Correction of Breech Presentation with Moxibustion and Acupuncture: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection and Data Extraction
2.3. Assessment of the Risk of Bias in Included Studies
2.4. Data Synthesis and Statistical Analysis
3. Results
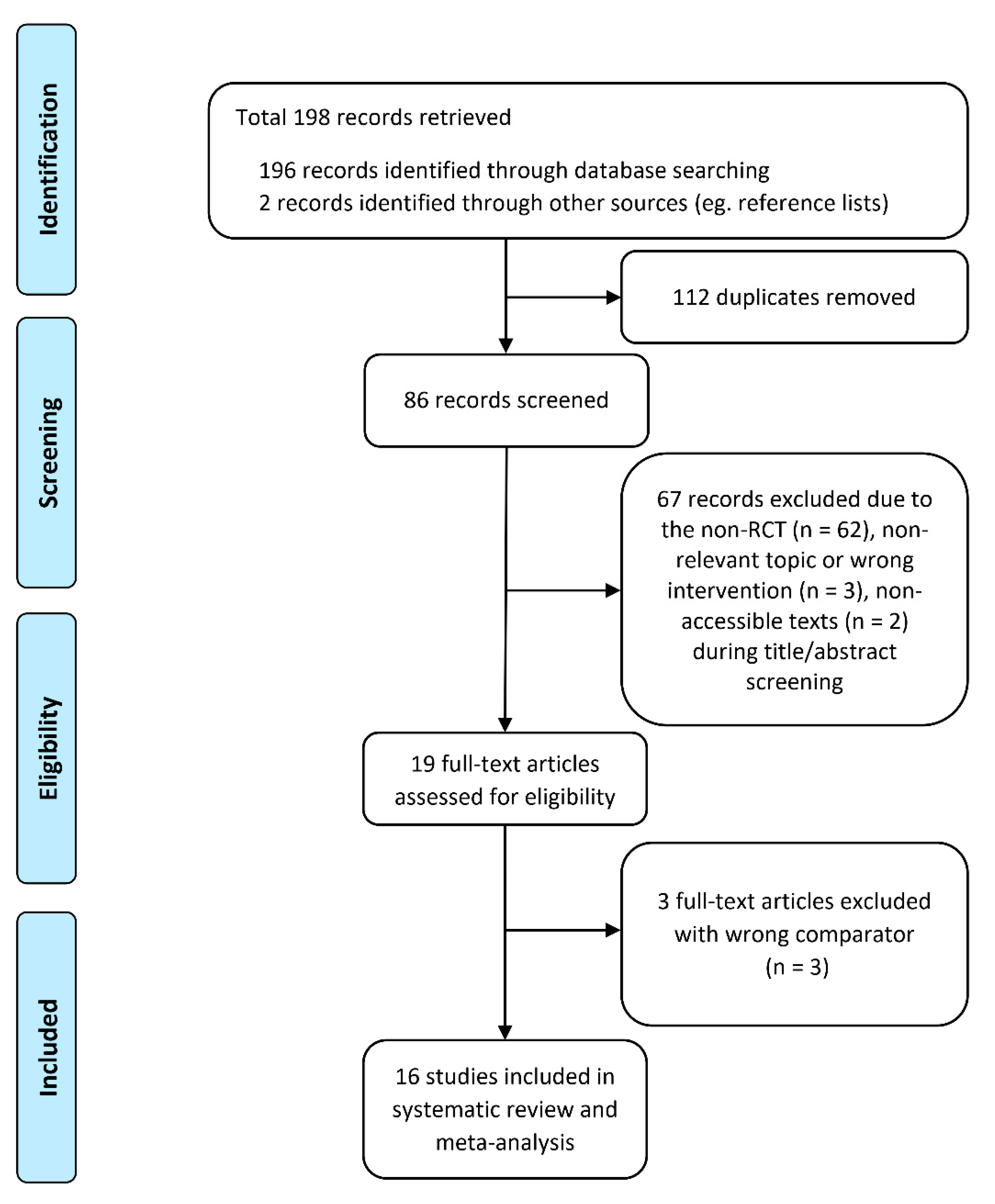
3.1. Study Selection and Characteristics
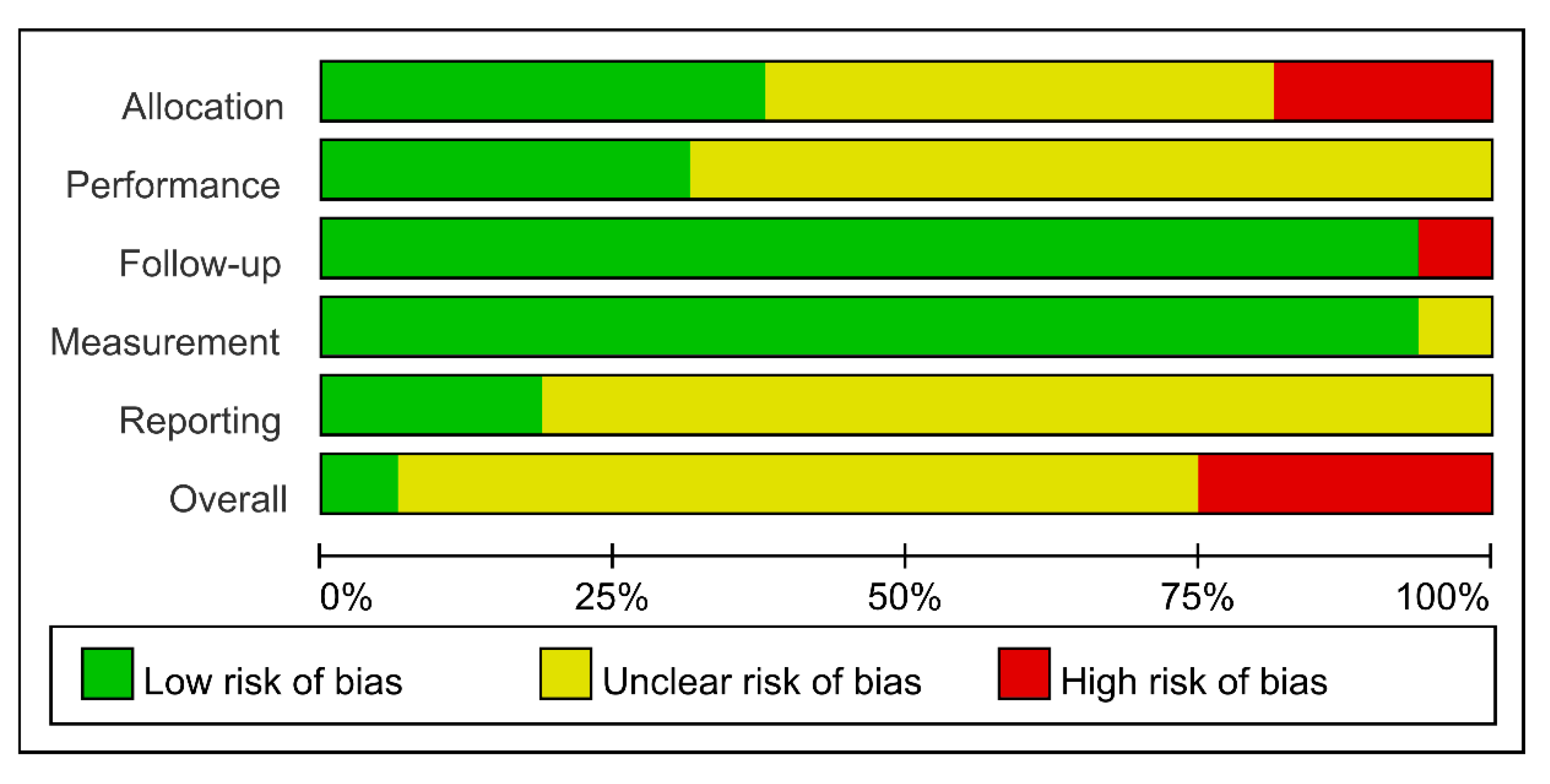
3.2. Methodological Quality of Included Studies
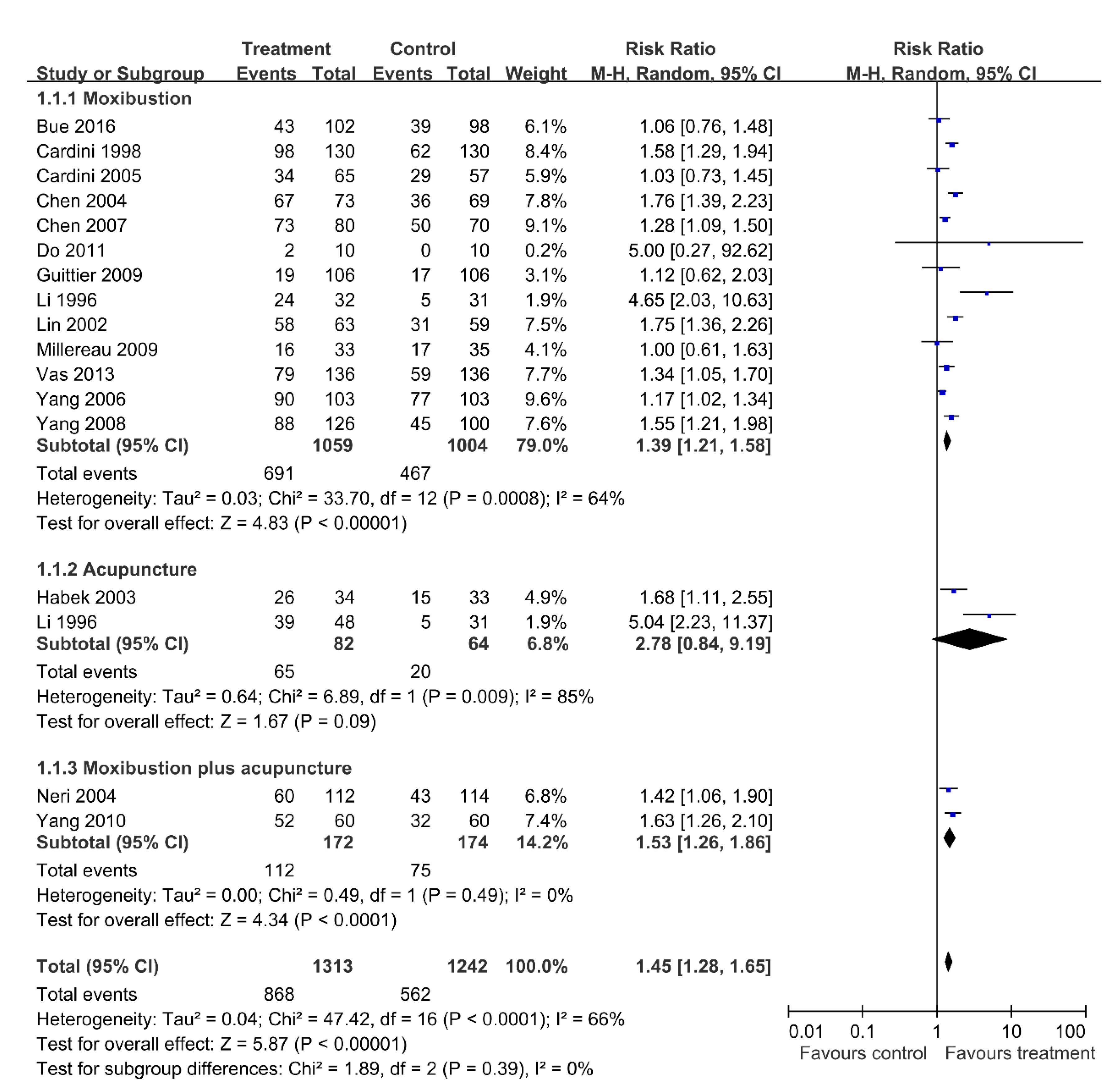
3.3. Efficacy of Interventions
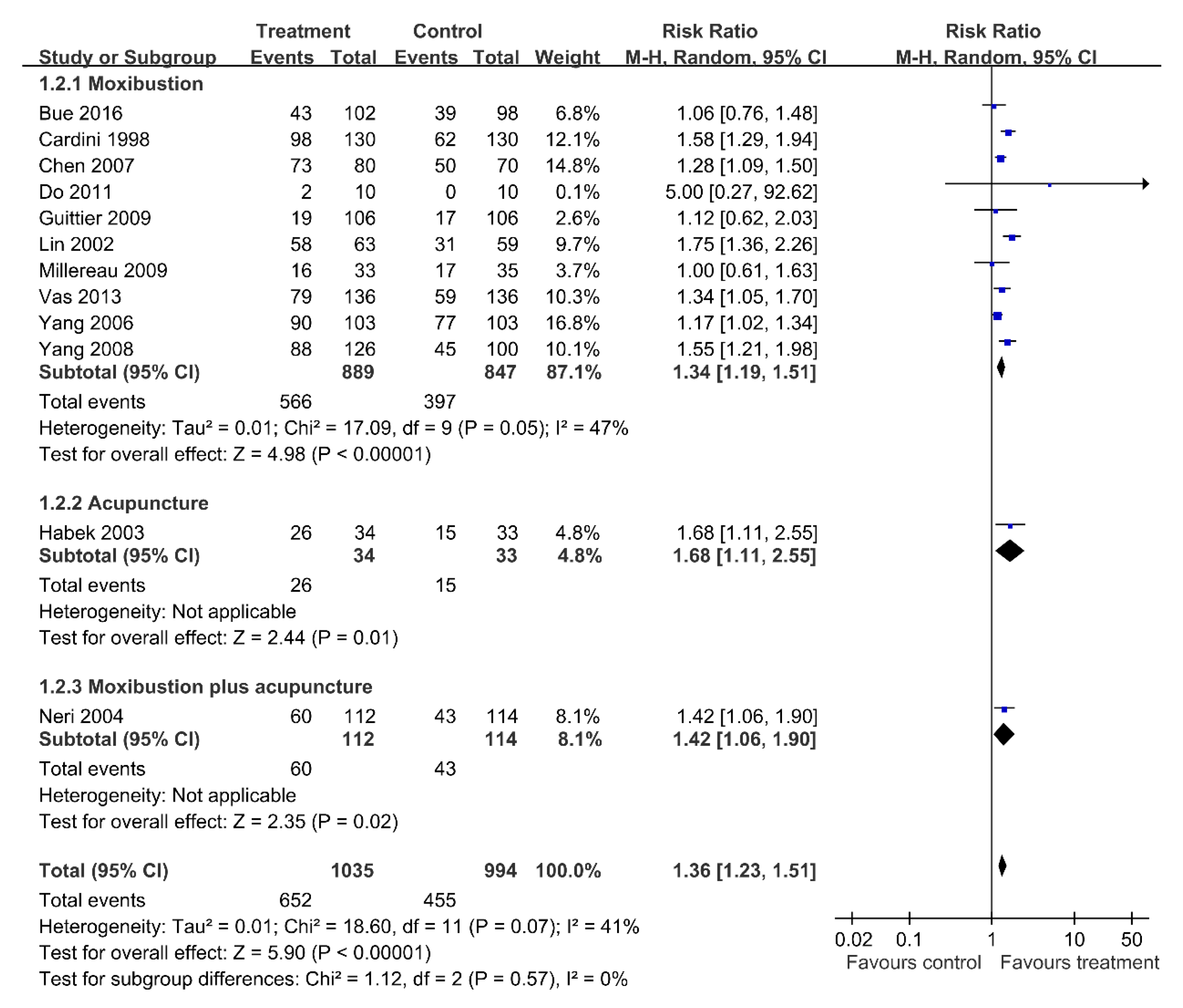
3.4. Sensitivity Analysis: Excluding Four Trials with a High Risk of Bias
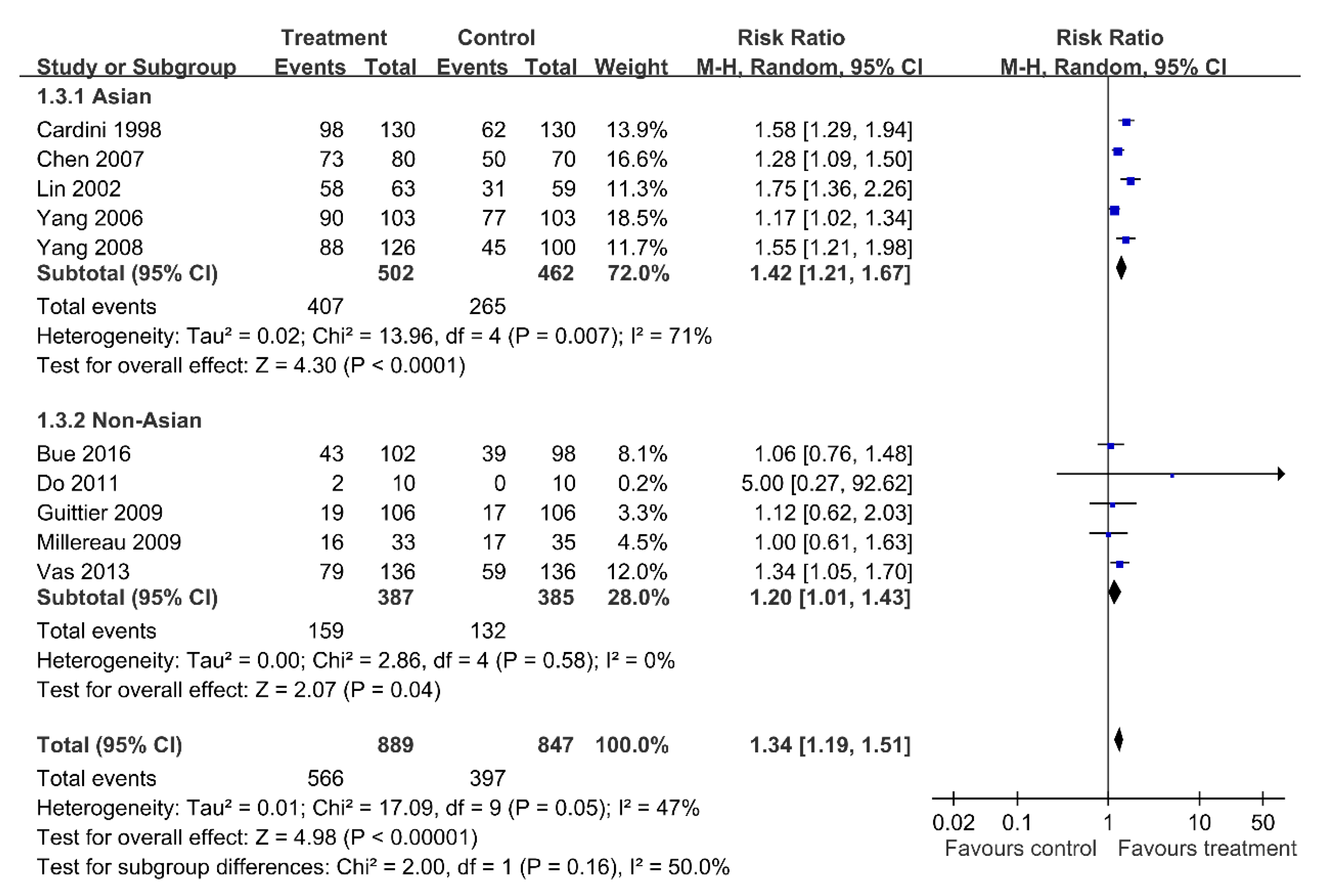
3.5. Subgroup Analysis of Moxibustion
3.6. Adverse Events
