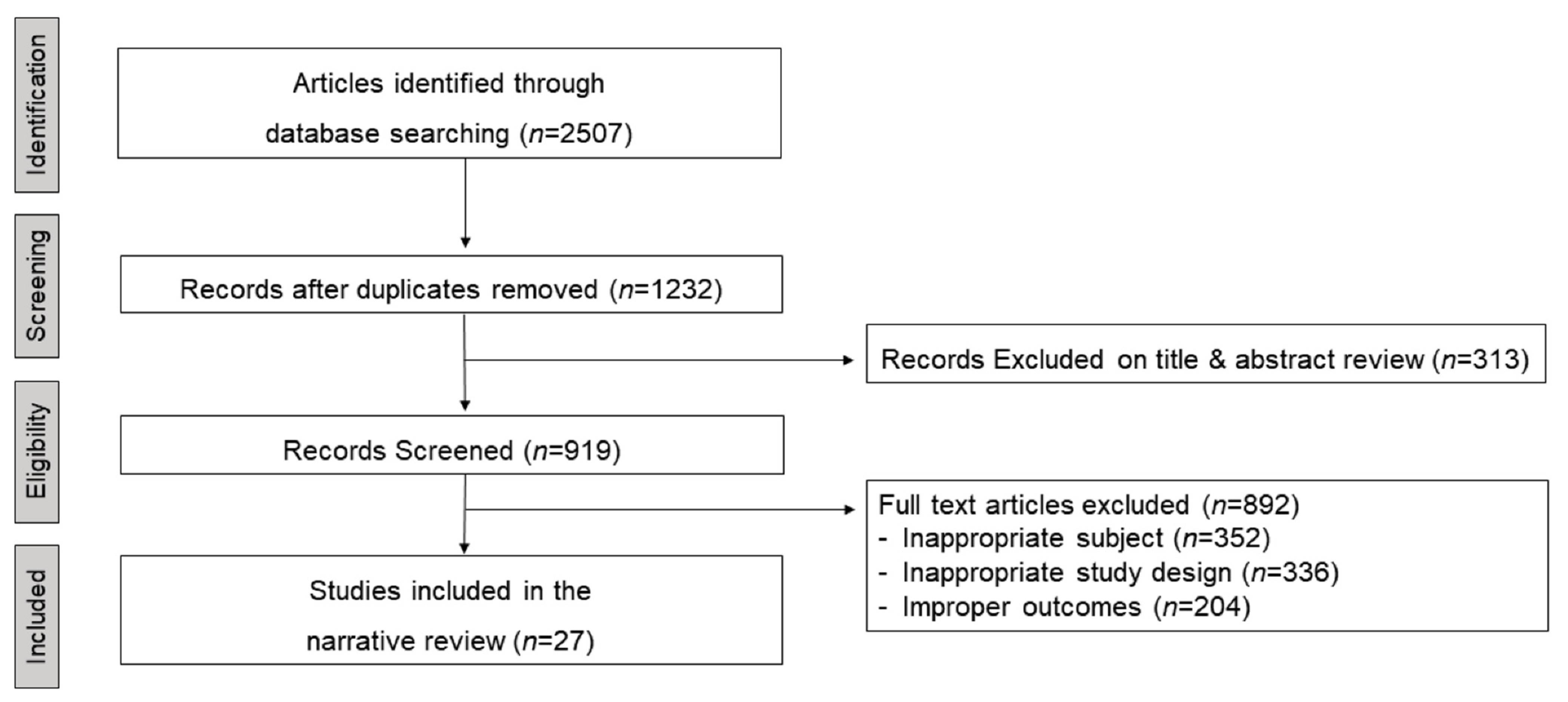
2. Methods
3. Results
3.1. Physical Activity, Sedentary Time, and Metabolic Health
3.1.1. Markers of Obesity
3.1.2. Blood Pressure
3.1.3. Blood Lipids
3.1.4. Glucose and Insulin
3.2. Effects of Replacing Sedentary Time with Physical Activity on Metabolic Health
3.2.1. Markers of Obesity
3.2.2. Blood Pressure
3.2.3. Blood Lipids
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- 2018 Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report; US Department of Health and Human Services: Washington, DC, USA, 2018.
