Online Problem-Based Learning in Clinical Dental Education: Students’ Self-Perception and Motivation
Abstract
1. Introduction
2. Materials and Methods
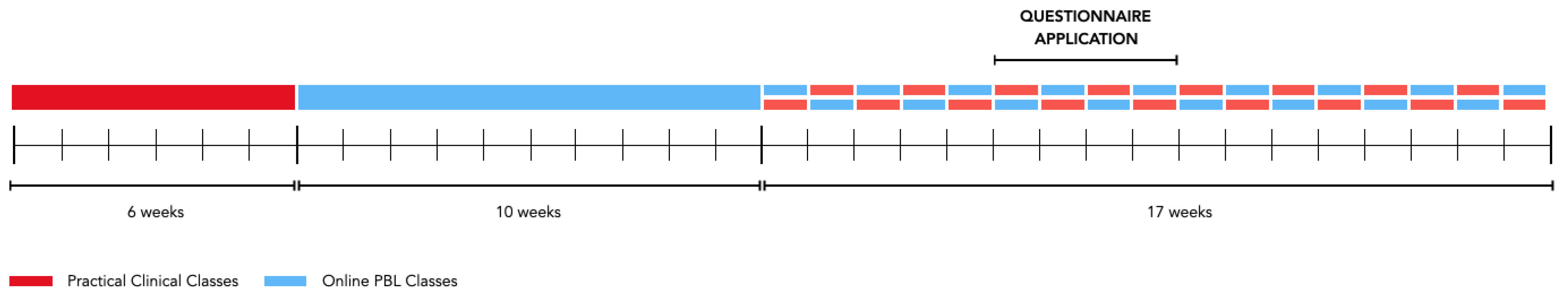
2.1. Course Description
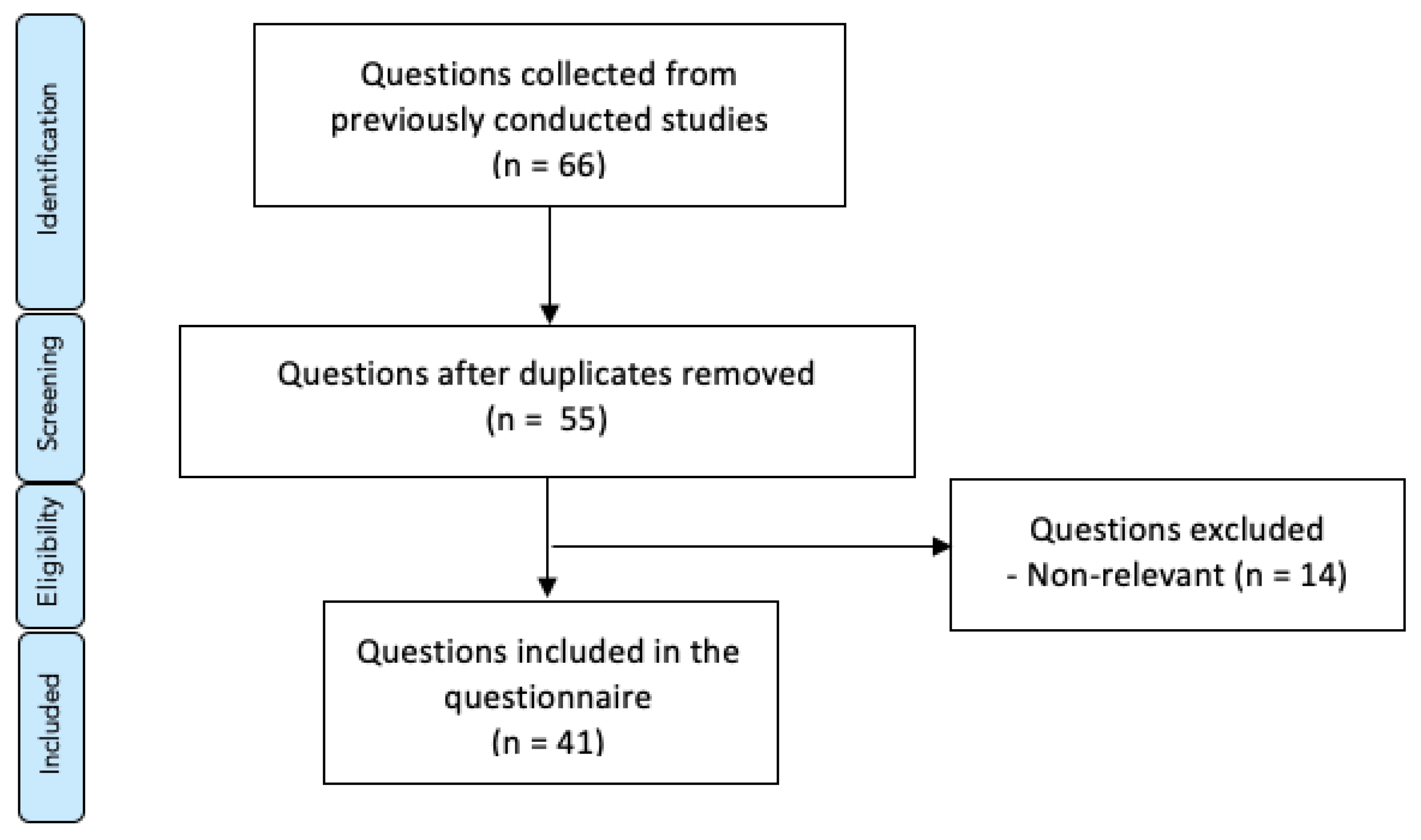
2.2. Study Design
2.3. Ethical Considerations
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hillen, H.; Scherpbier, A.; Wijnen, W. History of problem-based learning in medical education. In Lessons from Problem-Based Learning; Oxford University Press (OUP): Oxford, UK, 2010; pp. 5–12. [Google Scholar]
- Norman, G.R.; Schmidt, H.G. The psychological basis of problem-based learning: A review of the evidence. Acad. Med. 1992, 67, 557–565. [Google Scholar] [CrossRef] [PubMed]
- Foucault, M.; Sheridan, A. The Birth of the Clinic: An Archaeology of Medical Perception [Naissance de la Clinique.]; Presses Universitaires de France: Paris, France, 1963. [Google Scholar]
- McKeown, T. The Role of Medicine: Dream, Mirage, or Nemesis? Princeton University Press: Princeton, NJ, USA, 2014. [Google Scholar]
- Neufeld, V.R.; Barrows, H.S. The “McMaster Philosophy”: An approach to medical education. Acad. Med. 1974, 49, 1040–1050. [Google Scholar] [CrossRef]
- Boudier, H.A.J.S.; Smits, J.F.M. Problem-based learning: The Maastricht experience. Trends Pharmacol. Sci. 2002, 23, 164. [Google Scholar] [CrossRef]
- Rohlin, M.; Petersson, K.; Svensäter, G. The Malmö model: A problem-based learning curriculum in undergraduate dental education. Eur. J. Dent. Educ. 1998, 2, 103–114. [Google Scholar] [CrossRef]
- Holmboe, E.S. Faculty and the Observation of Trainees’ Clinical Skills: Problems and Opportunities. Acad. Med. 2004, 79, 16–22. [Google Scholar] [CrossRef]
- Suksudaj, N.; Townsend, G.C.; Kaidonis, J.; Lekkas, D.; Winning, T.A. Acquiring psychomotor skills in operative dentistry: Do innate ability and motivation matter? Eur. J. Dent. Educ. 2012, 16, e187–e194. [Google Scholar] [CrossRef]
- Rich, S.K.; Keim, R.G.; Shuler, C.F. Problem-Based Learning Versus a Traditional Educational Methodology: A Comparison of Preclinical and Clinical Periodontics Performance. J. Dent. Educ. 2005, 69, 649–662. [Google Scholar] [CrossRef]
- Kurzweil, R. The Law of Accelerating Returns. In Alan Turing: Life and Legacy of a Great Thinker; Springer: New York, NY, USA, 2004; pp. 381–416. [Google Scholar]
- Renes, S.L.; Strange, A.T. Using Technology to Enhance Higher Education. Altern. High. Educ. 2010, 36, 203–213. [Google Scholar] [CrossRef]
- Schmid, R.F.; Bernard, R.M.; Borokhovski, E.; Tamim, R.M.; Abrami, P.C.; Surkes, M.A.; Wade, C.A.; Woods, J. The effects of technology use in postsecondary education: A meta-analysis of classroom applications. Comput. Educ. 2014, 72, 271–291. [Google Scholar] [CrossRef]
- Anderson, T.; Dron, J. Three generations of distance education pedagogy. Int. Rev. Res. Open Distrib. Learn. 2011, 12, 80–97. [Google Scholar] [CrossRef]