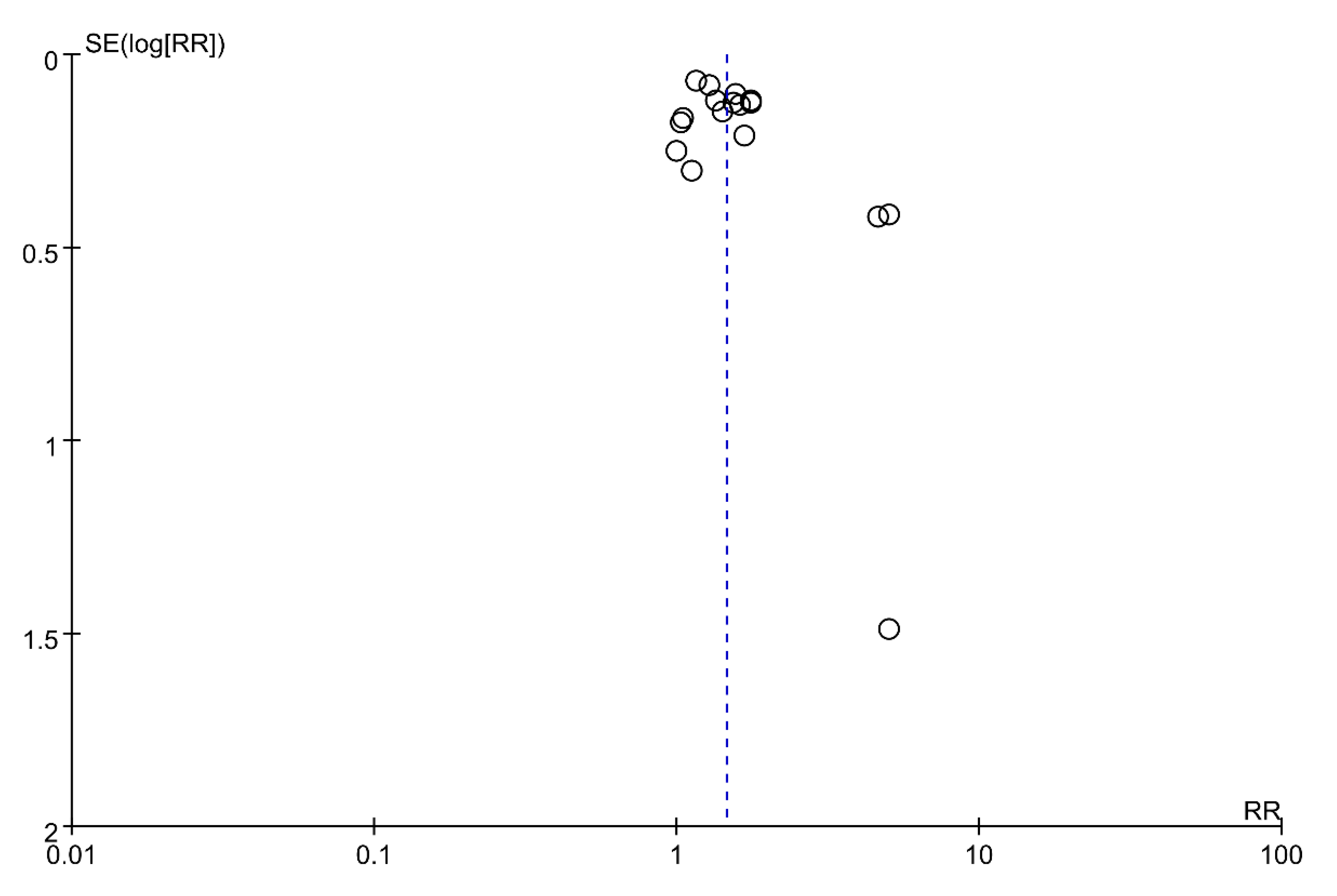
3.7. Publication Bias
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hickok, D.E.; Gordon, D.C.; Milberg, J.A.; Williams, M.A.; Daling, J.R. The frequency of breech presentation by gestational age at birth: A large population-based study. Am. J. Obstet. Gynecol. 1992, 166, 851–852. [Google Scholar] [CrossRef]
- Cui, H.; Chen, Y.; Li, Q.; Chen, J.; Liu, C.; Zhang, W. Cesarean Rate and Risk Factors for Singleton Breech Presentation in China. J. Reprod. Med. 2016, 61, 270–274. [Google Scholar]
- Sharshiner, R.; Silver, R.M. Management of fetal malpresentation. Clin. Obstet. Gynecol. 2015, 58, 246–255. [Google Scholar] [CrossRef] [PubMed]