- Child and Adolescent Health Measurement Initiative. 2016 National Survey of Children’s Health (NSCH) data query. Data Resource Center for Child and Adolescent Health supported by the U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB). Available online: https://www.childhealthdata.org/browse/survey/results?q=5190&r=1 (accessed on 13 March 2021).
- National Health and Nutrition Examination Survey (NHANES) 2015-16 Public Data General Release File Documentation. 2016. Available online: https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.aspx?BeginYear=2015 (accessed on 9 June 2021).
- Saunders, T.J.; Tremblay, M.S.; Mathieu, M.-È.; Henderson, M.; O’Loughlin, J.; Tremblay, A.; Chaput, J.-P.; on behalf of the QUALITY Cohort Research Group. Associations of Sedentary Behavior, Sedentary Bouts and Breaks in Sedentary Time with Cardiometabolic Risk in Children with a Family History of Obesity. PLoS ONE 2013, 8, e79143. [Google Scholar] [CrossRef] [PubMed]
- Berk, L. Child Development; Allyn and Bacon: Boston, MA, USA, 2006. [Google Scholar]
- Levine, J.; Bine, L. Helping Your Child Lose Weight the Healthy Way: A Family Approach to Weight Control. J. Am. Diet. Assoc. 1997, 97, A46. [Google Scholar] [CrossRef]
- Baker, J.L.; Olsen, L.W.; Sørensen, T.I.A. Childhood Body-Mass Index and the Risk of Coronary Heart Disease in Adulthood. N. Engl. J. Med. 2007, 357, 2329–2337. [Google Scholar] [CrossRef] [PubMed]
- Güngör, N.K. Overweight and obesity in children and adolescents. J Clin Res. Pediatr. Endocrinol. 2014, 6, 129–143. [Google Scholar] [CrossRef] [PubMed]
- Lindberg, L.; Danielsson, P.; Persson, M.; Marcus, C.; Hagman, E. Association of childhood obesity with risk of early all-cause and cause-specific mortality: A Swedish prospective cohort study. PLoS Med. 2020, 17, e1003078. [Google Scholar] [CrossRef] [PubMed]
- Telama, R.; Yang, X.; Viikari, J.; Välimäki, I.; Wanne, O.; Raitakari, O. Physical activity from childhood to adulthood: A 21-year tracking study. Am. J. Prev. Med. 2005, 28, 267–273. [Google Scholar] [CrossRef]
- Ainsworth, B.; Cahalin, L.; Buman, M.; Ross, R. The current state of physical activity assessment tools. Prog. Cardiovasc. Dis. 2015, 57, 387–395. [Google Scholar] [CrossRef]
- Adams, S.A.; Matthews, C.E.; Ebbeling, C.B.; Moore, C.G.; Cunningham, J.E.; Fulton, J.; Hebert, J.R. The Effect of Social Desirability and Social Approval on Self-Reports of Physical Activity. Am. J. Epidemiol. 2005, 161, 389–398. [Google Scholar] [CrossRef]
- Coughlin, S.S. Recall bias in epidemiologic studies. J. Clin. Epidemiol. 1990, 43, 87–91. [Google Scholar] [CrossRef]
- Sallis, J.F.; Saelens, B.E. Assessment of Physical Activity by Self-Report: Status, Limitations, and Future Directions. Res. Q. Exerc. Sport 2000, 71, 1–14. [Google Scholar] [CrossRef]
- Freedson, P.S.; Melanson, E.; Sirard, J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med. Sci. Sports Exerc. 1998, 30, 777–781. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.-M.; Shiroma, E.J.; Evenson, K.R.; Kamada, M.; LaCroix, A.Z.; Buring, J.E. Using Devices to Assess Physical Activity and Sedentary Behavior in a Large Cohort Study: The Women’s Health Study. J. Meas. Phys. Behav. 2018, 1, 60. [Google Scholar] [CrossRef]
- Migueles, J.H.; Cadenas-Sanchez, C.; Ekelund, U.; Delisle Nyström, C.; Mora-Gonzalez, J.; Löf, M.; Labayen, I.; Ruiz, J.R.; Ortega, F.B. Accelerometer Data Collection and Processing Criteria to Assess Physical Activity and Other Outcomes: A Systematic Review and Practical Considerations. Sports Med. 2017, 47, 1821–1845. [Google Scholar] [CrossRef] [PubMed]