- Chhetri, S.K. E-learning in neurology education: Principles, opportunities and challenges in combating neurophobia. J. Clin. Neurosci. 2017, 44, 80–83. [Google Scholar] [CrossRef] [PubMed]
- Restrepo, D.; Hunt, D.; Miloslavsky, E. Transforming traditional shadowing: Engaging millennial learners through the active apprenticeship. Clin. Teach. 2020, 17, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Mehta, N.B.; Hull, A.L.; Young, J.B.; Stoller, J.K. Just Imagine: New paradigms for medical education. Acad. Med. 2013, 88, 1418–1423. [Google Scholar] [CrossRef]
- Blumberg, P.; Pontiggia, L. Benchmarking the Degree of Implementation of Learner-Centered Approaches. Altern. High. Educ. 2010, 36, 189–202. [Google Scholar] [CrossRef]
- Thistlethwaite, J.E.; Davies, D.; Ekeocha, S.; Kidd, J.M.; MacDougall, C.; Matthews, P.; Purkis, J.; Clay, D. The effectiveness of case-based learning in health professional education. A BEME systematic review: BEME Guide No. 23. Med. Teach. 2012, 34, e421–e444. [Google Scholar] [CrossRef] [PubMed]
- Ramnanan, C.J.; Pound, L.D. Advances in medical education and practice: Student perceptions of the flipped classroom. Adv. Med. Educ. Pract. 2017, 8, 63–73. [Google Scholar] [CrossRef] [PubMed]
- Jones, F.; Passos-Neto, C.E.; Braghiroli, O.F.M. Simulation in medical education: Brief history and methodology. Princ. Pract. Clin. Res. J. 2015, 1, 56–63. [Google Scholar] [CrossRef]
- Hung, A.C.Y. A critique and defense of gamification. J. Interact. Online Learn. 2017, 15, 57–72. [Google Scholar]
- Ahmed, H.; Allaf, M.; Elghazaly, H. COVID-19 and medical education. Lancet Infect. Dis. 2020, 20, 777–778. [Google Scholar] [CrossRef]
- Alkhowailed, M.S.; Rasheed, Z.; Shariq, A.; Elzainy, A.; El Sadik, A.; Alkhamiss, A.; Alsolai, A.M.; Alduraibi, S.K.; Alduraibi, A.; Alamro, A.; et al. Digitalization plan in medical education during COVID-19 lockdown. Inform. Med. Unlocked 2020, 20, 100432. [Google Scholar] [CrossRef]
- Bennardo, F.; Buffone, C.; Fortunato, L.; Giudice, A. COVID-19 is a challenge for dental education—A commentary. Eur. J. Dent. Educ. 2020, 24, 822–824. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Luo, Y.; Wang, J.; Zhang, L.; Liang, Y.; Wu, Y.; Yu, H.; Cao, M. Comparison of student perception and performance between case-based learning and lecture-based learning in a clinical laboratory immunology course. LaboratoriumsMedizin 2016, 40, 283–289. [Google Scholar] [CrossRef]
- Banabilh, S.M.; Alkhuwaiter, S.S.; Aljuailan, R.I. Problem-based learning: Dental student’s perception of their education environments at Qassim University. J. Int. Soc. Prev. Community Dent. 2016, 6, 575–583. [Google Scholar] [CrossRef] [PubMed]
- Preeti, B.; Ashish, A.; Shriram, G. Problem Based Learning (PBL)—An Effective Approach to Improve Learning Outcomes in Medical Teaching. J. Clin. Diagn. Res. 2013, 7, 2896–2897. [Google Scholar] [CrossRef]
