The Mentor Mothers Program in the Department of Defense in Nigeria: An Evaluation of Healthcare Workers, Mentor Mothers, and Patients’ Experiences
Abstract
1. Background
2. Aim
3. Research Methods
3.1. Research Design
3.2. Research Setting
3.3. Research Participants
3.4. Recruitment Process
3.5. Instrument
4. Ethical Considerations
4.1. Data Collection
4.2. Data Analysis
4.3. Trustworthiness
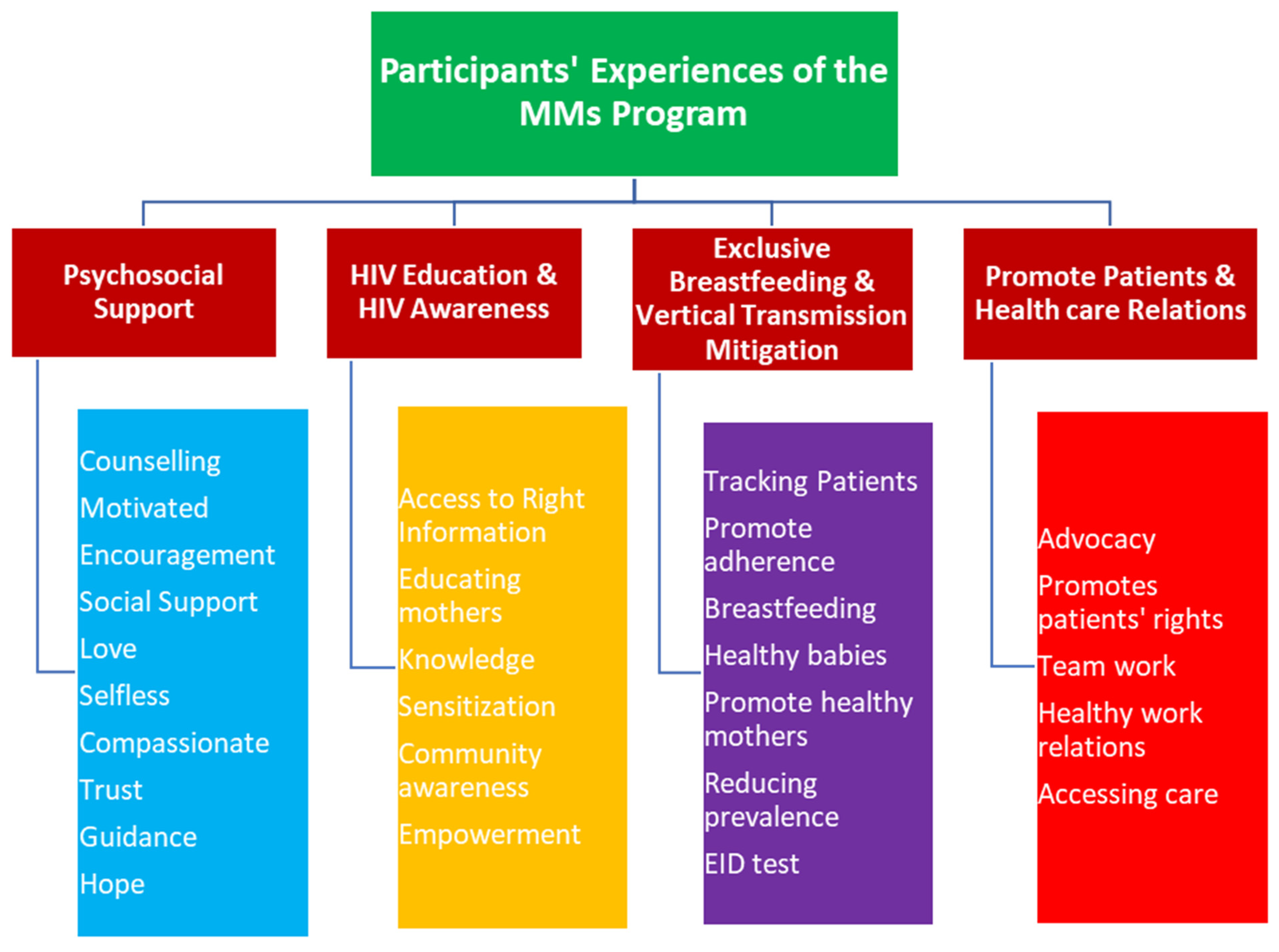
5. Psychosocial Support
“It’s all about trust … they really trust us, they believe whatever we tell them. Most of their husbands trust me because I am working with the knowledge I have … With the help of mentor mothers, these women can boldly breastfeed their babies even in the market, in the church, anywhere or even in front of family members who know they are HIV-positive”(mentor mother)
“They believe us more than they do the nurses”(mentor mother)
“When I met aunty C, she encouraged me … she brought me back to life so I am grateful for that … she is compassionate. Some people will look at you and say it is what you did; that’s the result of your bad character. They would be judgmental. It takes somebody who is compassionate to look at you and say there is still a way out without judging you irrespective of whatever thing you might have done”(patient)
“Some other people would make you feel bad like ‘after all you are positive’. But she carries us all along. She gives us special treatment. That sense of belonging is one thing I have enjoyed so far”(patient)
“She is so lovely. I feel loved … she gives me hope … mentor mothers are patient. They have this type of patience that I cannot describe. Even when you are crying for nothing they keep calming you down”(patient)
“I am so loved. I don’t even know what to say”(patient)
“The mentor mothers have the confidence, they can come out and say ‘yes, I am one of you and if you follow PMTCT guidelines, you will stay alive, you can live a positive life’. And people are really motivated by that … The Mentor Mothers program is good and should be sustained because the mentor mothers are doing a great job”(PMTCT focal nurse)
“The patients would describe it as interesting because it has helped them gain confidence in themselves, in their marriages, and in life generally. Like there is this hope, you see. Suddenly the clients will move from being sad and unhappy to being interested and lively once again”(PMTCT focal nurse)
5.1. HIV Education and Awareness
“One of the primary things that we do is counselling. This counselling cuts across every aspect. The education of the patient about how the disease can be contracted, the prevention, the complications if they do not take their drug, and the side effects of the drugs”(medical officer)
“We counsel them to the point that they are interested in helping others. They reach out to other positive mothers and talk with them, educate them, and give them enough knowledge for them to understand that it is possible to have an HIV-free baby even when the mother is positive”(medical officer)