- Colley, R.C.; Butler, G.; Garriguet, D.; Prince, S.A.; Roberts, K.C. Comparison of self-reported and accelerometer-measured physical activity among Canadian youth. Health Rep. 2019, 30, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Lim, J.; Mun, J.; Kim, Y. Objective versus Self-Reported Physical Activity and Cardiovascular Disease Risk Factors. Korean J. Sports Med. 2020, 38, 28–36. [Google Scholar] [CrossRef]
- Tucker, J.M.; Welk, G.J.; Beyler, N.K.; Kim, Y. Associations between Physical Activity and Metabolic Syndrome: Comparison between Self-Report and Accelerometry. Am. J. Health Promot. 2016, 30, 155–162. [Google Scholar] [CrossRef]
- Mekary, R.A.; Willett, W.C.; Hu, F.B.; Ding, E.L. Isotemporal Substitution Paradigm for Physical Activity Epidemiology and Weight Change. Am. J. Epidemiol. 2009, 170, 519–527. [Google Scholar] [CrossRef]
- Grgic, J.; Dumuid, D.; Bengoechea, E.G.; Shrestha, N.; Bauman, A.; Olds, T.; Pedisic, Z. Health outcomes associated with reallocations of time between sleep, sedentary behaviour, and physical activity: A systematic scoping review of isotemporal substitution studies. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 69. [Google Scholar] [CrossRef] [PubMed]
- Evenson, K.R.; Catellier, D.J.; Gill, K.; Ondrak, K.S.; McMurray, R.G. Calibration of two objective measures of physical activity for children. J. Sports Sci. 2008, 26, 1557–1565. [Google Scholar] [CrossRef]
- Pate, R.R.; Almeida, M.J.; McIver, K.L.; Pfeiffer, K.A.; Dowda, M. Validation and Calibration of an Accelerometer in Preschool Children. Obesity 2006, 14, 2000–2006. [Google Scholar] [CrossRef] [PubMed]
- Freedson, P.; Pober, D.; Janz, K.F. Calibration of accelerometer output for children. Med. Sci. Sports Exerc. 2005, 37, S523–S530. [Google Scholar] [CrossRef]
- Troiano, R.P.; Berrigan, D.; Dodd, K.W.; Masse, L.C.; Tilert, T.; McDowell, M. Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exerc. 2008, 40, 181. [Google Scholar] [CrossRef]
- Aadland, E.; Kvalheim, O.M.; Hansen, B.H.; Kriemler, S.; Ried-Larsen, M.; Wedderkopp, N.; Sardinha, L.B.; Møller, N.C.; Hallal, P.C.; Anderssen, S.A.; et al. The multivariate physical activity signature associated with metabolic health in children and youth: An International Children’s Accelerometry Database (ICAD) analysis. Prev. Med. 2020, 141, 106266. [Google Scholar] [CrossRef]
- Aadland, E.; Andersen, L.B.; Anderssen, S.A.; Resaland, G.K.; Kvalheim, O.M. Associations of volumes and patterns of physical activity with metabolic health in children: A multivariate pattern analysis approach. Prev. Med. 2018, 115, 12–18. [Google Scholar] [CrossRef]
- Bell, J.A.; Hamer, M.; Richmond, R.C.; Timpson, N.J.; Carslake, D.; Davey Smith, G. Associations of device-measured physical activity across adolescence with metabolic traits: Prospective cohort study. PLoS Med. 2018, 15, e1002649. [Google Scholar] [CrossRef]
- Carson, V.; Stone, M.; Faulkner, G. Patterns of Sedentary Behavior and Weight Status Among Children. Pediatric Exerc. Sci. 2014, 26, 95. [Google Scholar] [CrossRef]
- Carson, V.; Janssen, I. Volume, patterns, and types of sedentary behavior and cardio-metabolic health in children and adolescents: A cross-sectional study. BMC Public Health 2011, 11, 274. [Google Scholar] [CrossRef]