- Kotaska, A.; Menticoglou, S.; Gagnon, R. Vaginal delivery of breech presentation. J. Obstet. Gynaecol. Can. 2009, 31, 557–566. [Google Scholar] [CrossRef]
- Hofmeyr, G.J.; Hannah, M.; Lawrie, T.A. Planned caesarean section for term breech delivery. Cochrane Database Syst. Rev. 2015, 7, 18–20. [Google Scholar] [CrossRef] [PubMed]
- External Cephalic Version and Reducing the Incidence of Term Breech Presentation: Green-top Guideline No. 20a; Royal College of Obstetricians and Gynaecologists: London, UK, 2017; Volume 124, pp. e178–e192.
- Hofmeyr, G.J.; Kulier, R. Cephalic version by postural management for breech presentation. Cochrane Database Syst Rev. 2012, 10, 5–6. [Google Scholar] [CrossRef]
- Deng, H.; Shen, X. The mechanism of moxibustion: Ancient theory and modern research. Evidence Based Complementary Altern. Med. 2013, 2013, 379291. [Google Scholar] [CrossRef]
- Park, J.W.; Lee, B.H.; Lee, H. Moxibustion in the management of irritable bowel syndrome: Systematic review and meta-analysis. BMC Complement Altern. Med. 2013, 13, 247. [Google Scholar] [CrossRef]
- Cardini, F.; Weixin, H. Moxibustion for correction of breech presentation: A randomized controlled trial. JAMA 1998, 280, 1580–1584. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.Q. Comparison of knee-chest position plus moxibustion on Zhiyin with knee-chest position for breech presentation. J. Sichuan Tradit. Chin. Med. 2006, 2006, 106–107. [Google Scholar]