“We give them adherence counselling right from the day they are declared positive. This is followed by home visits. We visit them to know how they are taking their drugs … we follow them up and based on that they are doing very well”(PMTCT focal nurse)
5.2. Exclusive Breastfeeding and Mitigation of Vertical Transmission: Outcomes of the Program
“…formally our children were turning out positive … before I became the focal person here there were lots of positive babies, but these days, hardly will you see any positive baby. Since this mentor mother came, we have not recorded any positive baby from our unit. Whenever patients come to the clinic, they always appreciate us, they appreciate the mentor mother in our facility”(PMTCT focal nurse)
“PMTCT is functioning very well. Recently, people have the confidence, the belief that when they are adherent on their medication they are most nearly absolutely sure they are going to have a HIV negative baby. The tracking is reduced, they all just come by themselves. Maximum is a day or two they miss their appointment”(medical officer)
“This program is okay… Mentor Mothers and PMTCT…. great job. I want the program to continue so we can achieve that zero transmission level”(PMTCT focal nurse)
“The program has helped mothers live well … most mothers feel they will not give birth again…but with education by this mentor mother to live healthy, you can give birth to as many children as you like. Provided you keep to the rules, your children will come out healthy. The contribution of the mentor mothers to this program is very good”(patient)
5.3. Promoting Healthy Patients and Healthcare Relations
“Even though they have been trained, some still have misconceptions about HIV. Some of them still believe that the child has traces of HIV, so in those kinds of doubt, they fall back to us, we that are positive and have had negative children”(mentor mother)
“I have been able to take away fear from our women by encouraging them. Some left school due to fear. I protect my women … many families depend on us as mentor mothers”(mentor mother)
“Because we have a good rapport with them, they trust us … we protect them in the various sites so they come to clinic with boldness knowing the mentor is there … No mentor mother, no PMTCT. It’s just that simple”(mentor mother)
“Follow up, good result, encouraging them, and making sure that the confidentiality of these patients is maintained … those are the things that are encouraging the patients to fulfil good interpersonal relationship”(medical officer)
“Those that access care here are very comfortable because they can walk in at any time and meet a particular set of persons and there is no breach in confidentiality”(medical officer)