- Chinapaw, M.J.M.; Yıldırım, M.; Altenburg, T.M.; Singh, A.S.; Kovács, É.; Molnár, D.; Brug, J. Objective and Self-Rated Sedentary Time and Indicators of Metabolic Health in Dutch and Hungarian 10–12 Year Olds: The ENERGY-Project. PLoS ONE 2012, 7, e36657. [Google Scholar] [CrossRef] [PubMed]
- Colley, R.C.; Garriguet, D.; Janssen, I.; Wong, S.L.; Saunders, T.J.; Carson, V.; Tremblay, M.S. The association between accelerometer-measured patterns of sedentary time and health risk in children and youth: Results from the Canadian Health Measures Survey. BMC Public Health 2013, 13, 200. [Google Scholar] [CrossRef] [PubMed]
- Colley, R.C.; Wong, S.L.; Garriguet, D.; Janssen, I.; Gorber, S.C.; Tremblay, M.S. Physical activity, sedentary behaviour and sleep in Canadian children: Parent-report versus direct measures and relative associations with health risk. Health Rep. 2012, 23, A1. [Google Scholar]
- Dalene, K.E.; Anderssen, S.A.; Andersen, L.B.; Steene-Johannessen, J.; Ekelund, U.; Hansen, B.H.; Kolle, E. Cross-sectional and prospective associations between physical activity, body mass index and waist circumference in children and adolescents. Obes. Sci. Pract. 2017, 3, 249–257. [Google Scholar] [CrossRef] [PubMed]
- del Pozo-Cruz, B.; Gant, N.; del Pozo-Cruz, J.; Maddison, R. Relationships between sleep duration, physical activity and body mass index in young New Zealanders: An isotemporal substitution analysis. PLoS ONE 2017, 12, e0184472. [Google Scholar] [CrossRef]
- Ekelund, U.; Anderssen, S.A.; Froberg, K.; Sardinha, L.B.; Andersen, L.B.; Brage, S.; European Youth Heart Study, G. Independent associations of physical activity and cardiorespiratory fitness with metabolic risk factors in children: The European youth heart study. Diabetologia 2007, 50, 1832–1840. [Google Scholar] [CrossRef] [PubMed]
- Hansen, B.H.; Anderssen, S.A.; Andersen, L.B.; Hildebrand, M.; Kolle, E.; Steene-Johannessen, J.; Kriemler, S.; Page, A.S.; Puder, J.J.; Reilly, J.J.; et al. Cross-Sectional Associations of Reallocating Time Between Sedentary and Active Behaviours on Cardiometabolic Risk Factors in Young People: An International Children’s Accelerometry Database (ICAD) Analysis. Sports Med. 2018, 48, 2401–2412. [Google Scholar] [CrossRef] [PubMed]
- Katzmarzyk, P.T.; Barreira, T.V.; Broyles, S.T.; Champagne, C.M.; Chaput, J.P.; Fogelholm, M.; Hu, G.; Johnson, W.D.; Kuriyan, R.; Kurpad, A. Physical activity, sedentary time, and obesity in an international sample of children. Med. Sci. Sports Exerc. 2015, 47, 2062–2069. [Google Scholar] [CrossRef]
- Kuzik, N.; Carson, V.; Andersen, L.B.; Sardinha, L.B.; Grøntved, A.; Hansen, B.H.; Ekelund, U.; The International Children’s Accelerometry Database (ICAD) Collaborators. Physical Activity and Sedentary Time Associations with Metabolic Health Across Weight Statuses in Children and Adolescents. Obesity 2017, 25, 1762–1769. [Google Scholar] [CrossRef]
- Loprinzi, P.D.; Cardinal, B.J.; Lee, H.; Tudor-Locke, C. Markers of adiposity among children and adolescents: Implications of the isotemporal substitution paradigm with sedentary behavior and physical activity patterns. J. Diabetes Metab. Disord. 2015, 14, 46. [Google Scholar] [CrossRef]
- Mitchell, J.A.; Pate, R.R.; Beets, M.W.; Nader, P.R. Time spent in sedentary behavior and changes in childhood BMI: A longitudinal study from ages 9 to 15 years. Int. J. Obes. 2013, 37, 54–60. [Google Scholar] [CrossRef]