- Vas, J.; Aranda, J.M.; Nishishinya, B.; Mendez, C.; Martin, M.A.; Pons, J.; Liu, P.J.; Wang, C.Y.; Milla, P.E. Correction of nonvertex presentation with moxibustion: A systematic review and metaanalysis. Am. J. Obstet. Gynecol. 2009, 201, 241–259. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Hu, J.; Wang, X.; Zhang, H.; Liu, J. Moxibustion and other acupuncture point stimulation methods to treat breech presentation: A systematic review of clinical trials. Chin. Med. 2009, 4, 4. [Google Scholar] [CrossRef] [PubMed]
- Coyle, M.E.; Smith, C.A.; Peat, B. Cephalic version by moxibustion for breech presentation. Cochrane Database Syst. Rev. 2012, 5, 7–10. [Google Scholar] [CrossRef] [PubMed]
- Vas, J.; Aranda, J.R.; Modesto, M.; Monserrat, M.; Baron, M.; Aguilar, I.; Parejo, N.; Ramirez, C.; Rivas, F. Using moxibustion in primary healthcare to correct non-vertex presentation: A multicentre randomised controlled trial. Acupunct. Med. 2013, 31, 31–38. [Google Scholar] [CrossRef]
- Bue, L.; Lauszus, F.F. Moxibustion did not have an effect in a randomised clinical trial for version of breech position. Dan. Med. J. 2016, 63, 2–4. [Google Scholar]
- Habek, D.; Cerkez Habek, J.; Jagust, M. Acupuncture conversion of fetal breech presentation. Fetal. Diagn. Ther. 2003, 18, 418–421. [Google Scholar] [CrossRef]
- A Revised Tool for Assessing Risk of Bias in Randomized Trials. Available online: https://methods.cochrane.org/bias/resources/rob-2-revised-cochrane-risk-bias-tool-randomized-trials (accessed on 20 March 2021).