- Kim, Y.J. Observational Application Comparing Problem-Based Learning with the Conventional Teaching Method for Clinical Acupuncture Education. Evid.-Based Complement. Altern. Med. 2019, 2019, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Khoshnevisasl, P.; Sadeghzadeh, M.; Mazloomzadeh, S.; Feshareki, R.H.; Ahmadiafshar, A. Comparison of Problem-based Learning with Lecture-based Learning. Iran. Red Crescent Med. J. 2014, 16, e5186. [Google Scholar] [CrossRef] [PubMed]
- Asad, M.R.; Tadvi, N.; Amir, K.M.; Afzal, K.; Irfan, A.; Hussain, S.A. Medical Student’s Feedback towards Problem Based Learning and Interactive Lectures as a Teaching and Learning Method in an Outcome-Based Curriculum. Int. J. Med. Res. Health Sci. 2019, 8, 78–84. [Google Scholar]
- Usmani, A.; Sultan, S.T.; Ali, S.; Fatima, N.; Babar, S. Comparison of students and facilitators’ perception of implementing problem based learning. J. Pak. Med. Assoc. 2011, 61, 332–335. [Google Scholar]
| ID | Item |
|---|---|
| Q01 | PBL is interesting. |
| Q02 | PBL provides an interactive clinical learning environment. |
| Q03 | PBL facilitates the use of learning resources for clinical learning. |
| Q04 | PBL helps the achievement of curriculum outcomes. |
| Q05 | PBL helps understand basic concepts. |
| Q06 | PBL helps clinical exam preparation. |
| Q07 | PBL helps to have a better understanding about the subject. |
| Q08 | With PBL, students assume responsibility for their own learning. |
| Q09 | PBL is a reliable tool that can facilitate visual/spatial learning in a clinical context. |
| Q10 | PBL is a reliable tool that can facilitate auditory learning in a clinical context. |
| Q11 | PBL is a reliable tool that can facilitate kinesthetic learning in a clinical context. |
| Q12 | PBL helps convert from a passive to active lifelong learner in a clinical context. |
| Q13 | PBL increases the learning motivation in a clinical context. |
| Q14 | PBL helps to create clinical interest in the lectured lessons. |
| Q15 | PBL enhances the ability to find information using the internet/library. |
| Q16 | PBL enhances ability for public speaking in the clinical context. |
| Q17 | PBL increases the ability to manage time effectively in the clinical context. |
| Q18 | PBL improves decision-making skills in the clinical context. |
| Q19 | PBL enhances clinical problem-solving ability in the clinical context. |
| Q20 | PBL helps develop linguistic skills and self-confidence in the clinical context. |
| Q21 | PBL enhances clinical reasoning ability in the clinical context. |
| Q22 | A PBL hybrid system, composed by joining PBL and the conventional learning methods, is better than an exclusively conventional learning method. |
| Q23 | When compared to the exclusively conventional learning method, the knowledge achieved with PBL is more thorough. |
| Q24 | When compared to the exclusively conventional learning method, the focus of PBL on real medical/dental cases, makes it more relevant and interesting. |