- Moore, J.B.; Beets, M.W.; Brazendale, K.; Blair, S.N.; Pate, R.R.; Andersen, L.B.; Anderssen, S.A.; Grøntved, A.; Hallal, P.C.; Kordas, K.; et al. Associations of Vigorous-Intensity Physical Activity with Biomarkers in Youth. Med. Sci. Sports Exerc. 2017, 49, 1366–1374. [Google Scholar] [CrossRef]
- Moura, B.P.; Rufino, R.L.; Faria, R.C.; Amorim, P.R.S. Effects of isotemporal substitution of sedentary behavior with light-intensity or moderate-to-vigorous physical activity on cardiometabolic markers in male adolescents. PLoS ONE 2019, 14, e0225856. [Google Scholar] [CrossRef]
- Moura, B.P.; Rufino, R.L.; Faria, R.C.; Sasaki, J.E.; Amorim, P.R.S. Can Replacing Sitting Time with Standing Time Improve Adolescents’ Cardiometabolic Health? Int. J. Environ. Res. Public Health 2019, 16, 3115. [Google Scholar] [CrossRef]
- Nguyen, T.H.H.D.; Tang, H.K.; Kelly, P.; van der Ploeg, H.P.; Dibley, M.J. Association between physical activity and metabolic syndrome: A cross sectional survey in adolescents in Ho Chi Minh City, Vietnam. BMC Public Health 2010, 10, 141. [Google Scholar] [CrossRef]
- Rendo-Urteaga, T.; de Moraes, A.C.F.; Collese, T.S.; Manios, Y.; Hagströmer, M.; Sjöström, M.; Kafatos, A.; Widhalm, K.; Vanhelst, J.; Marcos, A.; et al. The combined effect of physical activity and sedentary behaviors on a clustered cardio-metabolic risk score: The Helena study. Int. J. Cardiol. 2015, 186, 186–195. [Google Scholar] [CrossRef]
- Stockwell, S.L.; Smith, L.R.; Weaver, H.M.; Hankins, D.J.; Bailey, D.P. Associations of Sitting Behavior Patterns With Cardiometabolic Risk in Children: The Sit Less for Health Cross-Sectional Study. J. Phys. Act. Health 2019, 16, 836. [Google Scholar] [CrossRef] [PubMed]
- Strizich, G.; Kaplan, R.C.; Sotres-Alvarez, D.; Diaz, K.M.; Daigre, A.L.; Carnethon, M.R.; Vidot, D.C.; Delamater, A.M.; Perez, L.; Perreira, K.; et al. Objectively Measured Sedentary Behavior, Physical Activity, and Cardiometabolic Risk in Hispanic Youth: Hispanic Community Health Study/Study of Latino Youth. J. Clin. Endocrinol. Metab. 2018, 103, 3289–3298. [Google Scholar] [CrossRef]
- Treuth, M.S.; Hou, N.; Young, D.R.; Maynard, L.M. Accelerometry-Measured Activity or Sedentary Time and Overweight in Rural Boys and Girls. Obes. Res. 2005, 13, 1606–1614. [Google Scholar] [CrossRef]
- Verswijveren, S.J.J.M.; Salmon, J.; Daly, R.M.; Arundell, L.; Cerin, E.; Dunstan, D.W.; Hesketh, K.D.; Della Gatta, P.A.; Ridgers, N.D. Reallocating sedentary time with total physical activity and physical activity bouts in children: Associations with cardiometabolic biomarkers. J. Sports Sci. 2021, 39, 332–340. [Google Scholar] [CrossRef] [PubMed]
- White, D.A.; Oh, Y.; Willis, E.A. The Effect of Physical Activity Bout Patterns on Metabolic Syndrome Risk Factors in Youth: National Health and Nutrition Examination Survey 2003–2006. J. Phys. Act. Health 2019, 16, 12. [Google Scholar] [CrossRef]
| Reference | Study Design | Country, n (Sample Size), Age | Outcome | Result |
|---|---|---|---|---|
| Aadland et al. [28] | CS | Brazil/Denmark/Estonia/Norway/Portugal/Switzerland/UK/US, 11,853, 6–18 Y | BMI, WC, SBP, TC, TG, HDL-C, glucose, insulin, HOMA | Associations with the composite metabolic health score were weak for SED and LPA but gradually strengthened with increasing time spent in moderate and vigorous-intensity PA (up to 4000–5000 CPM). |