- Yang, W.-W.; Zheng, W. Warm Argy Moxibustion Correct Abnormal Fetal Position 126 Cases. J. Zhe Jiang Coll. Tradit. Chin. Med. 2008, 32, 386. [Google Scholar]
- Yang, Y.; Yin, S.C.; Syu, S.Y. Integration Treatment of Traditional Chinese Medicine and Western Medicine in Breech Presentation: A Clinical Observation of 60 Cases. J. Shanhai Med Coll. Contin. Educ. 2010, 20, 54–55. [Google Scholar]
- Chen, Y. Moxibustion of zhiyin in breech presentation: 80 cases. Shaanxi Zhongyi 2007, 28, 334–335. [Google Scholar]
- Li, Q.; Wang, L. Clinical observation on correcting malposition of fetus by electro-acupuncture. J. Tradit. Chin. Med. 1996, 16, 260–262. [Google Scholar] [PubMed]
- Chen, Y.; Yang, L.W. Moxibustion on Zhiyin plus raising buttocks in a lateral position for correction fetal presentation in 73 cases. Clin. J. Tradit. Chin. Med. 2004, 333, 1. [Google Scholar]
- Lin, Y.P.; Deqing, Z.; Yongqing, H. Combination of moxibustion at point Zhiyin and knee-chest position for correction of breech pregnancy in 63 cases. Chin. Acupunct. Moxibustion 2002, 2002, 811–812. [Google Scholar]
- Cardini, F.; Lombardo, P.; Regalia, A.L.; Regaldo, G.; Zanini, A.; Negri, M.G.; Panepuccia, L.; Todroc, T. A randomised controlled trial of moxibustion for breech presentation. BJOB 2005, 112, 743–747. [Google Scholar] [CrossRef] [PubMed]
- Neri, I.; Airola, G.; Contu, G.; Allais, G.; Facchinetti, F.; Bnedetto, C. Acupuncture plus moxibustion to resolve breech presentation: A randomized controlled study. J. Matern. Fetal. Neonatal. Med. 2004, 15, 247–252. [Google Scholar] [CrossRef]
- Millereau, M.; Branger, B.; Darcel, F. Fetal version by acupuncture (moxibustion) versus control group. J. Gynecol. Obstet. Biol. Reprod. 2009, 38, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Do, C.K.; Smith, C.A.; Dahlen, H.; Bisists, A.; Schimied, V. Moxibustion for cephalic version: A feasibility randomised controlled trial. BMC Complement. Altern Med. 2011, 11, 81. [Google Scholar] [CrossRef]
- Guittier, M.J.; Pichon, M.; Dong, H.; Irion, O.; Boulvain, M. Moxibustion for breech version: A randomized controlled trial. Obstet. Gynecol. 2009, 114, 1034–1040. [Google Scholar] [CrossRef]
- West, Z. Acupuncture in Pregnancy and Childbirth; Elsevier Health Sciences: New York, NY, USA, 2008. [Google Scholar]
- Schlaeger, J.M.; Stoffel, C.L.; Bussell, J.L.; Cai, H.Y.; Takayama, M.; Yajima, H.; Takakura, N. Moxibustion for Cephalic Version of Breech Presentation. J. Midwifery Womens Health 2018, 63, 309–322. [Google Scholar] [CrossRef]
- O’Donnell, P.H.; Dolan, M.E. E. Cancer pharmacoethnicity: Ethnic differences in susceptibility to the effects of chemotherapy. Clin. Cancer Res. 2009, 15, 4806–4814. [Google Scholar] [CrossRef]
- Campbell, C.M.; Edwards, R.R. Ethnic differences in pain and pain management. Pain Manag. 2012, 2, 219–230. [Google Scholar] [CrossRef]
- Pennick, V.E.; Young, G. Interventions for preventing and treating pelvic and back pain in pregnancy. Cochrane Database Syst. Rev. 2007, 2, CD001139. [Google Scholar]
- Smith, C.A.; Collins, C.T.; Crowther, C.A.; Levett, K.M. Acupuncture or acupressure for pain management in labour. Cochrane Database Syst Rev. 2011, 7, CD009232. [Google Scholar] [CrossRef] [PubMed]
- Van den Berg, I.; Kaandorp, G.C.; Bosch, L.J.; Duvekot, J.J.; Arends, L.R.; Huning, M.G.M. Cost-effectiveness of breech version by acupuncture-type interventions on BL 67, including moxibustion, for women with a breech foetus at 33 weeks gestation: A modelling approach. Complement. Ther Med. 2010, 18, 67–77. [Google Scholar] [CrossRef] [PubMed]

| Study | Study Design | Patient Population | Intervention | Control | Outcomes |