| Q25 | When compared to the exclusively conventional learning method, the subject objectives are better understood with PBL. |
| Q26 | When compared to the exclusively conventional learning method, PBL is more time-consuming. |
| Q27 | PBL is effective without having any conventional lectures on the subject. |
| Q28 | With PBL, learners become active processors of information. |
| Q29 | PBL helps identify knowledge weak areas for further improvement. |
| Q30 | PBL enables the learners to establish a concrete action plan to achieve their learning goals. |
| Q31 | PBL enhances the practical and clinical application of the ideas. |
| Q32 | PBL helps develop clinical thinking, logical thinking, and abstract concepts. |
| Q33 | PBL fulfills an effective integration between different subjects of basic medical sciences (horizontal integration). |
| Q34 | PBL fulfills an effective integration between basic medical sciences with clinical sciences (vertical integration). |
| Q35 | PBL is a reliable tool for developing scientific reading and writing skills. |
| Q36 | PBL facilitates the development of interpersonal skills. |
| Q37 | PBL facilitates the development of intrapersonal skills. |
| Q38 | With PBL, knowledge activates prior knowledge around a problem, rather than specific subjects. |
| Q39 | PBL allows learners to activate prior knowledge and learn to elaborate and organize their knowledge. |
| Q40 | PBL enhances the retention of knowledge by practice, feedback, and evaluation. |
| Q41 | PBL increases the extent of more related knowledge. |
| n | (%) | ||
|---|---|---|---|
| Gender | Female | 77 | 65.3 |
| Male | 41 | 34.7 | |
| Nationality | Portuguese | 68 | 57.6 |
| Brazilian | 37 | 31.4 | |
| Other | 13 | 11.0 | |
| Mean | SD | ||
| Age | Years | 28.7 | 7.6 |
| ID | Item | Median (IQR) | Range (Min–Max) |
|---|---|---|---|
| Q01 | PBL interest | 4.0 (0) | 1–5 |
| Q02 | Interactive clinical learning environment | 4.0 (0) | 1–5 |
| Q03 | Use of learning resources for clinical learning | 4.0 (0) | 1–5 |
| Q04 | Achievement of curriculum outcomes | 4.0 (1) | 1–5 |
| Q05 | Understanding of basic concepts | 4.0 (0) | 1–5 |
| Q06 | Clinical exam preparation | 4.0 (1) | 1–5 |
| Q07 | Subject understanding | 4.0 (0) | 1–5 |
| Q08 | Student knowledge responsibility | 5.0 (1) | 1–5 |
| Q09 | Visual/spatial learning in a clinical context | 4.0 (1) | 1–5 |
| Q10 | Auditory learning in a clinical context | 4.0 (1) | 1–5 |
| Q11 | Kinesthetic learning in a clinical context | 3.0 (2) | 1–5 |
| Q12 | Conversion to active lifelong learner in a clinical context | 4.0 (2) | 1–5 |
| Q13 | Learning motivation in a clinical context | 4.0 (1) | 1–5 |
| Q14 | Clinical interest in the lectured lessons | 4.0 (1) | 1–5 |
| Q15 | Ability to find information using the internet/library | 4.0 (1) | 1–5 |
| Q16 | Ability for public speaking | 4.0 (2) | 1–5 |
| Q17 | Time-management skills | 4.0 (1) | 1–5 |
| Q18 | Decision-making skills | 4.0 (1) | 1–5 |