| Aadland et al. [29] | CS | Norway, 841, 5th grade (10.2 ± 0.3 Y) | BMI, WC, BP, TC, TG, HDL-C, glucose, insulin, LDL-C, HOMA | The strongest associations with metabolic health were found for VPA, while weaker associations were found for MPA and LPA, and no associations were found for SED. |
| Bell et al. [30] | Cohort | UK, 1826, 12–15 Y | BMI, BP, TC, TG, HDL-C, LDL-C, glucose, insulin, CRP | The associations of PA with metabolic traits were small and more robust for higher MVPA than lower SED. The activity was most strongly associated with cholesterol content in VLDL-C and HDL lipoprotein particles, with TG content in all particle types. |
| Carson et al. [31] | CS | Canada, 787, 11 Y | BMI | No association was observed between SED and BMI z-score. Conversely, MVPA was consistently associated with BMI z-score. |
| Carson & Janssen [32] | CS | US, 2527, 6–19 Y | WC, SBP, non-HDL-C, CRP | No association was observed between overall volume and patterns of SED with cardiometabolic risk factors. Conversely, high television watching and low MVPA were independently associated with cardiometabolic risk factors. |
| Chinapaw et al. [33] | CS | Hungary/Netherlands, 142, 10–13 Y | BMI, WC, TC, TG, HDL-C, LDL-C, glucose, C-peptide | Although BMI and WC were higher in the most sedentary versus the least sedentary children, no further evidence was found to support that more sedentary children were at increased metabolic risk. |
| Colley et al. [34] | CS | Canada, 799, 6–19 Y | BMI, WC, BP, non-HDL-C | SED accumulated during the after-school period was associated with BMI and WC, independent of MVPA, in boys aged 11–14 years. No sedentary behavior variables were independently associated with any health marker in older or younger boys or girls of any age. |
| Colley et al. [35] | CS | Canada, 878, 6–11 Y | BMI, WC, BP, non-HDL-C | Directly measured MVPA and sleep were significantly associated with BMI, directly measured MVPA was significantly associated with WC. |
| Dalene et al. [36] | CS | Norway, 970 (6 Y)/ 2423 (9 Y)/1544 (15 Y) | BMI, WC | Substituting 10 min/day of SED with LPA was associated with higher WC in all age groups. Substituting 10 min/day of SED with MPA was associated with lower WC in 6- and 9-year-olds. Substituting 10 min/day of SED with VPA was associated with lower WC in 9- and 15-year-olds. Associations were similar with BMI as the outcome. In prospective analyses, substituting SED with LPA, MPA, or VPA at age 9 was not associated with BMI or WC at age 15. |
| del Pozo-Cruz et al. [37] | CS | New Zealand, 1812, 5–24 Y | BMI, sleep time | MVPA and SED were found to have a unique effect on BMI. Further, substituting SED with LPA or MVPA was associated with a favorable effect on BMI across all age groups, with MVPA having the strongest association. |
| Ekelund et al. [38] | CS | Denmark, 1092 (9–10 Y)/829 (15–16 Y) | BMI, WC, skinfold thickness (triceps, biceps, subscapular, suprailiac), BP, TG, HDL-C, glucose, insulin, CRF (ergometer cycle test) | PA and CRF were found to be separately and independently associated with individual and clustered metabolic risk factors in children. |
| Hansen et al. [39] | CS | 10 countries, 10,836 (10–14.9 Y)/ 2393 (15–18.4 Y) | WC, BP, TG, HDL-C, LDL-C, glucose, insulin | Replacing SED and/or LPA with MVPA in children and adolescents was favorably associated with most markers of cardiometabolic risk. Efforts were aimed at replacing SED with active behaviors, particularly those of at least moderate intensity. |
