Distinct Ground Reaction Forces in Gait between the Paretic and Non-Paretic Leg of Stroke Patients: A Paradigm for Innovative Physiotherapy Intervention
Abstract
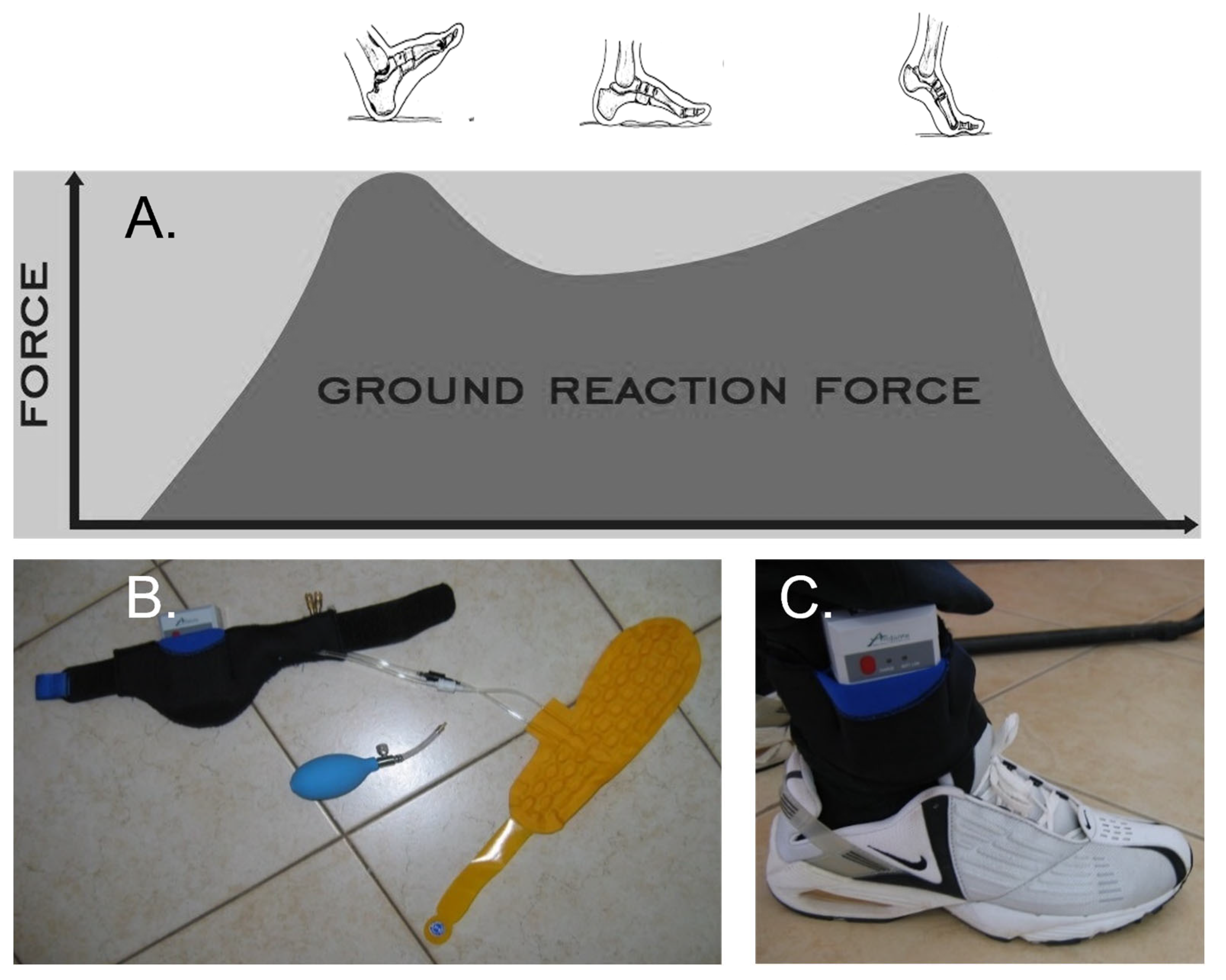
:1. Introduction
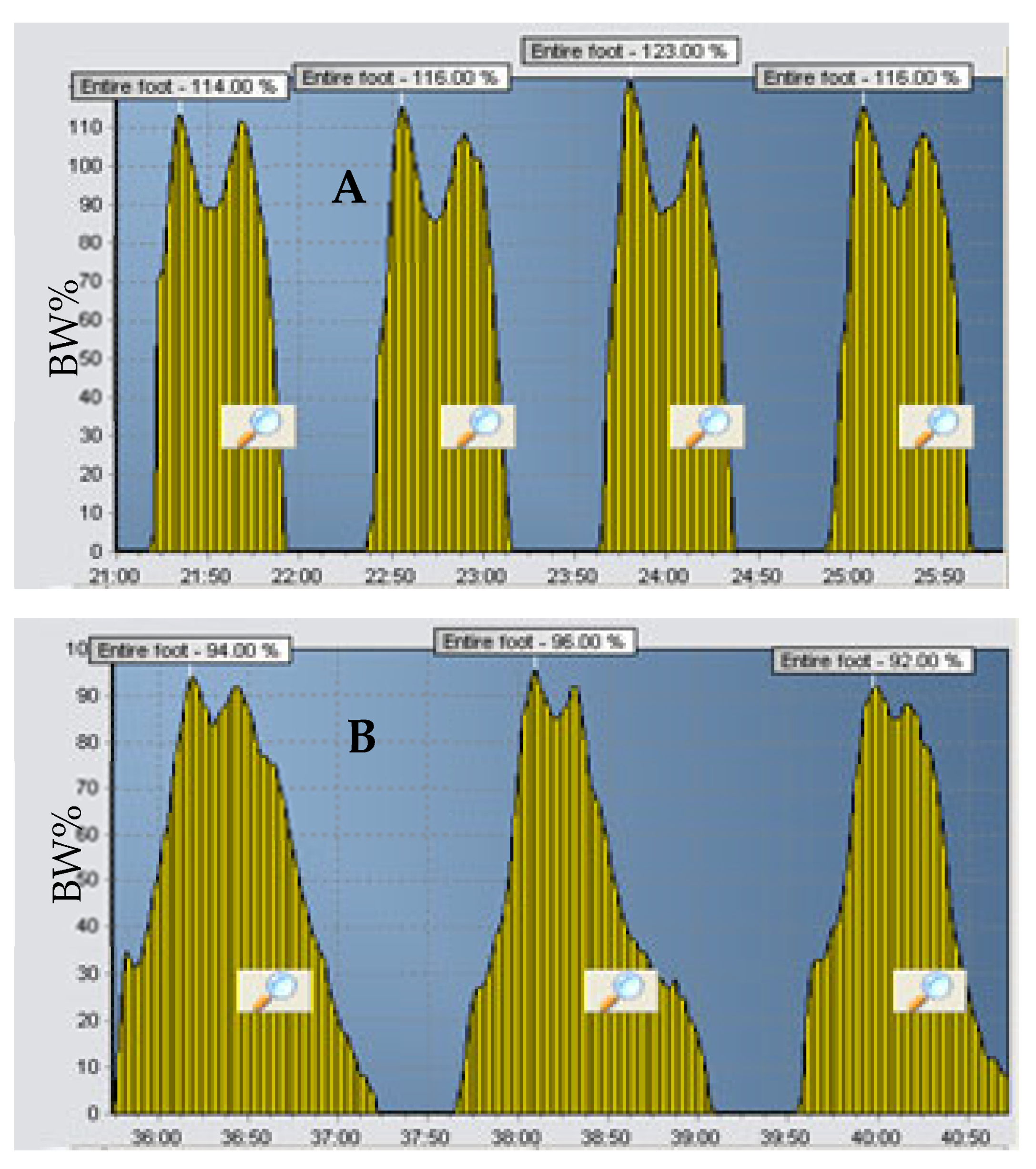
2. Presentation of Two Cases
3. Discussion
4. Conclusions/Clinical Message
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Winiarski, S.; Rutkowska-Kucharska, A. Estimated ground reaction force in normal and pathological gait. Acta Bioeng. Biomech. 2009, 11, 53–60. [Google Scholar] [PubMed]
- Vaverka, F.; Elfmark, M.; Svoboda, Z.; Janura, M. System of gait analysis based on ground reaction force assessment. Acta Gymnica 2015, 45, 187–193. [Google Scholar] [CrossRef] [Green Version]
- Li, S.; Francisco, G.E.; Zhou, P. Post-stroke Hemiplegic Gait: New Perspective and Insights. Front. Physiol. 2018, 9, 1021. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jørgensen, H.S.; Nakayama, H.; Raaschou, H.O.; Olsen, T.S. Intracerebral hemorrhage versus infarction: Stroke severity, risk factors, and prognosis. Ann. Neurol. Off. J. Am. Neurol. Assoc. Child Neurol. Soc. 1995, 38, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Winter, D.A. Kinematic and kinetic patterns in human gait: Variability and compensating effects. Hum. Mov. Sci. 1984, 3, 51–76. [Google Scholar] [CrossRef]