| Q19 | Clinical problem-solving ability | 4.0 (1) | 1–5 |
| Q20 | Development of linguistic skills and self-confidence in a clinical context | 4.0 (1) | 1–5 |
| Q21 | Clinical reasoning ability, in a clinical context | 4.0 (1) | 1–5 |
| Q22 | Comparison of the PBL hybrid system with the conventional method | 4.5 (1) | 1–5 |
| Q23 | Comparison of knowledge thoroughness gain | 3.0 (2) | 1–5 |
| Q24 | Comparison of relevance and interest | 4.0 (2) | 1–5 |
| Q25 | Comparison of understanding of objectives | 4.0 (1) | 1–5 |
| Q26 | Time consumption comparison | 3.0 (2) | 1–5 |
| Q27 | Effectiveness comparison | 3.0 (2) | 1–5 |
| Q28 | Active processing of information | 4.0 (1) | 1–5 |
| Q29 | Identification of weakness areas | 4.0 (1) | 1–5 |
| Q30 | Establishment of a concrete action plan for the achievement of learning goals | 4.0 (1) | 1–5 |
| Q31 | Practical and clinical application of ideas | 4.0 (1) | 1–5 |
| Q32 | Development of clinical thinking, logical thinking, and abstract concepts | 4.0 (0) | 1–5 |
| Q33 | Horizontal integration effectiveness | 4.0 (1) | 1–5 |
| Q34 | Vertical integration effectiveness | 4.0 (0) | 1–5 |
| Q35 | Development of scientific reading and writing skills | 4.0 (1) | 1–5 |
| Q36 | Development of interpersonal skills | 4.0 (1) | 1–5 |
| Q37 | Development of intrapersonal skills | 4.0 (1) | 1–5 |
| Q38 | Prior knowledge activation around a problem | 4.0 (0) | 1–5 |
| Q39 | Knowledge organization | 4.0 (1) | 1–5 |
| Q40 | Knowledge retention by practice, feedback, and evaluation | 4.0 (0) | 1–5 |
| Q41 | Extension of related knowledge | 4.0 (1) | 1–5 |
| Component | Item | Factor Loadings | Eigenvalue | Variance (%) | Communality |
|---|---|---|---|---|---|
| Component 1 | Learning motivation in a clinical context (Q13) | 0.773 | 19.251 | 46.955 | 0.824 |
| Clinical interest in the lectured lessons (Q14) | 0.762 | 0.781 | |||
| Comparison of relevance and interest (Q24) | 0.654 | 0.671 | |||
| Clinical problem-solving ability (Q19) | 0.625 | 0.842 | |||
| Comparison of understanding of objectives (Q25) | 0.623 | 0.707 | |||
| Effectiveness comparison (Q27) | 0.601 | 0.568 | |||
| Comparison of knowledge thoroughness gain (Q23) | 0.560 | 0.700 | |||
| Establishment of a concrete action plan for the achievement of learning goals (Q30) * | 0.498 | 0.664 | |||
| Identification of weakness areas (Q29) | 0.463 | 0.625 | |||
| Component 2 | PBL interest (Q01) | 0.700 | 2.299 | 5.607 | 0.727 |
| Use of learning resources for clinical learning (Q03) | 0.697 | 0.732 | |||
| Clinical exam preparation (Q06) | 0.693 | 0.771 | |||
| Achievement of curriculum outcomes (Q04) | 0.671 | 0.763 | |||
| Understanding of basic concepts (Q05) | 0.671 | 0.691 | |||
| Interactive clinical learning environment (Q02) | 0.666 | 0.733 | |||
| Subject understanding (Q07) | 0.646 | 0.683 | |||
| Extension of related knowledge (Q41) | 0.525 | 0.765 | |||
| Knowledge retention by practice, feedback, and evaluation (Q40) | 0.486 | 0.733 | |||