|---|---|---|---|---|---|
| Bue 2016 [16] | RCT | 200 | Moxibustion at BL67; daily for 15–20 mins, preferably in the evening; 14 days | Observation | Cephalic presentation; rate of ECV and Cesarean delivery |
| Cardini 1998 [10] | RCT | 260 | Moxibustion at bilateral BL67; 15 mins on each side; 7 days | Observation | Cephalic presentation; Cesarean delivery rate |
| Cardini 2005 [25] | RCT | 123 | Moxibustion at BL67; 15 mins; twice daily; 7 days | Observation | Cephalic presentation |
| Chen 2004 [23] | RCT | 142 | Moxibustion at BL67; twice daily, 10–15 mins each time; up to 14 days | Observation and knee-chest position | Cephalic presentation |
| Chen 2007 [21] | RCT | 150 | Moxibustion at bilateral BL67; 20 mins a day; up to 15 days | Knee-chest position | Cephalic presentation |
| Do 2011 [28] | RCT | 20 | Moxibustion at bilateral BL67; 10 mins on each side; 10 days | Observation | Cephalic presentation |
| Guittier 2009 [29] | RCT | 212 | Moxibustion at bilateral BL67; 10 mins on each side; 14 days | Observation | Cephalic presentation |
| Habek 2003 [17] | RCT | 67 | Acupuncture at BL67; 30 mins; twice a week | Observation | Cephalic presentation; Cesarean delivery rate |
| Li 1996 [22] | RCT | 111 | Electro-acupuncture at bilateral BL67; 30 mins; 6 days Moxibustion at bilateral BL67; 20 mins; 6 days | Observation | Cephalic presentation |
| Lin 2002 [24] | RCT | 122 | Moxibustion at bilateral BL67; twice daily for 20 mins | Knee-chest position | Cephalic presentation |
| Millereau 2009 [27] | RCT | 68 | Moxibustion at BL67; 15–20 mins; 7 days | Observation | Cephalic presentation |
| Neri 2004 [26] | RCT | 240 | Moxibustion plus acupuncture at bilateral BL 67; total 40 mins; twice a week; 14 days | Observation | Cephalic presentation; Cesarean section rate |
| Vas 2013 [15] | RCT | 406 | Moxibustion at bilateral BL67; 20 mins; 14 days | Observation | Cephalic presentation; Cesarean delivery rate |
| Yang 2006 [11] | RCT | 206 | Moxibustion at BL67; 15–20 mins; 7 days | Knee-chest position | Cephalic presentation |
| Yang 2008 [19] | RCT | 226 | Moxibustion at bilateral BL67; 15 mins; up to 14 days | Knee-chest position | Cephalic presentation |
| Yang 2010 [20] | RCT | 120 | Moxibustion plus acupuncture at bilateral BL67; once daily; 14 days | Knee-chest position | Cephalic presentation |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liao, J.-A.; Shao, S.-C.; Chang, C.-T.; Chai, P.Y.-C.; Owang, K.-L.; Huang, T.-H.; Yang, C.-H.; Lee, T.-J.; Chen, Y.-C. Correction of Breech Presentation with Moxibustion and Acupuncture: A Systematic Review and Meta-Analysis. Healthcare 2021, 9, 619. https://doi.org/10.3390/healthcare9060619
Liao J-A, Shao S-C, Chang C-T, Chai PY-C, Owang K-L, Huang T-H, Yang C-H, Lee T-J, Chen Y-C. Correction of Breech Presentation with Moxibustion and Acupuncture: A Systematic Review and Meta-Analysis. Healthcare. 2021; 9(6):619. https://doi.org/10.3390/healthcare9060619
Chicago/Turabian StyleLiao, Jian-An, Shih-Chieh Shao, Chian-Ting Chang, Pony Yee-Chee Chai, Kok-Loon Owang, Tse-Hung Huang, Chung-Han Yang, Tsai-Jen Lee, and Yung-Chih Chen. 2021. "Correction of Breech Presentation with Moxibustion and Acupuncture: A Systematic Review and Meta-Analysis" Healthcare 9, no. 6: 619. https://doi.org/10.3390/healthcare9060619
APA StyleLiao, J.-A., Shao, S.-C., Chang, C.-T., Chai, P. Y.-C., Owang, K.-L., Huang, T.-H., Yang, C.-H., Lee, T.-J., & Chen, Y.-C. (2021). Correction of Breech Presentation with Moxibustion and Acupuncture: A Systematic Review and Meta-Analysis. Healthcare, 9(6), 619. https://doi.org/10.3390/healthcare9060619