“They look out for the way you receive the patients, whether you maintain confidentiality or attend to them well”(PMTCT focal nurse)
6. Discussion
7. Conclusions
7.1. Limitations of the Study
- Due to the regimented nature of the Nigerian military, very limited information exists in the public domain on prevention of mother-to-child transmission of HIV using mentor mothers in the Nigerian DoD. In addition, research of this nature has not been conducted before now in the DoD, so researchers had limited literature on this subject in the DoD.
- Very few studies have previously addressed the experiences of healthcare workers, mentor mothers, and patients. The unavailability of adequate literature therefore limited extensive presentation of the discussion of findings in this study. The study was limited to Abuja, the Federal Capital City of Nigeria, which was chosen because it is the administrative headquarter of the Nigerian Military where the MMs program was implemented in 2014. However, due to the specific number of participants in this study, coupled with the fact that the study was conducted in one region of the country, the study findings cannot be generalized. It is suggested that further research be conducted in other DoD facilities to further explore the MMs strategy for PMTCT.
7.2. Recommendations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Joint United Nations Programme on HIV/AIDS, (UNAIDS). AIDS info 2017. Available online: http://aidsinfo.unaids.org/ (accessed on 26 August 2020).
- Owiredu, M.N.; Bellare, N.B.; Musanhu, C.C.C.; Oyelade, T.A.; Thom, E.M.; Bigirimana, F.; Anyaike, C.; Eliya, M.T.; Mushavi, A.; Nyarko, E.A.; et al. Building health system capacity through implementation research: Experience of INSPIRE—A multi-country PMTCT implementation research project. J. Acquir. Immune Defic. Syndr. 2017, 75, S240. [Google Scholar] [CrossRef] [PubMed]
- UNAIDS. Global Report: UNAIDS Report on the Global AIDS Epidemic 2013. WHO Library Cataloguing-in-Publication Data. UNAIDS/JC2502/1/E. Available online: https://www.unaids.org/en/resources/documents/2013/20130923_UNAIDS_Global_Report_2013#:~:text=The%202013%20report%20on%20the,deaths%20and%20HIV%20among%20children (accessed on 20 August 2020).
- UNAIDS. Global Report: UNAIDS Report on the Global AIDS Epidemic 2012. WHO Library Cataloguing-in-Publication Data. UNAIDS/JC2417E. Available online: https://www.unaids.org/sites/default/files/media_asset/20121120_UNAIDS_Global_Report_2012_with_annexes_en_1.pdf (accessed on 20 August 2020).
- UNAIDS. The Gap Report 2014. Available online: http://www.unaids.org/en/resources/campaigns/2014/2014gapreport/gapreport/ (accessed on 20 August 2020).
- UNAIDS. The Gap Report 2014: Epi Slides. Available online: http://www.unaids.org/en/media/unaids/contentassets/documents/document/2014/2014gapreportslides/01_Epi_slides_2014July.pdf (accessed on 20 August 2020).