| Prior knowledge activation around a problem (Q38) *1 | 0.406 | 0.664 | |||
| Component 3 | Ability for public speaking (Q16) | 0.860 | 1.981 | 4.833 | 0.800 |
| Development of linguistic skills and self-confidence in a clinical context (Q20) | 0.807 | 0.828 | |||
| Ability to find information using the internet/library (Q15) | 0.650 | 0.592 | |||
| Time-management skills (Q17) | 0.632 | 0.685 | |||
| Decision-making skills (Q18) | 0.611 | 0.696 | |||
| Clinical reasoning ability in a clinical context (Q21) | 0.516 | 0.800 | |||
| Development of scientific reading and writing skills (Q35) | 0.470 | 0.707 | |||
| Establishment of a concrete action plan for the achievement of learning goals (Q30) *1 | 0.454 | 0.664 | |||
| Component 4 | Horizontal integration effectiveness (Q33) | 0.769 | 1.632 | 3.980 | 0.854 |
| Vertical integration effectiveness (Q34) | 0.671 | 0.729 | |||
| Practical and clinical application of ideas (Q31) | 0.605 | 0.769 | |||
| Development of clinical thinking, logical thinking, and abstract concepts (Q32) | 0.549 | 0.741 | |||
| Knowledge organization (Q39) | 0.513 | 0.835 | |||
| Prior knowledge activation around a problem (Q38) * | 0.418 | 0.664 | |||
| Comparison between the PBL hybrid system with the conventional method (Q22) | 0.418 | 0.555 | |||
| Component 5 | Visual/spatial learning in a clinical context (Q09) | 0.711 | 1.598 | 3.899 | 0.748 |
| Conversion to active lifelong learner in a clinical context (Q12) | 0.754 | 0.743 | |||
| Kinesthetic learning in a clinical context (Q11) | 0.753 | 0.808 | |||
| Auditory learning in a clinical context (Q10) | 0.504 | 0.713 | |||
| Component 6 | Development of interpersonal skills (Q36) | 0.643 | 1.316 | 3.210 | 0.865 |
| Development of intrapersonal skills (Q37) | 0.587 | 0.839 | |||
| Component 7 | Student knowledge responsibility (Q08) | 0.841 | 1.104 | 2.692 | 0.795 |
| Active processing of information (Q28) | 0.522 | 0.750 | |||
| Component 8 | Time consumption (Q26) | 0.932 | 1.012 | 2.468 | 0.891 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morgado, M.; Mendes, J.J.; Proença, L. Online Problem-Based Learning in Clinical Dental Education: Students’ Self-Perception and Motivation. Healthcare 2021, 9, 420. https://doi.org/10.3390/healthcare9040420
Morgado M, Mendes JJ, Proença L. Online Problem-Based Learning in Clinical Dental Education: Students’ Self-Perception and Motivation. Healthcare. 2021; 9(4):420. https://doi.org/10.3390/healthcare9040420
Chicago/Turabian StyleMorgado, Mariana, José João Mendes, and Luís Proença. 2021. "Online Problem-Based Learning in Clinical Dental Education: Students’ Self-Perception and Motivation" Healthcare 9, no. 4: 420. https://doi.org/10.3390/healthcare9040420
APA StyleMorgado, M., Mendes, J. J., & Proença, L. (2021). Online Problem-Based Learning in Clinical Dental Education: Students’ Self-Perception and Motivation. Healthcare, 9(4), 420. https://doi.org/10.3390/healthcare9040420