- Li, S. Spasticity, Motor Recovery, and Neural Plasticity after Stroke. Front Neurol. 2017, 8, 120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lauziere, S.; Betschart, M.; Aissaoui, R.; Nadeau, S. Understanding spatial and temporal gait asymmetries in individuals post stroke. Int. J. Phys. Med. Rehabil. 2014, 2, 201. [Google Scholar]
- Hsiao, H.-Y.; Gray, V.L.; Borrelli, J.; Rogers, M.W. Biomechanical control of paretic lower limb during imposed weight transfer in individuals post-stroke. J. Neuroeng. Rehabil. 2020, 17, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Barroso, F.O.; Torricelli, D.; Molina-Rueda, F.; Alguacil-Diego, I.M.; Cano-De-La-Cuerda, R.; Santos, C.; Moreno, J.C.; Miangolarra-Page, J.C.; Pons, J.L. Combining muscle synergies and biomechanical analysis to assess gait in stroke patients. J. Biomech. 2017, 63, 98–103. [Google Scholar] [CrossRef]
- Wall, J.C.; Turnbull, G.I. Gait asymmetries in residual hemiplegia. Arch. Phys. Med. Rehabil. 1986, 67, 550–553. [Google Scholar]
- Bureš, V.; Ponce, D.; Čech, P.; Mls, K. The effect of trial repetition and problem size on the consistency of decision making. PLoS ONE 2019, 14, e0216235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fukuchi, C.; Fukuchi, R.K.; Duarte, M. Effects of walking speed on gait