| Katzmarzyk et al. [40] | CS | Australia/Brazil/Canada/ China/Colombia/Finland/ India/Kenya/Portugal/ South Africa/UK/US, 6539, 9–11 Y | BMI | Greater MVPA and VPA were both associated with lower odds of obesity independent of SED. SED was positively associated with obesity, but not independent of MVPA. |
| Kuzik et al. [41] | CS | Denmark/Estonia/Portugal/US, 4581, 5–18 Y | BMI, BP, TG, HDL-C, glucose, HOMA-IR | More MVPA was beneficial for metabolic health and weight status, whereas lower SED was beneficial for metabolic health alone, although associations were weak. |
| Loprinzi et al. [42] | CS | US, 2644, 6–17 Y | Height, weight, WC, %BF (by DEXA), skinfold thickness (triceps, subscapular), energy intake | The low proportion of children engaging in ≥ 60 min/day of MVPA and accumulating relatively more LPA than SED had the lowest DXA-BF%. |
| Mitchell et al. [43] | LS | US, 789, 9–15 Y | BMI | SED was associated with greater increases in BMI at the 90th, 75th, and 50th BMI percentiles between ages 9 and 15 years, independent of MVPA. No associations were observed between SED and changes at the 25th and 10th BMI percentiles. |
| Moore et al. [44] | LS | Brazil/Europe/ US, 11,588, 4–18 Y | WC, BP, TG, HDL-C, LDL-C, glucose, insulin | Substituting LPA with VPA was inversely associated with WC and insulin. However, VPA was inconsistently related to the remaining biomarkers after controlling for SED and MPA. |
| Moura et al. [45] | CS | Brazil, 84 (male), 14–18 Y | BMI, WC, BF%, BP, TC, TG, HDL-C, LDL-C, glucose, insulin, HOMA-IR, HOMA-β, HOMA2-S | Replacing SED with LPA showed positive results in HDL-C, HOMA2-S, and SBP, while replacing SED with MVPA was associated with only one obesity indicator (BF%). |
| Moura et al. [46] | CS | Brazil, 84 (male), 14–18 Y | BMI, WC, skinfold thickness (triceps), FM, TC, TG, HDL-C, LDL-C, non-HDL-C, HOMA-IR, HOMA-β, HOMA2-S | Sitting less and standing more may be an effective method to reduce cardiometabolic biomarker levels related to lipid metabolism (TC, TG, Non-HDL-C, LDL-C), regardless of MVPA. |
| Nguyen et al. [47] | CS | Vietnam, 617, high school students (13.9 ± 0.7 Y) | BMI, WC, BP, skinfold thickness (triceps, subscapular, abdominal, medial calf), TG, HDL-C, LDL-C | Elevated BP was the most common individual component of metabolic syndrome (21.5%), followed by hypertriglyceridemia (11.1%). The odds of metabolic syndrome among youth in the lowest PA group (<43 min of PA/day) were five times higher than those in the highest PA group (>103 min/day). |
| Rendo-Urteaga et al. [48] | CS | Austria/Belgium/France/ Germany/Greece/Hungary/Italy/Spain/Sweden, 769, 12.5–17.5 Y | BMI, WC, BP, skinfold thickness (biceps, triceps, subscapular, suprailiac), TC, TG, HDL-C, insulin, HOMA-IR, CRF (20 m shuttle run test) | A positive association was found between “PA ≥ 60 min/d; SED ≥ 2 h” and the ratio TC/HDL-c; a negative association was found between “MVPA ≥ 60 min/d; SED < 2 h” and ∑4Skinfolds. “SED ≥ 2 h/d” was associated with increased cardiometabolic risk, while “PA ≥ 60 min/d; SED < 2 h” had a protective effect against cardiometabolic risk. Adolescents should be encouraged to decrease SED and increase PA, especially VPA, to reduce cardiometabolic risk. |