- Joint United Nations Programme on HIV/AIDS, (UNAIDS). Fast-Track: Ending the AIDS Epidemic by 2030. Geneva, Switzerland 2017: Joint United Nations Programme on HIV. AIDS. Available online: https://www.unaids.org/sites/default/files/media_asset/JC2686_WAD2014report_en.pdf (accessed on 4 September 2020).
- Agboghoroma, C.O.; Sagay, S.A.; Ikechebelu, J.I. Nigerian prevention of mother to child transmission of human immunodeficiency virus program: The journey so far. J. HIV Hum. Reprod. 2013, 11, 1–7. [Google Scholar]
- Joint United Nations Programme on HIV/AIDS, (UNAIDS). HIV Data and Estimates; Joint United Nations Programme on HIV. AIDS: Geneva, Switzerland, 2016. [Google Scholar]
- Joint United Nations Programme on HIV/AIDS, (UNAIDS). Nigeria 2017. Available online: https://www.unaids.org/en/regionscountries/countries/nigeria (accessed on 16 July 2020).
- Joint United Nations Programme on HIV/AIDS, (UNAIDS). Fast-Track: Ending the AIDS Epidemic by 2030; Joint United Nations Programme on HIV. AIDS: Geneva, Switzerland, 2017. [Google Scholar]
- Sidibé, M.; Loures, L.; Samb, B. The UNAIDS 90–90–90 target: A clear choice for ending AIDS and for sustainable health and development. J. Int. AIDS Soc. 2016, 19, 21133. [Google Scholar]
- Sidibé, M. The sustainable development agenda and the end of AIDS. Lancet 2015, 386, 108–110. [Google Scholar] [CrossRef]
- UNAIDS. Countdown to ZERO: Global Plan Towards the Elimination of New HIV Infections Among Children by 2015 and Keeping Their Mother Alive; Joint United Nations Programme on HIV. AIDS: Geneva, Switzerland, 2011. [Google Scholar]
- Mutabazi, J.C.; Zarowsky, C.; Trottier, H. The impact of programs for prevention of mother-to-child transmission of HIV on health care services and systems in sub-Saharan Africa-A review. Public Health Rev. 2017, 38, 28. [Google Scholar] [CrossRef] [PubMed]
- Colvin, C.J.; Konopka, S.; Chalker, J.C.; Jonas, E.; Albertini, J.; Amzel, A.; Fogg, K. A systematic review of health system barriers and enablers for antiretroviral therapy (ART) for HIV-infected pregnant and postpartum women. PLoS ONE 2014, 9, e108150. [Google Scholar] [CrossRef] [PubMed]
- Sprague, C.; Chersich, M.F.; Black, V. Health system weaknesses constrain access to PMTCT and maternal HIV services in South Africa: A qualitative enquiry. AIDS Res. Ther. 2011, 8, 10. [Google Scholar] [CrossRef] [PubMed]
- Rotheram-Borus, M.J.; Le Roux, I.M.; Tomlinson, M.; Mbewu, N.; Comulada, W.S.; Le Roux, K.; Stewart, J.; O’Connor, M.J.; Hartley, M.; Desmond, K.; et al. Philani Plus (+): A Mentor Mother community health worker home visiting program to improve maternal and infants’ outcomes. Prev. Sci. 2011, 12, 372–388. [Google Scholar] [CrossRef] [PubMed]
- Futterman, D.; Shea, J.; Besser, M.; Stafford, S.; Desmond, K.; Comulada, W.S.; Greco, E. Mamekhaya: A pilot study combining a cognitive-behavioral intervention and mentor mothers with PMTCT services in South Africa. AIDS Care 2010, 22, 1093–1100. [Google Scholar] [CrossRef] [PubMed]
- Marcos, Y.; Phelps, B.R.; Bachman, G. Community strategies that improve care and retention along the prevention of mother-to-child transmission of HIV cascade: A review. J. Int. AIDS Soc. 2012, 15, 17394. [Google Scholar] [CrossRef] [PubMed]
- Summers, J.; Robinson, R.; Capps, L.; Zisook, S.; Atkinson, J.H.; Mccutchan, E.; Mccutchan, J.A.; Deutsch, R.; Patterson, T.; Grant, I. The influence of HIV-related support groups on survival in women who lived with HIV: A pilot study. Psychosomatics 2000, 41, 262–268. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization, (WHO). Health Systems Performance Assessment 2009: A Tool for Health Governance in the 21st Century. 2009. Available online: http://www.who.int/healthinfo/statistics/toolkit_hss/en/index.html (accessed on 15 June 2020).