biomechanics in healthy participants: A systematic review and meta-analysis. Syst. Rev. 2019, 8, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kokolevich, Z.M.; Biros, E.; Tirosh, O.; Reznik, J.E. Distinct Ground Reaction Forces in Gait between the Paretic and Non-Paretic Leg of Stroke Patients: A Paradigm for Innovative Physiotherapy Intervention. Healthcare 2021, 9, 1542. https://doi.org/10.3390/healthcare9111542
Kokolevich ZM, Biros E, Tirosh O, Reznik JE. Distinct Ground Reaction Forces in Gait between the Paretic and Non-Paretic Leg of Stroke Patients: A Paradigm for Innovative Physiotherapy Intervention. Healthcare. 2021; 9(11):1542. https://doi.org/10.3390/healthcare9111542
Chicago/Turabian StyleKokolevich, Zoe Mass, Erik Biros, Oren Tirosh, and Jacqueline Elise Reznik. 2021. "Distinct Ground Reaction Forces in Gait between the Paretic and Non-Paretic Leg of Stroke Patients: A Paradigm for Innovative Physiotherapy Intervention" Healthcare 9, no. 11: 1542. https://doi.org/10.3390/healthcare9111542
APA StyleKokolevich, Z. M., Biros, E., Tirosh, O., & Reznik, J. E. (2021). Distinct Ground Reaction Forces in Gait between the Paretic and Non-Paretic Leg of Stroke Patients: A Paradigm for Innovative Physiotherapy Intervention. Healthcare, 9(11), 1542. https://doi.org/10.3390/healthcare9111542