| Saunders et al. [5] | CS | Canada, 522, 8–11 Y | BMI, WC, BP, TG, HDL-C, glucose, insulin, hs-CRP | Breaks in SED and the number of sedentary bouts lasting 1–4 min were associated with a reduced cardiometabolic risk score, lower BMI z-score in both sexes. The number of sedentary bouts lasting 5–9 min was negatively associated with WC in girls only, while those lasting 10–14 min was positively associated with fasting glucose in girls, with a BMI z-score in boys. |
| Stockwell et al. [49] | CS | UK, 118, 11–12 Y | BMI, WC, BF%, BP, TC, HDL-C, LDL-C, glucose | The number of breaks in sitting per day was significantly negatively associated with weight, BMI, WC, and %BF and significantly positively associated with TC and HDL. Total time spent in prolonged sitting bouts was significantly negatively associated with weight, BMI, WC, and %BF, and significantly positively associated with TC and HDL in both regression models. |
| Strizich et al. [50] | CS | US, 1426, 8–16 Y | BMI, WC, BP, TG, HDL-C, LDL-C, glucose, insulin, HbA1c, HOMA-IR, hs-CRP, inhibitor-1, E-selectin, sRAGE | Deleterious levels of HDL-C, TG, IR, CRP, and plasminogen activator inhibitor-1 were associated with lower levels of MVPA and higher levels of SED. |
| Treuth et al. [51] | CS | US, 130, 7–19 Y | BMI, FM, FFM, BF% | No associations between measures of body composition and time spent in an activity level were seen in boys. FM and BF% were positively correlated to SED for girls. In contrast, FM and BF% were negatively related to time spent in LPA for girls. |
| Verswijveren et al. [52] | CS | Australia, 169, 8–9 Y | TC, TG, HDL-C, LDL-C, IR, HOMA-IR | Replacing 10 min of SED with VPA was associated with lower TG in the whole sample. Replacing SED with VPA was associated with better HDL-C and TG in children with healthy weight. Replacing SED with MPA was associated with better HOMA-IR and HDL-C in children with a healthy weight and overweight, respectively. Substituting SED with VPA specifically accumulated in ≥1-min bouts was detrimentally associated with HOMA-IR in children with a healthy weight, but beneficially with the cardiometabolic summary score in the overweight sample. |
| White et al. [53] | CS | US, 3165, 6–18 Y | BMI, WC, WHR, BP, TC, TG, HDL-C, LDL-C, glucose, insulin | Longer continuous bouts of MVPA had lower BMI percentile, WC, WC percentile, and WHR than participating in shorter bouts of MVPA. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lim, J.; Kim, J.-S.; Park, S.; Lee, O.; So, W.-Y. Relationship of Physical Activity and Sedentary Time with Metabolic Health in Children and Adolescents Measured by Accelerometer: A Narrative Review. Healthcare 2021, 9, 709. https://doi.org/10.3390/healthcare9060709
Lim J, Kim J-S, Park S, Lee O, So W-Y. Relationship of Physical Activity and Sedentary Time with Metabolic Health in Children and Adolescents Measured by Accelerometer: A Narrative Review. Healthcare. 2021; 9(6):709. https://doi.org/10.3390/healthcare9060709
Chicago/Turabian StyleLim, Jungjun, Joon-Sik Kim, Soyoung Park, On Lee, and Wi-Young So. 2021. "Relationship of Physical Activity and Sedentary Time with Metabolic Health in Children and Adolescents Measured by Accelerometer: A Narrative Review" Healthcare 9, no. 6: 709. https://doi.org/10.3390/healthcare9060709
APA StyleLim, J., Kim, J.-S., Park, S., Lee, O., & So, W.-Y. (2021). Relationship of Physical Activity and Sedentary Time with Metabolic Health in Children and Adolescents Measured by Accelerometer: A Narrative Review. Healthcare, 9(6), 709. https://doi.org/10.3390/healthcare9060709