- World Health Organization, (WHO). Key Informant Survey. 2001. Available online: https://www.who.int/responsiveness/surveys/ (accessed on 15 June 2020).
- World Health Organization, (WHO). Health Systems Responsiveness Questionnaires. 2000. Available online: https://www.who.int/responsiveness/surveys/ (accessed on 15 June 2020).
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Rice, P.L.; Ezzy, D. Qualitative Research Methods: A Health Focus; Oxford: Victoria, Australia, 1999; Volume 720, pp. 93–141. [Google Scholar]
- Chapman, S.; Chihana, N.K.; Scheepers, E.; Schmitz, K. An inferential analysis as to the impact of exposure to a peer Mentor Mother model on uptake of PMTCT services and maternal behavioural outcomes. J. Int. Aids Soc. 2016, 19. Available online: https://onlinelibrary.wiley.com/toc/17582652/2016/19/1 (accessed on 5 September 2020).
- UNAIDS. Mother Mentor and Mother Support 2013. Available online: https://www.msh.org/sites/msh.org/files/msh_ehandbook_complete.pdf (accessed on 11 June 2020).
- ICAP. ICAP’s Mentor Mothers in Mozambique Help Pregnant and Breastfeeding Mothers Achieve Viral Suppression: Stories from the Field. 2019. Available online: https://icap.columbia.edu/icaps-mentor-mothers-in-mozambique-help-pregnant-and-breastfeeding-mothers-achieve-viral-suppression/ (accessed on 20 July 2020).
- Odeny, T.A.; Onono, M.; Owuor, K.; Helova, A.; Wanga, I.; Bukusi, E.A.; Turan, J.M.; Abuogi, L.L. Maximizing adherence and retention for women living with HIV and their infants in Kenya (MOTIVATE! study): Study protocol for a randomized controlled trial. Trials 2018, 19, 1–10. [Google Scholar] [CrossRef] [PubMed]
- UNICEF. Innovative Approaches for Eliminating Mother-to-Child Transmission of HIV: Community Client Tracing Through Mentor Mothers in the Democratic Republic of the Congo 2018; HIV and AIDS Section, United Nations Children’s Fund, 3 United Nations Plaza: New York, NY, USA, 2018; p. 10017. [Google Scholar]
- Elizabeth Glaser Pediatric AIDS Foundation. Mentor Mothers: Connecting HIV-Positive Women in DRC. 2017. Available online: https://www.pedaids.org/wp-content/uploads/2017/11/DRCMentorMothers2015.pdf (accessed on 3 July 2020).
- Ambia, J.; Mandala, J. A systematic review of interventions to improve prevention of mother-to-child HIV transmission service delivery and promote retention. J. Int. AIDS Soc. 2016, 19, 20309. [Google Scholar] [CrossRef] [PubMed]
- Myers, A.; Okonji, E.; Besser, M.; Schmitz, K. mothers2mothers (m2m) Internal Evaluation of the Prevention of Mother-to-Child Transmission (PMTCT), Peer Education and Psychosocial Support Services in Kenya, Lesotho, Malawi, South Africa, Swaziland, Tanzania and Uganda. Cape Town 2012, Department of Programmes and Technical Support. Available online: https://m2m.org/wp-content/uploads/2019/10/2012ProgrammeEvaluation.pdf (accessed on 5 September 2020).
- Kenya Ministry of Health. National Guidelines for PMTCT Peer Education and Psychosocial Support in Kenya: The Kenya Mentor Mother Program 2012. First Edition: National AIDS and STI Control Program (NASCOP) Ministry of Health, Nairobi. Available online: http://guidelines.health.go.ke:8000/media/National_Guidelines__for__PMTCT_Peer_Education_and_Psychosocial_Support_in_Kenya_KMMP.pdf (accessed on 5 September 2020).
- Baek, C.; Mathambo, V.; Mkhize, S.; Friedman, I.; Apicella, L.; Rutenberg, N. Key Findings from an Evaluation of the mothers2mothers Program in KwaZulu-Natal, South Africa: Horizons Program Health Systems Trust 2007. Available online: https://knowledgecommons.popcouncil.org/cgi/viewcontent.cgi?article=1046&context=departments_sbsr-hiv (accessed on 20 July 2020).
- Shroufi, A.; Mafara, E.; Saint-Sauveur, J.F.; Taziwa, F.; Viñoles, M.C. Mother to mother (M2M) peer support for women in prevention of mother to child transmission (PMTCT) programmes: A qualitative study. PLoS ONE 2013, 8, e64717. [Google Scholar] [CrossRef] [PubMed]
- Krebs, L.D. Ethiopia’s Prevention of Mother-to-Child Transmission (pmtct) Programs: Addressing Attrition and Loss to Follow-Up; Simon Fraser University Library: Burnaby, UK, 2012. [Google Scholar]
| Pseudonym | Professional Position in Unit | Duration of employment |
|---|---|---|
| Effa | Medical officer (PMTCT) | 4 years |
| Kalan | Medical officer (PMTCT) | 13 years |
| Ovede | Medical officer (PMTCT) | 12 years |
| Fenky | Nurse (PMTCT focal person) | 16 years |
| Mokun | Nurse (PMTCT focal person) | 22 years |
| Ntewa | Nurse (PMTCT focal person) | 20 years |
| Cyuko | Mentor Mother | 3 years |
| Dobla | Mentor Mother | 4 years |
| Nancel | Mentor Mother | 2 years |
| Neki | Mentor Mother | 5 years |
| Nelly | Mentor Mother | 5 years |
| Savic | Mentor Mother | 5 years |
| Cecio | Patient | |
| Chima | Patient | |
| Chuke | Patient | |
| Hilda | Patient | |
| Katu | Patient | |
| Mabel | Patient |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ibu, J.M.; Mhlongo, E.M. The Mentor Mothers Program in the Department of Defense in Nigeria: An Evaluation of Healthcare Workers, Mentor Mothers, and Patients’ Experiences. Healthcare 2021, 9, 328. https://doi.org/10.3390/healthcare9030328
Ibu JM, Mhlongo EM. The Mentor Mothers Program in the Department of Defense in Nigeria: An Evaluation of Healthcare Workers, Mentor Mothers, and Patients’ Experiences. Healthcare. 2021; 9(3):328. https://doi.org/10.3390/healthcare9030328
Chicago/Turabian StyleIbu, Josephine Moshe, and Euphemia Mbali Mhlongo. 2021. "The Mentor Mothers Program in the Department of Defense in Nigeria: An Evaluation of Healthcare Workers, Mentor Mothers, and Patients’ Experiences" Healthcare 9, no. 3: 328. https://doi.org/10.3390/healthcare9030328
APA StyleIbu, J. M., & Mhlongo, E. M. (2021). The Mentor Mothers Program in the Department of Defense in Nigeria: An Evaluation of Healthcare Workers, Mentor Mothers, and Patients’ Experiences. Healthcare, 9(3), 328. https://doi.org/10.3390/healthcare9030328







